Aerobic: Clinical Exercise Testing and Interpretation
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
31 Terms
question intro…
1) What is the most common medical reason for referral to have a clinical exercise test performed on a patient?
2) As future clinician what clinical populations could benefit from a clinical exercise test?
1) symptoms (ex: chest pain)
2) anybody w/ chronic disease
Intro Clinical Exercise Testing (history + purpose)
-A part of exercise medicine for decades
historically not used (use to say don’t do PA)
1950’s Bruce: pushed HD patients (in controlled envionment) to predict mortality/morbidity
-Referred to as a graded exercise test (GXT) or cardiopulmonary exercise test (CPX).
-Purpose: to observe physiological responses to increasing or sustained metabolic demand
-The GXT/CPX typically continues until a sign or symptom-limited maximal level of exertion is reached
*so can safely do real-life activities
Indications for a Clinical Exercise Test: 3 general categories
-Diagnosis (e.g., presence of disease or abnormal physiologic response)
-Prognosis (e.g., risk for an adverse event)
*don’t want to be wrong here
-Evaluation of the physiologic response to exercise (e.g., blood pressure [BP] and peak exercise capacity)
-The most common diagnostic indication is…
-Current evidence does not support…
-the assessment of symptoms suggestive of ischemic heart disease (IHD).
-the routine use of exercise testing to screen for IHD in asymptomatic individuals who have a very low or low pretest probability of IHD.
-The clinical utility of exercise testing is aimed at
-Can be useful in the evaluation of individuals who
-Generally, exercise testing may be appropriate for individuals
-specific cardiac diagnoses
-present to emergency departments with chest pain…
-whose symptoms have resolved, have a normal ECG, and had no change in enzymes reflecting cardiac muscle damage
Conducting the Clinical Exercise Test
-Consider contraindications, the exercise test protocol and mode, test endpoint indicators, safety, medications, and staff and facility emergency preparedness.
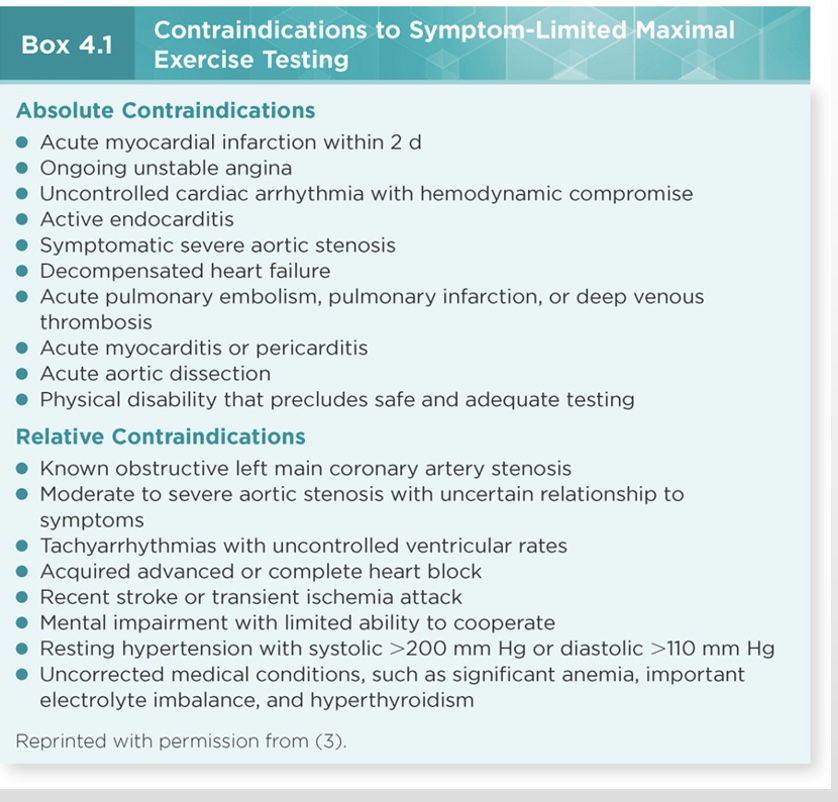
-AHA absolute/relative contraindications should be adhered to.
-Contraindications are intended to avoid unstable ischemic, rhythm, or hemodynamic conditions or other situations in which the risk associated with undergoing the exercise test is likely to exceed the benefit.
