Excretory system
Excretion is the removal of waste substances of metabolic reactions, toxic materials and substances above requirements.
The excretory system focuses on addressing two major issues:
maintaining osmotic balance - managing the water and solutes in the body
remove metabolic waste - carbon dioxide or nitrogenous wastes, etc.
Many organs play roles in the excretory system:
The skin → excrete water and substances
The liver → involved in detoxification and produces urea
The lungs → excrete gas waste carbon dioxide
The kidneys → excrete urea and excess water and ions
The role of the liver
Many digested food molecules absorbed into the blood in the small intestine are carried to the liver for assimilation (when food molecules are converted to other molecules that the body needs)
These include amino acids, which are used to build proteins such as fibrinogen, a protein found in blood plasma that is important in blood clotting
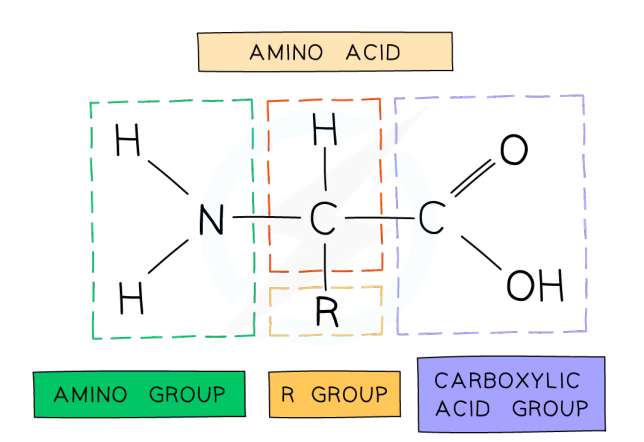
Excess amino acids absorbed in the blood that are not needed to make proteins cannot be stored, so they are broken down in a process called deamination Enzymes in the liver split up the amino acid molecules
The part of the molecule which contains carbon is turned into glycogen and stored
The other part, which contains nitrogen, is turned into ammonia, which is highly toxic, and so is immediately converted into urea, which is less toxic
The urea dissolves in the blood and is taken to the kidney to be excreted
A small amount is also excreted in sweat
In deamination, the nitrogen-containing amino group is removed and converted into ammonia and then urea to be excreted
Urinary system
 PARTS
PARTS
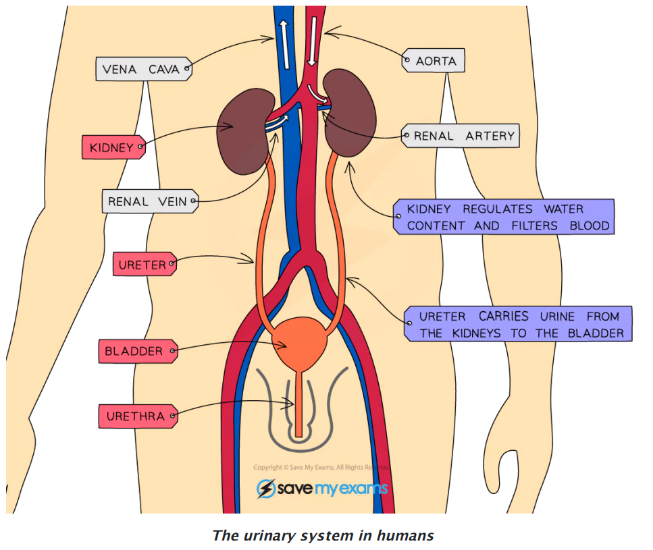
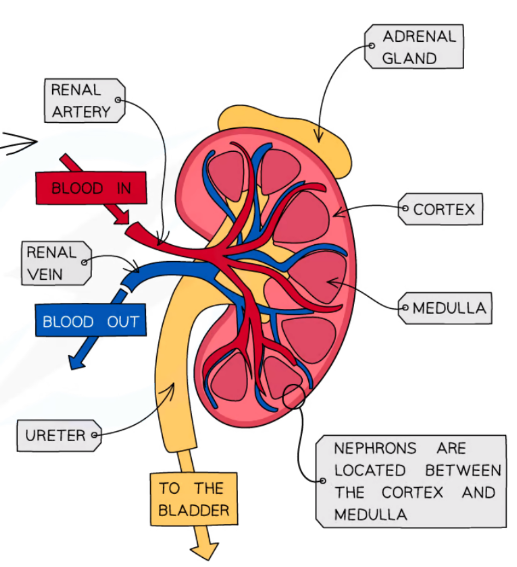
Kidneys - two bean-shaped organs that filter the blood
Cortex - the outer region of the kidney; the cortex contains nephrons.
Medulla - the inner region of the kidney.
