microbiology
1/18
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
19 Terms

A 61-year-old man with a history of COPD on systemic glucocorticoids presents with a 3-day history of a painful vesicular rash on his torso (shown in the image). Which event most likely immediately preceded the appearance of this rash?
✅ Correct Answer: E – Reactivation of latent pathogen in neural ganglia
Explanation:
The rash is in a dermatomal distribution with grouped vesicles → classic for herpes zoster (shingles) caused by reactivation of varicella-zoster virus (VZV).
After primary infection (chickenpox), VZV remains latent in the sensory dorsal root ganglia.
Immunosuppression (systemic glucocorticoids) can trigger viral reactivation.
The rash typically follows the affected dermatome and does not cross the midline.
💡 Memory hook: "Chicken hides in the ganglia" — VZV hides after chickenpox and comes back as shingles when immunity drops.
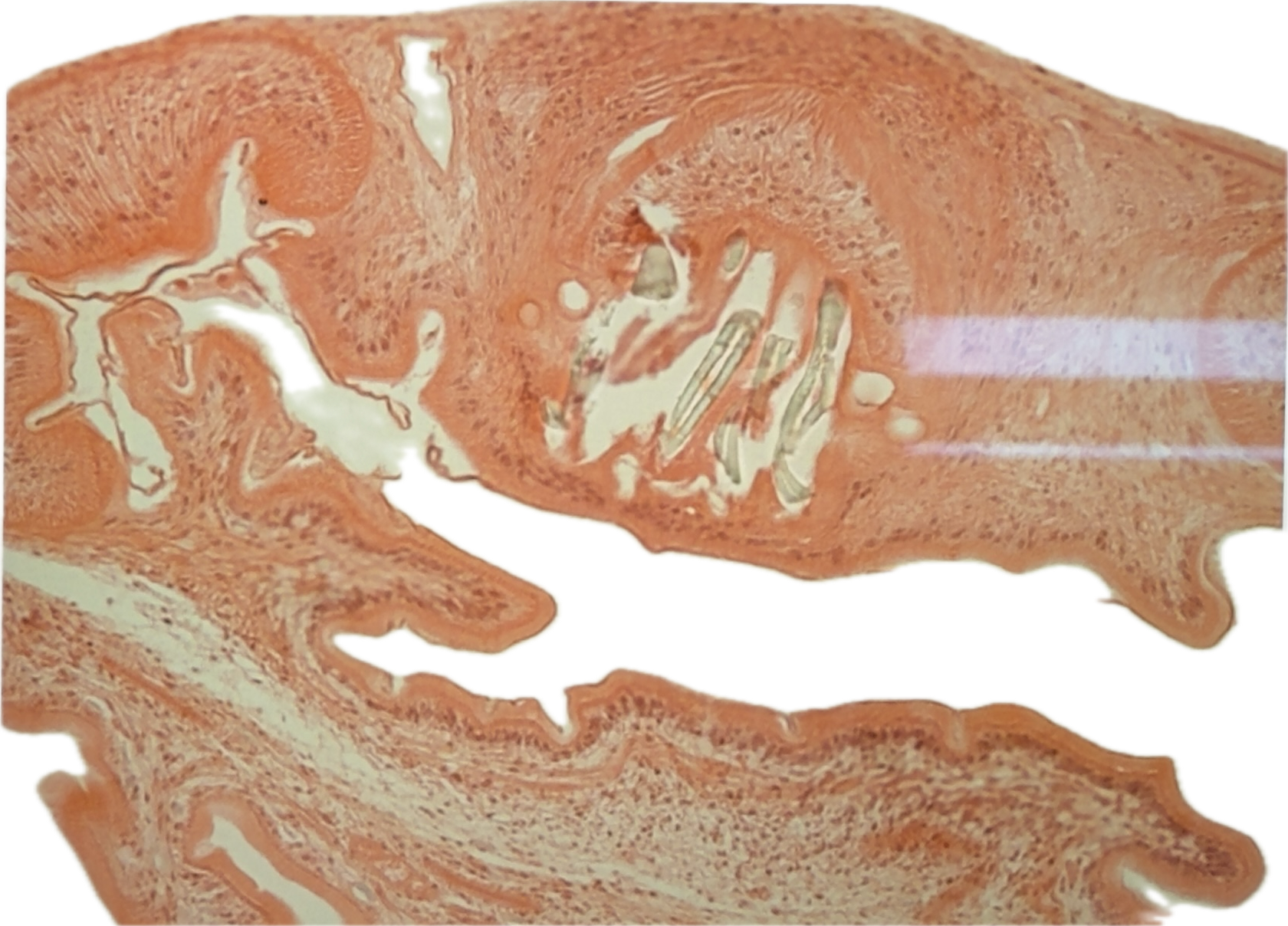
A 33-year-old man with new-onset seizures has a 3-cm cystic brain lesion. Histology shows a cyst with an invaginated scolex containing hooklets and suckers.
