Epidemiology & Communicable Diseases
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
62 Terms
Purpose of Epidemiology
Epidemiology is the study of populations to:
Monitor the health of the population.
Identify the determinants of health and disease in communities.
Investigate and evaluate interventions to prevent disease and maintain health.
Seeks to describe, quantify, and determine occurrences of diseases.
Some Early Epidemiologists
James Lind: identified the effects of diet on disease
Florence Nightingale: monitor disease mortality during the Crimean War
Hippocrates: first epidemiologist
John Snow: descriptive study on cholera outbreak in London
Epidemiology is the…
Study of the distribution and factors that determine health-related states or events in a population.
Information is used to control health problems.
Epidemic
A disease occurrence that clearly exceeds the normal or expected frequency in a community or region.
Example: Small pox in Africa, monkey pox
Pandemic
A epidemic that progresses to worldwide distribution (HIV, bubonic plague, COVID-19).
Endemic
Always, present, manageable, does not disrupt society.
Example: Influenza (the flu), Malaria, Syphilis
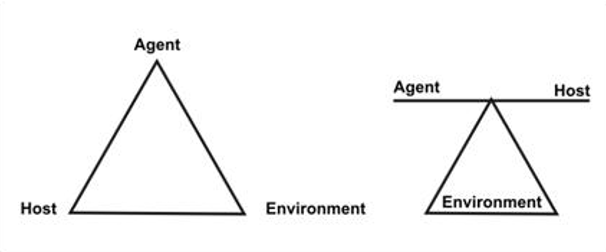
Epidemiologic Triangle
Host: Susceptible human or animal that carries the diseases.
Ex: demographics, immunity, disease history
Agent: A factor that causes or contributes to health problems.
Ex: virus, chemical, trauma
Environment: external factors that influence the host.
Ex: pollution, psychosocial environment, climate
Theories of Causality in Health and Illness
Causality is the relationship between a cause and its effect.
Chain of causation
Causation in noninfectious disease: such as cancer and diabetes: environmental exposure and potential health outcomes.
Multiple causations
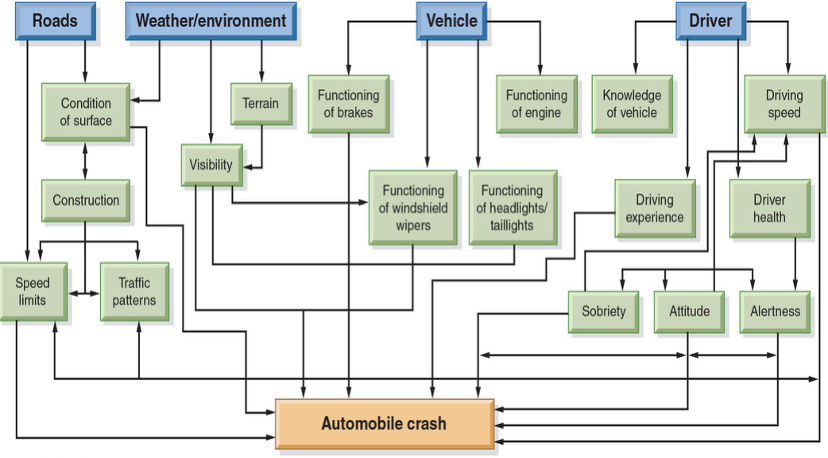
Web of Casuality
Web of Causality
Recognizes the complex interrelationships of many factors interacting, sometimes in subtle ways, to increase or decrease the risk for disease or event.
Relationships are sometimes mutual, with lines of causality going in both directions.
Encompasses multifactorial causes of health problems and issues.
Has been adapted to study the causation of both infectious and noninfectious diseases.
Immunity
A host’s ability to resist a particular infectious disease-causing agent.
Cross Immunity
Acquired from past exposure to a related pathogen or its antigens.
Ex: Protection against SARS-COV2 from past exposure to COVID-19; Small pox vaccine used to treat monkey pox.
Passive Immunity
Short term/temporary protection
Person is given antibodies
Ex: Newborn receives antibodies from mother; injection of snake venom.
Active Immunity
Long term protection
Can be acquired naturally/artificially
Ex: History of disease/vaccination
Herd Immunity
The resistance to the spread of a contagious disease within a population that results if a sufficiently high proportion of individuals are immune to the disease, especially through vaccination.
