Week 2 Anatomy study
1/69
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
70 Terms
Vital signs
determines when this self-regulation is out of balance.
The five vital signs are:
temperature (T),
pulse (heart rate [HR]),
blood pressure (BP),
respiratory rate (RR),
saturation of peripheral oxygen (SpO2).
Vital signs are interrelated; for example, an increase in respiratory rate often correlates with an increase in heart rate, while a decrease in oxygen saturation (if not corrected) may overtime, correspond with a decrease in blood pressure
Vital signs have established normal and abnormal ranges, but variations occur. Besides an individual’s personal baseline, vital sign parameters can also vary across the life span and change as a person gets older. What is considered normal for an infant or a toddler can be abnormal or problematic in an adult, and vice versa.
Homeostasis
The process of self-regulation that bodies maintain through multiple, interdependent physiological processes is called homeostasis.
Age-Related Variations
As people grow older, the risk for hypertension increases. Environmental and lifestyle influences such as smoking, drinking, and dietary choices have direct effects on the cardiovascular system.
Heart rate is inversely proportional to age.
Rates are faster at a younger age and get progressively slower as we get older.
A resting heart rate of 120 bpm in a newborn is acceptable but problematic in an adolescent or adult.
tachycardia, bradycardia, arrhythmia
When to Assess Vital Signs
Acute care facilities usually assess vital signs every four to eight hours, while critical care units may assess them every hour or more frequently.
Ambulatory facilities usually measure vital signs at the start of a patient visit.
The registered nurse is ultimately responsible for taking action should there be any issues.
Temperature
Normal body temperature fluctuates within the range of 36.5°C to 37.5°C. Fluctuations occur due to circadian rhythm, metabolism, and hormones.
Circadian rhythm: changes in body temperature naturally drop between the hours of 3 and 5 a.m. and again between 1 and 4 p.m.
Times of high metabolic activity (including exercise and infection) increase temperature because of the increase in chemical reactions producing heat within the body.
Fluctuations of the thyroid hormone affect metabolic activity as well, meaning that an increase in thyroid hormone will increase the temperature.
While the range of normal temperatures generally stays the same throughout the life span, it does become harder for the body to regulate temperature as it ages.
Loss (or gain) of body fat and hormonal changes can affect how comfortably warm or cool the body may feel, resulting in the need to adjust clothing layers or environmental temperature when possible.
Factors that affect temperature
Age:
Studies have shown that older adults tend to have lower baseline body temperatures. Newborns (smaller body size, higher surface area to body weight ratio, less subcutaneous fat)-immature thermoregulatory mechanisms.
Environment:
Changes in the environment can affect a patient’s temperature, especially if they are older and cannot thermoregulate as well anymore due to reduced muscle mass and body fat.
Hormones:
(Thyroid stimulating hormone [TSH], cortisol, insulin etc.). Recent research has shown that the hormonal changes that accompany menopause can cause a reduction of core body temperature.
The decreased levels of estrogen in the body cause the hypothalamus to become more sensitive to minor changes in body temperature.
When the hypothalamus “thinks” the body is too warm, it sends messages to thermoregulate, which is why menopausal women often shiver after a hot flash.
Thermoregulation
body’s ability to maintain temperature within normal ranges the hypothalamus is responsible for this and is an endogenous OR internal (originates from within the body), mechanism of heat regulation.
Normothermia
when core body temperature is normal —> 36.5°C to 37.5°
Hyperthermia
when core body temperature is more than 105.8°F (41°C). (via external factors exogenous)
Hypothermia
when core body temperature is less than 95°F (35°C). (via external factors exogenous)
Pyrexia (Fever)
A body temperature greater than 100.4°F (38°C)
Febrile
what it means to be a patient with a fever. *These conditions are a result of endogenous factors Some hospitals have policies in place whereby if a patient has a fever >38.5 C, standing orders exist to have blood cultures drawn (high temp may be an early indicator of a larger impending issue such as bacteremia or blood infection, which can lead to sepsis, a life- threatening medical condition)
Afebril
when the patient’s body temperature returns to normal after a fever or is without fever. *These conditions are a result of endogenous factors Some hospitals have policies in place whereby if a patient has a fever >38.5 C, standing orders exist to have blood cultures drawn (high temp may be an early indicator of a larger impending issue such as bacteremia or blood infection, which can lead to sepsis, a life- threatening medical condition)
Evaporation (The 4 Mechanisms of Heat Transfer)
the transfer of heat through dissipation of sweat from the skin, thus cooling the body
Radiation (The 4 Mechanisms of Heat Transfer)
the process by which the body loses heat to cooler objects/surroundings and gains heat from warmer objects/surroundings through infrared waves (infrared radiation). Main way the body loses heat when it's warmer than its surroundings.
