8. small animal med- pancreatitis
1/70
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
71 Terms
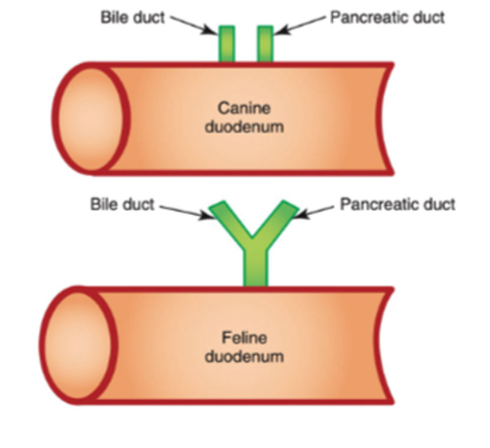
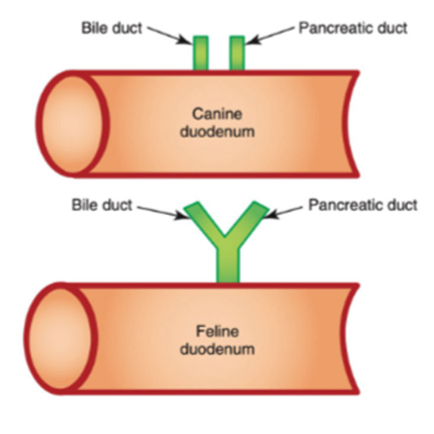
How do cats and dogs differ with their pancreatic duct?
pancreatic duct of cats and bile duct join together before opening into duodenum
bile duct and pancreatic duct of dogs do not join together
what are pancreatic acinar cells?
secretory epithelial cells
what are the functions of the pancreatic acinar cells?
produce and store proteolytic enzymes in inactive forms (zymogens) and other enzymes in active form (amylase, lipase)
what is the function of zymogens?
protect against autodigestion
-released into duodenum
-converted to active enzymes by enterokinase at small intestine brush border
what is acute pancreatitis?
inflammation that is completely reversible after removal of inciting cause
what is chronic pancreatitis?
inflammation that results in irreversible histopathologic changes
is acute or chronic pancreatitis more common in dogs and cats?
acute pancreatitis is most common in dogs
chronic pancreatitis is most common in cats :(
what are the main differences between acute and chronic pancreatitis (besides chronicity)?
histopathologic differences;
difference is not necessarily clinical can be difficult to distinguish between episode of acute pancreatitis vs acute exacerbation of chronic pancreatitis
are chronic cases of pancreatitis more commonly mild or severe?
mild
are acute cases of pancreatitis more commonly mild or severe?
severe
how does mild pancreatitis present?
-few systemic complications
-minimal pancreatic necrosis
-low mortality
how does severe pancreatitis present?
-extensive pancreatic necrosis
-poor prognosis in some cases
what are indicators of severe necrotizing pancreatitis?
-severe dehydration (8-10%)
-persistent clinical signs despite medical management
-hypotension
-hypoglycemia
-ionized hypocalcemia
what are complications of severe necrotizing pancreatitis?
-extrahepatic bile duct obstruction (cholestatic to mixed hepatopathy)
-SIRS
-cardiovascular shock
-DIC
-pulmonary thromboembolism
-multiorgan failure (AKI, lung injury)
what is the etiology of pancreatitis?
1. idiopathic (most common in dogs and cats)
2. immune mediated:
-cats: anecdotal response to immunosuppression
-cocker spaniels: multiorgan autoimmune disease (KCS, proteinuria, etc)
what are risk factors for acute pancreatitis?
-hypotension associated with anesthesia
-dietary indiscretion/high fat diet
-zinc toxicity (penny ingestion)
-drugs (phenobarb, KBr, azathioprine, clomipramine)
what are risk factors for chronic pancreatitis?
-obesity
-endocrinopathies
-hypertriglyceridemia (dogs)