*don’t have to memorize picture!
Conducting the Clinical Exercise Test: Testing Staff
-Exercise test supervision has shifted to nonphysician allied health professionals, such as clinical exercise physiologists, nurses, physical therapists, and physician assistants.
*increased skill overtime
-According to the ACC and AHA, the nonphysician allied health care professional who administers clinical exercise tests should have cognitive skills similar to, although not as extensive as, the physician who provides the final interpretation.
Conducting the Clinical Exercise Test: Standard protocols and guidelines
-Standardized protocols represents a convenient and repeatable way to conduct the exercise test.
-Guidelines recommend that the protocol should be individualized based on a given individual’s age, exercise tolerance, or symptoms.
-Protocols most suitable for GXT include a low intensity warm-up phase followed by progressive, continuous exercise in which the demand is elevated to an individual’s maximal level.
true or false: never do a sub-max test in the clinical world?
true!
-need to push them
-do max test in a healthy person to predict their VO2
Monitoring and Test Termination
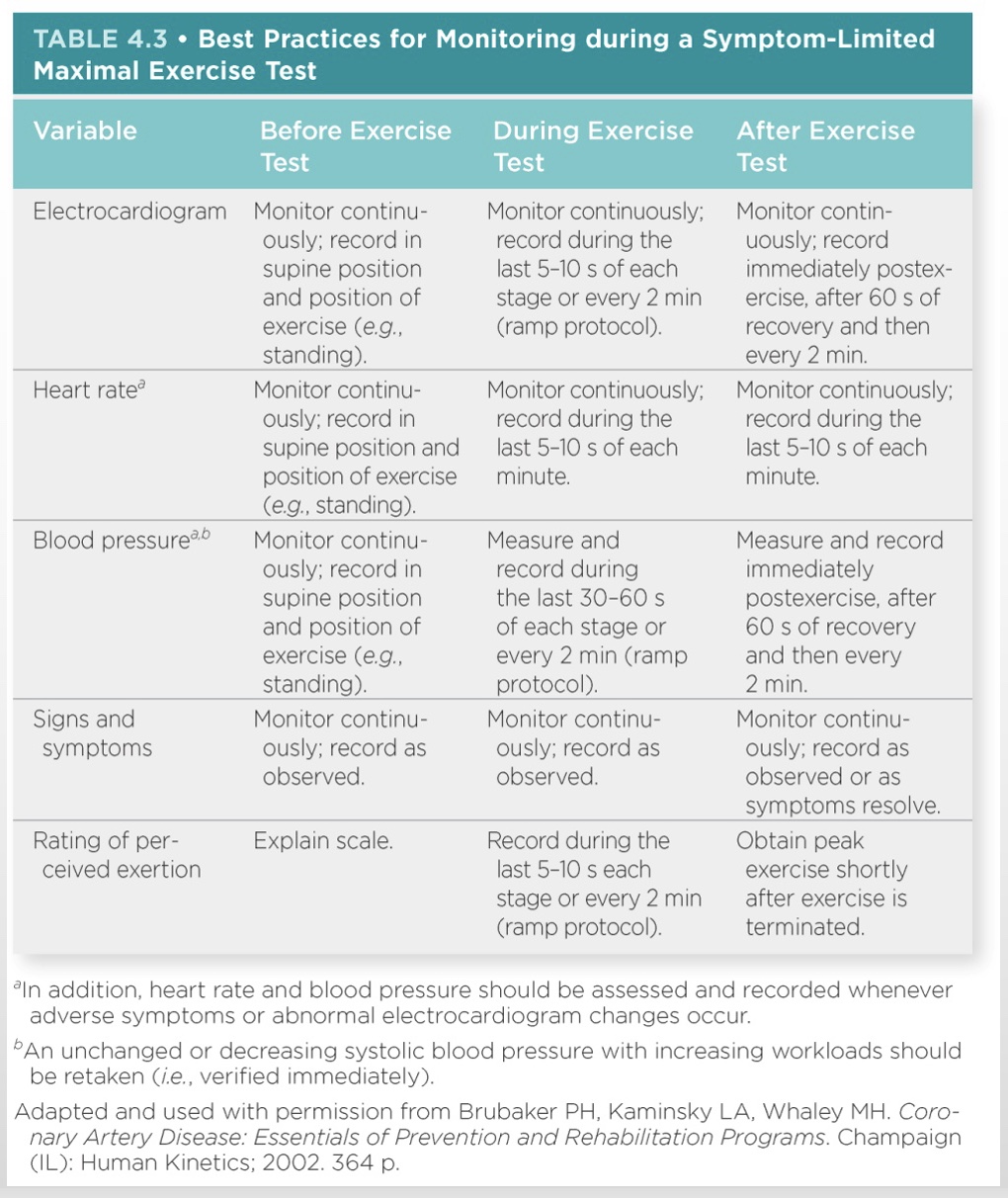
*Monitor: EKG, BP, RPE, clinical signs and reported symptoms
*Measure expired gas (important but not necessary)
-Variables typically monitored during GXT include HR; ECG; cardiac rhythm; BP; RPE; clinical signs & reported symptoms suggestive of myocardial ischemia; inadequate blood perfusion, gas diffusion, and limitations in pulmonary ventilation
-Measurement of expired gases during a CPET and O2 saturation of blood through pulse oximetry and/or arterial blood gases are also obtained when indicated.
