L21 - Airflow through Tubes AND Expiratory Flow Limitations AND Flow-Volume Loops
1/56
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
57 Terms
Airflow through tubes
Pressure falls with distance as flow proceeds through a tube
Due to frictional forces, which are caused by the resistance to the flow.
The greater the resistance to the flow, the greater the fall in pressure for any given flow
Airflow through tubes
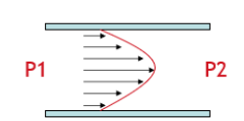
Flow profile of Laminar flow
Parabolic flow profile → molecules move faster in the middle and slowest at the edges as this is where frictional forces are largest
Airflow through tubes
Flow profile of Turbulent flow
Linear flow profile
Airflow through tubes
The amount pressure falls with distance depends on…
the profile of the flow itself
Airflow through tubes
Two extremes of flow patterns
laminar flow
turbulent flow
Airflow through tubes
Sustaining flow of laminar vs turbulent flow
Different flow profiles require different amounts of energy in order to sustain flow
Laminar flow: Δ Pressure ∝ flow
Turbulent flow: Δ Pressure ∝ flow2
A greater pressure difference (and therefore more energy) is required to sustain a turbulent flow rather than a laminar flow:
Laminar flow: If I want to double the flow, I would just have to double the pressure difference
Turbulent flow: If I want to double the flow I would need a 4x increase in pressure difference.
Airflow through tubes
What determines flow pattern (laminar or turbulent)
Reynolds number
Larger Reynolds Number= more likely to have turbulence.
Increasing radius and/or increasing velocity increases turbulence.
Air we breathe will have a constant viscosity and density, so ignore those terms.

Airflow through tubes
Use Reynolds number to show type of flow in resting breathing
Large number = more turbulent
Flow transitions from laminar air flow in the small airways towards turbulent flow in the larger airways
This is because the radius of the airways and speed of gas both increases.
There is always a pressure drop from the alveolus to mouth, this drop is greatest in the larger airways in order to maintain a constant turbulent airflow).

Airflow through tubes
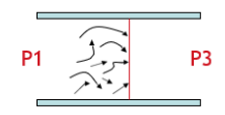
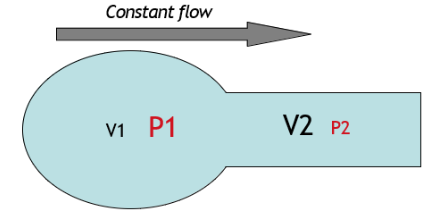
What does Bernoulli’s Principle State
If we have flow going through a tube, at the point where the tube narrows the velocity must increase in order to maintain a constant flow
Bernoulli’s Principle: When velocity of a fluid increases, there must be a fall in pressure
Airflow through tubes
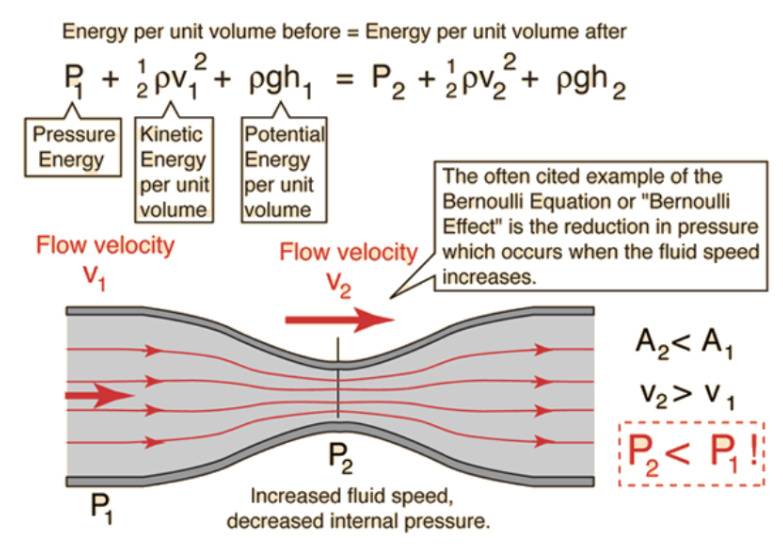
Bernoulli’s principle + lift in aeroplanes
Aeroplane wings have a specific shape that generate a greater path length on the surface than underneath.
Because airflow is moving at a fixed flow, air molecules will have to go faster on top of wing the wing than below.
Therefore, according to Bernoulli’s principle, pressure underneath the wing must be greater than pressure above the wing if flow is constant
This then generates the lift.
Airflow through tubes
Bernoulli’s Principle and Lungs
Flow of gas (V̇) = u (speed, cm/sec) x A (area, cm2)
Therefore, if flow is constant then the velocity (V) must increase as total surface area falls.
