L19- Adaptive Immunity and Immunization Pt.1
1/56
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
57 Terms
Innate and adaptive immunity work together…
to protect the host.
Innate is more…
generalized protection while adaptive is more specific and long lasting.
3 Functions of adaptive immunity:
Recognize foreign molecules
Defend the host
Remember the foreign molecules.
5 characteristics of Adpative Immunity
Discriminate
Specificity
Diversity
Timing
Memory
Discriminate-
Between self and non-self
Specificity-
Respond to specific antigens
Diversity-
Great diversity in the types of
antibodies generated.
Timing-
Adaptive immunity takes some time to kick in.
Memory-
Memory cells are generated to
protect against re-exposure.
Components of Adaptive Immunity
Also known as acquired immunity against a specific agent.
Adaptive immunity relies on the activity of T and B lymphocytes.
This response will clear the foreign molecule from the body and develop memory.
A later infection can trigger memory cells.
Much fast response than the first encounter.
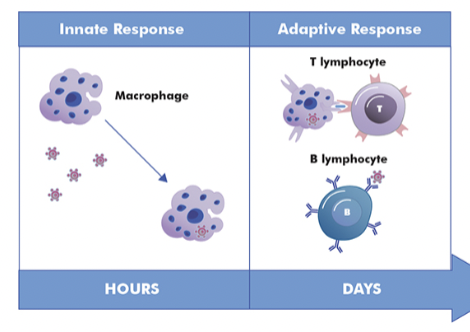
Adaptive immunity relies on the activity of…
T and B lymphocytes
Adaptive Immunity includes what 2 things?
Humoral
Cell-mediated Immunity
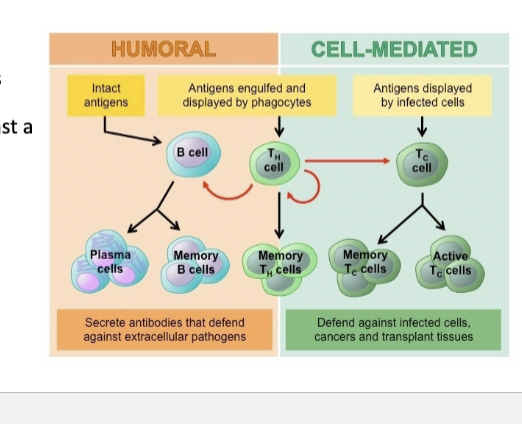
Humoral Response
B-cells producing antibodies against a pathogen
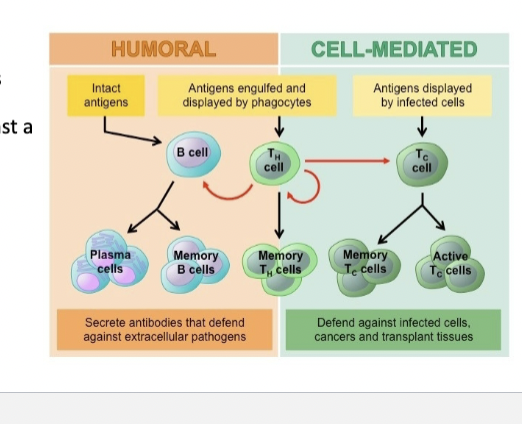
Cell-mediated immunity:
T-cell recognize abnormal antigens on host cells (from virus or tumors).
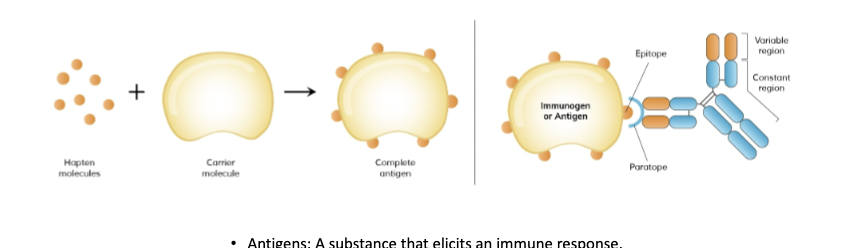
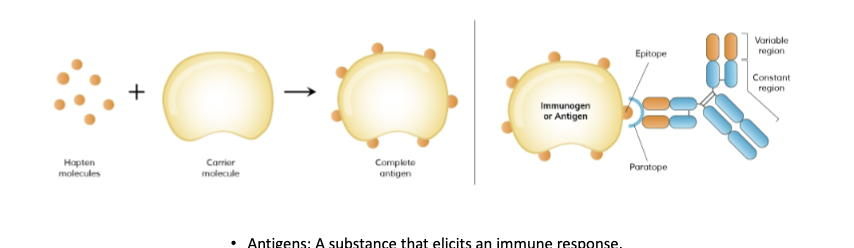
Antigens:
A substance that elicits an immune response.
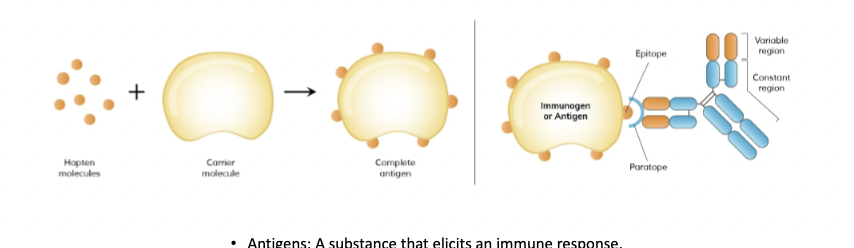
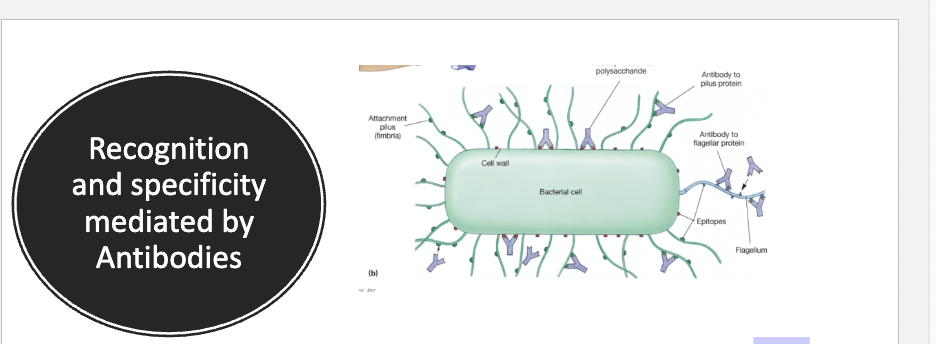
Structure of Antigens
Complex in structure.