what endocrinopathies are risk factors for chronic pancreatitis?
dogs: hyperadrenocorticism, hypothyroidism
dogs and cats: diabetes mellitus
what is the pathophysiology of acute pancreatitis?
premature activation of digestive enzymes and zymogens, particularly trypsinogen, within acinar cells
results in autodigestion
what is the pathophysiology of chronic pancreatitis?
trypsin activation not considered the inciting event:
-oxidative stress activates pancreatic stellate cells (leads to fibrosis and low-grade inflammation)
-inflammation in neighboring biliary system or intestines may cause inflammation in the pancreas (eg feline triaditis)
what are the clinical signs of pancreatitis?
clinical signs are nonspecific:
-lethargy
-partial/complete anorexia
-vomiting
-weight loss
-diarrhea (small, large, mixed)
-dyspnea
how can chronic pancreatitis be diagnosed based off of physical exam?
GI symptoms may be subtle and often intermittent in cases of chronic pancreatitis
what are physical exam findings of acute pancreatitis?
-dehydration
-hypothermia
-icterus
-abdominal pain
-hyperthermia/fever
-abdominal mass/cranial abdominal organomegaly

what clinpath changes may be seen with pancreatitis?
CBC and biochem panel (nonspecific findings):
-leukocytosis, left shift neutrophilia
-cholestatic or mixed liver enzyme elevation, hyperbilirubinemia
-azotemia (pre-renal or renal[AKI])
-hyperlipidemia
-hypoalbuminemia
-hypo or hyper-glycemia
-hypokalemia
-hypocalcemia
clin path may be normal with chronic pancreatitis
is serum lipase reported on chemistry panels specific for pancreatic lipase?
no
-lipase originates from other organs (esp. stomach and liver)
-not recommended for as standalone test to diagnose pancreatitis
-if 3-5x elevated, consider pancreatitis as ddx if consistent clinical signs
-better to measure pancreatic lipase
what do pancreatic lipase immunoreactivity (cPLI/fPLI) tests measure?
measures lipase of pancreatic origin
what are 2 types of cPLI/fPLI tests?
1. spec cPLI/fPLI: quantitative assay (send-out test)
2. SNAP cPLI/fPLI: semi-quantitative assay (normal vs abnormal; bed-side test)

which PLI test is considered to have the highest sensitivity/specificity for pancreatitis?
spec cPLI/fPLI quantitative assay (send-out test)
if positive--> pancreatitis is a differential
if negative--> unlikely to have pancreatitis
is the SNAP cPLI/fPLI a reliable test for diagnosing pancreatitis?
has good sensitivity and can be used as a rule out test (if negative, unlikely to be pancreatitis)
but, has poor specificity (if positive, animal might have pancreatitis, but consider other ddx)

how can lipase activity assays be used to diagnose pancreatitis?
uses DGGR as a substrate for pancreatic lipase
-lipase cleaves DGGR and products of this reaction are measured
however, this test is found to measure other lipases, so not specific for pancreatitis
what are causes for false positives on pancreatic lipase assays?
-hyperadrenocorticism/Cushing’s (or exogenous steroid use)
-GI foreign body obstruction
-decreased renal clearance (renal dz)
-pancreatic inflammation associated with diffuse abdominal inflammation (septic peritonitis)
-subclinical inflammation
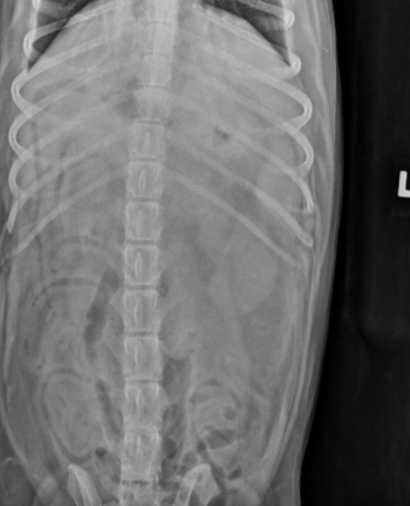
are radiographs useful in diagnosing pancreatitis?
not really, rads are insensitive and nonspecific; used to rule out other ddx
rads are frequently normal especially in chronic pancreatitis