Smaller air ways have largest total surface area so the velocity of air increases from the lower airways to the upper airways.
Using Bernoulli’s principle → by air speeding up as it moves through the airways during expiration (alveolus to trachea) there is a further fall in pressure.
P1 greater than P2 anyway during expiration but Bernoulli's principle is adding to that.
The greater we want to accelerate air through airways, on expiration, the greater the fall in pressure must be
Airflow through tubes
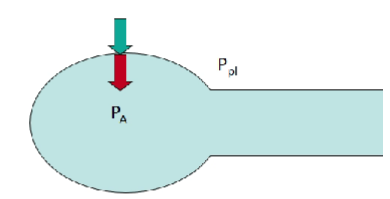
Pressure falls as air progresses from the alveoli, up the airways, and out the mouth.
Why (3)
Pressure is lost as the resistance of airways is overcome (energy lost as heat)
Velocity increases and radius increases as you move up the airways
Reynolds number increases
So turbulence increases, causing an even greater fall in pressure.
Decreasing total cross sectional area
Velocity of gas must increase
Get an additional fall in pressure (Bernoulli effect)
Expiratory flow limitations
When can intrapleural pressure be positive
intrapleural pressure = Ppl
When you breathe out maximally
Expiratory flow limitations
What is peak flow determined by
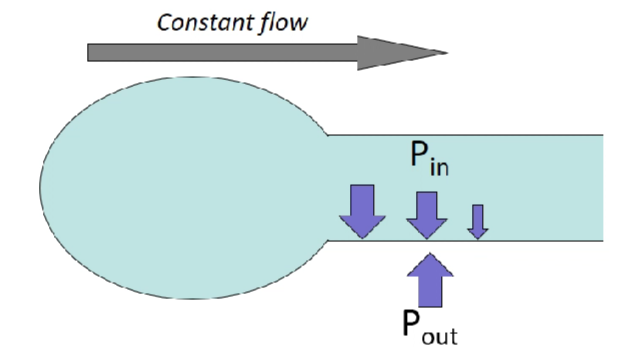
Pressure inside the airways falls as air moves through them
Therefore, there may come a point where intrapleural pressure becomes greater than the pressure inside the airways at a certain point.
At this point the airways will collapse (unless it is supported by a tracheal ring) which will restrict airflow.
So your peak flow is determined by the point where airways collapse.
Expiratory flow limitations
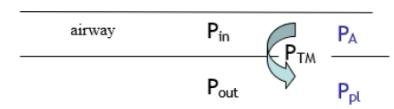
What is transmural pressure
Transmural pressure (PTM) = PA – Ppl
A positive PTM indicates a distending pressure (Pin>Pout), it holds the airway open
Expiratory flow limitations
What determines Ppl
Recoil of the chest wall and the lung pulling away from each other
Or in a maximal expiration where the chest wall is pushing down to make pleural pressure positive
Expiratory flow limitations
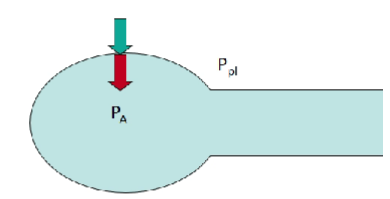
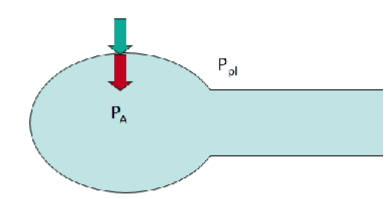
What determines PA
Pleural pressure (green)
Elastic recoil pressure of the lung (Pel) (red)
Therefore PA = Pel + Ppl
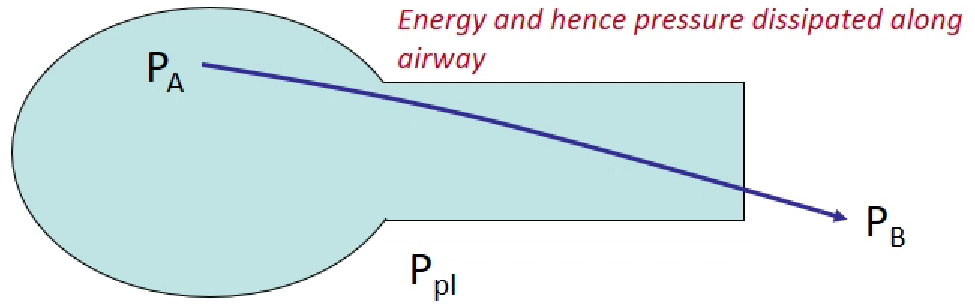
Expiratory flow limitations
Combination of PTM and PA equations
PA = Pel + Ppl
Therefore, by substitution:
PTM = PA - Ppl
PTM = (Pel + Ppl) – Ppl
PTM = Pel
Under static conditions the transmural pressure is the elastic recoil pressure.