Question: What is the most likely diagnosis?
Answer: Helminth infection
Neurocysticercosis caused by Taenia solium (pork tapeworm) larval cysts.
Transmission: Ingestion of T. solium eggs from human feces (fecal-oral).
Pathophysiology: Eggs hatch in the intestine → larvae penetrate intestinal wall → hematogenous spread to brain, muscle, eye → form cysticerci.
Histology: Thick eosinophilic cyst wall + scolex with hooklets & suckers.
Presentation: Seizures, focal neurologic deficits, intracranial hypertension.
Treatment: Albendazole + corticosteroids (to reduce inflammatory response from dying parasites).
Memory hook: "Pork tapeworm in the brain = scolex staring at you"
During the course of a week at an overnight summer camp, 4 children (age 7–9) develop fever, cough, congestion, sore throat, and red eyes. PE: bilateral conjunctival injection, erythematous oropharynx; one child has crackles in LLL. All recover in 7 days with supportive care.
Question: What is the most likely cause of the outbreak?
Adenovirus – common cause of pharyngoconjunctival fever in children, often seen in crowded settings (camp, military barracks, daycare).
Transmission: Respiratory droplets, fecal-oral, waterborne (swimming pools).
Clinical triad: Fever, pharyngitis, conjunctivitis.
May also cause pneumonia, gastroenteritis, hemorrhagic cystitis.
Why not others:
Coxsackievirus: Herpangina or hand-foot-mouth, not conjunctivitis.
Influenza: Prominent myalgias, abrupt onset, seasonal pattern.
Norovirus: GI symptoms (vomiting, diarrhea).
Parvovirus B19: Fifth disease – “slapped cheek” rash.
RSV: Bronchiolitis in infants <2 y/o, not school-aged.
Memory hook: “Adeno at camp → red eyes, sore throat, fever.”
A 38-year-old woman presents with 2 days of headache, nausea, photophobia, and neck pain. Hx of migraines, but current episode is more severe and preceded by a flulike illness. Temp: 38.3°C (100.9°F), BP: 144/86, HR: 110. Patient appears lethargic, has nuchal rigidity, normal neuro exam, no rash, and normal non-contrast head CT.
Question: Best next step in management?
B – Lumbar puncture – This presentation is highly suspicious for meningitis (fever, headache, photophobia, nuchal rigidity).
Normal head CT rules out mass effect that would make LP unsafe.
LP allows CSF analysis to confirm diagnosis & guide therapy.
Empiric antibiotics should be started immediately after LP in stable patients; if unstable or high ICP suspicion → start antibiotics before LP.
Why not others:
A (O₂): Used for cluster headaches, not meningitis.
C (Metoclopramide): Migraine adjunct, but symptoms suggest infection.
D (MRI): Not needed before LP unless CT abnormal or neuro deficits present.