what radiographic changes may be seen in the abdomen with acute pancreatitis?
-loss of peritoneal detail in cranial abdomen
-mass effect in cranial abdomen
-mild gas dilation of the duodenum
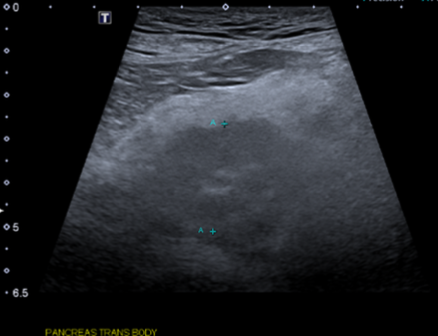
what is the first-line diagnostic imaging modality for diagnosing pancreatitis?
ultrasound
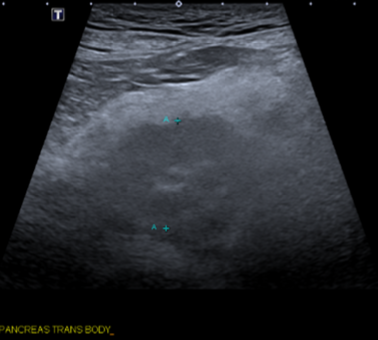
what U/S changes will be seen in patients with chronic pancreatitis?
normal to mild changes

what U/S changes will be seen in patients with acute pancreatitis?
-pancreatic enlargement
-hyperechoic mesentery
-focal abdominal effusion
-duodenum distended or corrugated
-pancreatic abscessation/necrosis
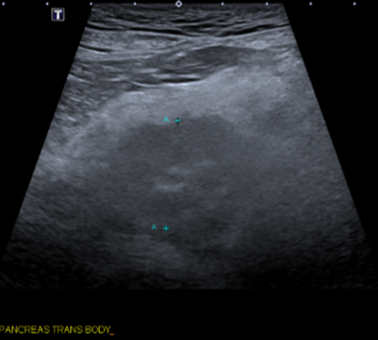
what are the limitations of abdominal ultrasound for diagnosing pancreatitis?
-better for identifying acute pancreatitis (poor for chronic)
-difficult to differentiate chronic pancreatitis from pancreatic nodular hyperplasia (incidental finding in older pets)
-may not be able to see LEFT limb of pancreas - difficult to visualize due to gas artifact (acoustic shadowing) from the stomach and/or colon
what are the advantages of using abdominal CT angiography for diagnosing pancreatitis?
-able to visualize entire pancreas
-better identification of acute pancreatitis, abscessation, masses than ultrasound
-identification of portal vein thrombosis