Polysaccharides /glycoproteins/nucleoproteins.
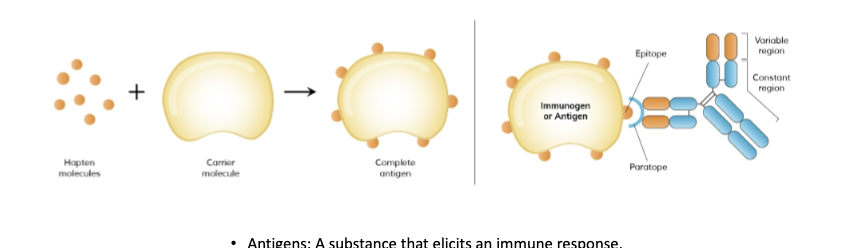
Valent
Number of epitopes on an antigen (the specific small part of an antigen that an antibody or T-cell receptor recognizes and binds to)
Antigens have several epitopes
Multivalent is better because it means more than 1 kind of antibody can attach to the same antigen.
Where are antigens found?
Found on the surface of bacteria (cell wall, membrane, flagella), viruses and determine by organism's genetic information.
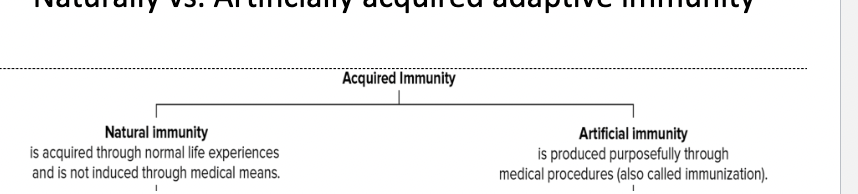
2 types of acquired apdaptive immunity
Natural Immunity
Artificial immunity
Naturally acquired adaptive immunity
Obtained by specific disease.
Antibodies produced due to antigens on an invading infectious agent. Memory.
Antibodies transferred to fetus: via placenta or colostrum.
Artificially acquired adaptive immunity
Receiving an antigen via injection (vaccine)
Immunization
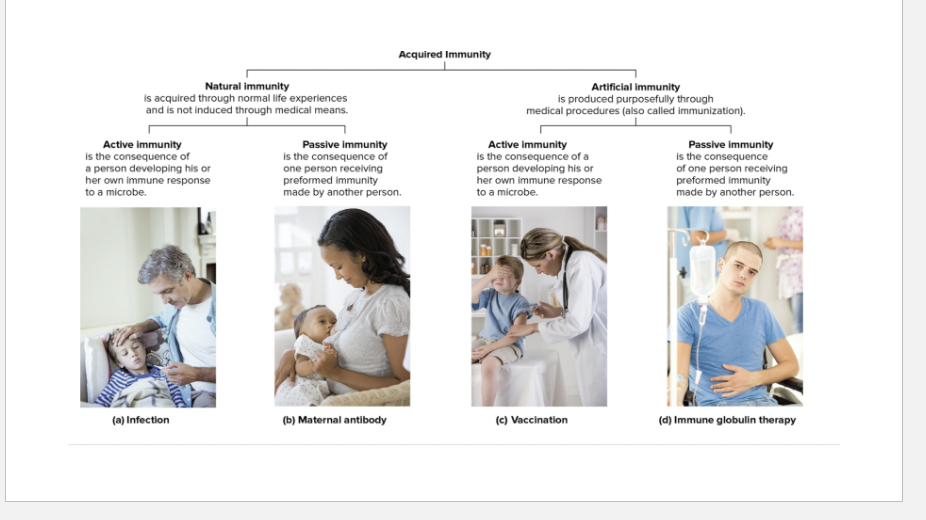
Active Immunity
The person’s own immune system activates lymphocytes and produces antibodies.
Immunity can last for weeks to a lifetime.
Antigen is remembered.
Naturally acquired active immunity: Person is exposed to infectious agent.
Artificially acquired active immunity: Person is exposed to a vaccine
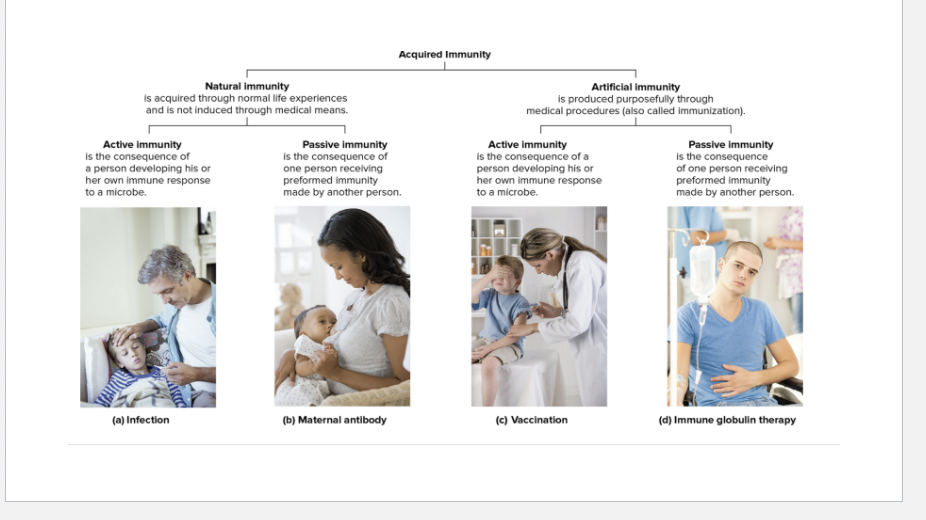
Passive Immunity
Antibodies are introduced to the body. Antibodies are not made by the person’s immune system.