Example: walking outside during the winter without a coat, heating a room with a fireplace.
Convection (The 4 Mechanisms of Heat Transfer)
heat transfer through movement of air/liquids/gases across the skin, such as when entering a room with air-conditioning or using a fan, the body cools. Amount of heat loss from convection is dependent upon airflow.
Conduction (The 4 Mechanisms of Heat Transfer)
When skin encounters a warmer or cooler object (such as an ice pack, holding a hot cup of coffee), temperature changes.
Pulse
A pulse is the palpable way to assess each time the heart beats. Pulse refers to the pressure wave that expands and recoils arteries when the left ventricle contracts.
A normal pulse has a regular rhythm.
Pulse force ranges from absent to bounding.
Pulse equality compares pulses on both sides of the body.
Carotid pulses should never be palpated at the same time.
heart rate is the number of times the heart beats in one minute; these two terms are often used interchangeably. Measuring a patient’s pulse is an accurate and rapid method of assessing their heart rate.
Physiology of the Pulse
Pulse refers to the pressure wave that expands and recoils arteries when the left ventricle of the heart contracts. It is palpated at many points throughout the body.
The most common locations to assess pulses as part of vital sign measurement include radial, brachial, carotid, and apical areas.
A patient’s pulse is most readily measured at the radial artery but can be measured at any of the pulse points shown.
In a patient who has had coronary artery bypass grafting and has had their radial artery harvested for the procedure, the radial pulse may be reduced or not palpable at all. Always check for surgical scars!
Pulse Characteristics
Rhythm: is it regular or irregular?
Rate: how fast is it?
Equality: A comparison of the pulse forces on both sides of the body.
Force: strength of the pulsation felt on palpation, can range from absent to bounding.
Pulse force chart
Pulse force is documented using a four-point scale:
3+: full, bounding
2+: normal/strong
1+: weak, diminished, thready
0: absent/nonpalpable
Respiratory Status
The action of breathing is termed respiration. Respiration → Gas exchange
There are two types of respiration: external and internal.
12-20 RPM is normal
Internal respiration
The exchange of oxygen for carbon dioxide that occurs within the cells.
→ Gas exchange between the blood and the tissues
External respiration
The act of breathing in oxygen (O2) and breathing out carbon dioxide (CO2). → Gas exchange between the air in the lung and the blood
Inspiration
The thoracic cavity expands
External intercostal muscles contract
Diaphragm contracts
(inhaling/breathing in) The diaphragm moves down as the lungs expand and fill with air, bringing oxygen into the body. This expansion increases the volume of space and air in the chest and enables air to flow inward. (pressure also a factor here)
Expiration
The thoracic cavity reduces
External intercostal muscles relax
Diaphragm relaxes
(exhaling/breathing out), the lungs naturally recoil as the air is expelled from the lungs, and the diaphragm moves back to its original position.
A complete respiratory cycle of one sequence of inspiration and expiration is considered one breath while measuring a patient’s respiratory rate.
Respiratory Characteristics
Quality
Rhythm
Rate of respirations
Factors Affecting Respiratory Status
The quality of the respiration can be affected by:
acid-base imbalances
Example: elevated CO2 levels in respiratory acidosis, the body responds by increasing RR to help "blow off" excess CO2, increasing pH)
low oxygen levels: need for an increase in O2 done so by increasing RR
carbon dioxide levels
damage to any component of the respiratory system § Trauma, tumor
Infection
Stroke
More factors include
Age
Activity level
Disease status
Environment
Lifestyle
Emotions
Oxygen Saturation
Oxygen saturation (SpO2) is the measure of arterial oxyhemoglobin saturation.
A range of 95 to 100 percent is considered normal. Values less than 95 percent are abnormal and indicate inadequate oxygenation.
Oxygen saturation is measured using a pulse oximeter.
Oxygen desaturation is considered a late sign of respiratory compromise.
Factors Affecting Oxygen Saturation
Oxygenation is affected by many factors that are interconnected with other vital signs; thus, anything that affects one of the other vital signs can also affect oxygen saturation.
