Veterinary Toxicology
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
30 Terms
Key Points in Managing Toxic Exposures
• Any substance has the potential to be toxic
• Treat the pet and not the poison
• If the pet is stressed or symptomatic, stabilize it first. Examination should be performed before decontamination
• The decontamination plan should be designed based on nature and amount of substance, number of substances involved, time and route of exposure, and the pet’s condition, signalment, and species
• Wear impermeable PPE
• Proper client education is crucial to poison prevention
Toxicologic History
Questions
1. Client Information?
2. Patient Information?
3. Clinical Status?
4. Agent Information? Bring the package!
5. Exposure Information?
6. Implemented treatment?
Triage
Baseline Patient Parameters
Weight (kg)
Mentation
Heart rate
Pulse rate and Quality
Respiratory rate
Respiratory effort
Mucous membrane color
Capillary refill time
Blood pressure
Decontamination
= The neutralization or removal of dangerous substances
Goal: minimize exposure by preventing absorption or enhancing elimination
Cases:
1. Oral Exposures
2. Dermal Exposures
3. Inhalant Exposures
4. Ocular Exposures
Oral Decontamination
1. Induction of Emesis
2. Rinsing and Dilutions
3. Activated Charcoal
4. Cathartics
5. Other GI Decontamination Techniques
◦ Enemas
◦ Gastric Lavage
◦ Endoscopy
INDUCTION OF EMESIS
When?
◦ Up to 90 minutes after exposure ideal, but may induce up to 4 hours post ingestion
◦ If animal has not vomited already
When not?
◦ Caustic/corrosive substances-—battery ingestion (acid), bleach, ammonia, fabric softener, potpourri
◦ Hydrocarbons (aka petroleum products) - aspiration risk, i.e., liquid fuels - kerosene, engine oil, tiki-torch fluid, gasoline
◦ If animal unable to control its airway: sedated, seizing, comatose
◦ Animals that can’t vomit
With what?
◦ Dogs? Cats?
Oral Decontamination: Emetics
CENTRALLY ACTING
Stimulates emetic center or CRTZ directly
Examples:
◦ Apomorphine (DOG)
◦ Xylazine (CAT)
LOCALLY ACTING
Stimulate GI tract directly → stimulates either CRTZ or emetic center
Examples:
◦ 3% Hydrogen Peroxide
Apomorphine
Mechanism? Stimulates dopamine receptors in CRTZ
Routes? IV, SQ, conjunctival sac (of the eye)
Which species? Dog
Reversal? Naloxone for sedation, but can’t reverse vomiting effect (you could give an antiemetic, though)
Xylazine
Mechanism? Stimulates alpha receptors in both CRTZ and Emetic Center
Which species? Cats
Contraindications? Avoid in patients in shock, cardiac/renal disease
Reversals? Yohimbine and Atipamezole
Hydrogen Peroxide (H₂O₂)
Mechanism? Bubbling against stomach lining, oxygen production → irritation/stretching → sends signals to emetic center → cause vomiting
Routes? Orally
Dose/Considerations?
• 0.5-1mL/lb (dogs only; not for use in cats) – (15mL =1 tbsp)
• A single dose should not exceed 45-50ml in dogs that exceed 100lbs
• If first dose doesn’t work in 10min, can give a second. Two doses maximum
• Must be “fresh” bottle (opened 3 months ago or less)
• Do not use in cats, can cause gastritis; dogs could also potentially get gastritis
“Mamey”
- We’re in Florida
- 5yo FS Golden Retriever presents shortly after owner saw him pick up a toad into his mouth; the owner took a photo of the toad
- PE: BAR, NSF except for hypersalivation
- We determine the toad was a Cane Toad (usually >4-6”inches in size)
- invasive species to Florida; native to South and Central America
- bufo toxicosis: toxic to most animals that bite them, also humans
◦ Enlarged glands behind the eyes secrete toxin
◦ Thick, creamy white, highly irritating substance: bufo toxin
◦ Other toads from the Bufo spp. also have this toxin
- In Mamey’s case: performed oral rinsing, since appears that p just mouthed the toad (just effects to oral cavity)
More on Bufotoxicosis:
Clinical signs/findings: variable; depends on how much toxin absorbed and dog’s size, systemic signs usually occur after few minutes
◦ Hyperemic gums, drooling, pawing at mouth, head shaking
◦ Vomit
◦ Seizures, ataxia
◦ Arrythmias, tachycardia, dyspnea, death
◦ Bufotoxin similar in effects to digoxin (cardiac glycoside): inhibits cardiac sodium-potassium-ATPase pump→potentially fatal cardiac arrhythmias
Oral Decontamination: RINSING and DILUTION
Rinsing: flushing mouth with water to remove/decrease toxin ingested/absorbed through mucous membranes
◦ May be used in: toad poisoning (ex: Cane Toad), topical insecticide ingestion
◦ Use large syringe, rinse attachment for sink- careful with aspiration, position at commissure of lips and direct water rostrally
◦ May need to rinse for 5-10 min with tepid water
Dilution: milk/plain yogurt to sooth irritation/create protective film
◦ May be used in:
◦ Detergents: soap, enzymatic cleaners, fabric softeners
◦ Corrosive substances: bleach, ammonia
◦ Acid or alkalis: batteries, some cleaning agents
When not to use?
• Not with vomiting, sedated, seizuring, or comatose patient
Oral Decontamination: ACTIVATED CHARCOAL (ie ToxiBan)
• Carbon that has been chemically treated to create small pores, which increases surface area for binding other substances - adsorbent
• Adsorbents allow other substances to adhere to their outer coating. This prevents absorption of toxic, irritating, or harmful molecules. Facilitates toxin elimination via feces
• Ensure hydration-—can cause hypernatremia
• Will make feces black
• May use for toxicities like acetaminophen and aspirin
When NOT to use it because it doesn’t bind the toxin:
◦ Acids and Alkalis, Alcohols and Glycols (ie Ethylene Glycol)
◦ Heavy metals (lead, iron), Hydrocarbons, Detergents, Salt/Paintball toxicosis
◦ And if patient cannot swallow, is sedated, seizuring, or comatose
Oral Decontamination
CATHARTICS
Enhance the elimination of toxins by moving things through the GI tract more quickly. Promote evacuation from the colon
Osmotic cathartics
◦ 70% sorbitol—commonly added to activated charcoal
Should not be administered to patients with diarrhea, dehydration, ileus, intestinal obstruction
FYI: to remind ourselves- Lactulose/Kristallose, PEG3350 (Miralax) are ex of cathartics
Oral/GI Decontamination
ENEMAS
Goal: Increase lower GI transit time
Potential adverse side effects: intestinal perforation, hypothermia, metabolic derangement
◦ Never use Fleet Enemas in cats-—phosphate in enema can cause metabolic abnormalities; can also affect dogs
GASTRIC LAVAGE
Goal: Remove toxic contents from stomach
Performed under general anesthesia
Potential adverse side effects: injury to mouth, throat, esophagus; hypothermia; aspiration pneumonia
ENDOSCOPY and GASTROTOMY
When?