E (Sumatriptan): Migraine-specific; contraindicated in possible infection.
F (Topiramate): Prophylaxis for migraines, not acute management.
Memory hook: Fever + headache + stiff neck = rule out meningitis with LP (unless CT shows contraindication).
A 24-year-old woman presents with dysuria, urgency, and frequency. She is sexually active. Urine culture grows catalase-positive, gram-positive cocci.
Question: The organism is most likely to be?
C – Novobiocin resistant – This is Staphylococcus saprophyticus, a common cause of urinary tract infections in sexually active young women.
Gram-positive cocci in clusters → Staphylococcus species.
Catalase-positive → Staphylococcus (vs Streptococcus).
Coagulase-negative → Not S. aureus → likely S. epidermidis or S. saprophyticus.
Novobiocin resistance → S. saprophyticus (S. epidermidis is novobiocin sensitive).
Why not others:
A (Coagulase positive) → S. aureus (causes skin infections, abscesses, endocarditis, not primary UTI in healthy young women).
B (Hemolytic) → Could apply to S. aureus or Streptococcus, but here not specific enough & not fitting coagulase result.
D (DNase positive) → S. aureus, not S. saprophyticus.
E (Yellow pigment producer) → S. aureus (golden pigment).
Memory hook:
“Saprophyticus sticks to new brides’ bladders” → honeymoon cystitis; catalase+, coagulase–, novobiocin resistant.
Which characteristic explains why Plasmodium falciparum causes more severe malaria than other Plasmodium species?
Answer: Ability to infect erythrocytes of all ages.
Why it matters:
P. falciparum invades both young & mature RBCs → much higher parasite load.
Leads to severe complications like cerebral malaria & severe anemia.
Other species target only certain-aged RBCs (e.g., P. vivax & P. ovale → reticulocytes; P. malariae → older RBCs) → lower parasitemia.
High parasitemia → microvascular blockage from infected RBC adhesion (via PfEMP1).
Memory Hook:
💡 "Falciparum is not picky — it takes all the seats on the RBC bus."
Imagine a bus (the bloodstream) where other malaria species only take certain seats (reticulocytes or old RBCs).
P. falciparum grabs every seat → bus gets overcrowded → traffic jam (microvascular obstruction).
A 6-year-old unvaccinated boy has worsening paroxysmal cough followed by vomiting, afebrile, lungs clear. Gram-negative coccobacilli found in respiratory secretions.
Which mechanism explains his symptoms?
Answer: Loss of ciliated respiratory epithelial cells (Bordetella pertussis)
Key points:
Pertussis toxin impairs phagocytosis & lymphocyte migration (↑ lymphocytosis)
Tracheal cytotoxin directly damages ciliated epithelial cells → impaired mucociliary clearance → mucus accumulation → paroxysmal cough + post-tussive emesis
Three stages:
Catarrhal (mild URI symptoms)
Paroxysmal (severe cough fits, inspiratory "whoop", vomiting)
Convalescent (gradual recovery)
Spread by respiratory droplets
Memory Hook:
💡 "The cilia carpet gets ripped out" — imagine the airway as a carpeted hallway, and B. pertussis is ripping out the carpet fibers (cilia), so mucus just piles up in the hall until violent coughing tries to push it out.
A 1-year-old boy presents with fever, irritability, photophobia, and signs of meningitis after recent cochlear implant surgery. CSF culture grows coagulase-negative Staphylococcus. What is the most important virulence factor responsible for this infection?
✅ Answer: Synthesis of an extracellular polysaccharide matrix (biofilm)
Mechanism: Biofilm formation allows bacteria to adhere to prosthetic devices (e.g., cochlear implants) and protect themselves from host immune responses and antibiotics.
Organism: Commonly Staphylococcus epidermidis in prosthetic infections.
Importance: Biofilms resist phagocytosis, complement, and penetration by antibiotics, making infections chronic and difficult to eradicate.