Expiratory flow limitations
Loss of elasticity and transmural pressure
PTM = Pel
If elasticity is lost (emphysema) you will able to generate a lower PA → greater tendency for the airways to collapse
Expiratory flow limitations
At FRC PA = 0.
Therefore: PTM = 0 - Ppl (e.g. if Ppl = -0.5kPa, PTM = 0 - -5 = +0.5kPa)
Greater PTM indicates a greater more negative Ppl which indicates a greater lung volume → indicates a greater elastic recoil → indicates a greater distending pressure
More intrapleural pressure when pulling the lungs away from where they want to be and is retracting
This retraction back to its equilibrium volume is generating a greater elastic recoil → greater distending pressure
Larger lung volume creates a greater flow
Expiratory flow limitations
Ppl at forced expiration
PTM is +ve in quiet breathing as Ppl is always negative (PTM = PA - Ppl) so there is always a distending pressure throughout a breath when breathing quietly so airways are held open.
However: during eg exercise, expiratory muscles become active (crush down volume) and Ppl can become +ve. (likely to be in large airways as pressure falls greatest in larger airways)
If Ppl can become +ve and > PA, then small airways (which lack smooth muscle or cartilage) may collapse and limit airflow during expiration
This is determined, in part, by ΔP along the airway during expiration.
Expiratory flow limitations
What determines whether an airway collapses?
Difference between PA and Ppl.
Remember:
PA = Pel+ Ppl
PA - Ppl = Pel
So, elastic recoil of the lung is a major determinant of PTM so determines whether airways collapse during expiration
Flow limitation (determined by height, age and sex)
Expiratory flow limitations
Can you train yourself to have a higher peak flow
Elastic recoil is a major determinant of PTM
Elastic recoil determines peak flow (thus airway collapse)