Naturally acquired passive immunity: made by the mother's immune system and transferred to offspring
Artificially acquired passive immunity: antibodies made by another host are introduced into a new host.
Ex :snake antivenin injection.
Antibodies:
also called immunoglobulin
is a protein that is made to bind a specific antigen.
Can bind to specific epitopes.
The body can recognize the foreign molecules as non-self using antibodies.
The body still needs a mechanism to recognize self as self.
The system in place to do this is called the Major Histocompatibility Complex.
The Major Histocompatibility Complex
Composed of a collection of genes located on the human
chromosome 6 called the Human Leukocyte Antigen (HLA)
(polymorphic).There are 3 classes of MHC proteins
Class I
Class II
Class III
Class I MHC proteins:
proteins expressed in nucleated body cells
Class II MHC proteins:
Proteins expressed in antigen presenting cells such as macrophages, dendritic cells , and B cells.
Class III MHC proteins:
secreted proteins that function in the immune process.

MHC Class I components
Consists of a 2-protein complex.
Large alpha chain that spans the membrane, small beta chain.
Together they make a binding pocket that binds to
antigens.
Recognizes self and non-self.
If it binds a non-self antigen, it signals an immune response.
Not present on RBC since they are anucleated.
Many forms of Class I MHC exists.
Class I typing is considered for organ transplant.
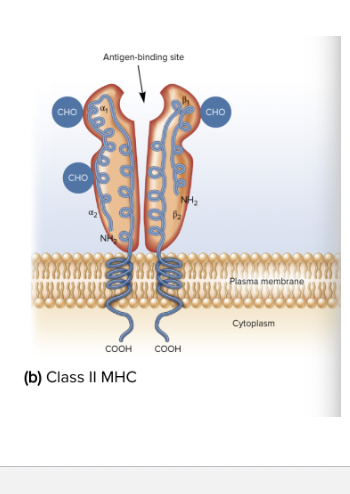
Class II MHC Components
Class II MHC are only found on antigen presenting cells.
This plays a major role in antibody production.
Generates a deeper binding pocket than MHC I.
Can bind self and non-self.
Triggers a reaction when bound to non-self antigen.
Antigen processing
refers to the process of processing and attaching the antigen to the MHC.
Endogenous antigen processing:
Molecules in the cell (self or pathogen) are digested in a continuous process of recycling proteins in the cells.
This process sends the digested fragments to the ER.
The molecules binds to one of the many MHC class I receptors.
Exogenous antigen process
bind molecules that enter the cell from outside (bacteria, viruses, toxins that come into the cells)
MHC Class II
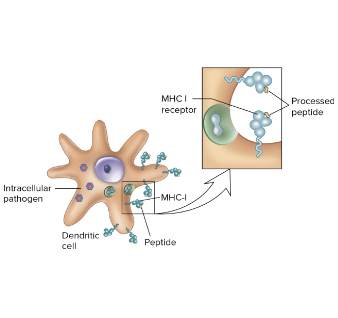
Antigen processing- Class I MHC
Endogenous Antigen Processing ( digestion and recycling of proteins in cells. digested fragments sent to ER, and moplecules bind to MHC class I receptors)
The MHC then presents that molecule to a type of T cell called CD8+ or cytotoxic T cell which determines if the molecule is self or non-self.
If self, it leaves it alone. If non-self, the T cell with kill
the host cell.
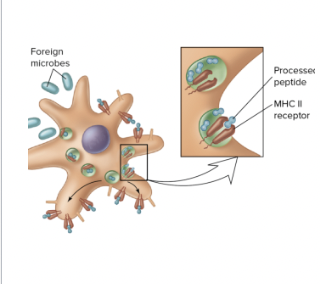
Antigen processing- Class II
Exogenous Antigen Processing
Class II will only bind molecules that enter the cell from
outside (bacteria, viruses, toxins that come into the cells) and undergo a process called exogenous antigen process.
Antigen presenting cells (macrophages, DC) will ingest the
invader.The digested foreign molecules are attached to the MHC I molecule.
Those that fit the pocket will remain bound and this complex can recognize by T cells called CD4+ (helper cells).
CD4+ do not kill the host cell like CD8+, rather they release
cytokines that signal that an infection is present.This results in a more global effect.
Differentiation of stem cells into…
B cells and T cells.
Occurs in the bone marrow and thymus, respectively.
Thymus in adult vs. children
Still active and differentiating T-cells, but at a lower rate.
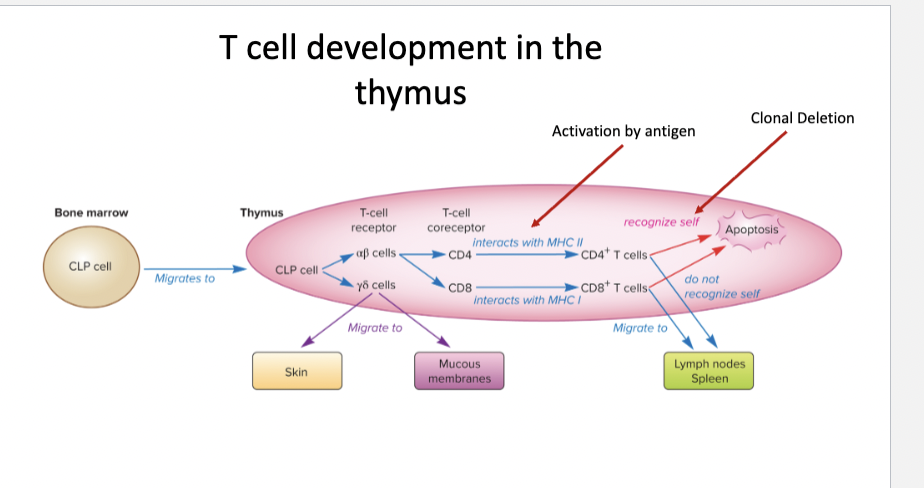
T cell development in the thymus
The thymus determines what kind of T-cell develops.