Why not the others?
Protein A (choice C) binds Fc region of IgG — important in S. aureus immune evasion, but not the main virulence for prosthetic infections by coagulase-negative staph.
Capsule (choice B) aids immune evasion but is less crucial than biofilm in device-associated infections.
Memory Hook:
💡 “SErious Devices” → S. Epidermidis loves Sticky Encasements → biofilms stick to implants like glue.
43-year-old man with HIV on antiretroviral therapy develops fatigue, lower extremity edema, proteinuria, glucosuria, and signs of proximal tubule dysfunction; renal biopsy shows enlarged epithelial cells with intranuclear & intracytoplasmic inclusions. Most likely diagnosis?
Diagnosis: Tenofovir-induced nephrotoxicity
Mechanism: Tenofovir accumulates in proximal tubular epithelial cells → mitochondrial DNA damage & cell injury → proximal tubular dysfunction (Fanconi-like syndrome).
Histology: Cytoplasmic vacuolization, enlarged epithelial cells with eosinophilic inclusions.
Key clues:
HIV patient on tenofovir
Proteinuria + glucosuria (without hyperglycemia) → proximal tubule defect
Normal BP & no immune-complex signs → rules out hypertensive nephrosclerosis or postinfectious GN.
Memory hook:
💊 "Tenofovir hits the Tenants first" → Think "tenants" = cells lining the proximal tubules (where the damage happens).
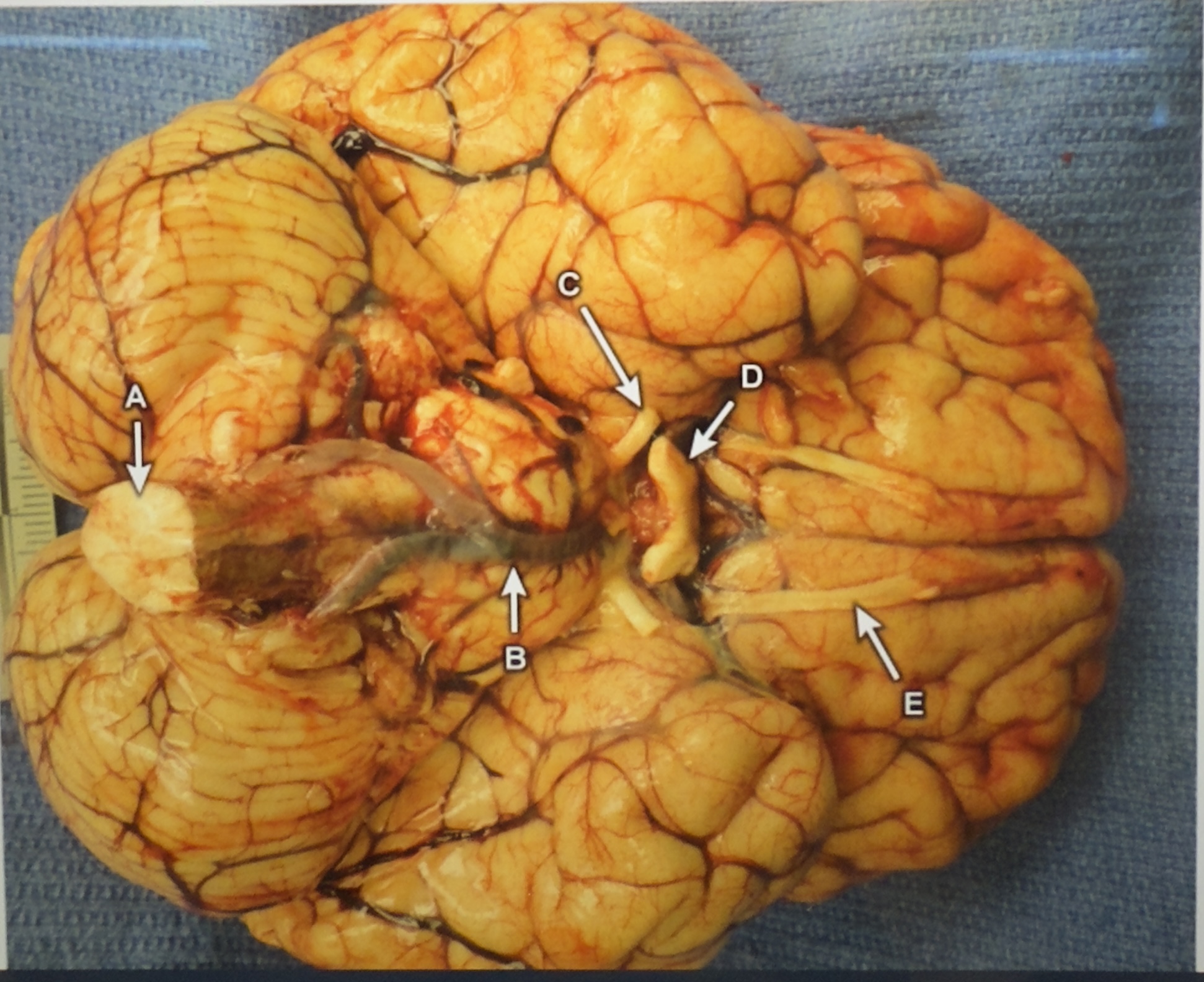
A 24-year-old man presents with seizures after 2 days of fever, headache, vomiting, and meningeal signs. He rapidly deteriorates and dies within 48 hours despite treatment. Autopsy shows congested leptomeninges with fibrinopurulent exudate, and microscopy reveals numerous amoebae in the brain tissue.
Question: What is the most likely portal of entry for this pathogen into the CNS?
Correct Answer: E, Cribriform plate (via olfactory nerve from nasal mucosa)
