CHAPTER 12: STRUCTURE & FUNCTIONS OF DENTIN-PULP COMPLEX
1/70
Earn XP
Description and Tags
from book + summer endo basic + ppt/discussion
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
71 Terms
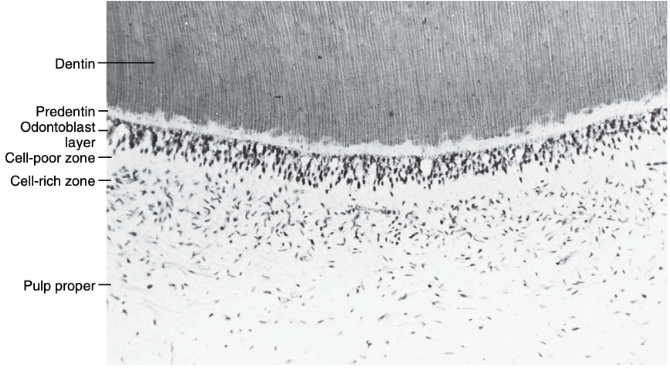
morphologic zones of the pulp
pulp-dentin complex
odontoblast layer
cell-poor zone
cell-rich zone
pulp proper
pulp-dentin complex
function as a single biologic unit
if there is an impact on dentin may affect the pulpal components, and that disturbances in the dental pulp will in turn affect the quantity and quality of the dentin produced.
any stimulus to dentin (caries, trauma, heat) can affect the pulp, and pulpal disease alters dentin formation (reactionary/reparative dentin)
dentin depends on pulp for formation and nourishment
pulp depends on dentin and enamel for protection
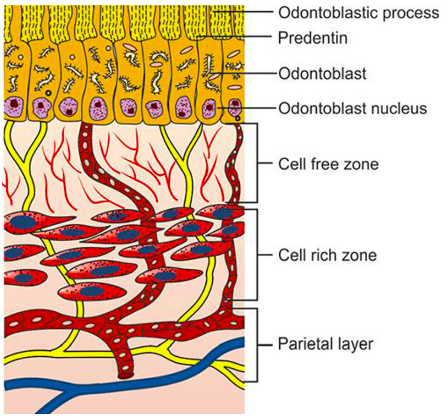
odontoblast layer / zone
consists of odontoblast cell bodies
located immediately beneath predentin
outermost cellular layer of the dental pulp
thickness varies with age and tooth type and location
cell density: coronal pulp > radicular pulp; decreases with aging.
odontoblastic processes extend:
through predentin
into the inner dentin (dentinal tubules)
also contains:
capillaries
nerve fibers
dendritic (immune) cells
replaced by stem-like cells from the cell- rich zone that differentiate into new odontoblasts.
root dentin
has fewer dentinal tubules, so odontoblasts are:
less crowded
spread laterally
tall, columnar
height of odontoblast layer in the coronal pulp (young, active teeth)
shorter
height of odontoblast layer in the radicular pulp
mid-root → cuboidal
near apical foramen → flattened (squamous)
function of odontoblast layer
defense and signaling
regulation of dentin permeability
increase dentin formation to protect pulp
dentin formation throughout life (primary, secondary, tertiary)
sensory transmission via odontoblast processes and nerve endings
palisade arrangement
tall and column-shaped
appearance of odontoblast layer in young teeth
appears 3–5 cells thick, but is actually only one layer
with aging:
pulp chamber narrows
apoptosis helps regulate cell number
odontoblast crowding increases (especially coronally)
—in older teeth, this layer may change: odontoblasts can become smaller or die
30–40 nm wide
narrow spaces between odontoblasts
allow passage of fluids and small molecules
gap junctions
aka: nexuses
formed by connexin proteins
most numerous during primary dentin formation
allow direct passage of:
ions, small signaling molecules
electrical & chemical signals
function:
synchronize odontoblast activity
produce uniform predentin
also connect odontoblasts with:
fibroblast processes in subodontoblastic zone
adherens and desmosomes
aka: zonula adherens
help maintain structural integrity
located mainly in apical portions
provide mechanical attachment
tight junctions
aka: zonula occludens
found mainly in young teeth, located in apical part of odontoblasts
regulate:
permeability between pulp and predentin
movement of substances and keep the pulp environment sealed
restrict passage of:
molecules
ions, fluids
important when dentin is covered by:
enamel & cementum
cell-poor zone
aka: cell-free zone / zone of Weil
this zone doesn’t always appear in young pulps
sensory transmission, lies beneath the odontoblastic layer
may be absent or poorly defined:
in young pulps → rapid dentin formation
in older pulps → reparative dentin formation
