PCT Patient Assessment
1/29
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
30 Terms
Components of Patient Assessment
Information gathering (MOI for trauma, NOI for medical, ascertain Hx, SAMPLE)
Physical examination (ABC or CAB, appropriate examination for medical/trauma)
BLS-PCS 10-12
Fundamental components of Patient Assessment
Identify problems (surveys), set priorities (primary and RTM/RMA), develop a care plan (interventions), execute the plan (perform interventions and ALWAYS REASSESS)
Scene Survey
Confirm the Call
Environment
MOI/NOI
Casualty Count
Additional/Allied Resources
PPE
Level of Consciousness
Introduction
AVPU
Hx of Event
C-Spine (Y/N)
Pt primary survey
Scene
LOC
(a) Conscious
Airway (patency, OPA/NPA indicated, look for obstructions)
Breathing (Look - RRV breathing, SpO2, position, expose and observe; Listen - Auscultate x 4, stridor, wheezes, etc.; Feel - tracheal deviation, subcutaneous emphysema, intercostal indrawing, diaphragmatic breathing, tenderness)
Circulation (Compare radial vs carotid, RRV of pulse, skin colour/temp, capillary refill, wet check, JVD, Apply cardiac monitor, 12 lead?)
(b) Unconscious
C - pulse? No → CPR, Yes, move to A
A - patency? No → Use A/W clearing maneuvers, Yes, move to B
B - Are they Breathing? No → PPV via BVM, Yes, do they need O2? Mode of delivery?, YES to all three, move to
(a) TRAUMA
Neck (Tracheal deviation, JVD, palpate c-spine for tenderness & step, deformity, CLAPS/TICS, Apply cervical collar)
Abdomen (CLAPS/T or DR GERM, guarding, previous surgeries, palpate for rebound tenderness rigidity)
Pelvis (check 3 plains - in down & up, CLAPSS/TICS)
Femur (CLAPS/TICS)
(b) MEDICAL
Disability - altered LOC?
Stroke Assessment
OPQRST - pain assessment
Check PEARL
Note patient positioning
Treat & GO
you must get pt to ER but you must first decide on a Tx. This will be based on current findings from primary survey
decide on an extrication plan
ANY PT WITH CARDIAC, RESP, ALTERED LOC - DO NOT WALK THESE PTS
History Taking must be completed before Tx
Primary Survey Overview
CEMCAP
LOA
Manual C-spine
A or C
B or A
C or B
Critical Injuries and gross bleed check
critical interventions
Medical General Impression
Is my pt hurt?
How bad?
Trauma General Impression
Is my pt sick?
If so, how sick are they?
signs of significant distress
altered mental status
anxiousness
laboured breathing
difficulty speaking
diaphoresis
poor colour
obvious pain
obvious deformity, guarding, or splinting
gross external hemorrhage
AVPU
Alert and Oriented
Verbal stimulus is required
Painful stimulus is required
Unconscious
Chief Complaint
Verbal - Pt tells you
Non-Verbal - What you can ascertain
Second-Hand - What other people say
SMR
Spinal Motion Restriction (BLS-PCS pg 34)
ABCDE
Airway (open airway, clear, insert npa or opa), Breathing (Assess, bvm, oxygen), Circulation (assess pulses, CPR, pt unconscious → CAB), Disability (pupillary response + neuro deficits), Expose (inspect the pt, cut away clothing)
Airway Status questions
Is the airway open and patent? (how it pt positioned, fbao?)