• Coin ingestion (zinc: pennies minted after 1982 have high levels of zinc)
• Corrosive ingestion (batteries)
• Ingested toys
• Ingested gorilla glue
• Patients must be stable for anesthesia
Dermal Decontamination: BATHING AND GROOMING
Exposure: flea and tick topicals, oils, tars, tree sap, asphalt, glue traps
Goal: Prevent transdermal absorption and oral exposure via grooming
Dermal decontamination should take place in well-ventilated area, with PPE, protective eyewear, and respiratory protection (ie, surgical mask) depending on toxicant
Repeated bathing often needed
Methods:
• Liquid dish soap (NOT electric dishwashing soap): ex: greasy substances like herbicides, topical insecticides, glow sticks, essential oils
• Vegetable oils, butter, peanut butter followed by clipping shaving or combing for sticky materials:
ex: glue traps, tar, oil-based paint
• Copious rinsing with water: irritating/corrosive substances- ex: fabric softener sheets (unused, and potentially used), liquid potpourri, drain cleaners, gasoline
Methods:
• Brushing/vacuuming fur: dry substances- permethrin powders for dogs/cows sprinkled on a cat
• “Skunk off” mixtures for skunk spray: always bathe in well ventilated area away from heat sources/open flames; discard all unused mixture, do not store in closed container (mixture could generate pressure/explode if closed)
• Pets should not ingest substances used in dermal decontamination because can cause GI upset
Inhalant Decontamination
REMOVE and PROVIDE FRESH AIR
Exposures:
◦ Gases, smoke, toxic fumes, dusts, powders, and granules
◦ PTFE (Teflon), aerosols and ammonia: can adversely affect birds
◦ Burning/overheated Teflon: can cause acute death in birds
Goal: remove pet from inhaled substance and prevent re-exposure.
◦ O2 therapy for animals in respiratory distress
◦ Bronchodilator therapy
◦ Pepper spray, zinc/aluminum phosphide, phosphine gas are hazardous for staff-decontamination needs to happen outdoors
Exposure: Any substance not formulated for the eyes can cause irritation,
ulceration, blindness.
Goal: Remove substances from the eyes and reduce tissue damage
FLUSHING
◦ Sterile eye wash solution
◦ Repeated for 20-30 min
◦ No high-pressure sprays
◦ Follow with fluorescein staining
◦ Do NOT use VisineR or similar products: contains imidazoline; small amounts ingested can cause vomiting, ataxia, hypotension
Decontamination Drugs/Products
1. Apomorphine/Xylazine/Dexmedetomidine
2. Reversal Agents- Naloxone/Yohimbine/Atipamezole
2. 3% Hydrogen Peroxide
3. Sterile Eye Wash
4. Liquid Dishwashing Detergent and Shampoos
5. Activated Charcoal (with and without Sorbitol)
Therapeutic Drugs and Antidotes Used In Toxicology Cases
DRUGS
1. Acepromazine
2. Atropine
3. Atipamezole
4. Methocarbamol
5. Injectable B-blockers
6. Naloxone
7. Diazepam
8. Dextrose
9. SAMe
ANTIDOTES
1. Vitamin K1
2. N-Acetylcysteine
3. Pralidoxime (2PAM)
4. Fomepizole (4-MP)
5. Chelators: CaEDTA, Dimercaprol (BAL),
D- Penicillamine
6. Pamidronate
7. Digoxin Immune FAB
Drugs and Antidotes
Methocarbamol
• Centrally acting skeletal muscle relaxant
Used for: muscle tremors and rigidity
Exposures: permethrin, metaldehyde, tetanus, tremorgenic mycotoxins (from some moldy foods), hops, strychnine
Dantrolene
• Skeletal muscle relaxant; directly acts on mm, mechanism unknown
Use:
◦ Hops toxicosis in dogs
◦ Malignant hyperthermia: hypermetabolic disorder of skeletal mm causing dramatic rise in body temp and muscle contractures
◦ Can be triggered by stress, inhalant ax, hops toxicosis; can be fatal