Explanation: The presentation is consistent with Naegleria fowleri primary amebic meningoencephalitis, which typically enters the CNS through the olfactory nerve after swimming in warm freshwater. The organism migrates via the cribriform plate to the brain, causing rapidly fatal necrotizing meningoencephalitis.
Key Facts:
Source: Freshwater (lakes, rivers, poorly chlorinated pools)
Portal of entry: Nasal mucosa → olfactory nerve → cribriform plate → CNS
Rapid progression (death within days)
Prevention: Avoid water entering nasal passages during freshwater activities
Memory Hook:
"Freshwater up the nose, brain’s where it goes" — think Naegleria riding the olfactory nerve like a water slide straight to the brain.
A 24-year-old man develops swelling, redness, and warmth around a dog bite from the previous day. The dog is fully vaccinated and lives with the patient. Wound cultures grow gram-negative coccobacilli with a mouse-like odor.
Question: Which organism is most likely responsible for this infection?
Correct Answer: Pasteurella multocida
Explanation:
Pasteurella multocida is a small, gram-negative coccobacillus commonly found in the mouths of cats and dogs.
Transmission: animal bites, scratches, or licking of wounds.
Clinical presentation: rapid-onset cellulitis, often within 24 hours, with pain, erythema, swelling, and possible lymphadenitis.
Culture clue: mouse-like odor on culture media.
Treatment: amoxicillin-clavulanate (covers Pasteurella & anaerobes).
Memory Hook:
"Pets pass Pasteurella" — think of your pet passing you a bad "present" after a bite. Mouse-like smell = small gram-negative culprit.
A 42-year-old man presents with dysuria and terminal hematuria after returning from several months in Africa. He went spelunking, bathed in lakes/beaches, and ate street food. Ultrasound: mild bilateral hydronephrosis & bladder wall thickening.
Question: Which animal is the most likely source of this patient’s infection?
Correct Answer: Freshwater snails (Bulinus species)
Explanation:
Infection: Schistosoma haematobium — trematode causing urinary schistosomiasis.