You can’t train yourself to have a higher peak flow
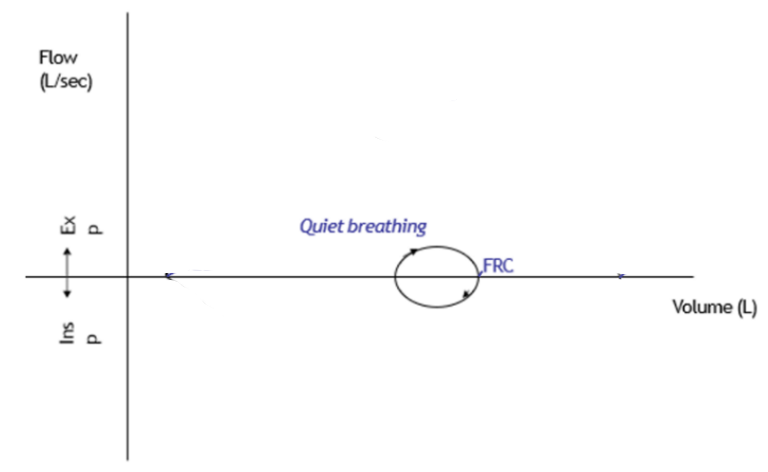
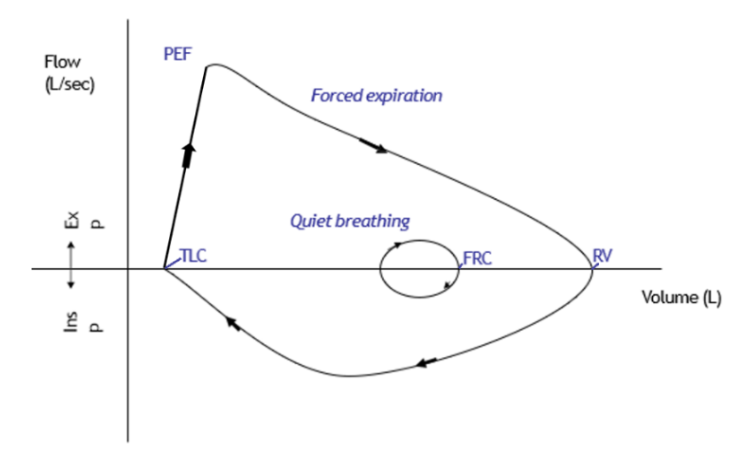
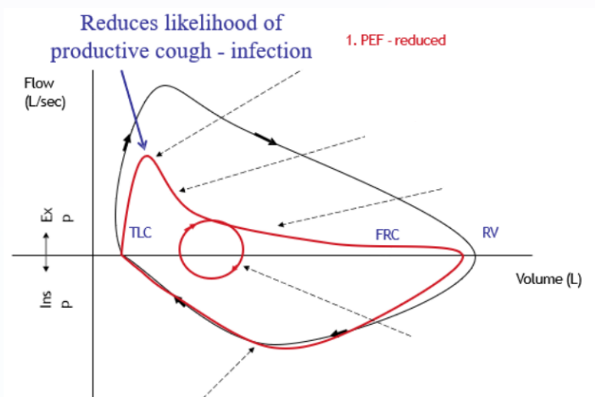
Flow Volume Loop
What is on the x and y axis
explain what does the +ve and -ve y axis mean
Y axis: Flow (L/sec)
-ve Y axis: inspiratory flow rate
+ve Y axis: expiratory flow rate
X axis: Lung volumes: TLC → FRC → RV
At both Residual volume and TLC, flow = 0
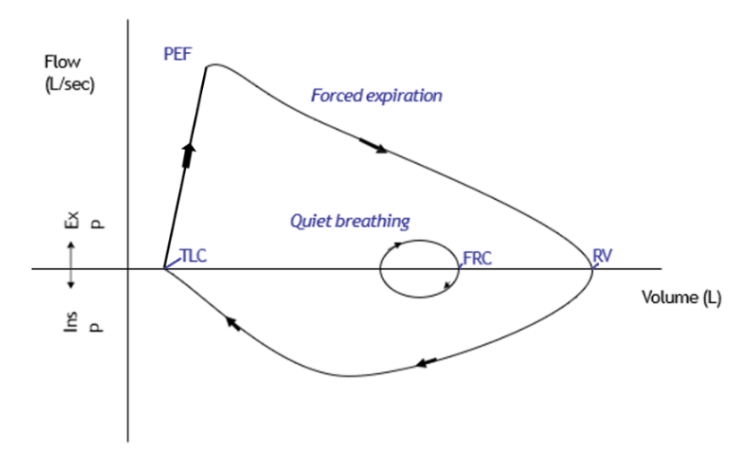
Flow Volume Loop
in Quiet breathing
Small change in volume
Horizontal diameter of small circle = Tidal Volume
In quiet breathing both inspiratory flow rate expiratory flow is ~equal → get circle.
Flow Volume Loop
PEF to RV
What is the Maximum Envelope
Occurs during forced expiration from TLC to RV.
Horizontal diameter of peak expiratory flow loop is vital capacity.
Maximum envelope
Deep breath in + exhale → cannot increase flow from the maximum envelope (line which goes from PEF to RV during forced expiration)
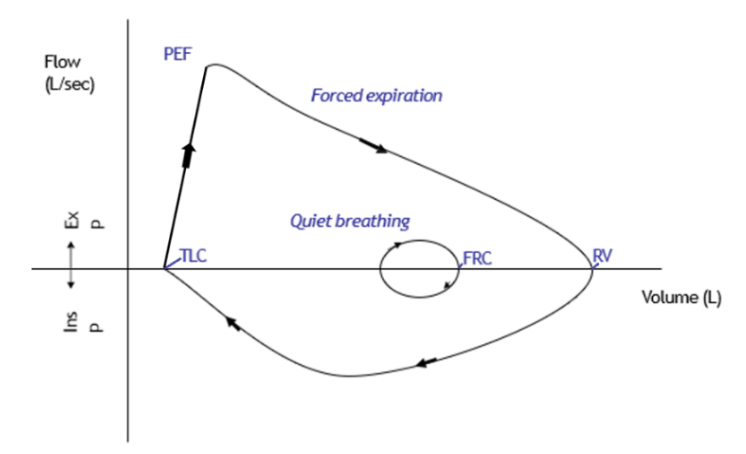
Flow Volume Loop
PEF is much greater/less than PIF
PIF occurs…….
PEF occurs……..
Expiratory flow decline is normally linear/exponential/plateaus
PEF is much greater than PIF
PIF occurs mid-inspiration
PEF occurs close to TLC
Expiratory flow decline is normally linear
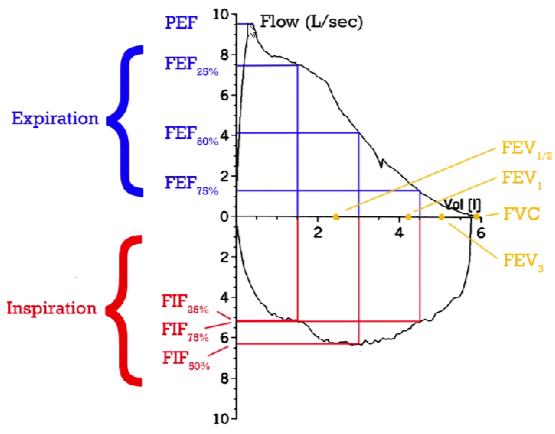
Flow Volume Loop
FEF - Fractional Expiratory Flow
FIF - Fractional Inspiratory Flow
FEF and FIF gives information of flow in smaller airways
Respiratory disease often progress from smaller airways
If someone presents with a reduced PEF → often a progressed disorder
PEF measures flow at larger airways
Why is Maximum Expiratory flow near TLC? (4 factors)
Elastic recoil
Surface tension
Pleural pressure
Lung volume
These create a greater transmural pressure, less chance of developing a choke point which would reduce peak expiratory flow.