Lung diseases such as COPD and asthma will affect oxygen saturation; pain and anxiety can affect it as well. If heart rate or respirations are abnormal, oxygen saturation may be affected as well.
False low readings can be caused by:
Cold limbs
Poor circulation from peripheral vascular disease
Certain blood disorders, such as sickle cell disease
Incorrectly placed oxygen probe
Fingernail polish on the finger being used
Older adults cannot adjust to temperature changes as quickly as younger people
Blood Pressure
Blood pressure is the pressure of blood pushing against the walls of the arteries and is essential for maintaining perfusion.
A person needs a certain level of blood pressure to maintain adequate blood flow (perfusion), to their organs to stay alive.
A person’s blood pressure must be enough to maintain perfusion to oxygenate and nourish the brain, the kidneys, the liver, the intestines, along with all other areas.
A lack of perfusion results in a lack of oxygen
Systolic
pressure reflects ventricular contraction. (typically around 120 mmHg) The higher value and reflects the arterial pressure resulting from the ejection of blood during ventricular contraction, or systole.
Diastolic
pressure reflects ventricular relaxation. the lower value (usually about 80 mmHg) represents the arterial pressure of blood during ventricular relaxation, or diastole.
Because of the physiology of the heart, the systolic pressure will never be lower than the diastolic pressure.
Factors Affecting Blood Pressure
Emotional states
Disease states
Social and dietary habits
Medications
Pulse pressure
is the difference between systolic and diastolic pressure.
A low or narrow pulse pressure may occur in patients with low stroke volume, which may be seen in congestive heart failure, severe stenosis of the aortic valve, or significant blood loss following trauma.
In contrast, a high or wide pulse pressure is common in healthy people following strenuous exercise, when their resting pulse pressure of 30 to 40 mm Hg may increase temporarily to 100 mm Hg as stroke volume increases.
A persistently high pulse pressure at or above 100 mm Hg may indicate excessive resistance in the arteries and can be caused by a variety of disorders (atherosclerosis, hypertension).
Chronic high resting pulse pressures can degrade the heart, brain, and kidneys and warrant medical treatment.
Mean arterial pressure
normally ranges from 70 to 110 mm Hg.
The mean arterial pressure (MAP) represents the “average” pressure of blood in the arteries, that is, the average force driving blood into vessels that serve the tissues.
Calculating MAP (IMPORTANT)
MAP = diastolic BP + (systolic-diastolic BP)/3
Example : Diastolic = 90mmHg, Systolic = 120mmHg
MAP = 90 + (120 - 90) / 3
= 90 + (30)/3
= 90 + 10
= 100
Ischemia
insufficient blood flow, Is when MAP (mean arterial pressure) is below 60 mm Hg. Hypoxia usually accompanies this ischemia.
Hypoxia
low levels of oxygen in your body tissues. It causes symptoms like confusion, restlessness, difficulty breathing, rapid heart rate, and bluish skin.
Hypoxemia
Refers to low levels of oxygen in systemic arterial blood. Neurons are especially sensitive to hypoxia and may die or be damaged if blood flow and oxygen supplies are not quickly restored.
Physiology of Sleep
basic neurological function controlled by the brain stem.
During sleep, the brain stores new information, converts short-term memories into long-term memories, and removes waste through the glymphatic system.
This system clears substances like potassium, lactic acid, beta amyloid, and tau proteins, which are linked to Alzheimer disease.
Adequate sleep supports learning, memory, immune function, insulin use, heart health, and emotional regulation.
Lack of sleep interferes with coping and can lead to unhealthy behaviors such as substance use.
Sleep needs change with age, from 16–18 hours in newborns to about 7–9 hours in adults.
Sleep is regulated by both homeostasis (the body’s need for rest) and circadian rhythm (the body’s response to light and dark).
Melatonin increases in darkness to promote sleep and decreases during daylight.
Brain Activity During Sleep
Although consciousness is reduced during sleep, the brain remains active. As sleep begins, the hypothalamus suppresses arousal systems. Brain regions gradually disengage, and sleep stages can be identified using an EEG.
Two main types of sleep
NREM sleep (Stages I–III)
REM sleep
Each stage has distinct brain wave patterns.
Reticular Activating System (RAS)
The RAS is located in the brain stem and controls consciousness, alertness, and the sleep–wake cycle.
It helps regulate sleep rhythms and muscle tone, especially the muscle paralysis seen during REM sleep.
The RAS is also involved in pain responses and disorders such as Parkinson disease, PTSD, schizophrenia, and narcolepsy.