Depends on the T-cell receptor and coreceptor.
Receptor alpha:Beta
Receptor Gamma:Delta
Before leaving the thymus, all T cells are screened to determined if they can recognize self.
If they can, they undergo apoptosis.
This results in nearly 98% of T cells dying.
Those that mature are still naïve since they have not responded to antigen by Antigen presenting cells.
Receptor alpha:Beta-
The majority of T cells.
Remain in the thymus where they receive a coreceptor.
Countless possibilities of co-receptors determined by molecules called cluster of differentiation (CD).
The CD4+ coreceptor(T-helper cells) on the T cell will allow it to interact with MHC class II
The CD8+ coreceptor(Cytotoxic T-cells) on the T cell will allow it to interact with MHC class
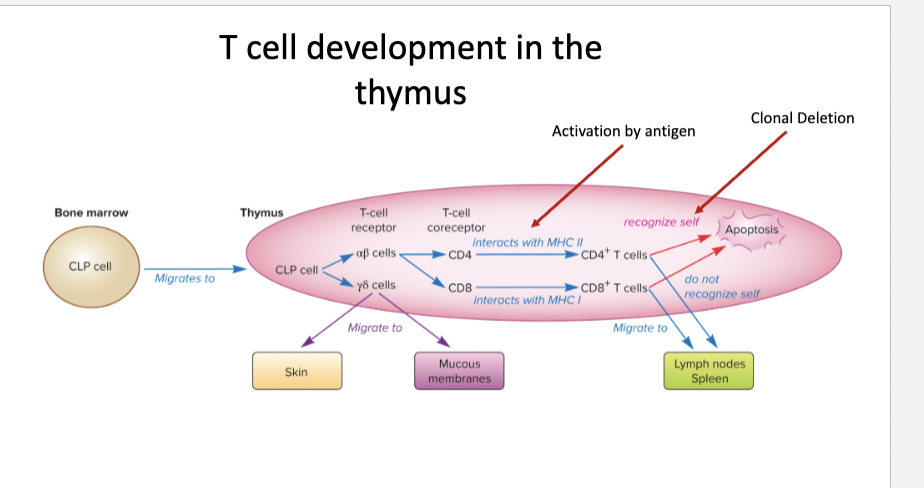
Receptor Gamma:Delta-
Migrate to the lymphoid tissue and do not receive a coreceptor.
Found in skin/mucus membranes
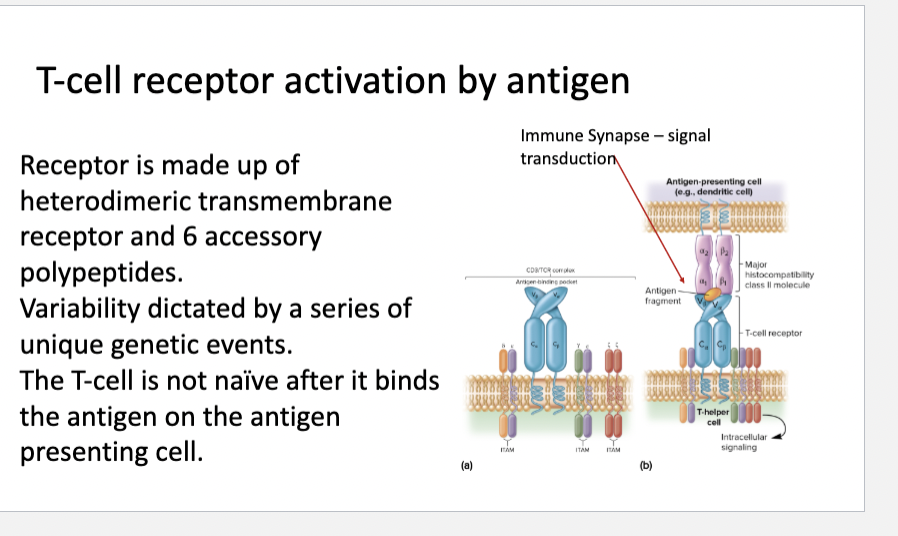
T-cell receptor activation by antigen
Receptor is made up of heterodimeric transmembrane receptor and 6 accessory polypeptides.
Variability dictated by a series of unique genetic events.
The T-cell is not naïve after it binds the antigen on the antigen presenting cell.
Immune Synapse – signal transduction
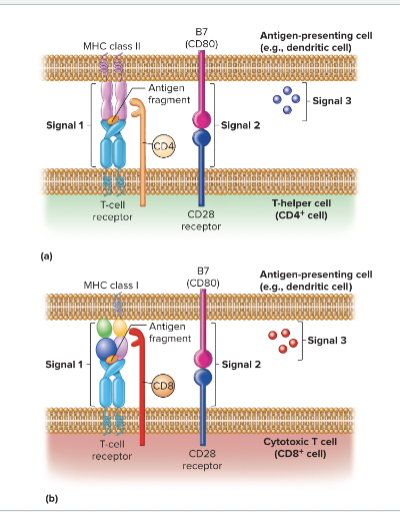
T-cell activation Signal 2
Signal 1: MHC binding to TCR.
Signal 2: B7 receptor on APC binds to on of the T-cell accessory receptors.
Signal 3: is not well understood but includes a chemical signal between the 2 cells.

Recognition of self: Clonal Deletion
Takes place in the bone marrow and thymus during fetal development.
Removes lymphocytes that have receptors for self antigens.