◦ Most frequently seen in heavily muscled dogs like Greyhounds
◦ Can also be genetic; has been reported in Pointers, Greyhounds, Labrador Retrievers, Saint Bernards, Springer Spaniels, Bichon Frises, Golden Retrievers, and Border Collies
◦ Also seen in pigs
Phytonadione (Vitamin K1)
Use: Antidote for anticoagulant rodenticide toxicosis- anticoagulant rodenticides interfere with ability of the liver to recycle Vitamin K
◦ Vitamin K1 is needed for regeneration of Vitamin K1 dependent clotting factors (2, 7, 9, 10)
◦ Must be given for weeks (2-4 wks) until rodenticide eliminated
◦ Risk of anaphylaxis with IV use
◦ Oral formulation should be given with fatty meal to increase bioavailability
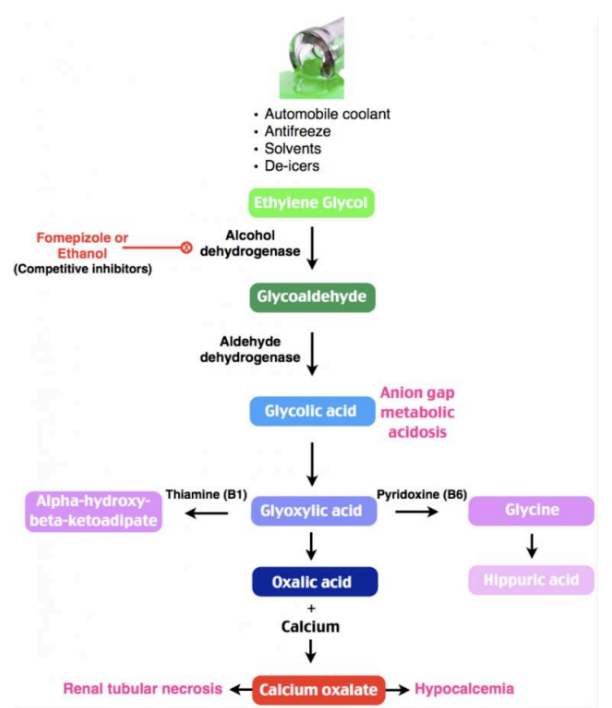
Fomepizole (4-MP)
Use: Antidote for ethylene glycol (ie antifreeze, de-icers, brake fluids)
Fomepizole inhibits alcohol dehydrogenase from metabolizing ethylene glycol:
◦ Specifically it prevents alcohol dehydrogenase from changing ethylene glycol into metabolites (oxalic acid) that cause renal failure and acidosis
Better than ethanol (vodka, Everclear) for treatment because does not cause CNS depression
Need to give within 3hr of exposure-cats, within 8hr of exposure-dogs
Acetylcysteine (Mucomyst, Acetadote)
Is a glutothione precursor and mucolytic (can be used in nebulization to break up mucus to be more easily coughed up)
◦ Glutathione is produced by hepatocytes; antioxidant involved in detoxification reactions in liver
◦ Required to protect hemoglobin and protects RBC’s against oxidative damage
Use: treats methemoglobinemia and liver damage associated with acetaminophen (Tylenol) toxicosis
Acetaminophen can cause liver damage (usually dogs) and decrease ability of RBC’s to carry oxygen (methemoglobinemia- usually cats). Cats are more sensitive to acetominophen
Acetylcysteine detoxifies reactive metabolites of acetaminophen so that they can be excreted
SAMe S-Adenosylmethionine (Denosyl)
Use: acetaminophen toxicosis, various hepatopathies
Nutraceutical that supports glutathione production for improved liver function
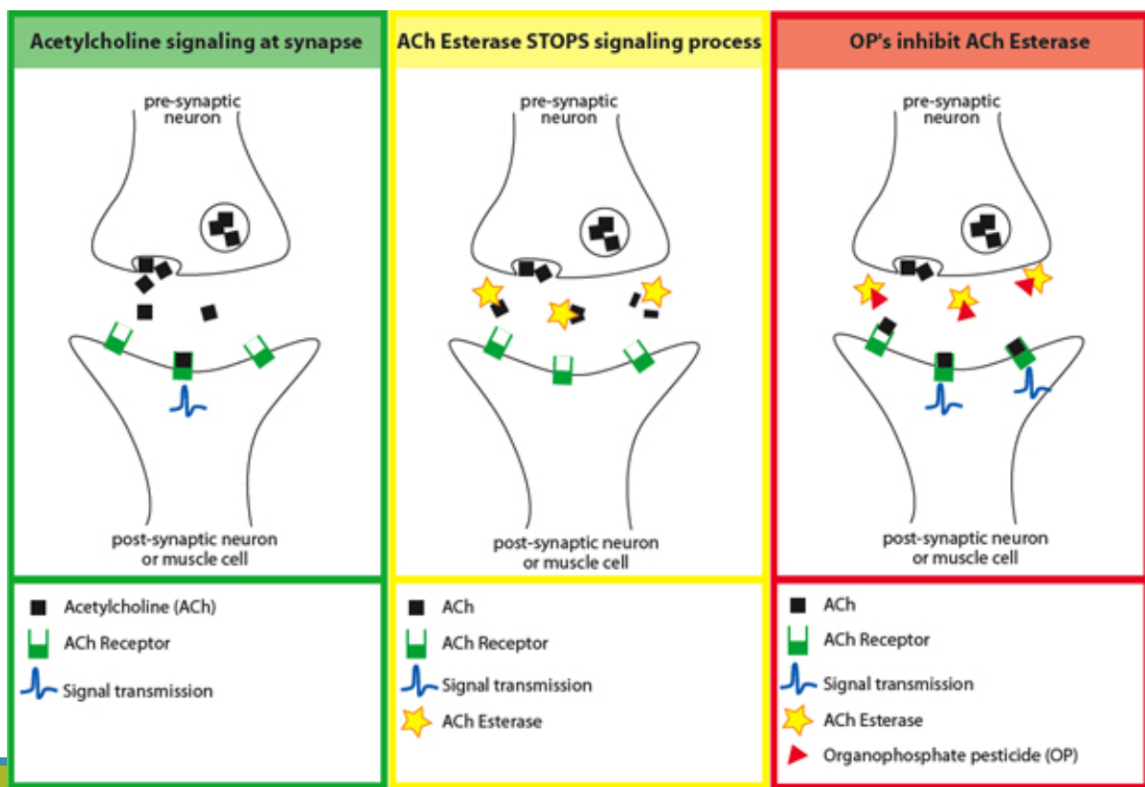
Pralidoxime (2PAM)
• Normally acetylcholinesterase breaks down acetylcholine
• Organophosphates inhibit acetylcholine from being broken down, so it persists→ increased skeletal muscle contractions/neurological signs
Use: Antidote to control nicotinic signs associated with organophosphate toxicosis: muscle tremors/ataxia which can lead to paralysis and hypoxia
• Knocks acetylcholinesterase inhibitor (organophosphates) off enzyme so acetylcholine can be broken down
• Only good when used immediately after exposure
• If organophosphate bond to acetylcholinesterase “ages”, no longer effective as antidote
• “ages”= when organophosphates irreversibly inhibit acetylcholinesterase
Pamidronate
Use: treatment of hypercalcemia from cholecalciferol rodenticide or Vitamin D toxicosis from psoriasis cremes or Vitamin D supplements
• Inhibits osteoclastic bone resorption therefore reversing hypercalcemia and hyperphosphatemia
“Calamansi”
-We’re working in a 24hr specialty hospital on ER shift, it is now early afternoon
-”Calamansi” is a 6yr MN Mixed Breed dog with no known health concerns, UTD on vaccinations, no meds.
-P presents because o is concerned that p may have ingested some pennies that were on the kitchen counter this morning. P looked like they tried to vomit once, but it was non productive.
-On exam: BAR, TPR NSF. Mucous membranes are pink with CRT <2, eupneic with normal RR and RE
-What are some concerns with the hx?
-What should we consider doing next?