Immune people outnumber the susceptible people.
Level varies with diseases.
Depends on risk

Risk
Probability that a disease or unfavorable health condition will develop.
Directly influenced by biology, environment, lifestyle, and system of health care.
Risk Factors: negative influences.
Epidemiologists studying population at risk: collection of people among whom a health problem has the possibility of developing because certain influencing factors are present or absent or because there are modifiable risk factors.
Risk of disease name with or without risk factor 1:1 considered relative risk of 1.0.
Relative risk > 1.0 indicates greater likelihood of acquiring disease.
Relative risk of 2.5 means that exposed group is 2.5 time likely more to acquire the disease than the unexposed group.
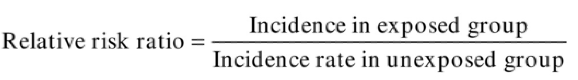
**Relative risk ratio = Incidence in exposed group / Incidence rate unexposed group**
Primary Prevention: Natural History of a Disease
Health Promotion & Education:
May include:
Nutrition counseling—diabetes
Sex education—pregnancy
Smoking cessation—lung cancer
Health Protection:
May include:
Improved housing and sanitation—waterborne diseases
Immunizations—communicable diseases
Removal of environmental hazards—accidents
Secondary Prevention: Natural History of a Disease
Early Diagnosis:
The third stage in the natural history of disease, the early pathogenesis or onset stage:
Screening programs—breast and testicular cancer, vision and hearing loss, hypertension, tuberculosis, diabetes.
Prompt Treatment:
Initiate prompt treatment.
Arrest progression.
Prevent associated disability,
Tertiary Prevention: Natural History of a Disease
Rehabilitation:
Reduce the extent and severity of a health problem to minimize disability.
Restore or preserve function.
Primary Prevention:
Health Promotion and Education:
Training for employment—homeless population.
Group treatment and rehabilitation—adolescent drug users.
Food, shelter, rest/sleep, exercise
Health Protection:
Health services
Immunization as needed
Sources of Information for Epidemiological Study
Existing Data:
Routinely collected data (census data, vital records, surveillance data)
Reportable diseases
Disease registries (e.g., ALS, Rapid Response Registry, WTC)
Surveillance systems (monitors diseases to develop and evaluate control strategies)
Environmental monitoring (hazards in the environment)
National Center for Health Statistics
Health Surveys
Centers for Disease Control and Prevention Reports
Informal Observational Studies:
Raises questions and suggests hypotheses for larger-scale investigations.
Scientific Studies:
Epidemiologic Studies
Descriptive Epidemiology
Person:
Race, sex, age, education, occupation, income, and marital status.
Place:
Examine geographical patterns.
Time:
Secular trends
Point epidemic
Cyclical time patterns (seasonal fluctuation; calendar events)
Non-simultaneous; event-related clusters
What is the goal of descriptive epidemiology?
Identify the cause of health problems and develop measures to prevent illness.
Observe and describe patterns of health-related conditions that occur naturally:
Data on Measles Immunizations
Counts:
# of deaths due to specific disease.
Time delay to gather data.
Rates:
Proportion of people with given health problem.
Total number of people is denominator.
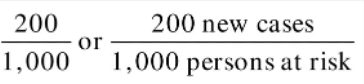
Rates: Incidence
Refers to all new cases of a disease or health condition appearing during a given time.
The numerator is all new cases, denominator population is at risk for a specific period of time.
**New Cases / Person at Risk**
Rates: Prevalence
All people with a particular health condition in a given population at a given point time.
Period prevalence rate: the prevalence rate over a defined period of time.
**Prevalence Rate = # of persons with a characteristic / Total number in population**
Analytic Epidemiology seeks to…+ Studies
Identify associations between a particular human disease or health problem and its possible causes.
Prevalence Studies:
Describes patterns of occurrence.
Same point in time and in same population.
Examines casual factors and based on inferences from a single examination.
Case-Control Studies:
Compares people who have health or illness condition (number of cases with the condition) with those who lack this condition (controls)
Retrospective—begins with the cases and looks back over time.
Cohort Studies:
Group of people who share a common experience in a specific time period (elderly, employees of specific industry)
Often used with environmental hazard exposures
The people are the focus of the study.
Casual Relationships
Cross-Sectional Study:
Explore health condition’s relation to other variables (broken window index).
Retrospective Study:
Looks backward into time to find casual relationships.