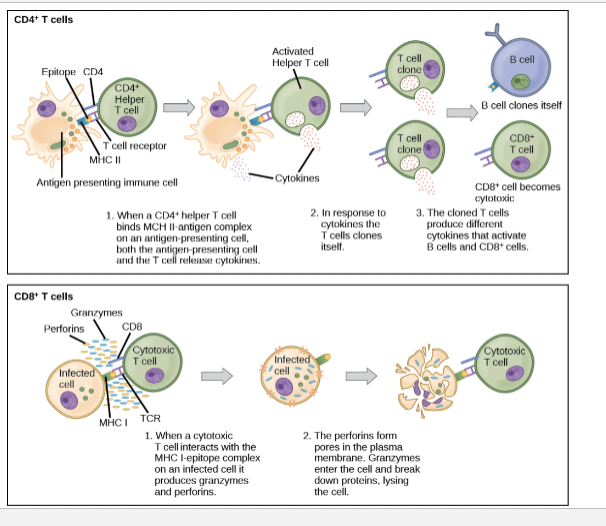
2 types of T-cells
T-helper cells
Cytotoxic T cells
T-helper cells:
Known as CD4+ T cells.
Interferon and interleukin can stimulate the differentiation of TH0 into TH1 or TH2 (most important 2).
TH1- Activates macrophages, inflammation, interleukins, interferons, tumor necrosis factor.
Production of interleukins + interferons further amplifies the effect.TH2- Activates antibody response (B-cells to generate antibodies). Activates IL-4-6, and IL 13
which responses to worm infections.TH17- Recruits neutrophils and inflammatory response.
Tregs- help decrease the immune response by producing the anti-inflammatory cytokine IL-
10.
TH1-
Activates macrophages, inflammation, interleukins, interferons, tumor necrosis factor.
Production of interleukins + interferons further amplifies the effect.
TH2-
Activates antibody response (B-cells to generate antibodies).
Activates IL-4-6, and IL 13 which responses to worm infections.
TH17-
Recruits neutrophils and inflammatory response.
Tregs-
help decrease the immune response by producing the anti inflammatory cytokine IL- 10.
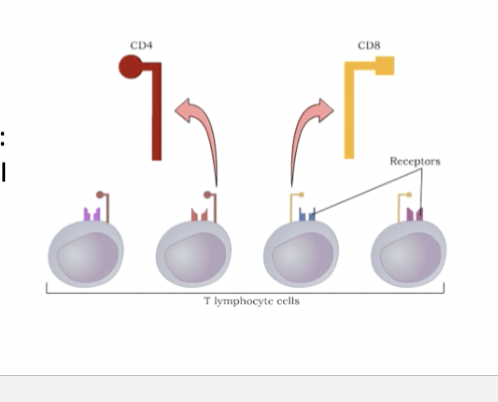
T-cells components
Are found on helper T-cells:
Bind to MHCII
Are found onvcytotoxic T- cells:
Bind to MHCI
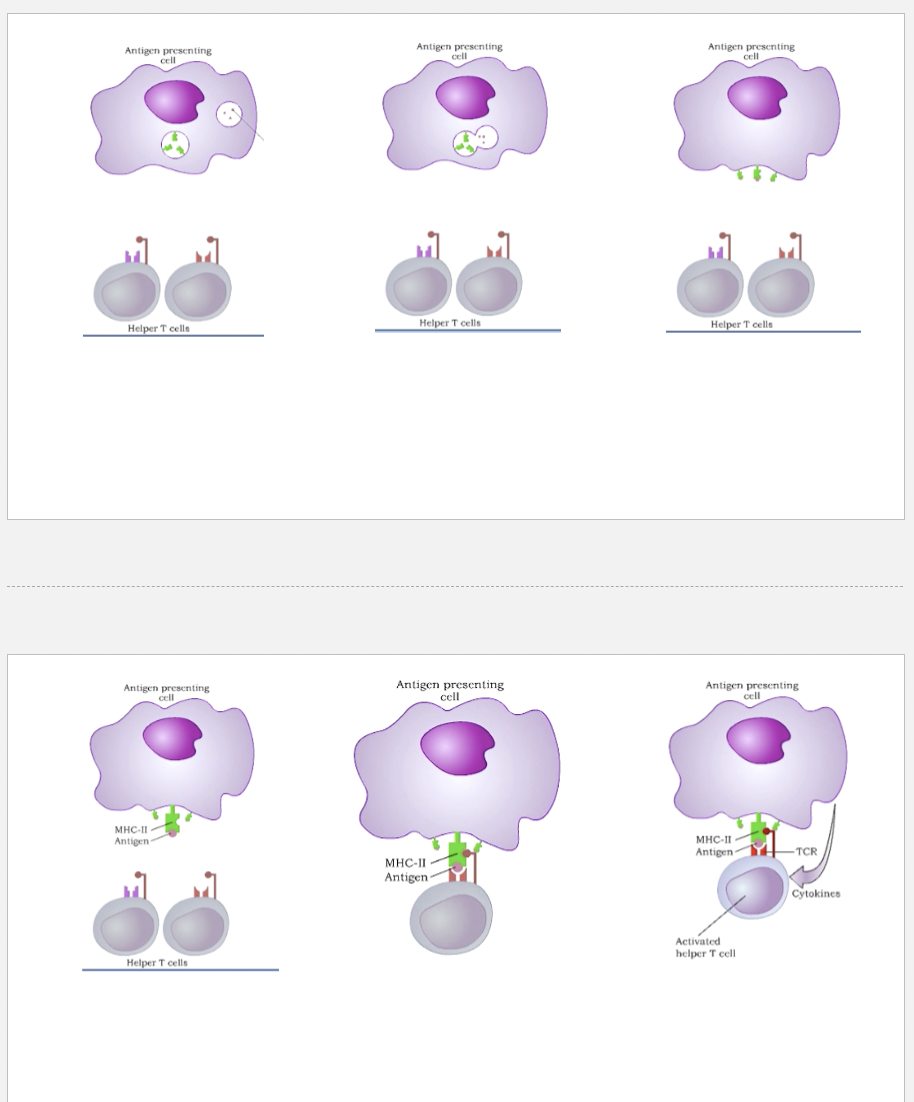
1st step of Cell Mediated Immunity
B-cells, dendritic cells or macrophages encounter pathogenic agent.