prominent only when the pulp is in a relatively stable functional state
cell-poor zone contains:
few cells, many nerves
blood capillaries plexus
cytoplasmic processes of fibroblasts
unmyelinated nerve fibers (Raschkow’s plexus)
approximate width of cell-poor zone
40 μm
function of cell-poor zone
helps to transport nutrients and signals
acts as a transitional area between odontoblasts and deeper pulp
important zone for:
nerve plexus (Raschkow’s plexus)
sensory transmission
nerve plexus of Raschkow
specific structure found in cell-poor zone
cell-rich zone
repair & regeneration
found beneath the cell-poor zone
begins around the time of tooth eruption
forms due to peripheral migration of cells from the pulp core
immune cells migrate in and out in response to antigenic challenge
can be easily recognized because it has more fibroblasts than the pulp proper
function of cell-rich zone
defense and repair
cell replacement / reservoir
source of new odontoblast-like cells after injury
it’s like the backup team that keeps the pulp healthy and functioning
cell-rich zone contains:
immune cells:
stem cells
macrophages
dendritic cells
fibroblasts → most abundant
undifferentiated mesenchymal cells
pulp proper
aka: pulp core / central pulp
vessels & nerves
the central mass of the pulp
explains sensitivity, pulpitis, healing capacity of pulp
is like the heart of the pulp — keeping the tooth nourished, protected, and alive.
pulp proper contains:
loose connective tissue
fibroblasts (most prominent)
ground substance and fibers
larger blood vessels, major nerve trunks
functions of pulp proper
innervation
immune response
responds to injury / defense
support of peripheral pulp zones
supplies nutrients & supports tooth vitality
mild irritation
reactionary dentin
severe injury
reparative dentin
cells of the pulp
mast cell
odontoblast
macrophage
dendritic cell
lymphocyte
odontoblast process
pulp fibroblast
odontoblast
most characteristic & specialized cells
their processes extend into dentinal tubules
the key link between the pulp-dentin complex
fixed & post-mitotic (do not divide after differentiation)
cell body remains outside (periphery) mineralized tissue
presence of odontoblastic processes in tubules makes dentin a living, responsive tissue
responsible for dentinogenesis:
during tooth development
throughout aging
form:
dentin matrix
dentinal tubules
odontoblasts, osteoblasts, cementoblasts similarities
are matrix-forming cells, capable of mineralization
rich in RNA
nuclei with prominent nucleoli → typical features of protein-secreting cells
produce:
collagen fibrils
noncollagenous proteins
proteoglycans
share ultrastructural features:
well-developed rough endoplasmic reticulum (RER)
prominent Golgi apparatus
numerous mitochondria
secretory granules
ultrastructural features of active odontoblasts:
nucleus
large, up to four nucleoli
located at the basal end, enclosed by a nuclear envelope
cytoplasmic organelles
golgi complex
well developed, in supranuclear region
consists of smooth-walled vesicles and cisternae
rough endoplasmic reticulum (RER)
highly prominent, closely stacked cisternae in parallel arrays
numerous ribosomes → protein synthesis
filamentous material → newly synthesized protein
mitochondria
numerous, evenly distributed throughout cytoplasm
morphologic distinctions
odontoblasts:
tall columnar cells in coronal pulp
leaves behind a process
cell body remains outside, interconnect via canaliculi
osteoblasts and cementoblasts:
polygonal to cuboidal
become osterocytes/cementocytes
cells may become entrapped
secretory products of odontoblasts
mainly type I collagen
small amounts of type V collagen
noncollagenous proteins:
dentin sialoprotein (DSP)
dentin proteoglycans (DPG)
dentin phosphophoryn (DPP)
phosphophoryn
unique to dentin
essential for mineralization
not found in other mesenchymal cells
highly phosphorylated phosphoprotein
enzymes of odontoblast
alkaline phosphatase
acid phosphatase
alkaline phosphatase
closely associated with mineralization
exact role not fully understood
acid phosphatase
a lysosomal enzyme
involved in digestion of resorbed predentin matrix
active odontoblast
numerous organelles
actively producing primary dentin
resting (inactive) odontoblast
fewer organelles
seen after:
completion of root development
tooth eruption
dentin formation shifts from:
primary dentin → secondary dentin
odontoblast process
living extensions of pulpal cells
process extends through the entire thickness of dentin
each dentinal tubule forms around a major odontoblastic process
the process:
occupies most of the tubule space
coordinates formation of peritubular dentin
represents a cytoplasmic extension of the odontoblast cell body
explains why:
dentin is a vital tissue
destruction of dentin affects the pulp
during cavity preparation:
odontoblast processes may be disrupted
leading to pulpal irritation or injury
according to transmission electron microscopy (TEM)
odontoblastic process is limited to inner third of dentin
possibly due to shrinkage artifacts
according to scanning electron microscopy (SEM)
odontoblastic process appears to extend to DEJ
but structures observed may be lamina limitans, not the process itself
according to confocal microscopy findings
in rat molars:
processes do not reach outer dentin or DEJ
except during early tooth development
conclusion:
proteins derived from odontoblasts may remain in tubule walls even after the process retracts
dentin matrix does not remodel, so these antigens persist
cytoskeletal / ultrastructural components of odontoblast
microtubules
microfilaments
functions of microtubules & microfilaments
cytoplasmic extension
structural framework
intracellular transport of materials
microtubules
give rigidity and structural support
extend from the odontoblast cell body
run parallel to the long axis of the process
microfilaments
are thin for movement
present in the main process and lateral branches
occasional mitochondria
found where the process passes through predentin
suggest metabolic activity within the process
lamina limitans
lined the dentinal tubule wall via:
electron-dense limiting membrane
a narrow space separates:
lamina limitans
plasma membrane of the odontoblast process
except where the process is constricted
microtubules contain tubulin
collagen synthesis pathway
rough endoplasmic reticulum (RER)
rapid incorporation of isotope
synthesis of procollagen
golgi apparatus
procollagen packaged and concentrated into secretory vesicles
proteoglycan modification
vesicular transport
vesicles migrate to the base of the odontoblast process
exocytosis
vesicles fuse with plasma membrane
release tropocollagen into predentin
3H-proline
processed in the Golgi
measures new collagen formation
tracing shows collagen is synthesized in the RER
demonstrate protein synthesis and secretion pathways in odontoblasts
transported via secretory vesicles to the odontoblast process base for exocytosis into predentin.