Why is Maximum Expiratory flow near TLC?
Role of Elastic recoil
Elastic recoil is determined by intrinsic properties of the lung and by the lung volume → the greater the lung volume, the greater the elastic recoil pressure.
The greater the elastic recoil pressure the greater the PA that can be generated (PA = Pel + Ppl), and therefore the greater the difference between PA and Ppl.
So at TLC (the largest lung volume) there is the largest elastic recoil so on expiration you can produce the largest PA and so the greatest difference between PA and Ppl
Why is Maximum Expiratory flow near TLC?
Surface tension
Surface tension → contributes to elastic recoil.
Surfactant reduces surface tension forces.
At TLC, the surfactant molecules are the most spread out, so surfactant is least effect, so the surface tension forces are greatest and then so is the elastic recoil of the lung → so the greatest PA can be generated at TLC, with the greatest difference between PA and Ppl
Why is Maximum Expiratory flow near TLC?
Pleural pressure
Most +ve on expiration from TLC
The chest wall is maximally above its equilibrium volume at TLC (NOT at FRC) and so it has its greatest collapsing tendency → so the greatest PA can be generated at TLC with the greatest difference between PA and Ppl
Expiratory muscles are at maximum tension development length
Why is Maximum Expiratory flow near TLC?
Lung volume
Greater lung volume results in a greater elastic recoil which induces greater tethering to the chest wall.
Greater tethering forces means a greater diameter of the airways and so there is a lower resistance.
Therefore, resistance is at its least at TLC → greatest flow can be generated.
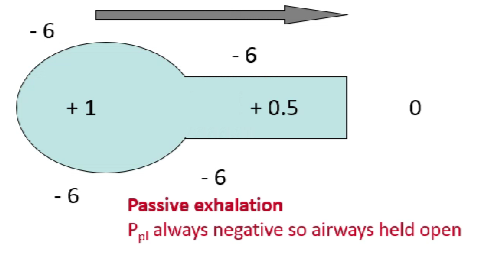
Airways being held open
In normal passive expiration
You always have a -ve intrapleural pressure.
During expiration we generate a slightly positive PA
Because of recoil compared to barometric pressure
Then get a fall in pressure as we move through the airways towards the mouth
But because Ppl is –ve the airways will always be held open.
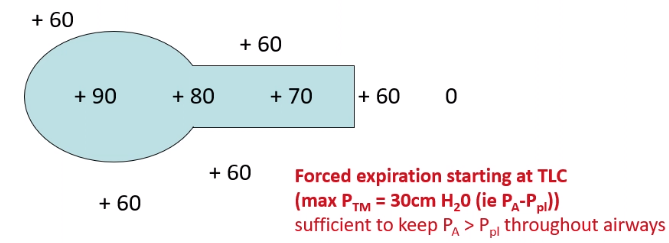
Airways being held open
In forced expiration starting at TLC
We take a maximum deep breath in and then force air out.
This generates a high +ve intrapleural
As chest wall is collapsing strongly with expiratory muscle activity
Have a larger elastic recoil pressure
These will generate a high PA (PA = Ppl + Pel) e.g. 90
Therefore, because you have generated a large elastic recoil pressure, max Transmural pressure will be high → 30cm H2O (PA-Ppl)
As we breathe out the pressure in the airways will fall but will stay greater than Ppl until we reach the trachea (where may be lower) so the airways are held open.
Airways being held open
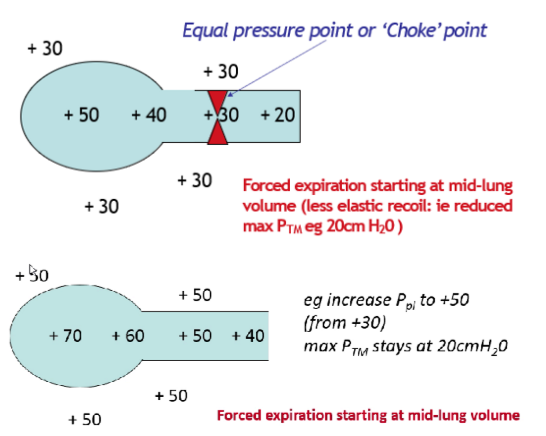
In forced expiration starting at mid-lung volume
4 factors are not working together to create a large PTM
Lower elastic recoil and generates a lower +ve intrapleural pressure e.g., 30 cm H2O
Generates a lower PA (PA = Pel+ Ppl)
Therefore max Transmural pressure is lower (PTM = Pel) = 20 cm H2O
Results in intrapleural pressure equalling airway pressure at some point in the smaller air ways (no cartilage) = choke point
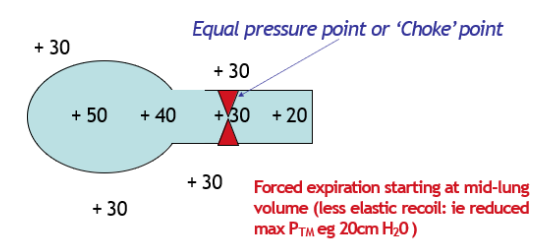
Choke point
Intrapleural pressure equalling airway pressure at some point in the smaller air ways (no cartilage)
Equal pressure point (EPP) develops in smaller, peripheral airways if expiration has begun between TLC and FRC
Continue to breathe out (forced expiration)
Airway pressure behind choke point builds up and so the choke is relieved.