Circadian Rhythms
Circadian rhythms control sleep timing, wakefulness, metabolism, and body temperature.
These rhythms are regulated by the hypothalamus and respond to light signals from the eyes.
Normally, people feel sleepy a few hours after dark and wake near sunrise.
Wakefulness, metabolism, temperature, and the timing of sleepiness and subsequent sleep, are part of circadian rhythms, which likely originated historically from humans as hunters and gatherers.
These early peoples, by necessity, would use the improved visibility during daylight hours for most hunting, searching for other food sources, and other activities.
Their own safety was also of paramount importance, and therefore it was also valuable to be able to see potential dangers.
The control of circadian rhythms initiate within the hypothalamus, where there are centers for sleep and wakefulness.
These are set to respond to light and darkness through messages from the retinas. The results include feeling sleepy, physiologically welcoming the onset of sleep two or three hours after dark, and naturally awakening shortly before, or at sunrise.
In evening, Serotonin (neurotransmitter), is released by raphe nuclei of brainstem. It is a precursor to melatonin. Melatonin (hormone) released by pineal gland. Reduced levels of serotonin are related to insomnia and sleep disturbances.
The circadian rhythm includes the influences of light and dark on organ systems during related periods of day and night.
Hormones influenced by circadian rhythm include
Melatonin (promotes sleep)
Cortisol (helps with morning wakefulness)
Adenosine (builds sleep pressure)
ACTH, prolactin, and norepinephrine
Shift work can disrupt circadian rhythms, leading to long-term sleep difficulties.
Tachycardia
fast heart rate
Bradycardia
slow heart rate
Arrhythmia
abnormal heart rhythm
Physiology of sleep
Sleep, like respiration, is a basic physiological function, under neurological control and originating in the brain stem.
There are a variety of processes that occur while sleeping, including storing and cataloguing new information, and changing short-term memories into long-term memories. Certain areas of the brain, such as the amygdala and hippocampus relate to emotional regulation, are more active during sleep.
The glymphatic system is involved in regulation of interstitial fluid movement and subsequent removal of waste from the brain and cerebrospinal fluid (CSF) and is directed by sleep and circadian cycles.
Potassium and lactic acid are two of the waste products removed by processes of the glymphatic system.
A peptide implicated in development of Alzheimer disease, called beta amyloid, and tau, a protein also associated with Alzheimer disease development, are other wastes eliminated by the glymphatic system.
Sleep Coordination
Sleep involves coordination of the properties of homeostasis and circadian rhythm.
A person tends to associate feelings of fatigue and drowsiness with a need for sleep, which is the homeostatic mechanisms at work.
The circadian rhythm includes the body’s natural responses to light and dark, which normally involve being awake and alert during hours of light, and feeling tired, sleepy, and subsequently sleeping, during periods of darkness.
Melatonin is a modulator involved in circadian rhythm changes, with increasing levels during darkness, and decreasing levels during hours of light.
Sleepiness
During hours of sleep, consciousness remains active, but is generally reduced, with a change in responsiveness.
When a person is awake, they are acutely aware of external stimuli; while asleep, consciousness is predominantly responsive to internal stimuli rather than external stimuli.
As a person experiences sleepiness, if there is a safe environment for sleep, the hypothalamus initiates actions to inhibit areas of the brain involved in arousal.
As the person reaches the sleep state, the regions of the brain stem, thalamus, and cortex operationally disengage.
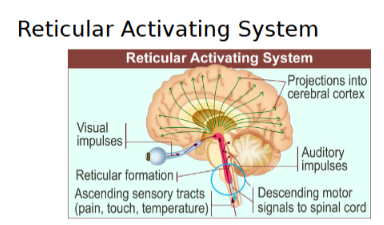
Reticular Activating System (RAS)
Located in the anterior of the brain stem.
the reticular activating system (RAS) is integral in some of the most basic functions, including consciousness, sensory perceptions and responses, ability to focus, and the sleep-wake cycle.
The RAS adjusts fast and slow sleep rhythms, which assist with coordination of wakefulness and sleep.
The RAS moderates muscle tone during different stages of sleep, most particularly contributing to the lack of muscle tone apparent during REM sleep, which prevents movement of the extremities during dreams.
The RAS is also involved in responses to pain and some mental health and neurological disorders, such as schizophrenia, Parkinson disease, post-traumatic stress disorder (PTSD), and narcolepsy.