They ingest and degrade the pathogen
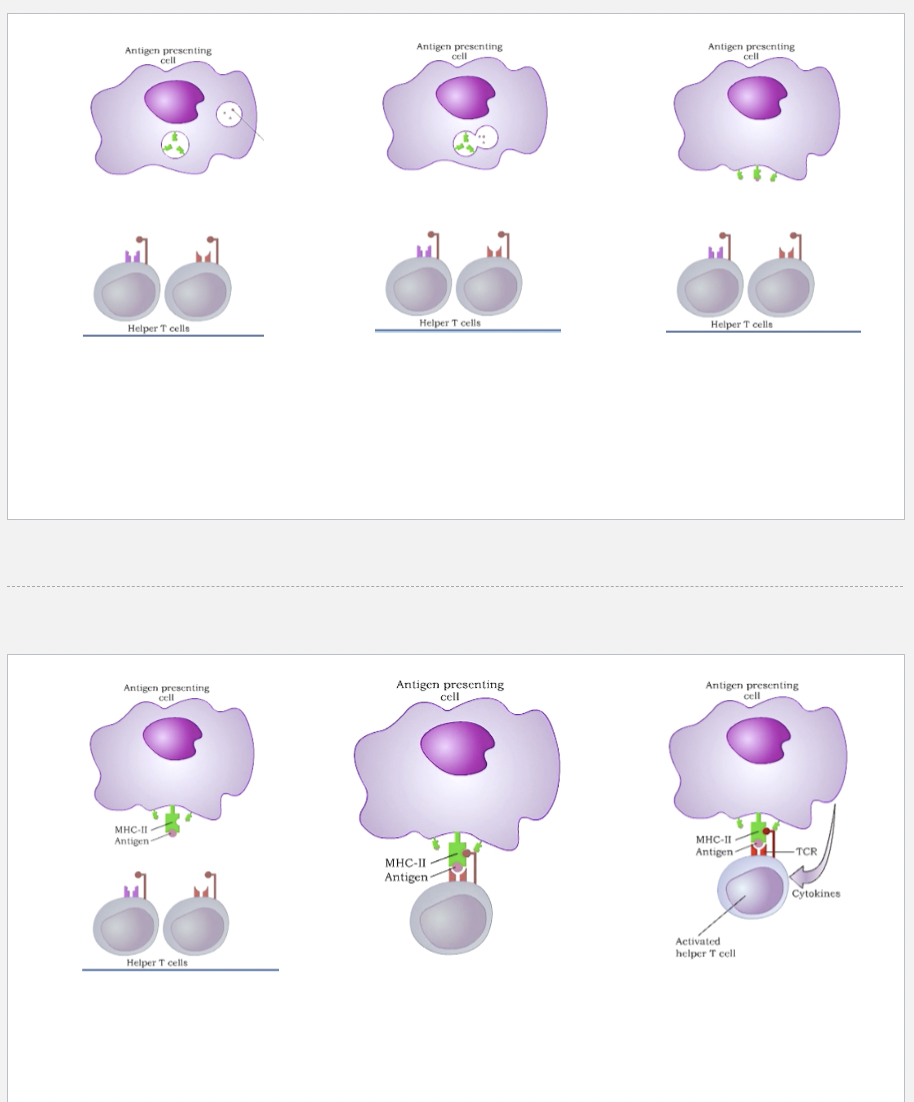
2nd step of Cell Mediated Immunity
Pieces of the pathogen/peptide are associate with MHC and form
an MHC-antigen complex
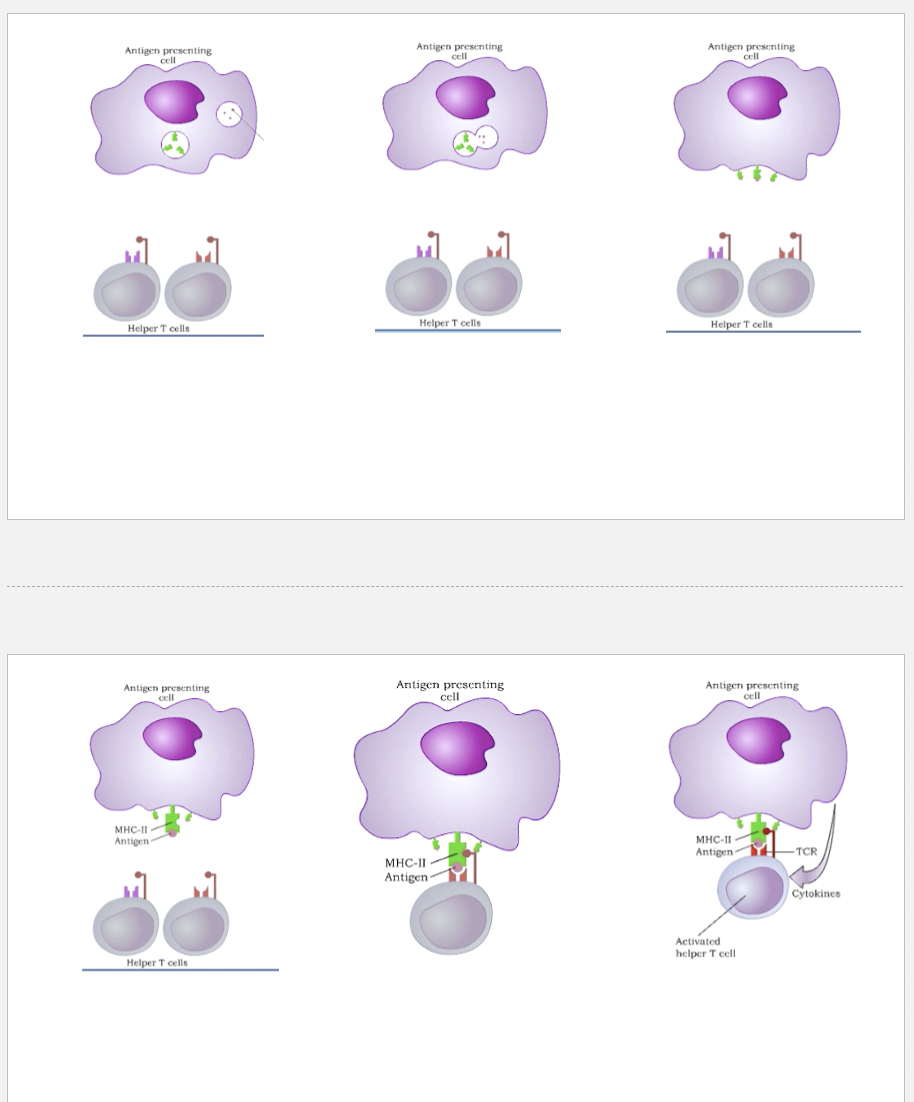
3rd step of Cell Mediated Immunity
MHC-antigen complex is transported to the surface of the dendritic
cells, macrophages, B-cells.