-2v abdominal rads demonstrate multiple round, metal opacity objects in the stomach. No obstructive pattern or other abN noted in rest of GI tract or abdomen
-What are the next steps?
-CBC/chemistry panel in house: what are we looking for in relation to the hx and findings?
-We are concerned with Zinc toxicosis: pennies minted after 1982 contain large amounts of zinc
-Zinc toxicosis can cause hemolytic anemia: believes to damage and cause rupture of RBCs
-CBC: may see regenerative anemia, spherocytes, and Heinz bodies
◦ Regenerative anemia: see immature RBCs (reticulocytes)
◦ Spherocytes: indicate RBCs are being destroyed (loss of central pallor and normal disc shape of cell)
◦ Heinz bodies: denatured hemoglobin stuck to RBC that indicate oxidative damage
-Zinc toxicity can also damage kidneys, pancreas, liver, and abN may be present on chemistry panel
-Potential clinical signs of zinc toxicosis depend on how much ingested, how long has been in body:
◦ Initial phase: vomiting, diarrhea, anorexia, lethargy, gastric ulcers, melena (can develop within minutes to several hours or days)
◦ Second phase, when zinc leaching starts to cause clinical signs, may be several hours to days later: anemia, possible heart murmur, tachycardia, icterus, acute kidney and/or liver failure, pancreatitis, death
-What we did with Calamansi:
◦ CBC: no evidence of anemia or RBC damage, rest WNL
◦ Chemistry: WNL
-Internist performed endoscopy and scoped out the pennies. Luckily they were all minted in the 1970s!
-If these pennies were minted 1983 or after, given the p had no abN or clinical evidence of hemolytic
anemia, it would be recommended recheck a CBC/chem 2-3 days later to ensure no delayed effects
Endoscopic removal of penny from stomach: https://www.youtube.com/watch?v=8_okx3Nc5EM
Drugs and Antidotes
Chelators
Mechanism: Bind to heavy metals
Ex: CaEDTA
Other chelators:
Dimercaprol (BAL)
D- Penicillamine
Use:
-Lead toxicosis (paint, toys, sinkers for fishing)
-Zinc toxicosis (pennies minted after 1982, nuts/bolts, zinc oxide cremes, Zicam, multivitamins)
Work by decreasing metal concentrations in blood/tissues by increasing their water solubility and excretion in urine
Their use is controversial because they increase renal excretion of zinc, but also increase intestinal absorption
◦ No studies establishing efficacy
Digoxin Immune Fab (Digibind)
Use:
-Antidote for digoxin overdose
Cardiac glycoside drug that acts by inhibiting Na/K ATPase pump; may treat , promote cardiac muscle contraction, slow down heart rate
-Antidote for bufotoxin (Bufo toads- Ex Cane Toad)
-Antidote for ingestion of digitalis containing plants (Oleander, Foxglove)
Digitalis can cause arrythmias
-Digoxin Immune Fab contains antidigoxin antibodies that bind to digoxin or digoxin like-substances and inactivates them
Expensive, so reserved for life threatening cases
Toxicities: Rodenticides
1. Anticoagulant: affect liver’s ability to recycle Vitamin K causing coagulopathy
2. Bromethalin: disables ATP production causing neurologic signs
3. Cholecalciferol: causes hypercalcemia and hyperphosphatemia
4. Strychnine: blocks inhibitory neurotransmitters causing neurologic signs
5. Zinc Phosphide: produces toxic gas in stomach
6. Corn Gluten: causes dehydration and GI obstruction in rats and mice
Toxicities: Rodenticides
Anticoagulant Rodenticides
First generation
◦ Warfarin, dicoumarol, pindone, chlorphacinone, diphacinone, valone
Second Generation
◦ Bromediolone, brodifacoum, difenthialone
Mechanism
• Interfere with ability of liver to recycle Vitamin K
• Vitamin K necessary for production of the active forms of clotting factors II, VII, IX, X
• Takes 3-7 days for depletion of factors to occur
Clinical signs: Spontaneous bleeding, petechia, ecchymosis
Management
1. Induce emesis if < 4h since exposure
2. Give single dose of activated charcoal
3. Administer antidote: Vitamin K1 14-30 days
4. Monitor PT or PIVKA 48-72 h after stopping the Vitamin K
5. If actively bleeding FFP or whole blood
Bromethalin
Developed to kill anticoagulant resistant rodents
Is a neurotoxin, not an anticoagulant
Disables ATP production. Na+ builds up in cells- can’t be pumped out. Nerve cells swell and burst
Clinical signs: hindlimb weakness, ataxia, paresis, paralysis, CNS depression, cerebral edema, seizures, death
Management
1. Decontamination- emesis, activated charcoal
2. No antidote, manage supportively and symptomatically
Cholecalciferol (in d-Con)
One of most deadly rodenticides
Form of Vitamin D3
Metabolized to calcitriol causing severe hypercalcemia and hyperphosphatemia
Can lead to acute renal failure due to mineralization of kidneys within 2-3 days
Soft tissues/organs may start to calcify (dystrophic mineralization)
Clinical signs: may take 1-2 days before seen after exposure. Polyuria/polydipsia, vomiting, decreased appetite, weakness/lethargy
Management
1. Induce emesis and give multiple doses of activated charcoal since toxin undergoes enterohepatic recirculation
◦ Enterohepatic circulation: toxin enters bloodstream through GI tract, processed by liver, then is excreted back into small
intestine via bile from gall bladder
3. Monitor chemistry profile (BUN, Creat, Ca, Phosphorus)
4. Administer fluids (0.9% saline) -diuresis
5. Consider meds to promote calciuresis (furosemide,prednisone)
◦ Furosemide inhibits Ca+ reabsorption in loop of Henle
◦ Glucocorticoids increase Ca+ excretion via kidneys and decrease intestinal absorption
6. Pamidronate- to decrease blood calcium
Strychnine
Used to kill rodents and burrowing animals Extremely toxic to dogs and cats
Blocks glycine, an inhibitory neurotransmitter
Signs: Nerves fire rapidly resulting in violent muscle spasms, extensor rigidity. Death from respiratory mm failure → respiratory arrest
Clinical signs can be seen within 15min-2hrs following lethal dose
Management
1. Induce emesis and give activated charcoal before symptomatic if possible
2. Control of spasms and seizures: with methocarbamol, propofol/sedation, gas anesthesia
3. Offer intensive supportive care and fluids, quiet, dark room to avoid stimulation
Zinc Phosphide
Used to kill rats, mice, voles, moles, rabbits.