Uses existing data.
Prospective Study:
Looks forwards to find casual relationship
Cancer Prevention Study
Experimental Study:
Investigator control or changes factors suspected of causing the condition and observes results.
Used to confirm observational studies.
Applications of Epidemiology in Community-Oriented Nursing
Examples of Nursing Positions that Use Epidemiology:
Nurse epidemiologist
School nurses
Communicable disease nurse
Environmental risk communicators
Hospital infections control nurse
All nursing documentation on patient charrs is an important source of data for epidemiologic reviews
Global Impact
According to the WHO, three disease are responsible for all infectious diseases each year (approximately 5 million):
HIV/AIDS
TB
Malaria
COVID-19 in 2020~
National Impact
Infectious diseases of concern in the U.S:
Sexually transmitted diseases (including HIV)
Mosquito-borne illnesses (Zika and Dengue)
Whooping Cough
Hepatitis (A, B, C)
TB
Influenza and pneumonia (vaccinations)
Measles (vaccinations)
COVID-19 (EUA vaccines)
Emerging Infectious Diseases
Diseases in which the incidence has increased in the past several decades or has the potential to increase in the future.
Ebola virus
MRSA
HIV/AIDS
SARS-Corona Virus
Hantavirus (pulmonary syndrome)
Re-Emerging Infectious Diseases
Diseases that once were a major health problem globally or in a specific country and then declined, but are becoming significant health problems again:
TB
Malaria
Syphilis
Whooping Cough
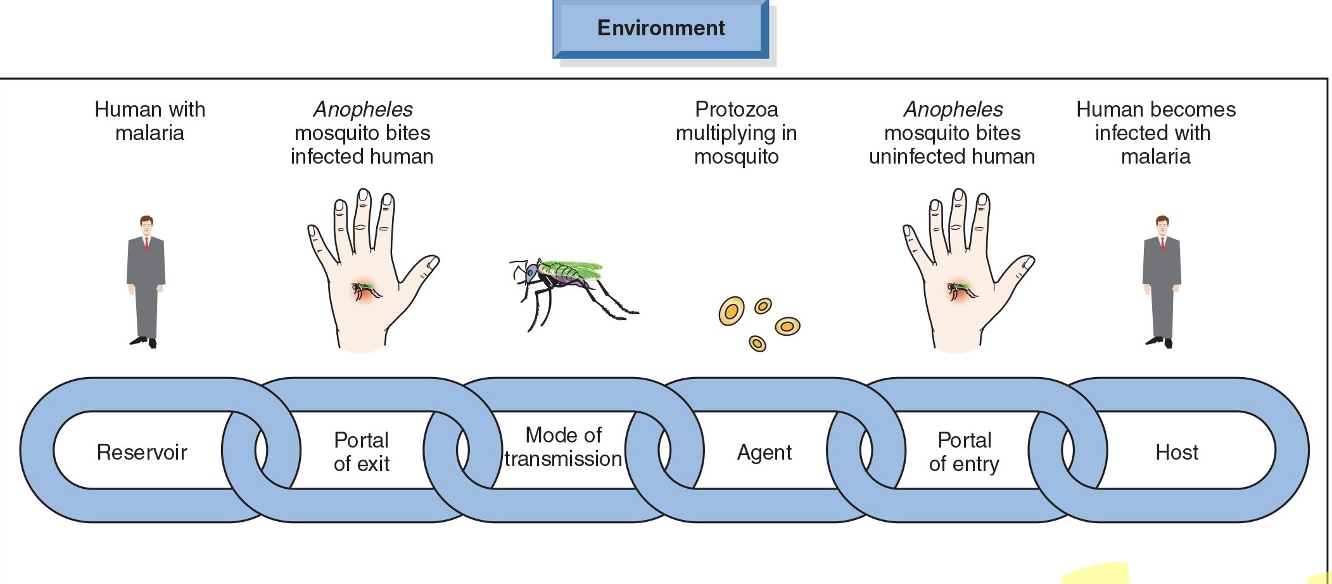
Mode of Transmission
Vertical Transmission:
Mother to child. (breastfeeding and utero)
Horizontal Transmission:
Direct: direct contact or droplets (coughing or sneezing)
Indirect: transmitted by fomites (insect, water, food, inanimate objects)
Vector-Borne Transmission:
Medical transmission—does not require infectious organisms to multiply
Biological transmission—requires an incubation period
Airborne Transmission:
Suspended in the air or cling to inanimate objects. (e.g., TB, flu)
Foodborne Diseases
Infection:
Results from bacterial, viral, or parasitic infection of food.