But as choke is relieved the airway pressure falls again and choke re-develops. (presented as wheezing)
This limits your flow.
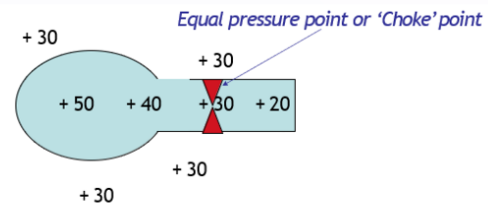
Can you ‘train’ expiratory muscles to create a greater force and hence greater PA - and hence greater flows at volumes less than TLC?
No! Trying to exhale more forcibly raises Ppl, which raises PA by the same amount (PA = Pel +Ppl) and so the max transmural pressure remains the same (20cm water) – so you still get choke point.
Whether a choke point occurs (which limits flow) is determined by the size of transmural pressure.
You can not change your elastic recoil pressure so you can not change your flow rates for a set lung volume.
Lungs cannot be trained to create a greater pressure as it is made up of smooth muscle (not skeletal muscle)
Airways being held open
Forced Expiration in Emphysema
Patients with emphysema, have a reduced elastic recoil as lung tissue is damaged.
Lose the ability to generate a high PA.
Max transmural pressure is lower e.g. 10cmH2O
Therefore, it is more likely they will get choke point forming in more peripheral (lower) airways limits ability to generate a high flow.
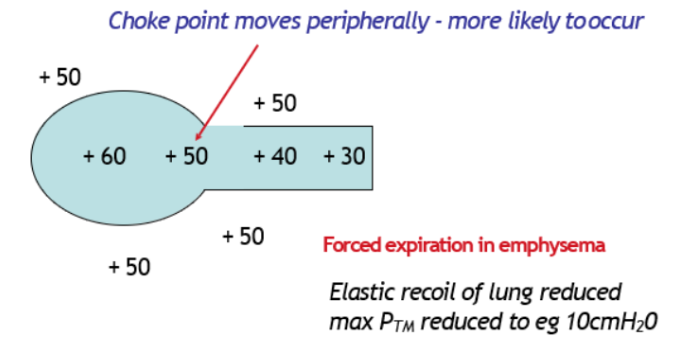
elastic recoil and cross sectional area
Major determinant of small airways cross sectional area and thus airway resistance
Effect of tethering force
Greater lung volume = greater elastic recoil = greater tethering to the chest wall
Lung volume is a major determinant of small airway (without smooth muscle) cross sectional diameter
Greater tethering forces means smaller airways are held open more → greater total cross-sectional area → ↓ resistance.