After ingestion reacts with acid in stomach→phosphine gas which can be inhaled/absorbed:
◦ oxidative damage to multiple organs, can cause liver and kidney failure
◦ Affects cellular energy production → cell death
Clinical signs: bloody vomit, garlicky or rotten smell to breath. Severe GI pain, ataxia, seizures, tremors, weakness. If inhaled can cause acute non cardiogenic pulmonary edema
May see signs within 4hrs
Management
1. Give antacids to neutralize stomach pH
2. Induce emesis with apomorphine- not hydrogen peroxide (may cause more phosphine gas production)
3. No antidote- supportive care: anticonvulsants, methocarbomol)
NB- Risk to medical staff!
• Phosphine gas coming from patient can affect personnel in room: GI, cardiac, neuro signs
• Ensure well ventilated room; prompt disposal of vomitus
Corn Gluten
Usually pellet or disc form
Corn gluten can cause GI obstruction and sodium chloride to dehydrate rats and mice
As per manufacturer eating large amounts of corn gluten in rats/mice → dehydration and GI obstruction → eventually death
In dogs and cats ingestion usually only causes GI upset, but if large amount ingested can cause dehydration or GI obstruction
Management
Treat symptomatically, treat dehydration and GI obstruction
Toxicities: Home and Garden
Ethylene Glycol
Found in antifreeze, de-icers, brake fluids
◦ Sweet taste
◦ Cats-1.5mL/kg, Dogs 6.6mL/kg
Mechanism:
◦ Ethylene glycol is oxidized by alcohol dehydrogenase in liver in multi-step process → oxalic acid → forms insoluble crystals in kidneys and brain-causing acute renal failure (ARF) and acidosis
Clinical signs:
◦ Stage 1: CNS depression, lethargy, polyuria/polydipsia, vomiting (1-12hrs post exposure)
◦ Stage 2: Initial clinical signs may fade (12-24hrs post exposure), tachycardia, tachypnea
◦ Stage 3: Neurological signs, ARF- oliguria → anuria → death (12-72hrs post exposure); cats sooner than dogs)
Management
1. Give Antidote-Fomepizole (4-MP) within 3-8 hrs
2. or Ethanol IV (vodka diluted with NaCl, Everclear) as alternative- but causes CNS depression
◦ Ethanol has high affinity for alcohol dehydrogenase, so it competes with ethylene glycol which slows its metabolism
3. Aggressive diuresis -ARF supportive care
Organophosphates (OG’s) and Carbamates:
insecticides, fertilizers, herbicides
Mechanism
◦ Acetylcholinesterase inhibitors found in insecticides, some OTC flea collars
◦ Inhibit acetylcholinesterase so that acetylcholine not broken down
◦ Blocking this enzyme causes overstimulation of muscarinic and nicotinic receptors by acetylcholine
Toxicity from ingested garden and insecticidal products common
Nicotinic signs-muscle tremors/ataxia, seizures, respiratory paralysis, death
Muscarinic signs- SLUDDE: salivation, lacrimation, urination, defecation, dyspnea, emesis
Antidotes/Tx for toxicity:
• 2PAM (Pralidoxime)-acetylcholinesterase reactivator
• Relieves nicotinic signs in OG’s by removing OG from acetylcholinesterase- not effective in carbamates because 2PAM doesn’t bind to carbamates
• Atropine (muscarinic antagonist): for both OG’s and carbamates
• +/- Diazepam: for seizures in carbamates
“Karaoke”
◦ 9 yr old MN DSH present to emergency hospital for seizuring, p is hyperthyroid and currently taking methimazole 2.5mg PO BID, recent bloodwork 2 weeks ago performed, thyroid and organ function stable. Received AM dose today, indoors only, lives with a dog.
◦ O explained to known exposure to poisons. She recently bought K9 Advantix II and applied it an hour ago to her dog, and then she saw Karaoke grooming her dog’s shoulder area because they are best friends
◦ Brief PE because of p status: temp: 103.3F, full body tremoring.
◦ What are your concerns?
-O shows you the package of K9 Advantix II:
What comes to mind with this product?
-Imidacloprid: neonicotinoid-kills fleas and lice
-Pyriproxyfen: insect growth regulator
-Permethrin: synthetic pyrethroid- kills/repels ticks, mosquitoes, flies...TOXIC TO CATS
What’s our approach to treating Karaoke?
-you were able to quickly place IV catheter
-administered IV methocarbamol to stop generalized tremors
-crucial step: once stable gently washed off remaining topical preventative with Dawn liquid soap/warm water and thoroughly dried p- why?
-placed on IV fluids
-monitor temp, monitor for further tremors, monitor BG- why?