Examples: Salmonella, Shigella, E.coli (food poisoning)
Accompanied by an immune response with antibodies.
Intoxication:
Production of toxins from bacteria.
Example: Botulism
Commonly occurs when cooked food is left out or by a food preparer.
Toxins are difficult to identify.
Waterborne Diseases
An outbreak occurs if two or more persons experience a similar illness after consuming contaminated water.
Examples:
Hepatitis A
Cholera
Typhoid Fever
Bacterial Dysentery
Vector-Borne Diseases
Illness for which infectious agents are transmitted by a carrier (vector):
Lyme disease (tick)
Rocky Mountain spotted fever (tick)
Malaria (mosquitos)
Zika Virus (mosquitos)
Prevention and control of vector-born diseases:
Prevent exposure
Use repellants
Vector control
Zoonoses Disease
An infection transmitted from a vertebrate animal to a human.
Ex: Rabies
Parasitic Diseases
More prevalent in tropical climates and countries with inadequate prevention and control methods.
Intestinal parasitic infections.
Parasitic opportunistic infections
Healthcare Associated Infections
Infectious acquired during hospitalization or any health care setting.
May involve patient, health care workers, visitors.
Also called nosocomial infections, hospital-acquired infections
UTI, surgical infections, and pneumonia are the most common.
Bacteria: staph (blood), E.coli (UTI), enterococci (blood, UTI, wound), pseudomonas (all)
Universal Precautions.
HIV, Hepatitis, & Sexually Transmitted Diseases
Often acquired through behaviors that can be avoided or changed.
Nursing actions should focus on disease prevention.
Vaccine administration, early detection, or teaching clients about abstinence or safer sex.
Infected individual can transmit to others.
Factors Associated with Risk for STIs
Younger than 25 years
Member of a minority group
Residing in a urban setting
Being impoverished
Substance use
Unsafe sex practices
Women have higher risks of complications from STIs (PID, sterility, cancer)
Can be transmitted to neonate
Gonorrhea
Second most reportable notifiable disease.
Increasing (transmission or reporting).
Men have symptoms: drainage from penis.
Women: are often asymptomatic.
Antimicrobial resistance: cephalosporin with azithromycin or doxycycline.
Can be transmitted to neonates during delivery: opthalmic prophylactic agent.
Syphilis
3 Stages:
Primary (charce)
Secondary (rash, fever, sore throat)
Latent (tertiary syphilis associated with neurological changes)
Treatment: Penicillin
**don’t treat unless definitely possible.
Chlamydia
Most commonly reported STD.
Silent with serious complications.
Specific screening recommendations by the CDC.
Herpes Simplex Virus-2 (genital herpes)
No cure, but can control symptoms.
Human Papillomavirus Infection (HPV)
HPV vaccine
HIV/AIDS
No cure
Prevention, treatments, and care focuses on early testing.
Rapid testing.
Positive status can be controlled with medications.
Levels of Prevention: HIV/AIDS
Primary Prevention:
Use of condoms
Clean needle sharing
Universal precautions
Secondary Prevention:
HIV counseling and testing
Early diagnosis with rapid testing
Screen for co-morbidities
Tertiary Prevention:
Medication control
Education to prevent re-infection and reduce co-morbidities
STIs & Ethics
Access to healthcare
Routine testing
Legal implications for transmission
Confidentiality, privacy, stigma, and discrimination
Infected healthcare workers
Preventing STIs
Requires diverse and multidisciplinary interventions:
Parents, families, schools. religious organizations, health departments, community agencies, and media.
Educational programs provide adolescents with the knowledge and skills to:
Refrain from early onset of sexual intercourse.
Make informed decisions related to sexual behavior and health.
Increased the use of contraceptive measures.
Hepatitis A Virus
Transmitted through fecal-oral route.
Sources: water, food, or sexual contact.
Treatment: Inactivated Hep A vaccine administered in 2 doses.
Hepatitis B
Spread through the blood and body fluids; can survive at room temperature for at least 1-week.
Treatment: 3 doses of the vaccine.
Hepatitis C
Spread through blood or boy fluids.