Monitoring symptoms before and during exercise
*RPE: <1-2 at rest?
*BP: measure manually at least once every stage OR if symptomatic
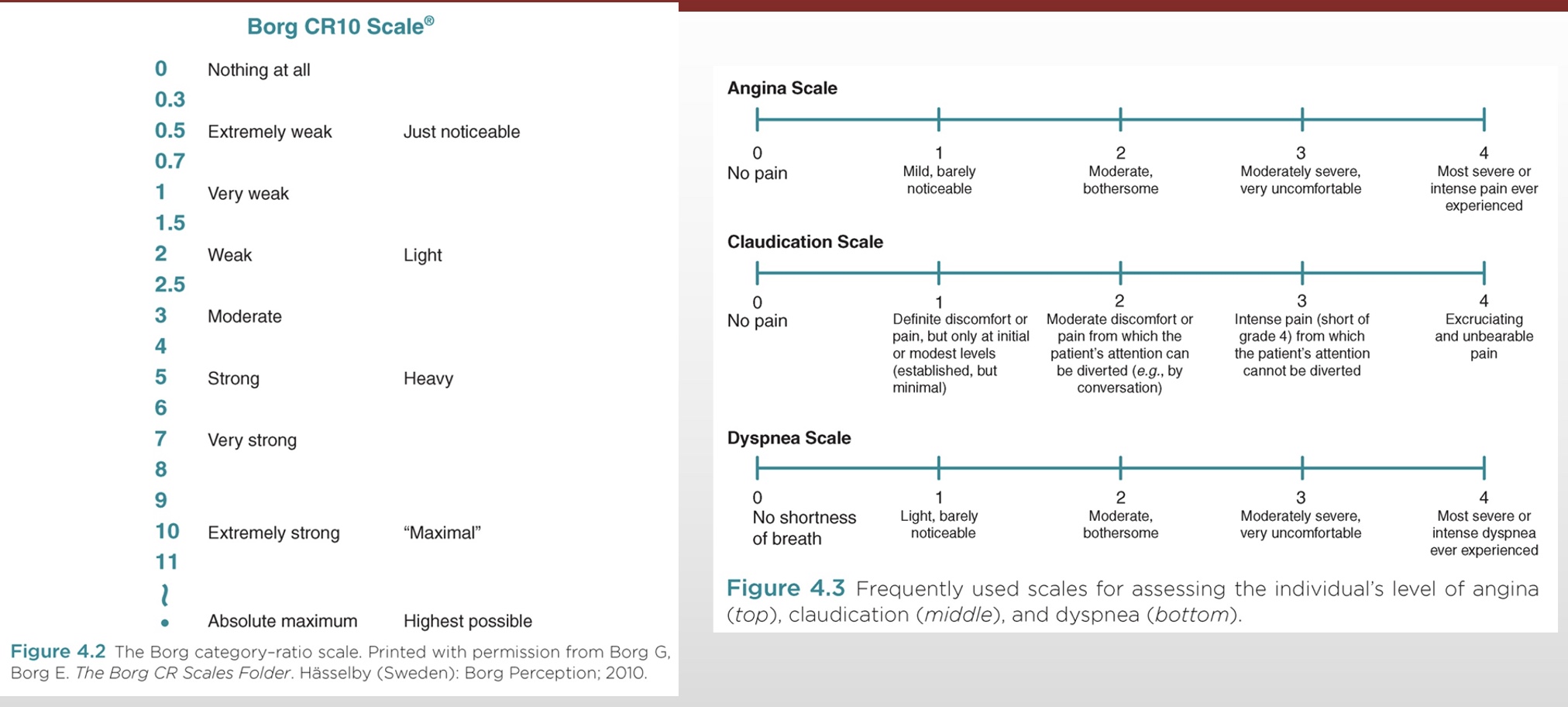
Frequently Used Scales for Reported Exertion, Angina, Claudication, and Dyspnea
-RPE: Borg
-Angina (chest pain): 2 where patient likely wants to stop test
-Claudication (peripheral vascular disease): 2-3 where patient likely wants to stop test; amputee if get to 4
-Dyspnea (shortness of breath)
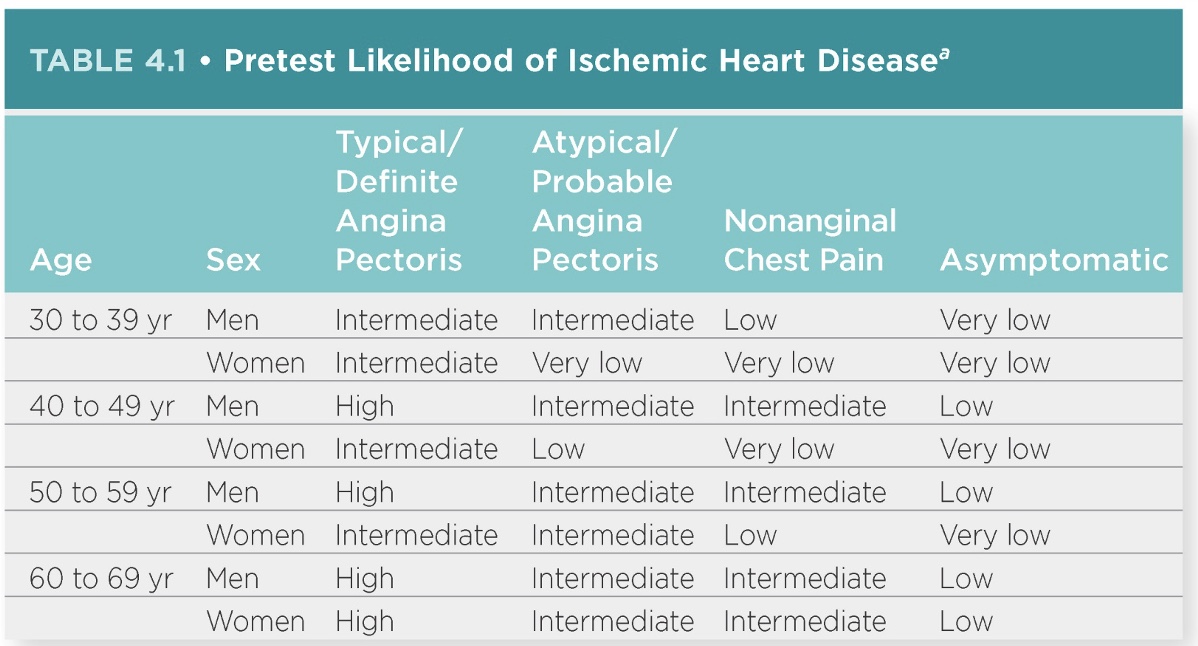
when are GXT truly predictive?
-age
-sex
-typical angina: classic heart pain? always intermediate-high
-atypical angina: less predictive
-nonangina chest pain: never relates heart pain
-asymptotic: very low; why no GXT
most accurate measure of exercise capacity
VO2
-It’s a useful index of overall cardiopulmonary health and may help overcome inaccuracies that may be associated with estimating exercise capacity from peak workload (e.g., treadmill speed and grade).
When the goal is a symptom-limited maximal exercise test…
a predetermined termination criteria should not be used as a reason to end the test.
*reproduce symptom
Postexecise and Safety
-Each laboratory should develop standardized procedures for the postexercise recovery period.
-Low intensity active recovery (ex: walk) is often practiced in order to support venous return and hemodynamic stability. (ex: middle school xc)
Exercise test sensitivity for the diagnosis of IHD can be maximized in a supine position immediately following exercise however this can result in profound hypotension and dangerous secondary ischemia. (*lay down protocol: put on bed immediately while measure things)
-Although events can occur, clinical exercise testing is generally safe when performed by appropriately trained clinicians.