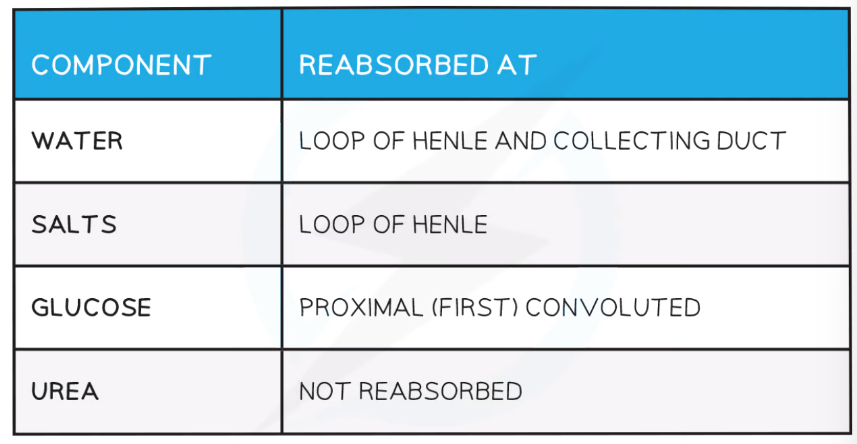
Tubule - All glucose, most water and some salts are reabsorbed into the blood in the tubule (after being filtered out in the glomerulus). This prevents the loss of too much water. Urea is not reabsorbed, leading to a high concentration of urea in the urine.
Nephron - the nephron is the functional unit of the kidney. It contains the glomerulus,
which is where the blood is filtered and glucose, urea, water and salts are removed.
Bladder - the single sac organ that will store urine produced by the kidney
Ureters - there are two and they drain urine produced from the kidneys to the bladder
Urethra - a single tube where urine will travel out of the body from the bladder
Blood is filtered by the KIDNEYS, producing urine, a portion of the body’s waste products that must be excreted.
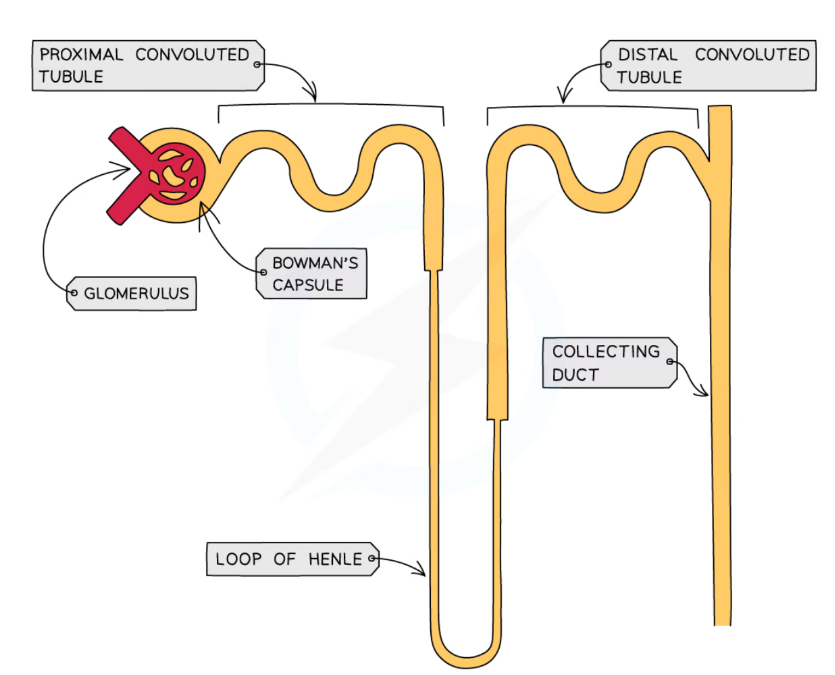
THE NEPHRON;
Each kidney has tons of them - they are the functional unit of the kidney. Its overall goal is to process waste products from the blood to create urine. The contents of the nephrons drain into the innermost part of the kidney and the urine collects D
before going down to the bladder.
The nephrons start in the cortex of the kidney, loop down into the medulla and back up to the cortex.
THE PROCESS:
Glomerulus - a specialised mass of capillaries that increase the blood pressure, the Bowman’s capsule surrounds it.
Blood pressure forces fluid from the blood in the glomerulus into the Bowman’s capsule. Once this fluid is in the Bowman’s capsule, the fluid is called the filtrate. The filtrate consists of water, some glucose and amino acids, salts, H+ ions, bicarbonate ions, medications and vitamins, and urea (a nitrogenous waste produced by the liver that the body needs to get rid of). This is the process of ULTRAFILTRATION.
The nephron is going to take this filtrate to process it.
some filtrate is reabsorbed back into the fluid surrounding the nephron (interstitial fluid) and then back into the body. This is SELECTIVE REABSORPTION
Proximal tubule - glucose and amino acids - are all reabsorbed here (some percentage of these aren’t absorbed). H+ and ammonium are secreted into the tubule.
Loop of Henle -water and remaining NaCl diffuse out.