Most common chronic blood-borne infection in the U.S.
Can be asymptomatic
Leading cause of chronic liver disease, end-stage liver disease, liver cancer, and liver transplants in the U.S.
Prevention: testing for people born between 1945 and 1965, IV drug abuser, organ transplant or blood donations before 1992, HIV/AIDS, liver, born to GCV+ mothers.
No vaccine, but there is a cure.
Tuberculosis
Spread by droplets
Poor nutrition, health status, and chronic disease can contribute to developing active disease.
Communicability depends on the length of exposure as well as proximity.
Incubation period: 10 to 12 weeks
Latent Phase: can last for many years
Active Phase: symptoms are evident such as cough, fatigue, loss of appetite, weight loss, and night sweats.
Chest x-ray shows infiltrate; positive for PPD
Control and elimination of TB
Screening can be detected through skin or blood test
Control and Elimination of TB
WHO characterizes TB burdens into 3 classifications:
Multidrug-resistant TB
Clients with HIV and TB
TB case management
Screening Tests:
Skin testing with purified protein derivative (PPD)
Two step testing
Interferon gamma release assays (IGRA)
Blood Test
For people who will not return for reading or BCG
Lack of adherence to medication (taken over 3 to 6 months)
Positive tests:
Followed up by chest radiography for persons with a positive skin reaction and pulmonary symptoms.
Isoniazid (INH) for those exposed and infected but no evidence of active disease.
Responds well to long-term treatment:
First Line Drugs: greatest activity against active bacteria
Second Line Drug
•Directly Observed Treatment (DOT)
Infectious Diseases of Bioterrorism
Anthrax:
Acute bacterial disease that affects mainly the skin (cutaneous or respiratory tract (inhalation)
Case Fatality: 5% to 20% for cutaneous; 100% for inhalation
Smallpox:
Variola virus transmitted person to person
Routine immunization not recommended
Risks associated with smallpox vaccination
Ring Vaccination Strategy
Nursing Process for Communicable Disease Control l
Assessment: Case identification, case finding, comprehensive, no assumptions, community’s need for surveillance or new or improved control programs
Planning: Assisting with immunizations, symptoms relief, controlling disease if present, limiting exposure, collaboration
Implementation: Service delivery, supervision of staff, primary prevention education for future infections, record keeping and reporting
Evaluation: What was the outcome? Did you get what you expected?
Communicable Diseases: CHN’s Role
Help with investigating reportable communicable diseases using a systematic approach.
Review information
Clarify disease is suspect or lab confirmed
Review case definition
Review disease information
Use specific questionnaires when available
At all levels of prevention, the nurse functions in the following roles:
Counselor
Educator
Advocate
Case manager
Primary care provider
Primary Prevention: Communicable Diseases
Education:
Use of mass media
Targeting meaningful health messages to aggregates.
Immunization:
Vaccine preventable diseases and schedules.
Assessing immunization status of community (possible barriers); planning and implementing immunization programs.
Adult immunizations.
Vaccine-Preventable Diseases
Routine recommended childhood immunizations includes:
Hepatitis A & B
Diphtheria
Pertussis
Measles, mumps, rubella (MMR)
Rotavirus
Polio
Haemophilus influenza
Meningococcal conjugate
Varicella (chickenpox)
Influenza (seasonal)
Human papillomavirus
Covid-19
Secondary & Tertiary Prevention: Communicable Diseases
Secondary Prevention:
Screening
Case and contact investigation; partner notification
Tertiary Prevention:
Isolation and quarantine:
Control transmission by health care workers
Safe handling and control of infectious wastes
Reporting Communicable Diseases
CDC and WHO offer guidelines for investigative procedures.
Diseases are reported to local health authorities, and initial point of contact is investigated.
Reportable diseases are reported to the State Health Department and then to CDC
Each state has a disease report form
Any outbreak
Unusual disease
Disease Reporting in Georgia
All physicians, laboratories and other health care professionals are required by law to report conditions listed under the Notifiable Disease Reporting Requirements.
Both laboratory and clinical diagnoses are reportable within specified time intervals.
Most diseases are reportable within 7 days.
Diseases that need to be reported immediately are done through a telephone call to the public health district.
Communicable Diseases: Ethical Issues
Health Care Access:
Cost
Enforced Compliance:
Direct observation therapy (DOT)
Confidentiality and Discrimination:
Partner notification