*can also use medicines instead of exercise test (but uncomfortable; medicines have half lives)
factors to consider during an exercise test
-Individual symptoms, ECG responses, exercise capacity, hemodynamic responses, and the combination of multiple responses
Heart Rate Responses
-Equations exist to predict HRmax in individuals who are not taking a b-adrenergic blocking agent. (slows HR)
-HRmax decreases with age and is attenuated in individuals on b-adrenergic blocking agents.
▪All HRmax estimates have large interindividual variability with standard deviations of 10 beats or more.
*want symptom limited test
HR Responses: exercise and recovery
-Among individuals referred for testing secondary to IHD, and in the absence of b-adrenergic blocking agents, failure to achieve an age-predicted HRmax >85% in the presence of maximal effort is an indicator of chronotropic incompetence and is independently associated with increased risk of morbidity and mortality.
*most likely severe enough to elicit EKG changes
-A failure of the HR to decrease by >12 beats during the first minute or >22 beats by the end of the second minute of active postexercise recovery is strongly associated with an increased risk of mortality in individuals diagnosed with or at increased risk for IHD.
BP Response
*BP should go up! (don’t have great criteria)
-The normal systolic blood pressure (SBP) response to exercise is to increase at a rate of ~10 mm Hg per 1 MET.
-There is normally no change or a slight decrease in diastolic blood pressure (DBP) during an exercise test.
-Potential SBP responses: (and thus would terminate)
▪Hypertensive response (250/110)
▪Hypotensive response (w/ symptoms OR BP decreases while exercising)
▪Blunted response
▪Postexercise response
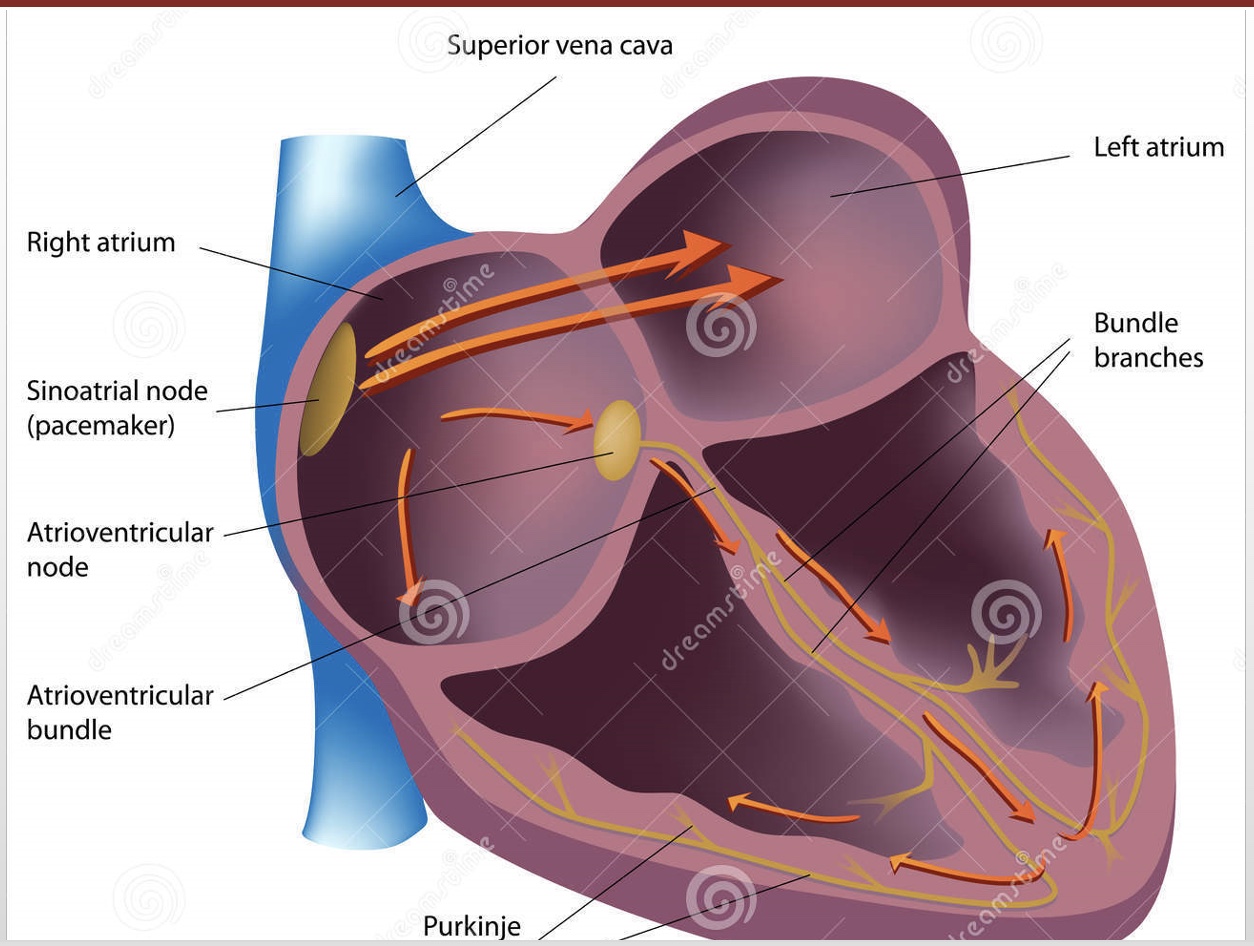
Heart conducting anatomy
-SA node
-AV node
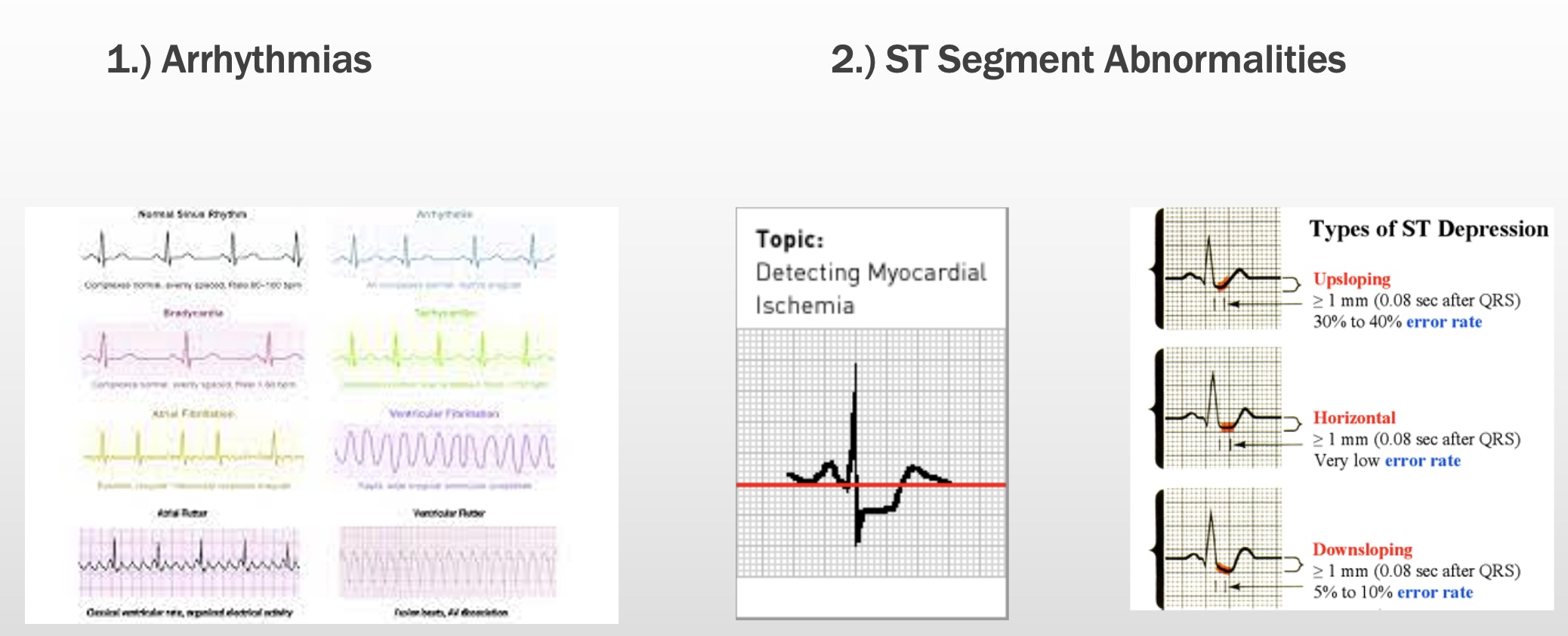
EKG Common Concerns
1.) Arrhythmias
-rhythm not expected at a given time
*ex: “sinus arrhythmia” w/ breathing is normal
2.) ST Segment Abnormalities
-ST depression=2mm depressed; coronary arteries not getting enough O2
-ST elevation= active myocardial infarction
Symptoms consistent with…. should be noted and correlated with…
-Symptoms that are consistent with myocardial ischemia (e.g., angina, dyspnea) or hemodynamic instability (e.g., light-headedness) should be noted and correlated with ECG, HR, and BP abnormalities (when present).