after intraperitoneal injection:
label appears first in odontoblasts
then in predentin matrix
fibrillogenesis
occurs on the outer surface of the odontoblast plasma membrane
forms predentin/dentin matrix, provides structural strength, guides mineralization
process by which collagen molecules assemble into fibrils, which then form fibers
fibrils:
~15 nm diameter near odontoblast process
increase to ~50 nm near calcification front
released into predentin and thicken toward mineralized dentin
tropocollagen
precipitates extracellularly
aggregates into collagen fibrils at the cell surface
fibrils thicken from 15 nm (base) to 50 nm (calcification front)
the basic structural unit of collagen—a triple helix of three polypeptide chains
proteoglycans
ex: chondroitin sulfate
inhibit mineralization
accumulate near the calcification front
may inhibit calcification by binding calcium
synthesized in the RER, modified in the golgi, and secreted into predentin
lysosomal enzymes
used to destroy ingested materials
likely remove proteoglycans before mineralization begins
mineralization begins only after proteoglycans are removed from the predentin matrix
pulp fibroblast
found throughout the pulp
produces and destroys collagen
most abundant cells in the pulp (cell-rich zone)
tissue-specific cells capable of:
maintaining extracellular matrix (ECM)
differentiating into odontoblast-like cells when properly stimulated
function of pulp fibroblast
maintain extracellular matrix
phagocytose and digest collagen → collagen turnover
participate in pulpal repair and inflammation
synthesize:
type I & III collagen
proteoglycans
glycosaminoglycans (GAGs)
immature fibroblasts
polygonal, widely spaced in ground substance
inactive cells which maintain structure and communicate with other cell
organelles:
inconspicuous golgi
sparse RER
many free ribosomes
multiple processes → form gap junctions
enable electrical and chemical signaling
mature fibroblasts
fully functional actively producing proteins and helping build and repair the pulp
characteristics:
appear as active protein-secreting cells
collagen fibrils accumulate along cell surface
proliferated RER, prominent golgi complex
secretory vesicles present, stellate (star-shaped) in shape
fibroblast
stimulated by neuropeptides
with aging:
blood vessels, nerves, and collagen fibers increase
relative number of fibroblasts decreases
many pulpal fibroblasts remain relatively undifferentiated
functionally similar to stem cells
pulp contains many argyrophilic fibers
previously thought to be reticulin
now believed to be collagen fibers with a GAG sheath
non-argyrophilic collagen fibers increase with age
functions of fibroblast
multiply near the injury site
can turn into odontoblast-like cells to help form a dentinal bridge that seals the damage
they produce collagen and other proteins needed to rebuild and support the pulp’s structure
secretes:
Nerve Growth Factor (NGF) → links pulp inflammation and nerve response
Pro-inflammatory cytokines → to guide healing and manage inflammation
NGF:
regulates neuronal development
influences odontoblast response to injury
macrophage
commonly located near blood vessels
involved in signaling pathways within the pulp
identified by antigenic markers in immunohistochemical studies
derived from blood monocytes, digestion occurs via lysosomal enzymes
migrate into pulp tissue and differentiate into various subpopulations
highly active in:
endocytosis
phagocytosis
functions of macrophage
phagocytosis & scavenging
remove:
foreign bodies
dead or damaged cells
extravasated red blood cells
antigen presentation:
process antigens and present them to T lymphocytes
processed antigen binds to:
MHC class II molecules
essential for T cell–dependent immunity
signaling & inflammation:
participate actively in pulpal signaling pathways
released by macrophage:
other cytokines
growth factors (GF)
interleukin 1 (IL1)
tumor necrosis factor (TNF)
dendritic cell
aka: antigen-presenting cells (APCs)
accessory immune cells
equivalent to langerhans cells in epithelium (in the epidermis & mucous membranes)
primarily found in lymphoid tissues but also present in:
connective tissues
dental pulp
in normal pulp:
located mainly in peripheral coronal pulp near predentin
after antigenic challenge:
migrate centrally within the pulp
dendritic cell is characterized by:
possess dendritic cytoplasmic processes
function as professional antigen-presenting cells
express major histocompatibility complex (MHC) class II molecules
function of dendritic cell
play a central role in T cell–dependent immunity
process protein antigens and present:
peptide fragments + MHC class II
recognized by:
T-cell receptors
leads to T-cell activation
lymphocyte
core soldiers of the immune system
works w/ macrophages and dendritic cells
B lymphocytes → rarely found in normal pulp
T lymphocytes → are present in normal human pulp
observed in:
normal pulps
impacted teeth
inflamed pulps
lymphocyte contains:
T lymphocytes
macrophages, dendritic cells
T8 suppressor → the predominant subset
presence of macrophages, dendritic cells, T lymphocytes
indicates that dental pulp is:
immunocompetent tissue
capable of initiating immune responses
mast cell
rare in normal pulp
found near blood vessels
common in chronically inflamed pulp
widely distributed in connective tissues
mast cells contain granules loaded with:
heparin → anticoagulant
histamine → major inflammatory mediator
additional chemical factors involved in inflammation
functions of mast cells
chronic pulpitis
vascular changes
inflammatory reactions