is there a single diagnostic test that has high enough specificity to conclusively diagnose pancreatitis based on a single test result?
no, need to look at entire clinical picture as no single diagnostic test has high enough specificity!
what is the general management of acute pancreatitis?
1. ID and treat inciting cause if present
2. fluid therapy
3. antiemetics and GI prokinetics
4. pain management
5. nutrition
what are the goals of fluid therapy when using to treat acute pancreatitis?
correct dehydration, electrolyte imbalances, lactic acidosis
and to restore perfusion to pancreas
which IV fluid types should be used for treatment of acute pancreatitis?
balanced crystalloid solution
how are IV fluid plans created and monitored for treatment of acute pancreatitis?
create goal-directed fluid plan to avoid over-hydration:
-determine % dehydration based on PE, rehydrate over 4-6 hours (slower in Ps with advanced heart disease)
-provide maintenance fluid rate 2-3ml/kg/hr (+/- account for ongoing losses)
monitoring: reassessment of hydration and metabolic status
What is important with regards to fluid therapy in acute pancreatitis?
reassess, reassess, reasssess
what antiemetics are used for treatment of acute pancreatitis?
can be used in combination:
1. maropitant (IV, SQ, or PO)
2. ondansetron (IV, SQ, or PO)
Maropitant MOA? Ondansetron MOA?
Maropitant: neurokinin-1 (NK 1) receptor antagonist
Ondansetron: selective serotonin 5-HT3 receptor antagonist
what appetite stimulants can be used for treatment of acute pancreatitis?
1. oral or transdermal mitrazapine (cats)- has anti-nausea properties
2. capromorelin
-Elura for cats
-Entyce for dogs
Capromorelin MOA?
ghrelin receptor agonist, mimics action of endogenous ghrelin
what is the purpose of using prokinetics for treatment of acute pancreatitis?
for gastroparesis or ileus
what prokinetic medications are used for treatment of acute pancreatitis?
used to treat gastroparesis or ileus
-metoclopramide CRI
-cisapride PO
-erythromycin (low dose) in refractory and/or critical patients
what are the first-line agents for pain management in patients with acute pancreatitis?
full mu-opioids (fentanyl, methadone, morphine)
use cautiously in cases of gastroparesis or severe ileus
what adjunctive analgesic drugs can be used in cases of acute pancreatitis with severe/refractory pain or ileus?
ketamine and or lidocaine (dogs only) CRI
what analgesics can be given for outpatients or for mild pain after discharge for acute pancreatitis?
gabapentin
oral buprenorphine (cats)
codeine
which pain medications should be avoided in patients with acute pancreatitis?
NSAIDs
-will have GI adverse effects
-in combo with hypovolemia/dehydration, increases risk of AKI
why is early enteral nutrition for treatment of acute pancreatitis so important?
-improves GI motility
-maintains integrity of gut barrier
-minimizes pancreatic necrosis
-decreases incidence of multi-organ failure
-prevents hepatic lipidosis (cats)
-improves outcomes
-faster return to voluntary intake
-reduced rates of GI upset
how can early enteral nutrition be achieved in patients with acute pancreatitis?
start supportive care immediately with anti-nausea meds and appetite stimulants
what are indications for NE/NG tube or esophagostomy tubes in patients with acute pancreatitis?
1. failure to respond to supportive care within 48 hours
2. history of prolonged anorexia before presentation
3. hepatic lipidosis (cats)

what are benefits of feeding tubes for treating acute pancreatitis?
-used to provide nutrition
-gastric decompression with gastroparesis (NG tube only)
-can administer liquid PO medications
-can be used for hydration

what type of diets are used for nutrition in acute/chronic cases of pancreatitis?
for acute cases, prioritize caloric intake
general recommendations for acute and chronic cases:
dogs: low fat diet (<3g/100kcal)
cats: hydrolyzed protein diet
why are hydrolyzed protein diets fed to cats in cases of pancreatitis?
cats more commonly have chronic pancreatitis and associated with CIE
hydrolyzed proteins are less prone to stimulating pancreatic secretions than intact protein in cats
how are corticosteroids used for treatment of pancreatitis in dogs and cats?
have anti-inflammatory effects
-improved outcomes shown in dogs with acute pancreatitis
-can be used in management of chronic pancreatitis in cats (treat common comorbidities- sterile cholangitis, CIE)
is including antibiotics in treatment of pancreatitis recommended?
acute pancreatitis is considered sterile in most cases-
abx are not recommended unless infection is strongly suspected/confirmed
when may antibiotics be included in treatment of pancreatitis?
suspected/confirmed infection:
-pancreatic abscess, infected necrotic tissue
-concurrent bacterial cholangiohepatitis
-aspiration pneumonia
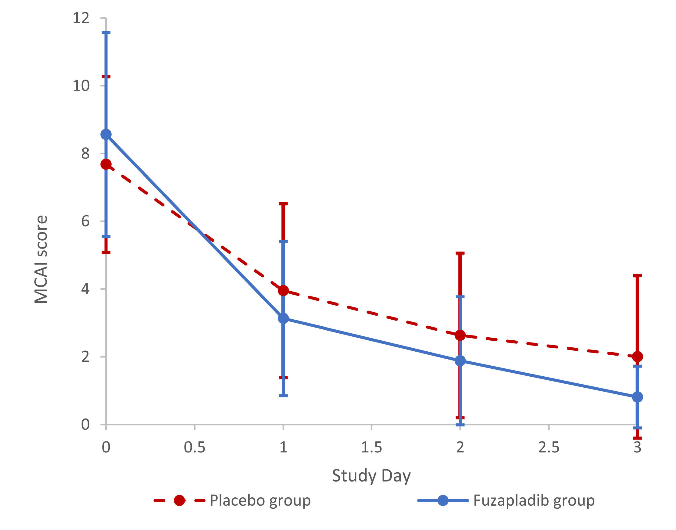
what is fuzapladip (panoquell, ceva)?
conditionally FDA approved drug for acute pancreatitis in dogs