Transmission: Free-swimming cercariae released by freshwater snails penetrate human skin during swimming/bathing.
Pathogenesis: Eggs cause granulomatous inflammation → bladder wall thickening, hydronephrosis, and terminal hematuria.
Endemic areas: Africa & Middle East.
Chronic complication: Increased risk of squamous cell carcinoma of the bladder.
Memory Hook:
"Snails shoot schistosoma" — remember that in Africa, lakes + hematuria = Schistosoma haematobium from freshwater snails.
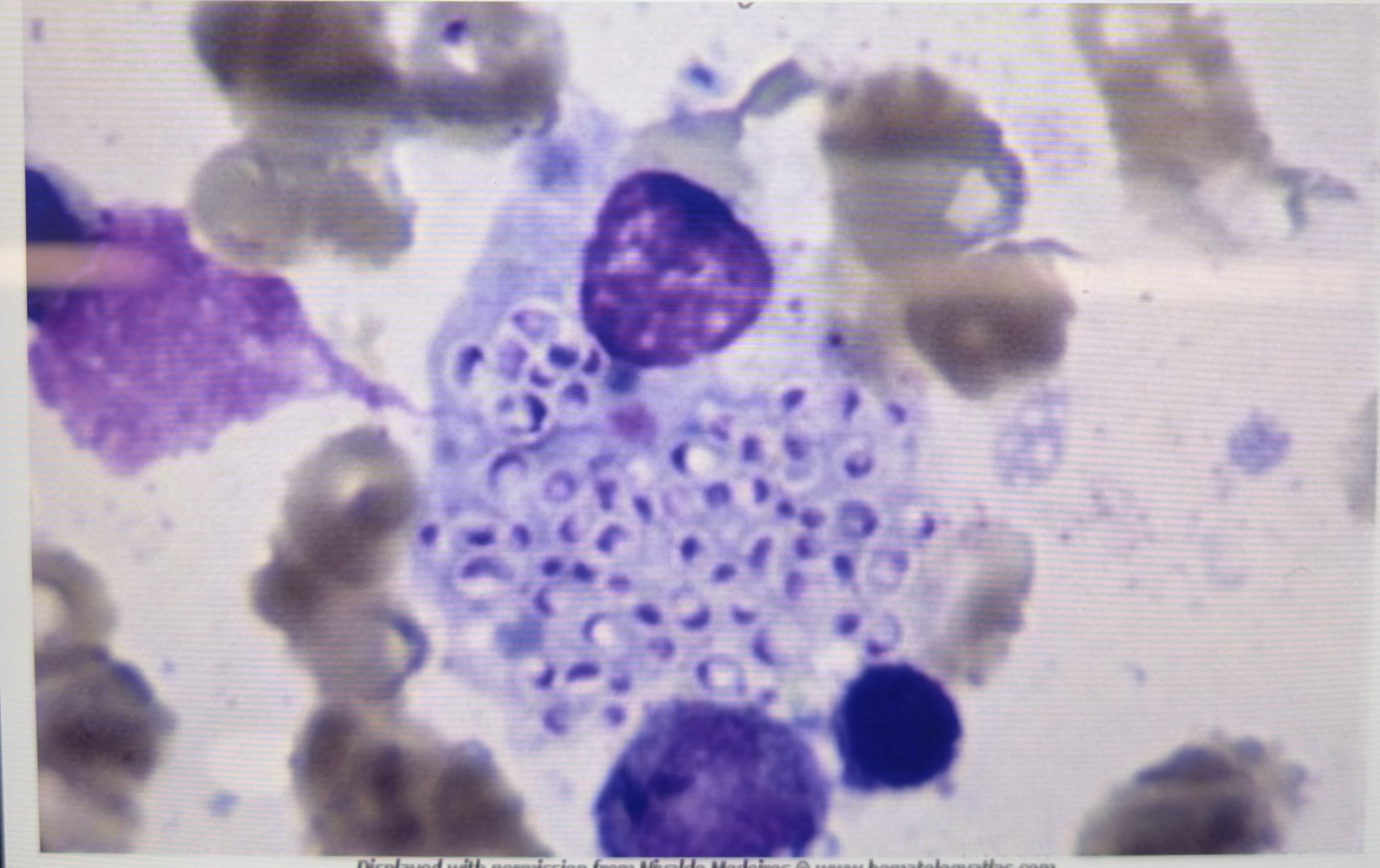
HIV-positive man with chronic cough, hepatosplenomegaly, pancytopenia, elevated liver enzymes. Bone marrow aspirate shows intracellular oval yeast forms within macrophages. What is the most likely pathogen?