Exercise Capacity
*how long did the patient go?
-Evaluating exercise capacity is an important aspect of exercise testing.
▪High exercise capacity is indicative of a high Q and suggests the absence of serious limitations of left ventricular function.
-A significant issue relative to exercise capacity is the imprecision of estimating exercise capacity from exercise time or peak workload.
▪The standard error in estimating exercise capacity from various published prediction equations is at least ±1 MET.
*dif if w/ athletes and see abnormality; their heart suffers and adapts; ex: high troponin levels in marathoners; ex: exercised dogs survived cardiac event
CEP: VO2 vs. No VO2?
*useful? important for organ transplant criteria
-A major advantage of measuring gas exchange during exercise is a more accurate measurement of exercise capacity.
-CPET data may be particularly useful in defining prognosis and defining the timing of cardiac transplantation and other advanced therapies in individuals with heart failure.
-CPET is also helpful in the differential diagnosis of individuals with suspected cardiovascular and respiratory diseases.
Maximal vs. Peak Cardiorespiratory Stress
-When an exercise test is performed as part of the evaluation of IHD, individuals should be encouraged to exercise to their maximal level of exertion or until a clinical indication to stop the rest is observed.
-Various criteria have been used to confirm that a maximal effort has been elicited during a GXT:
▪A plateau in VO2 peak (*typically not in kids)
▪Failure of HR to increase with increases in workload
▪A postexercise venous lactate concentration >8.0 mmol . L−1
▪RPE at peal exercise >17 (6–20 scale) or >7 (0–10 scale)
▪A peak RER ≥1.10 (*gold standard; higher CO2 and no increase O2)
Diagnostic Value of Exercise Testing and Detection of Ischemic HD
-The diagnostic value of the clinical exercise test for the detection of IHD is influenced by the principles of conditional probability.
-The factors that determine the diagnostic value of exercise testing (and other diagnostic tests) are the sensitivity, specificity, and predictive value of the test procedure and prevalence of IHD in the population tested.
Sensitivity vs Specificity (and Predictive Value)
-Sensitivity: the ability to positively identify individuals who truly have IHD
*find disease in those who have it; ex: treadmill test have high sensitivity
-Specificity: the ability to correctly identify individuals who do not have IHD
*not high in treadmill test
*The predictive value is a measure of how accurately a test result correctly identifies the presence or absence of IHD and is calculated from sensitivity and specificity; These calculations yield true positive and false negative results
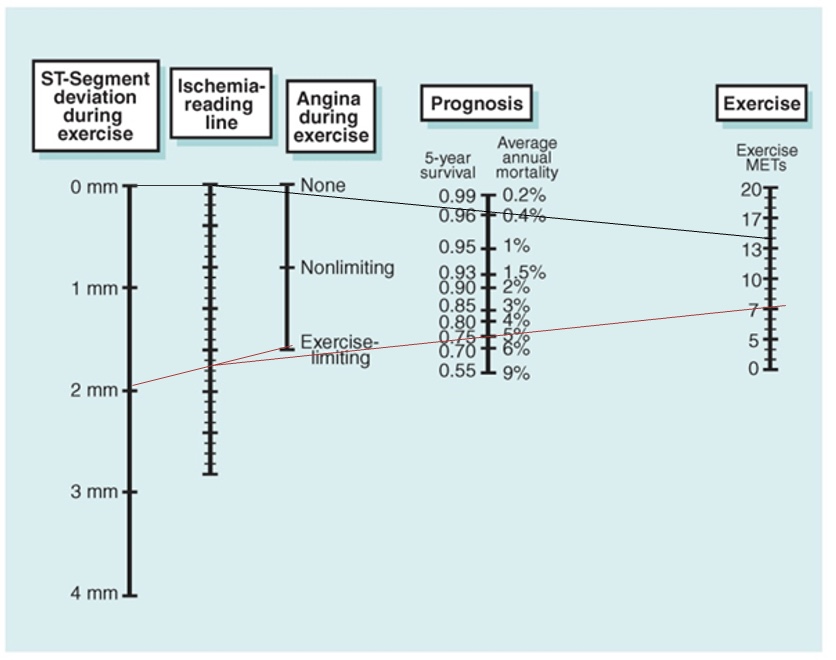
Diagnostic Value of Exercise Testing and Detection of Ischemic HD: chart
-The implementation of various exercise test scores that combine information derived during the exercise test into a single prognostic estimate has gained popularity.