Chemicals of Sleep
Chemical contributions to sleep are regulated by the circadian rhythm and include the nighttime secretion of melatonin, which assists in promoting sleep by opening the “sleep gate”, promoting Non-Rapid Eye Movement (NREM) sleep and improving the continuity of Rapid-Eye Movement (REM) sleep.
The release of prolactin, adrenocorticotropic hormone (ACTH), and norepinephrine are also under circadian influence.
The neurotransmitter adenosine is associated with a person’s feeling the need for sleep.
Additionally, adenosine is thought to promote deep slow-wave sleep and its restorative properties. It is metabolized during sleep, so low levels are apparent in the morning.
Cortisol is another chemical involved in circadian rhythm, as its early- morning release prepares the body to awaken.
Stages of Sleep
Sleep occurs in a series of four stages which accord with associated Electroencephalogram (EEG) waves.
These sleep stages happen throughout the sleep session (typically overnight) in a cyclical pattern, with a person spending about 75 percent of sleep time in Non-Rapid Eye Movement (NREM) stages I through III, and 25 percent in stage IV Rapid Eye Movement (REM) sleep.
Each cycle encompasses approximately 90 to 110 minutes, and it is normal to experience four or five cycles during a night’s sleep.
A full sleep cycle is comprised of three NREM stages and one REM stage. For most adults, the first cycle encompasses approximately 70 to 100 minutes, and subsequent cycles involve 90 to 100 minutes
Adults typically experience four to six cycles of sleep nightly, or during the major session of sleep.
The most restorative sleep occurs during the N3 stage, and most of this sleep stage occurs in the first few hours of sleep, with REM increasing in the latter cycles of sleep.
The first sleep cycle of the night, if undisturbed, includes all three NREM stages, including a repeat of N2, followed by REM, with continued cycles through the stages in this manner: N1—N2—N3—N2—REM.
Unless wakened, N1 is not repeated.
Stage I
Stage I (N1) is the first stage of sleep onset; this stage normally happens quickly, on average taking no more than seven minutes of body and brain relaxation to fall asleep.
About 5% of total sleep time is spent in stage I. (1-7 minutes)
As the individual relaxes, physiological activities, including those in the brain, become slower. This is often noted by a reduced heart rate, slow and regular respirations, and slow, rolling eye movements.
There may be occasional muscular movements seen, because skeletal muscle tone remains present during this phase.
If not disturbed during stage I, a person usually proceeds promptly to stage II and may not return to this stage for any significant amount of time. It is easy to awaken someone from stage I sleep
Stage II
Stage II (N2) sleep involves more changes, as sleep becomes deeper, with heart rate, respiratory rate and temperature all continuing to decrease.
Eye movement that slowed during stage I stops and people may grind teeth, with brief episodes of brain activitythat offer resistance to wakening.
Such bursts of activity within the brain are presumed to be involved in the solidification of memories.
The first stage II cycle lasts between ten and twenty-five minutes, and each following cycle becomes longer, until a total of about 45% of sleep time is spent in this stage.
Stage III
Slower brain waves
This stage is called: slow-wave sleep (SWS).
Metabolic, Immune, and Restorative actions occurring include:
Production of growth hormones
Regulation of immune function
Repair of muscle tissue
Decrease of temperature, heart, and respiratory rates,
Relaxation to the point of loss of skeletal muscle tone.
• Thought to contribute to creativity, memory, and higher-level thinking.
Approximately 25% of sleep is spent in stage III.
Deepest sleep; it is hard to be awakened.
If awakened during this stage, it is typical for the person to experience sleep inertia, or slowed processing of thoughts.
Urinating while asleep (enuresis) and sleepwalking.
Dreams are typically realistic in nature.
Occurs predominantly within the first half of a night’s sleep
Early cycles lasting twenty to forty minutes each and getting shorter throughout the night as more REM sleep begins.
Stage IV Rapid Eye Movement (REM) Sleep
REM sleep is considered stage IV of the sleep cycle. REM sleep, as the name indicates, is characterized by rapid movements of the eyes.
Additionally, during this stage:
Metabolism and brain activity increase
Memory storage, integration of learned concepts, and creativity
A lack of REM sleep can have negative impacts on:
Processing thoughts and emotions
Making connections
Can lead to psychophysiological symptoms and diagnoses related to sleep deprivation (depression, anxiety, lack of clarity in thinking, or decreased higher-level cognition)
• Dreams are common and tend to be very clear, emotional, and unbelievable. Nightmares also may occur during this phase, as well as sexual stimulation in the form of penile erections and clitoral dilation.
electroencephalogram
a linear tracing of the electricity of brain waves able to identify the different periods or stages of sleep. The EEG waveforms change during the different stages.