-when hospitalized and going home consider nutritional support if p not eating well
-after tremors controlled may send home with oral methocarbamol
-client education
Toxicities: Home and Garden
Permethrin
Synthetic pyrethroid- neurotoxins that interfere with neuronal sodium channels in parasite. But also causes these effects in cats- toxic in cats
Exposure often when owners use OTC dog flea and tick products on cats
Clinical Signs:
Generalized tremors, seizures, muscle fasciculations, dyspnea, hypersalivation, hyperthermia, ataxia, hyperesthesia, death
◦ BUT flumethrin (Seresto Collar for CATS) safe in cats
Management
1. Bathe cat to decontaminate
2. Manage tremors with methocarbamol
3. Sedatives/anticonvulsants PRN
◦ methocarbamol IV, phenobarbital IV,
benzodiazepines IV, general gas ax
4.Fluid therapy to reduce temperature and provide hydration support
Pyrethrin/Pyrethroid Toxicity
*Pyrethrin: recall at low, “cat safe” doses these can technically be safe to cats, but at high concentrations is TOXIC TO CATS- so do not use pyrethrin for dogs on cats
*Pyrethroids (synthetic pyrethrins), including permethrin: always TOXIC TO CATS (except flumethrin which is ingredients in Seresto Collar for CATS)
Toxicities: Home and Garden
Metaldehyde (molluscicide)
In slug and snail baits (sweet taste because may contain molasses), camping fuels
Mechanism:
◦ Converted to acetaldehyde which is toxic to pets
◦ Likely alters action of GABA, serotonin and norepinephrine in brain
Signs:
◦ 30 minutes post exposure- tachycardia, nystagmus, ataxia, seizures, dyspnea, cyanosis, uncontrolled hyperthermia, and multi-organ failure
Management:
1. No antidote
2. Induce emesis if not seizuring
3. Control muscular tremors and seizures with methocarbamol and benzodiazepines
4. Supportive care: IV fluids
Petroleum based hydrocarbons
• Gasoline, oil, kerosene, diesel
Aromatic hydrocarbons
• Quick drying paints, lacquers
Clinical Signs:
• Oral burns, blisters, coughing, aspiration- chemical pneumonia, fever, hypoxia
• Inhalation can severely irritate lungs
• Salivation, vomiting, abdominal pain, arrythmias
• Seizures, coma, death
• In ruminants: aspiration/pulmonary damage can occur from ruminal eructation, acute bloat, decreased rumen motility, anorexia
• Ex: Accidental exposure from farm equipment contaminated with crude oil
Management:
1. Emesis and gastric lavage contraindicated because of high aspiration risk
2. Activated charcoal not effective
3. Tx: supportive
Essential Oils (volatile oils-meaning they vaporize readily)
Sources: insecticides, aromatherapy, herbal remedies, personal care products, potpourri, essential oil diffusers
Easily inhaled and can be absorbed via skin
• ie wintergreen, tea tree oil, citrus oil, pine oil, peppermint oil, cinnamon oil, eucalyptus oil etc
• Cats very sensitive due to inability to metabolize phenol and phenolic compounds in liver
• Some are toxic to dogs; best strategy: keep away from pets
Signs: drooling, vomiting , tremors, ataxia, respiratory distress, liver failure, depending on oil
It is recommended to avoid essential oils on/in/around pets
Zinc
Sources:
◦ Galvanized bird cages
◦ Coin ingestion (pennies made after 1982- 97% zinc), hardware
◦ Zinc oxide ointments and sunscreen
Mechanism:
◦ Causes oxidative damage to RBC’s →hemolytic anemia
Clinical signs:
◦ Hemolytic anemia, vomiting, death in dogs and cats. (Ddx: IMHA)
◦ Birds: sudden death possible, lethargy, neuro signs, weight loss with chronic exposure
Management:
1. Rapid removal of object- endoscopy, surgical removal
2. Supportive care: ex: IV fluids
3. +/-Blood transfusions
4. Chelators (controversial if should be used): CaEDTA, D-Penicillamine, Dimercaprol
STRONG ACIDS (CORROSIVES)
Ex: Car batteries, toilet bowel cleaners, pool chemicals, (cationic detergents especially corrosive ie Roccal)
Clinical Signs: necrosis of tissues and mucosal burns- difficulty swallowing, corneal ulcers, pulmonary irritation
ALKALIS
Ex: Alkaline batteries, drain openers, dishwashing detergents
Clinical Signs: Same as acids
Management for both acids and alkalis
◦ Dilution with milk orally
◦ May take radiographs if battery ingested
◦ Sucralfate, feeding tubes, endoscopy to remove batteries
◦ Gentle flushing eye, fluorescein staining
◦ Do not: perform gastric lavage or induce vomiting- can corrode esophagus on the way back out
◦ Do not: administer activated charcoal- ineffective, can mask oral lesions
Toxicities: Plants
Lilies (Lilium spp.)
***This group does not include Peace Lily or Calla Lily –they are not true lilies— Peace and Calla Lilly just cause GI signs/oral irritation
Lillium spp. are nephrotoxic in cats
◦ Contain insoluble calcium oxalate crystals
◦ All plant parts toxic (including pollen!)
Clinical signs:
◦ Acute vomiting, anorexia, depression.
◦ Acute elevation in BUN, creatinine, phosphorus
◦ Acute renal failure from renal tubular necrosis
Treatment:
◦ Decontamination, fluid diuresis
Poinsettia (Euphorbia pulcherrima)
Mechanism:
◦ Mild irritant
◦ Leaves contain irritating sap.
Clinical signs:
◦ Salivation, vomiting, anorexia
◦ Self-limiting signs requiring minimal to no treatment
◦ NPO for several hours after ingestion may help with GI irritation to allow GI tract to “calm”
Dieffenbachia, Philodendron
Leaves contain insoluble calcium oxalates
Cause oral irritation when eaten: needle like crystals are released penetrating the oral mucosa, possibly esophagus and stomach
Clinical signs: Irritation and swelling of mouth, lips, and gums Also salivation, difficulty swallowing, vomiting
Management: Self limiting; if pronounced, may use dilution with milk to sooth; in severe cases soft food, pain medications
Hops (Humulus lupulus)
Hops contain essential oils, phenolic compounds, and resins
Spent/used hops (after beer brewing) consumed by dogs leading to toxicity
Mechanism unknown
Clinical signs/findings:
◦ Tremors, seizures, possible death
◦ Creatine kinase levels markedly elevated on chemistry
◦ Temperatures >105F-malignant hyperthermia (uncontrollable rise in body temp that can be fatal)
Management:
◦ Decontamination- emesis, Activated Charcoal
◦ IV fluids and supportive care
◦ Cooling: cool water on foot pads, fan
◦ Methocarbamol, Dantrolene for muscle relaxation
◦ Monitor for:
◦ DIC (disseminated intravascular coagulation)
◦ Rhabdomyolysis (muscle tissue breakdown → release of protein myoglobin into bloodstream → damage to kidneys)
Marijuana (Cannabinoids)
◦ Cat/dog eats stash of marijuana (gummies, brownies, candy, etc); secondhand smoke also possible
◦ Marijuana aka “Cannabis” (species-Cannabis sativa) =dried leaves, seeds, stems of plant
◦ Cannabinoids: compounds in marijuana
◦ THC and cannabidiol (CBD)
◦ THC: causes psychotropic effects (affects mental state) with toxicity to cats and dogs
◦ CBD: non-psychotropic; felt by many investigators to be non-toxic or have limited toxicity; early research suggests MAY help pets with anxiety, chronic pain, and seizures
◦ N.B: Hemp is same species of plant as Cannabis. Unlike Cannabis, hemp contains very low levels of THC; it contains higher levels of CBD
Clinical signs:
◦ 30-60 minutes after eating (sooner if inhaled) – may last for >24h
◦ Ataxia
◦ Lack of energy
◦ Dilated pupils
◦ Urinary incontinence, vomiting, tremors
◦ Vocalization
◦ Bradycardia, tachycardia, hypotension
◦ (Ddx: ethylene glycol or alcohol toxicosis), anything that causes CNS depression
Management:
◦ Induce emesis if hasn’t vomited already
◦ Activated charcoal: may need more than one dose
◦ IV fluids, anti seizure meds, anti emetics
Toxicities: Foods (and Drink)
Xylitol
◦ Sugar alcohol (used as a sweetener)
◦ Found in gum, candy, dental sprays, lozenges, toothpaste, diabetic products, vitamins, some peanut butters
◦ May be ingredient in gabapentin liquid formulated for humans
Mechanism of toxicity
• Metabolized to D-xylulose which regulates insulin release
• Large amount of insulin released from pancreas in response to this sweetener in dog
• Dogs- only species affected
Clinical signs: hypoglycemia, vomiting, lethargy, ataxia, seizures, liver failure
Management:
1. Induce emesis
2. Monitor BG levels and liver enzymes
3. Give dextrose as needed to treat hypoglycemia
◦ NEVER give dextrose or dextrose containing fluids SQ (can lead to necrosis).