Is it likely to remain so? (Sonorous sounds, are there gurgling or bubbling sounds)
Airway adjuncts
oropharyngeal or nasopharyngeal airway, king-LT
open and clear the airway
chin lift and/or modified jaw thrust
visualize oropharynx
suction and/or remove foreign bodies
insert oral airway if the pt has decreased LOC and NO gag reflex (holds back tongue)
insert nasal airway if the pt has a decreased LOC and a gag reflex
V-VAC
Suction device, measure from corner of mouth to tragus, no more than 10 sec intervals adult 380mmHG, child 170mmHG, adequate oxygenation between intervals
King LT different sizes in adults
depends on height
yellow 4-5 feet
red 5-6 feet
purple over 6 feet
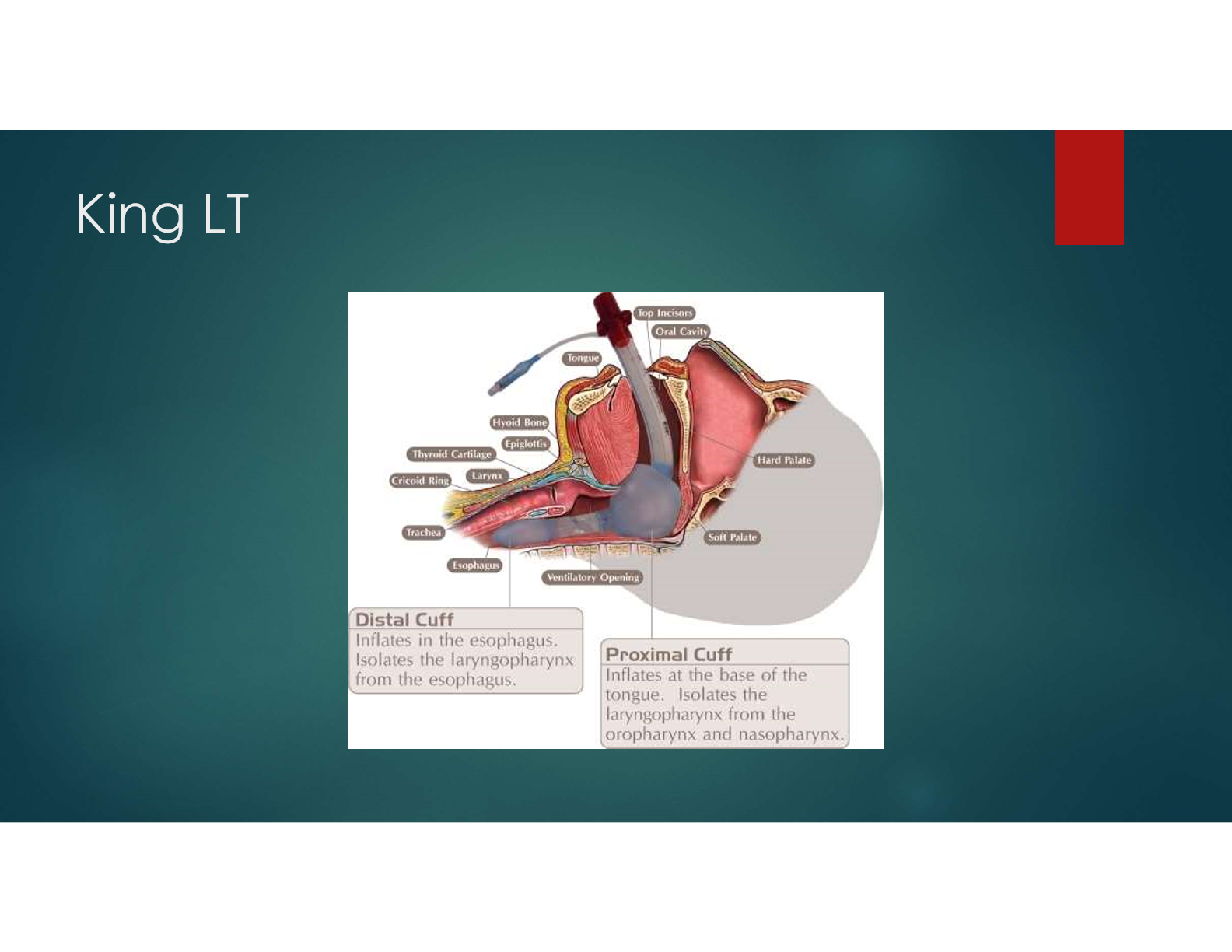
Supraglottic Airway Directive
Need for ventilatory assistance or airway control and other airway management is ineffective
PT must be in cardiac arrest, contraindications are inability to clear the airway, stridor, active vomiting, airway edema, caustic ingestion
max attempts is 2
Confirm placement with ETCO2 (non-waveform device), auscultation, chest rise, waveform capnogrpahy
Breathing Assessment questions
Is pt breathing?
If pt is breathing, is breathing adequate?
Minute volume
RR*Vt
Breathing Assessment
Look - for rise and fall of the chest
Listen - for the sound of moving air
Feel - for breath on your hand or cheek
determine whether pt is breathing and then whether the pt is breathing adequately, determine approx. rate, rhythm, and quality
Inadequate breathing
<8-10rpm = assist ventilations
>28 rpm with decreased LOC = assist ventilations
Adequate → provide supplemental oxygen prn
PRN
pro re nata - as needed
CLAPS/TICS-D
injuries to thorax and lungs
C- Contusions
L- Lacerations
A- Abrasions
P- Penetrations
S- Subcutaneous Emphysema
ribs, sternum, clavicles
T- Tenderness
I- Instability
C- Crepitus
S- Swelling
D- Dwelling
Auscultations
Listen in at least 4 sites comparing base to base and apex to apex
Are they present and equal in all fields?
Adequate?
Adventitious?
Symmetrical? Accessory muscle use
ACLS
Advanced Cardio Life Support