Answer: Histoplasma capsulatum — dimorphic fungus endemic to the Ohio & Mississippi River valleys; acquired via inhalation of spores from bird/bat droppings. In immunocompromised patients, disseminates via macrophages to reticuloendothelial system (liver, spleen, bone marrow).
Why others are wrong:
Aspergillus fumigatus – Septate hyphae, not yeast; typically causes pulmonary aspergillosis, not intracellular yeast in macrophages.
Blastomyces dermatitidis – Broad-based budding yeast; not seen inside macrophages.
Candida albicans – Budding yeast with pseudohyphae; not intracellular.
Coccidioides immitis – Spherules with endospores; not small ovoid yeast.
Cryptococcus neoformans – Encapsulated yeast (India ink positive); not intracellular in macrophages.
Memory hook:
Think “Histo hides in macrophages” — small ovoid yeast clustered inside macrophages, especially in AIDS patients.
Advanced HIV patient with pulmonary nodules, hilar lymphadenopathy, and mucicarmine-positive, encapsulated, budding yeast in bronchoalveolar lavage. What is the most common manifestation caused by this organism outside the lungs?
Answer: Meningoencephalitis — Cryptococcus neoformans is an encapsulated yeast acquired via inhalation from environmental sources (often pigeon droppings). In immunocompromised hosts, it can disseminate hematogenously, most commonly to the CNS, causing subacute to chronic meningoencephalitis.
Why others are wrong:
Esophagitis – More often due to Candida, CMV, or HSV in HIV patients.
Interstitial pneumonia – Seen with Pneumocystis jirovecii, viral infections; not typical of Cryptococcus.
Oral plaques – Common in Candida albicans (oral thrush).
Sinusitis – Usually bacterial or due to fungi like Aspergillus in neutropenic patients.
Skin infection – Rare in Cryptococcus, usually in disseminated disease but not most common site.
Memory hook:
Think “Crypto → CNS” — after starting in the lungs, it loves to travel to the brain, especially in AIDS patients.
Young woman with fever, dysuria, flank pain, nitrite-positive urine, and culture showing motile gram-negative rods with metallic green sheen on EMB agar & hemolysis on blood agar. Which virulence factor is most important for causing her condition?
Answer: P fimbriae — Escherichia coli is the most common cause of acute pyelonephritis. P fimbriae (also called pili) are adhesins that allow the bacteria to bind tightly to uroepithelial cells, resist being washed away by urine flow, and ascend from the bladder to the kidneys.
Why others are wrong:
Capsule – E. coli’s K capsule helps evade phagocytosis and is important in neonatal meningitis, not pyelonephritis pathogenesis.
Heat-labile enterotoxin – Causes watery diarrhea in enterotoxigenic E. coli, not UTIs.
Lipid A – Endotoxin component causing septic shock; not the main driver of ascending UTI.
O antigen – Part of LPS outer membrane, used for serotyping; not related to urinary tract adherence.
Memory hook:
Think “P for Pyelonephritis” — P fimbriae let E. coli grab on and climb up the urinary tract.