4. Give hepatosupportive drugs/Tx
◦ SAMe
◦ Silymarin (Milk Thistle)
◦ IV Fluids
Grapes, Raisins, Tamarinds, Cream of Tartar, and Zante Currants
Mechanism of toxicity: dogs primarily affected
◦ Contain tartaric acid → accumulates in kidneys → damage
◦ Tartaric acid content varies, resulting in variable effects following ingestion
◦ Cream of Tartar contains tartaric acid (sometimes ingredient in play dough); also toxic to dogs
Clinical signs:
◦ Vomiting, lethargy, anorexia 12-15 hr post ingestion
◦ Acute renal failure – dogs primary species affected (anecdotal reports of toxicity in cats and ferrets)
Management:
1. Induce emesis
2. Activated charcoal: efficacy unknown
3. Monitor renal values, consider IV fluid diuresis
◦ In general, more than one grape or raisin per 4.5 kg (10 pounds) of body weight may contain enough tartaric acid to pose a risk for renal effects in dogs
◦ With ingestion of a large quantity or in cases in which diarrhea spontaneously develops within 12 hours after ingestion, rec aggressive IV fluid therapy and monitor renal function
Onions, Garlic, Leeks, Scallions, Shallots, Chives
◦ Allium spp. (raw, cooked, or dehydrated)
Mechanism:
◦ Crushing or chewing releases Allicin which is metabolized to sulfur compounds.
◦ Sulfur compounds cause oxidative damage to RBCs- Heinz body anemia (a type of hemolytic anemia), methemoglobinemia
◦ Cats very sensitive, but also affects dogs
Clinical signs:
◦ Lethargy, anorexia, vomiting, anemia, icterus possible from RBC breakdown
Management:
1. Induce emesis
2. Activated charcoal
3. O2, blood transfusions
4. Control of GI signs
Macadamia Nuts
Mechanism:
◦ Unknown
◦ Dogs only
Clinical signs: weakness, ataxia, stiffness rear limbs, tremors, vomiting; usually seen within 12 hrs
Management:
1. Induce emesis
2. Supportive care
3. Good prognosis
Alcohol (Ethanol)
◦ Alcoholic beverages, medications, raw yeast bread dough
◦ Hand sanitizer, after shave, perfume, mouthwash
Clinical signs:
◦ Can be lethal
◦ Ataxia, decreased reflexes, smell of alcohol on breath
◦ Depression, respiratory failure, arrythmias, tachycardia, hypotension, hypothermia, seizures, metabolic acidosis
Management:
◦ Induce emesis if conscious
◦ IV fluids, cardiovascular support, manage acidosis
◦ Monitor for aspiration; with CNS depression gag reflex may be affected
“Batik”
-4yo MN English Bulldog presented for gastric distention and retching after
eating raw bread dough 1 hour ago
-PE: tachycardia (HR=170BPM), moderately distended abdomen, non
productive retching
-What are the concerns with ingesting raw bread dough?
-What diagnostics could we do?
-Bloodwork (in house CBC/chem): WNL
-2v abdominal radiographs: severe abdominal distention, stomach filled with
ingesta, no GDV or obstructive pattern
-What’s the plan?
Toxicities: Foods
Raw Yeast Bread Dough
Toxic ingredients/properties:
◦ Ethanol produced as yeast is metabolized
◦ Potential as a foreign body as yeast expands (CO2 gas)
Clinical Signs/Findings:
◦ Retching to vomit, gastric distension, foreign body, GDV, rupture
◦ ataxia, lethargy
◦ Can be lethal
◦ Ataxia, smell of alcohol on breath
◦ Depression, respiratory failure, arrythmias, tachycardia, hypotension, hypothermia, seizures, metabolic acidosis
Management:
1. Be cautious with emesis
◦ Stomach could rupture if dough blocks esophageal sphincter (dough rising and carbon dioxide may expand/stretch stomach)
2. Cold water, gastric lavage, surgical removal
3. Stabilize alcohol toxicity: Manage acidosis, arrythmias, offer fluid support
Avocados
Toxic ingredient
◦ Persin
◦ Unknown mechanism of intoxication
◦ Skin, seeds, leaves most toxic, but also fruit; don’t forget: seed could act as foreign body
Species affected:
• Birds: extremely susceptible to Persin