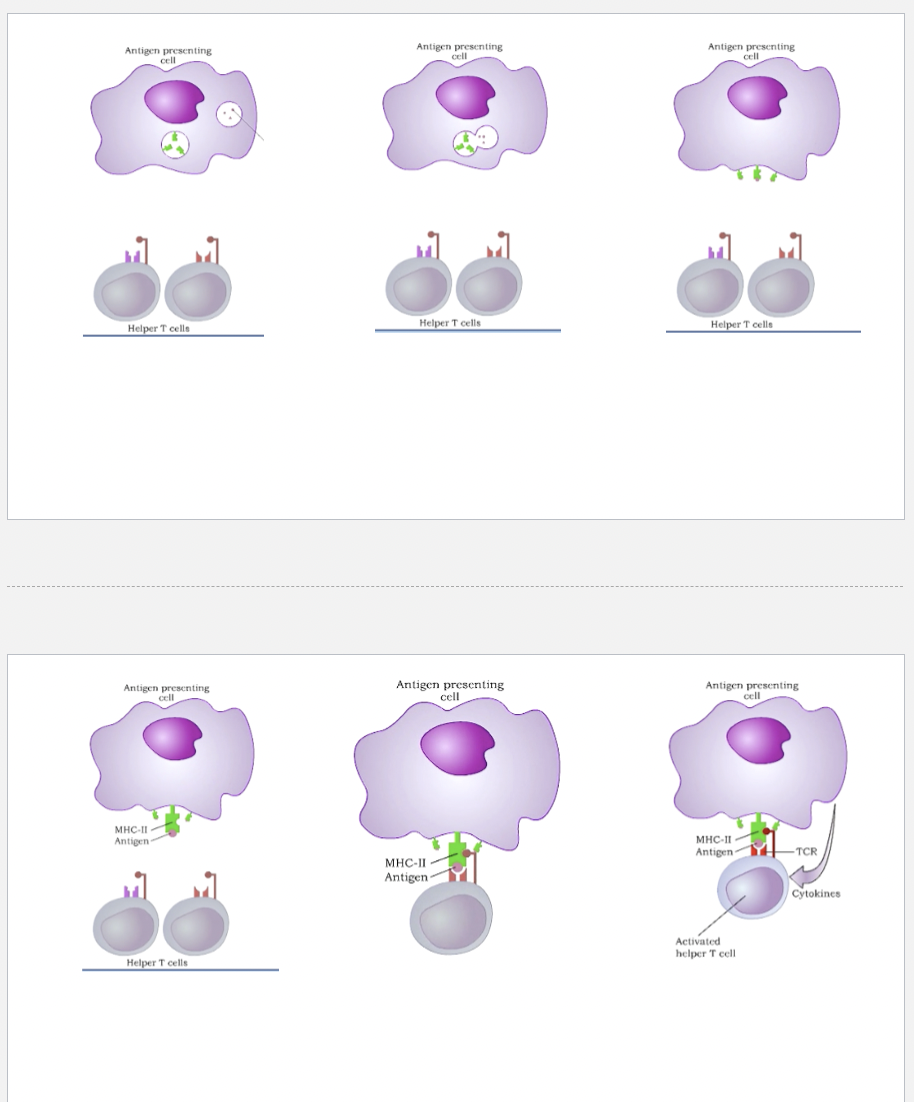
4th step of Cell Mediated Immunity
A T-cell that has the proper antigen receptor can recognize and
bind the antigen on the antigen presenting cell.T-helper cells: activated by MHC-II antigen presenting cells
Cytotoxic T cells: activated by MHC-I (virus, bacterial, cancer cells, organ transplant
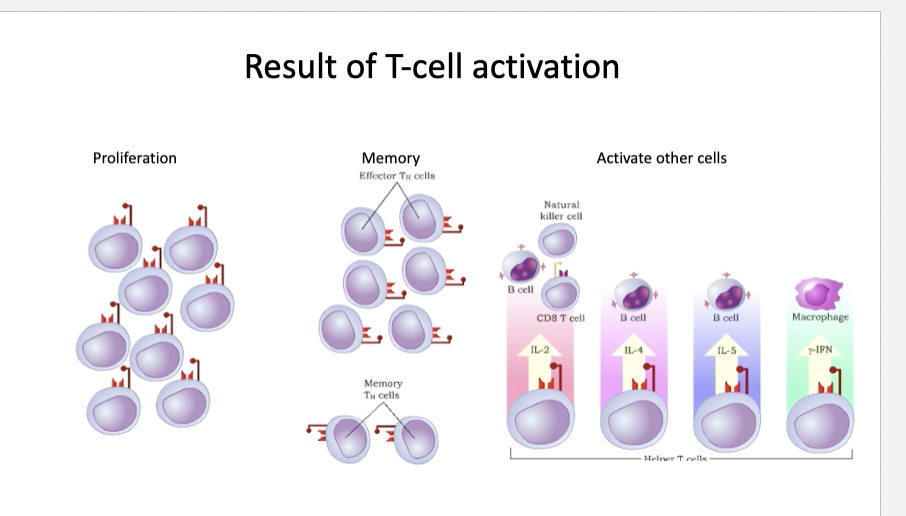
5th step of Cell Mediated Immunity
Once activated, T cells can stimulate other T and B cells or destroy