What determines the tethering effect
Integrity / elasticity of the lung tissue
Weak tethering effect
Consequence
Weakened in e.g. emphysema
Therefore, emphysema patients have a lower total cross-sectional area of their smaller airways
Higher airway resistance → increases the rate of fall in PA during forced expiration
Further decreases the maximal expiratory flow rate
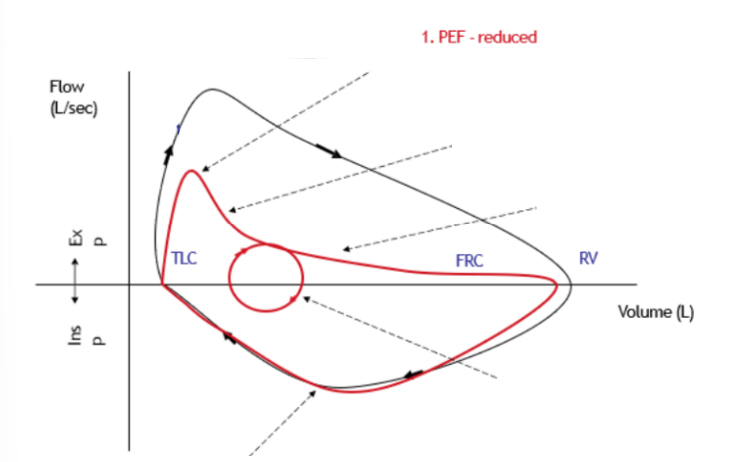
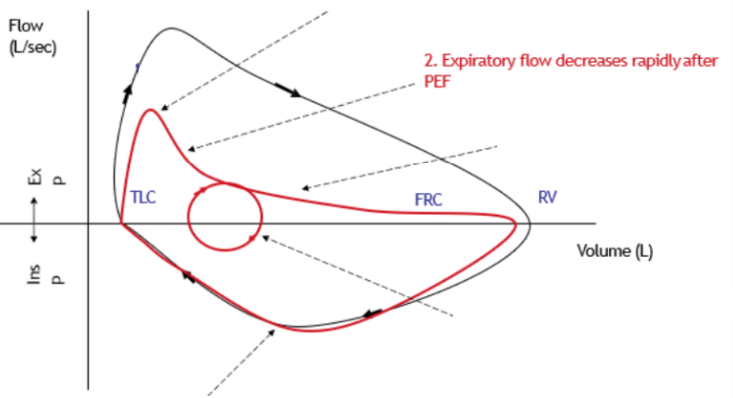
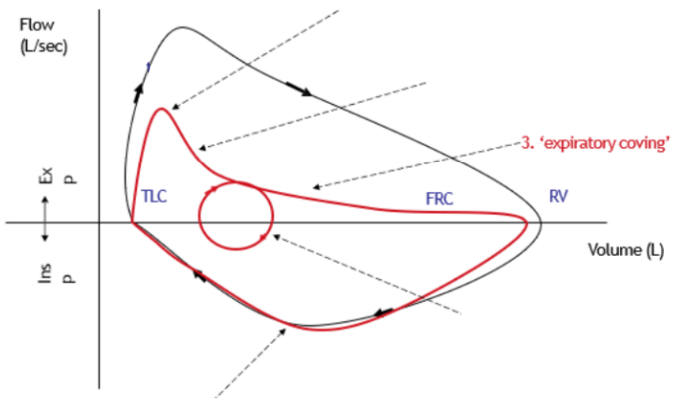
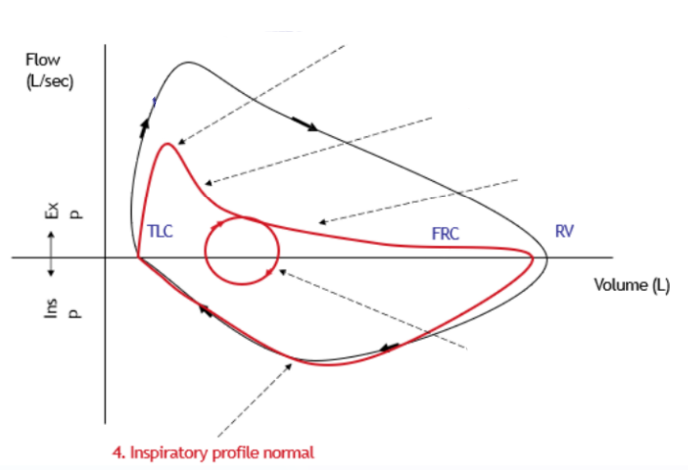
Differences/Similarities in Flow volume loop in Emphysema compared to normal (5)
Reduced PEF
Expiratory flow decreases rapidly after PEF
‘Expiratory Coving‘
Normal inspiratory profile
Tidal breathing moved to higher lung volume
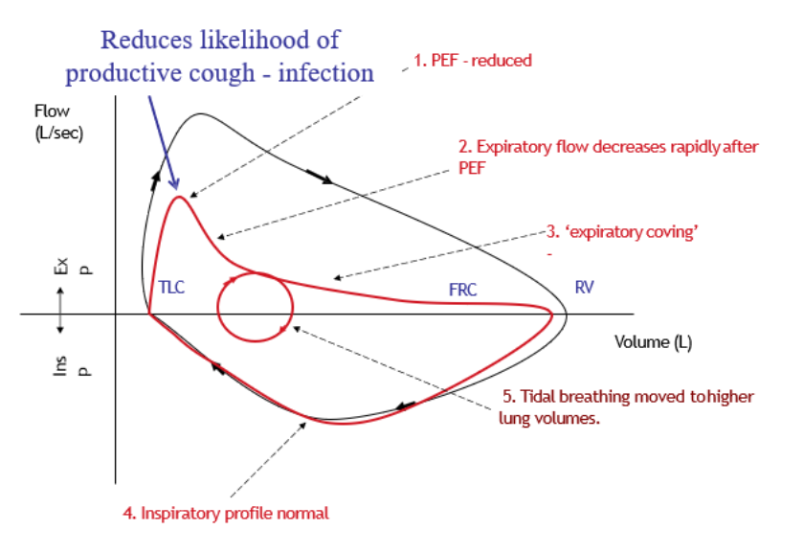
Differences/Similarities in Flow/volume loop in Emphysema compared to normal
PEF
Reduced:
Elastic recoil reduced → greater tendency for airways to collapse as reduced peak alveolar pressure
Results in a reduced driving pressure during expiration → reduced PEF
Differences/Similarities in Flow/volume loop in Emphysema compared to normal
Expiratory flow after PEF
Expiratory flow decreases rapidly after PEF
Due to narrowing of airways (loss of tethering force so can’t get same flow due to higher resistance)
Differences/Similarities in Flow/volume loop in Emphysema compared to normal
‘Expiratory coving‘
Indicative of emphysema
PEF to RV is no longer a linear line
Differences/Similarities in Flow/volume loop in Emphysema compared to normal
Inspiratory profile
Normal
Ppl is always negative so PTM is always +ve during inspiration so loss of elastic recoil has no effect
No issue with airway collapse during inspiration
Differences/Similarities in Flow/volume loop in Emphysema compared to normal
Tidal breathing
Moved to higher lung volumes.