• Cattle, goats, sheep, mice, rats, rabbits
• Dogs/cats rarely affected (aside from foreign body possibility, potential GI upset)
Clinical signs: (Birds)- 12hr to onset
-Inability to perch, anorexia, lethargy
-Dyspnea
-Organ failure (including myocardial necrosis), sudden death
Clinical signs for other species
If they eat enough-cattle, sheep horses, goats, rats, rabbits:
-Mastitis, agalactia, curdled milk, hard mammary glands, edema of the body, weakness, respiratory distress, cardiac arrythmias
Treat symptomatically: NSAIDs for mastitis, address cardiac abN
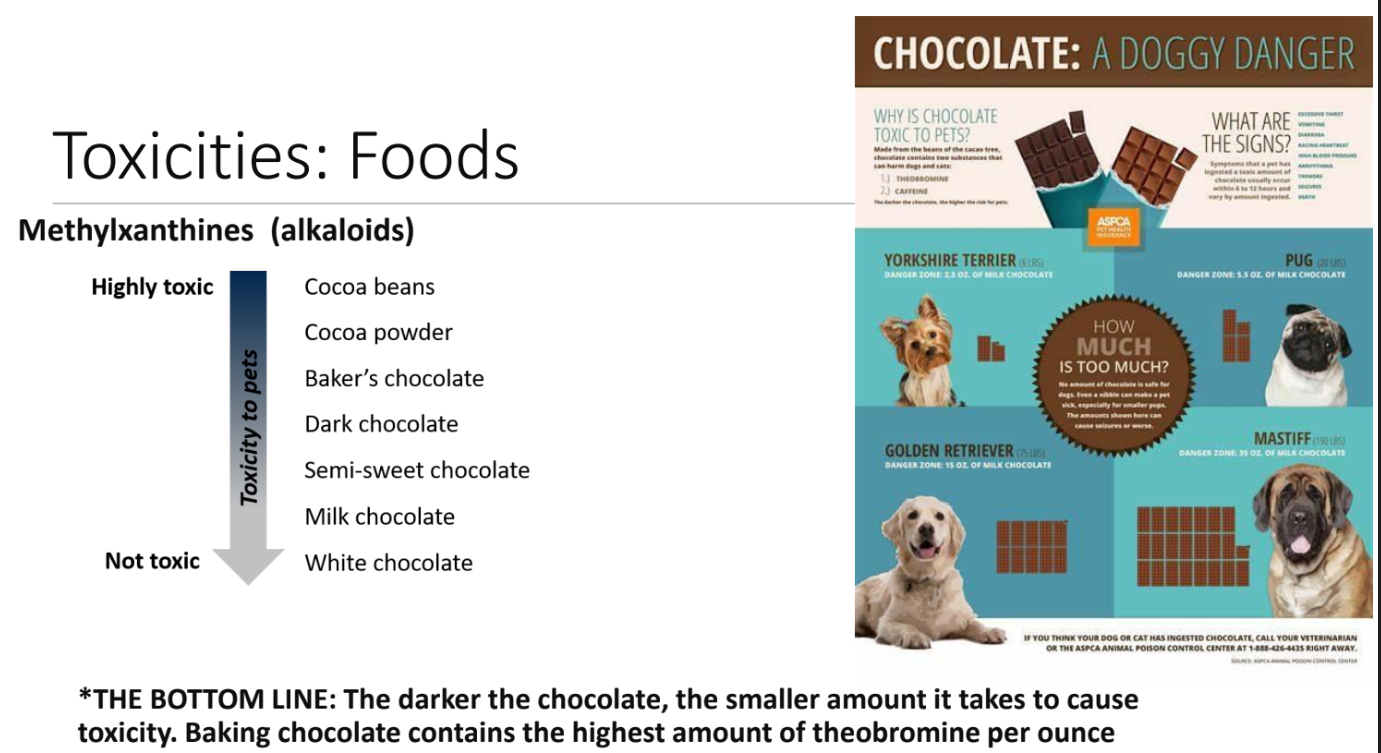
Methylxanthines (alkaloids) Chocolate
Sources of methylxanthines:
◦ Theobromines: milk and dark chocolate, cocoa powder, cocoa bean mulches
◦ Caffeine: tea, coffee beans, caffeine pills, commercial beverages, chocolate
Mechanism:
◦ Poorly understood
Clinical signs: Vomiting , diarrhea, pancreatitis, hyperactivity, tachycardia, hyperthermia, cardiac arrythmias, seizures; usually start 6-12hrs after ingestion; death can occur if left untreated (4days)
Management:
1. Induce emesis; concretions of chocolate may need gastric lavage
2. Activated charcoal- multiple doses because of enterohepatic recirculation
3. Manage arrhythmias- B- blockers
4. Seizures and tremor management with methocarbamol, diazepam, phenobarbital
Theobromine and caffeine each have LD50 of 100 to 200 mg/kg in dogs (no established values in cats; suspected to be lower)
◦ Lethal dose (LD50) is amount of an ingested substance that kills 50 percent of a test sample
◦ Severe, life-threatening clinical signs may be seen well below this dose
Based on ASPCA Animal Poison Control Center experience:
◦ Mild signs occur in animals ingesting 20 mg/kg of theobromine and caffeine
◦ Severe signs are seen at 40-50 mg/kg
◦ Seizures occur at 60 mg/kg
To put this in perspective, for a medium-sized dog weighing 50 pounds to potentially show signs of toxicosis:
◦ Would only need to eat 1 ounce of baker's chocolate (usually that means one square)!
◦ Would need to eat 9 ounces of milk chocolate
◦ For many dogs, ingesting small amounts of milk chocolate is not harmful
•WHITE CHOCOLATE: barely poses any threat of poisoning with only 0.25 mg of theobromine per ounce
• But can still get sick from all the fat and sugar, which can cause pancreatitis in dogs
•CAROB: not toxic to dogs or cats
• is a legume
Toxicities: OTC Medications
Acetaminophen (Tylenol):
Mechanism
Cats: very sensitive to acetaminophen; it causes methemoglobinemia and Heinz body formation (hemolytic anemia possible), hepatotoxicity
◦ Methemoglobinemia: excessive methemoglobin, a form of hemoglobin, which inhibits the ability of RBCs to deliver O2 to organs
Dogs: can also cause hepatotoxicity, and at high doses methemoglobinemia
Clinical signs of methemoglobinemia:
◦ chocolate brown blood and mm, depression, weakness, hyperventilation, cyanosis, death
Signs of hepatotoxicity:
◦ vomiting, anorexia, depression, abdominal pain, icterus, death
Management:
1. Induce emesis, activated charcoal, stabilization including O2 therapy and blood transfusions
2. N-acetylcysteine (Mucomyst, Acetadote)
3. Prevention of liver damage- SAMe
Salicylate Toxicosis
Sources: Aspirin, Pepto Bismol, sulfasalazine, Kaopectate, Ben Gay, Icy Hot
Mechanism:
◦ COX inhibition
◦ Toxic to cats (and dogs with higher doses)
◦ Cats do not have glucuronyl transferase- cannot metabolize well in liver
Clinical signs:
◦ GI ulceration, coagulopathies, liver necrosis; rare: renal failure (can inhibit blood flow to kidneys)
Management:
1. Induce emesis, activated charcoal
2. GI protectants (H2 blockers, proton pump inhibitors, +/-misoprostol in high- risk p for ulcers, but misoprostol has side effects)
3. IV fluids