Distal Convoluted tubule - H+, ammonium, potassium, etc. are secreted while water and bicarbonate are reabsorbed
collecting duct - hormonal control regulates the amount of water here (the permeability of the duct to water) - depends on the level of hydration
urine created by the kidneys go down the two ureters to be stored in the bladder until it’s finally excreted through the urethra
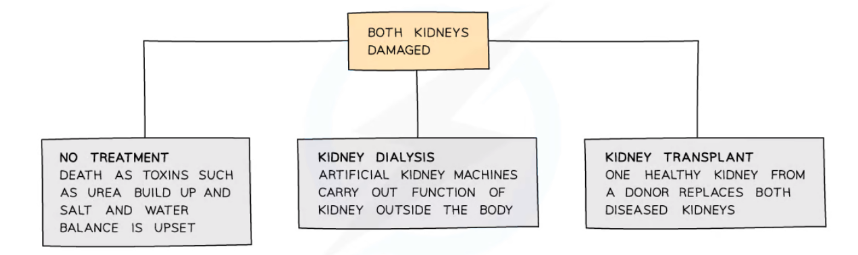
Kidney Failure
The kidneys might not work properly for several reasons, including accidents or disease.
Humans can survive with one functioning kidney, but if both are damaged then there will quickly be a build-up of toxic wastes in the body which will be fatal if not removed
 Health → Diuretics usually aim to increase the amount of water in the filtrate so there is more water in the urine. Dialysis helps filter the blood and helps in osmoregulation.
Health → Diuretics usually aim to increase the amount of water in the filtrate so there is more water in the urine. Dialysis helps filter the blood and helps in osmoregulation.
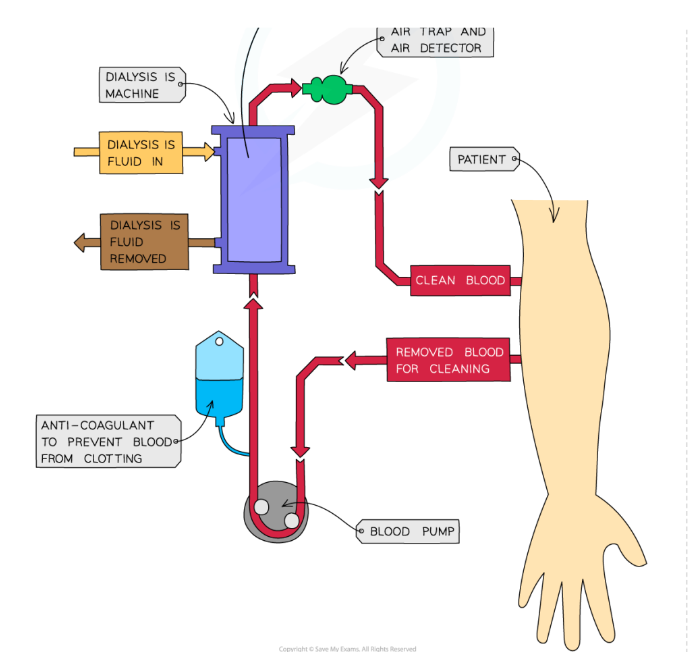
Kidney Dialysis → an artificial method of filtering the blood to remove toxins and excess substances - acts as an artificial kidney.
unfiltered blood is taken from an artery in the arm, pumped into the dialysis machine, and then returned to a vein in the arm.
Inside the machine the blood and dialysis fluid are separated by a partially permeable membrane - the blood flows in the opposite direction to dialysis fluid, allowing exchange to occur between the two where a concentration gradient exists
Dialysis fluid contains:
a glucose concentration similar to a normal level in the blood
a concentration of salts similar to a normal level in blood
no urea
As the dialysis fluid has no urea in it, there is a large concentration gradient -
meaning that urea diffuses across the partially permeable membrane, from the
blood to the dialysis fluid
As the dialysis fluid contains a glucose concentration equal to a normal blood
sugar level, this prevents the net movement of glucose across the membrane as no
concentration gradient exists
As the dialysis fluid contains a salt concentration similar to the ideal blood concentration, movement of salts across the membrane only occurs where there is an imbalance - if the blood is too low in salts, they will diffuse into the blood; if the blood is too high in salts, they will diffuse out of the blood.
The fluid in the machine is continually refreshed so that concentration gradients are maintained between the dialysis fluids and the blood.
Dialysis may take 3-4 hours to complete and needs to be done several times a week to prevent damage to the body from the buildup of toxic substances in the blood
An anticoagulant is added to the blood before it runs through the machine to prevent
the blood from clotting and slowing the flow
Kidney transplants vs dialysis:
Kidney transplants are a better long-term solution to kidney failure than dialysis; however, there are several disadvantages to kidney transplants, including:
Donors wonʼt have the same antigens on cell surfaces so there will be some immune response to the new kidney (risk of rejection is reduced – but not removed – by ʻtissue typingʼ the donor and the recipient first)
This has to be suppressed by taking immunosuppressant drugs for the rest of their lives – these can have long-term side effects and leave the patient vulnerable to infections.
There are not enough donors to cope with demand
However, if a healthy, close-matched kidney is available, then the benefits of a transplant over dialysis include:
the patient has much more freedom as they are not tied to having dialysis several times a week in one place
their diets can be much less restrictive than they are when on dialysis
use of dialysis machines is costly so this cost is removed
a kidney transplant is a long-term solution whereas dialysis will only work for a limited time