-The most widely accepted and used of these prognostic scores is the Duke Treadmill Score or the related Duke Treadmill Nomogram
*chart ex: 75% survival rate if no intervention; who would recommend revasculation
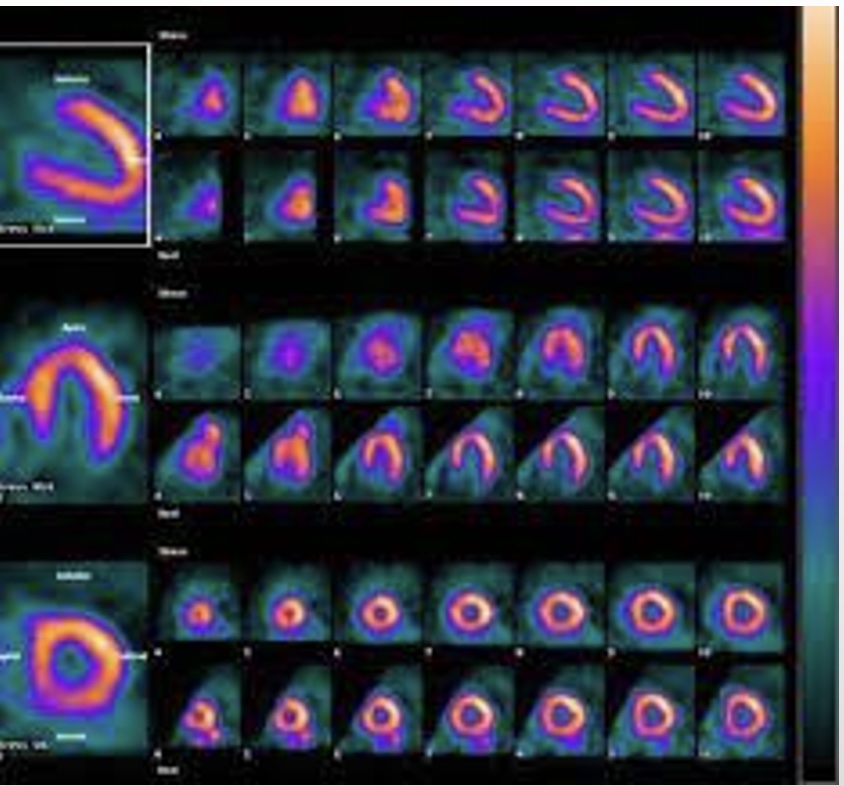
Clinical Exercise Tests with Imaging
*Nuclear study; picture of left ventricle, yellow=great profusion, dark=no blood flow
-When the resting ECG is abnormal, exercise testing may be coupled with other techniques designed to either augment or replace the ECG when resting abnormalities make evaluation of changes during exercise impossible.
-Myocardial perfusion imaging can be performed with a variety of agents and imaging approaches, although the two most common isotopes are 201thallium and 199mtechnetium sestamibi, also known as Cardiolite.
Field Walking Test
-Non-laboratory-based clinical exercise tests are also frequently used in individuals with chronic disease.
-These tests are generally classified as field or hallway walking tests and are typically considered submaximal.
-Similar to maximal exercise tests, field walking tests are used to evaluate exercise capacity, estimate prognosis, and evaluate response to treatment.
-Tests include 6-MWT, incremental, and endurance shuttle walk tests.
*lot w/ sick kids; already know their risk, disease, and what going on; chart prognosis based on ability to improve