The first period is non-rapid eye movement (NREM) sleep and is comprised of three stages of sleep itself.
Sleep waves in the first stage of NREM in itself
Stage I (falling asleep): EEG waves change from the beta waves (associated with being awake) to alpha waves (relaxed but awake state), to theta waves of light sleep.
• Two waves:
The fast alpha wave, which is typical while awake and resting
The alpha wave is followed by a theta wave, which is also fast, with variable frequencies
Stage II: sleep has two characteristic EEG changes:
a short, intermittent burst of neurological activity called sleep spindle and K- complex, each of which lasts about one second and is associated with the delta wave
Stage III:
the EEG displays slow delta waves; this stage is also referred to as slow-wave sleep (SWS)
The second period is rapid eye movement (REM) sleep is associated with fast movements of both eyes.
REM is generated by activation of “REM-on neurons” that stimulate responses from both the parasympathetic and sympathetic nervous systems.
This increased brain activity is apparent on the EEG, as the waveform during REM sleep appears much like that of someone who is awake.
Sleep Patterns
Monophasic sleep pattern: most common sleep pattern globally, in which one major block of time allocated for sleep.
A period of sleep is typically overnight, and sleep occurs in the stages described in cyclical fashion. Sleep cycles repeat until natural awakening, which frequently correlates with morning light, or until wakened by an alarm or other interruption.
Biphasic sleep pattern: two sleep sessions per day, including a sleep period of several hours overnight, and another, shorter sleep in the later morning or afternoon (siesta). Those working irregular hours/night shift workers
Polyphasic sleep pattern: normal for infants and young children, who sleep several times in a twenty-four-hour period.
Until a neonate’s sleep pattern normalizes to days and nights, even the overnight sleep cycles are not particularly long.
Monophasic sleep pattern
most common sleep pattern globally, in which one major block of time allocated for sleep.
A period of sleep is typically overnight, and sleep occurs in the stages described in cyclical fashion. Sleep cycles repeat until natural awakening, which frequently correlates with morning light, or until wakened by an alarm or other interruption.
Biphasic sleep pattern
two sleep sessions per day, including a sleep period of several hours overnight, and another, shorter sleep in the later morning or afternoon (siesta). Those working irregular hours/night shift workers
Polyphasic sleep pattern
Normal for infants and young children, who sleep several times in a twenty-four-hour period.
Until a neonate’s sleep pattern normalizes to days and nights, even the overnight sleep cycles are not particularly long.
Sleep Architecture
Sleep patterns are also referred to as sleep architecture.
A sleep study, or polysomnography, involves results of assorted physiologic monitors, including EEG, electrocardiogram (ECG), electrooculogram (EOG), electromyogram (EMG), and oxygen saturation (SaO2).
The individual’s sleep architecture is displayed as a graph, called a hypnogram.
Hypnogram
is a diagram of the stages of sleep as they occur during a period of sleep. This hypnogram illustrates how an individual moves through the currently recognized stages of sleep.
Sleep Hygiene
Healthy transitions between the stages of sleep happen more often if an individual has good sleep hygiene, or healthy sleep habits.
Factors affecting sleep hygiene include:
maintaining regular sleep and wake times
providing an environment conducive to sleep (e.g., dark, quiet, cool room),
allowing enough time for adequate sleep
reducing substance use (e.g., alcohol, caffeine, and nicotine)
addressing sleep-related disorders (e.g., sleep apnea, restlessleg syndrome, etc.)
Developmental Patterns
During growth and development phases, sleep patterns change.
This includes quality of sleep, time preference, sleep stages, and sleep patterns, with resulting adjustments to sleep architecture.
With advancing age, from infancy to older adults, the need for sleep tends to lessen to some extent, from the majority of a twenty-four-hour period to about eight hours.
Gender also has some general differences, with men in stage I sleep and waking more times overnight than women. Women tend to take longer entering sleep, and spend longer in SWS.
Pregnancy and the postpartum period bring their own challenges, with more sleepiness during the day and struggles to find comfortable positions in advanced stages of pregnancy.
During this stage of sleep, an individual is most likely to experience realistic dreams, enuresis, and sleep-walking:
C/ Stage 3