Cystic fibrosis patient with chronic cough unresponsive to oral antibiotics. Hospitalized for IV antibiotics & respiratory therapy. In addition to routine culture media, what selective agar should be used to detect a highly drug-resistant organism common in CF patients?
Answer: Burkholderia cepacia–selective agar — CF patients are at high risk for infection with Burkholderia cepacia complex, a group of multidrug-resistant, gram-negative bacteria that can cause rapid pulmonary decline. Special selective media (eg, B. cepacia-selective agar) are required for reliable detection from respiratory specimens.
Why others are wrong:
Bordetella pertussis–selective agar (eg, Bordet-Gengou, Regan-Lowe) — used for whooping cough diagnosis; not relevant in this case.
Corynebacterium-specific agar (eg, cystine-tellurite) — for C. diphtheriae, unrelated here.
Legionella-selective agar (eg, buffered charcoal yeast extract) — for Legionella pneumophila, which presents with pneumonia but not typical in CF exacerbations.
Salmonella-Shigella agar — for enteric pathogens from stool, not respiratory cultures.
Memory hook:
In CF, think “3 P’s”: Pseudomonas, Pandora’s box (many bugs), & Particularly Burkholderia — needs its own agar for detection.
Adult with community-acquired pneumonia (fever 39.4°C, focal R-lung infiltrate). Stem highlights immune response dominated by Th1, IFN-γ, and IL-2. Which pathogen fits?
Answer: Legionella pneumophila — facultative intracellular organism; clearance depends on Th1 → IFN-γ, IL-2–driven macrophage activation.
Why others are wrong (brief):
Streptococcus pneumoniae – extracellular pyogenic; neutrophil/Th17 response, not Th1-dominant.
Haemophilus influenzae – extracellular CAP; neutrophilic, not Th1-led.
Staphylococcus aureus – post-influenza/health-care–associated; extracellular.
Pseudomonas aeruginosa – structural lung disease, ventilators, CF; extracellular.
Memory hook:
Th1/IFN-γ → think intracellular CAP → Legionella.
A 68-year-old woman develops a vesicular rash localized to the right T4 dermatome that began 5 days ago and is now crusting. The rash does not cross the midline, and light touch to the area elicits severe pain. Which complication is she most at risk for?
Answer: Persistent pain in the affected region (postherpetic neuralgia).
Why others are wrong:
Disseminated rash: Possible mainly in immunocompromised; not the most likely in an otherwise healthy older adult.
Painful large-joint swelling: Not a herpes zoster complication.
Recurrent gross hematuria: Unrelated to VZV.
Glove-and-stocking sensory loss: Length-dependent peripheral neuropathy (e.g., diabetes), not dermatomal VZV.
Memory hook:
Dermatomal shingles in older adults → highest risk = postherpetic neuralgia.
A 16-year-old girl returns from a 2-week trip to Kenya and develops intermittent high fevers with chills and drenching sweats. Giemsa-stained peripheral blood smear confirms Plasmodium infection. Which event in the parasite life cycle directly causes her febrile episodes?
Correct Answer: E. Rupture of pathogen-infected erythrocytes
Fever spikes in malaria correspond to synchronous rupture of RBCs infected with Plasmodium species. This releases merozoites into the bloodstream, along with pyrogenic substances (e.g., hemozoin) that stimulate cytokine release (TNF-α, IL-1), producing chills and high fever.
Why others are wrong:
A. Circulation of sexual forms: Gametocytes circulate but don’t cause fever; they are important for transmission to mosquitoes.
B. Inoculation by vector: Occurs at initial infection, not linked to recurring fever spikes.
C. Invasion into hepatocytes: Asymptomatic liver stage (sporozoites → schizonts) precedes blood stage.
D. Toxin from lysed pathogens: Malaria symptoms are from host cytokine response to RBC rupture, not a secreted toxin.
Memory Hook:
Malaria fevers = Mass RBC rupture event → immune system “cytokine storm” → chills & sweats.