the infected cell
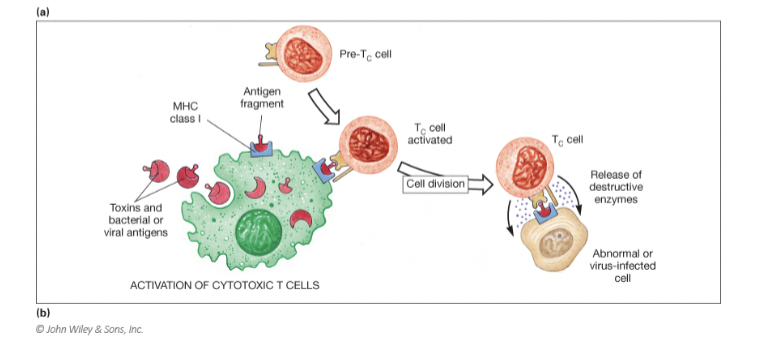
Activation of cytotoxic t-cells
Toxins and bacterial or viral antigens enter cells
MHC Class I binds with antigen fragment
Pre Tc cell binds to the antigen fragment MHC Class I complex
Cell division occurs
Tc cell releases destructive enzymes against abnormal virus infected cell
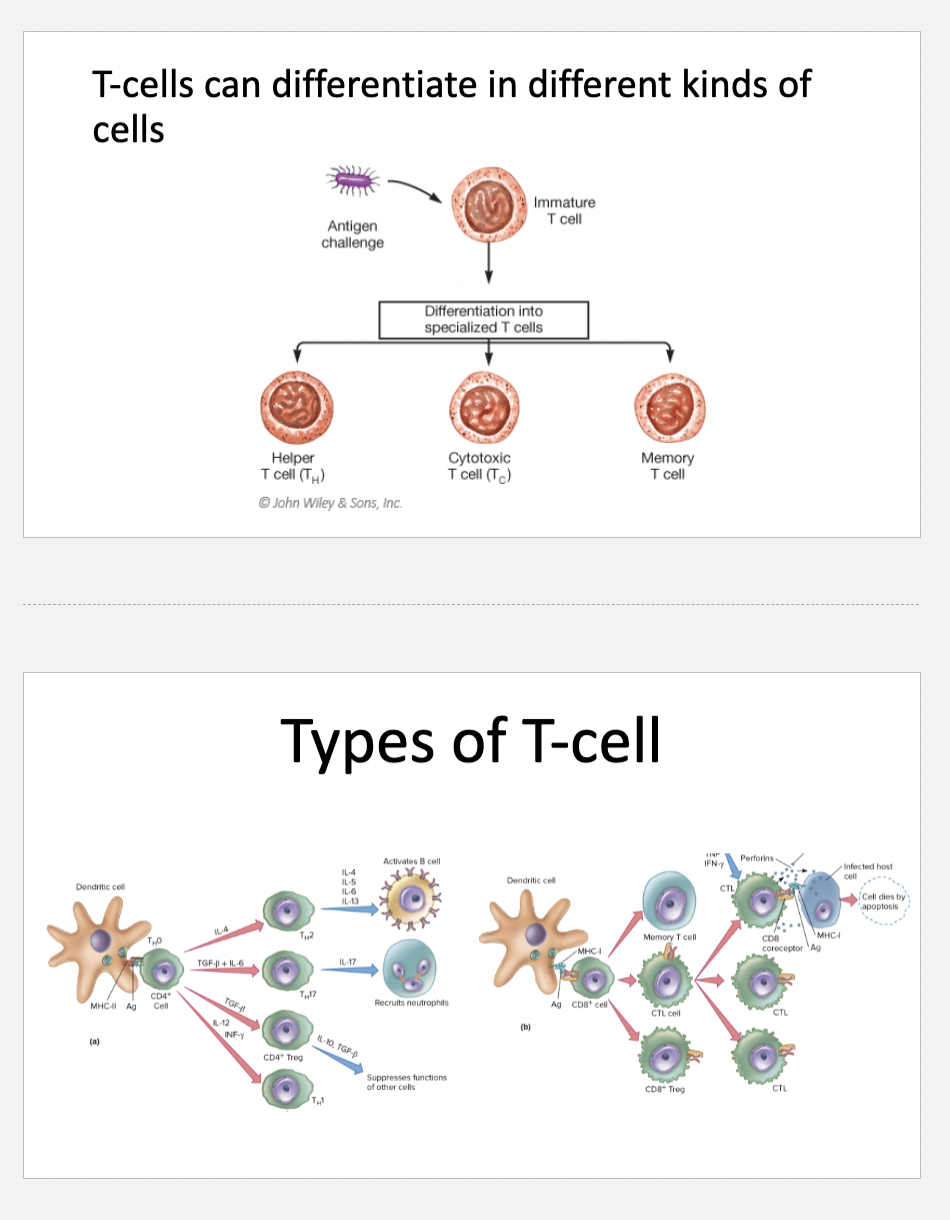
T-cells can differentiate in different kinds of cells
Helper T cell (Th)
Cytotoxic T cells (Tc)
Memory T cell