what is the MOA of fuzapladip for treating acute pancreatitis?
leukocyte function-associated antigen-1 (LFA) receptor inhibitor
--> inhibits neutrophil adhesion and infiltration into pancreas
when can patients with acute pancreatitis be discharged from hospitalization?
1. voluntarily consuming >50% RER by mouth
2. stable on oral medications (pain, anti-nausea, appetite stimulant)
what is the management for chronic pancreatitis?
more common in cats and often idiopathic--> may experience acute exacerbation of chronic pancreatitis (treat for acute pancreatitis)
long term tx: hydrolyzed protein diet, +/- corticosteroids
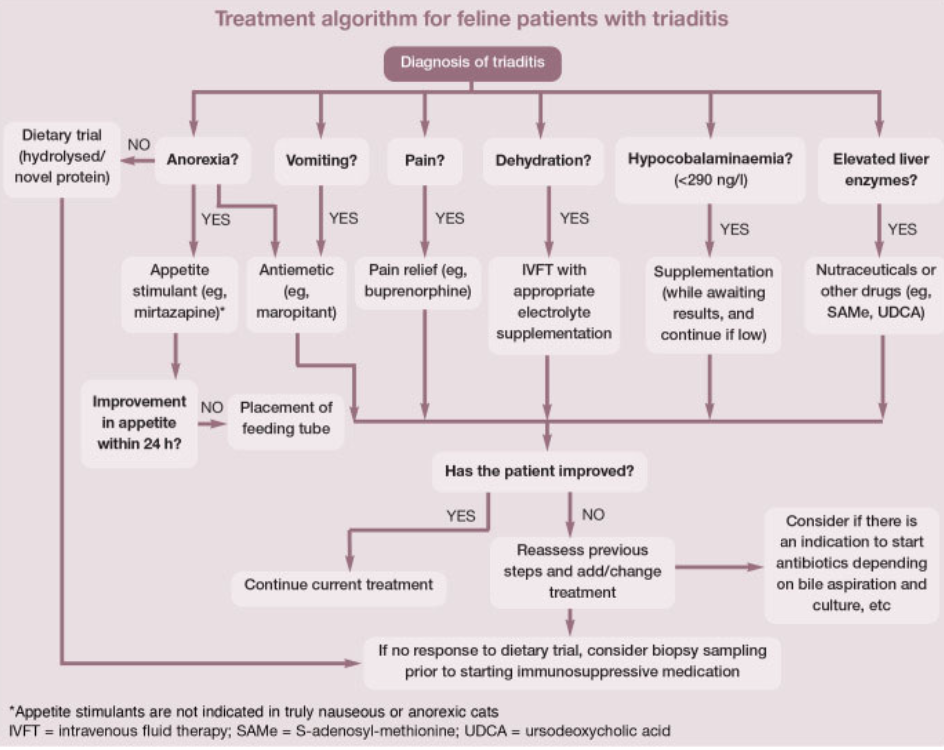
what is feline triaditis?
concurrent chronic pancreatitis, cholangitis, and CIE
why do cats get triaditis?
increased risk of bacterial reflux and parenchymal inflammation:
-short small intestine
-high bacterial load
-pancreatic duct joins common bile duct before entering duodenal papilla
how is feline triaditis diagnosed?
confirmed by histopath of all 3 organs
often presumptive diagnosis is made based off:
-chronic GI signs
-elevated liver enzymes +/- hyperbilirubinemia
-increased fPLI and/or abnormal pancreas on U/S
-evidence of CIE (thickened SI layers on U/S, low folate and/or cobalamin)
what are sequelae of severe acute or chronic pancreatitis?
1. exocrine pancreatic insufficiency (EPI)
2. diabetes mellitus
3. pancreatic pseudocysts