Every breath flow limited. Patient may develop pursed lip breathing and wheezing
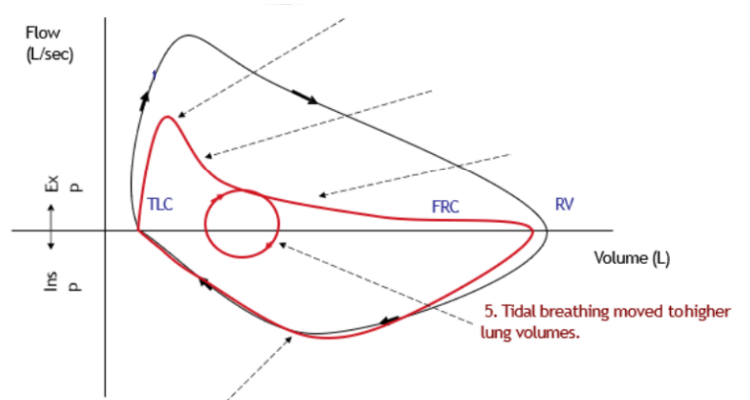
Differences/Similarities in Flow/volume loop in Emphysema compared to normal
Tidal breathing moved to higher lung volumes
Presentations (3)
Barrel chest
Pursed lip breathing
Wheezing
Differences/Similarities in Flow/volume loop in Emphysema compared to normal
Tidal breathing moved to higher lung volumes
Barrel chest
Loss of lung elasticity so is pulled up towards equilibrium volume of the chest wall
Differences/Similarities in Flow/volume loop in Emphysema compared to normal
Tidal breathing moved to higher lung volumes
Pursed lip breathing
Retains upper airways by splinting the airway open
Instead of air pressure falling rapidly, it retains airway pressure
Differences/Similarities in Flow/volume loop in Emphysema compared to normal
Tidal breathing moved to higher lung volumes
Wheezing
Due to opening and closing of choke point
Emphysema
Productive cough
Cough = maximal expiration against the closed glottis (space between vocal cords), squeeze and then an explosive airway flow to expel mucus
Patients with emphysema have a reduced likelihood of producing a productive cough due to their low peak expiratory flow rate.
So mucus is not removed from the airways and so infection occurs is highly likely
Flow volume loop in restrictive disease
less lung volume
the maximum flow rate is reduced, as is the total volume expired.
The flow is abnormally high in the latter part of expiration because of increased recoil.

Flow volume loop in obstructive disease
Flow rate is very low in relation to lung volume
Scooped-out appearance is often seen following the point of maximal flow
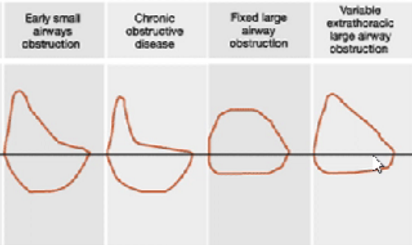
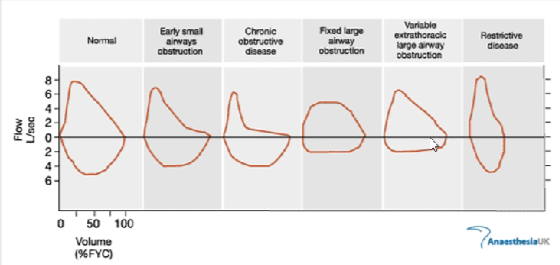
Flow volume loops provide a graphical illustration of a patient's spirometry efforts.