Ocular Disorders: Orbits, Lids, and Lacrimal Apparatus
1/110
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
111 Terms
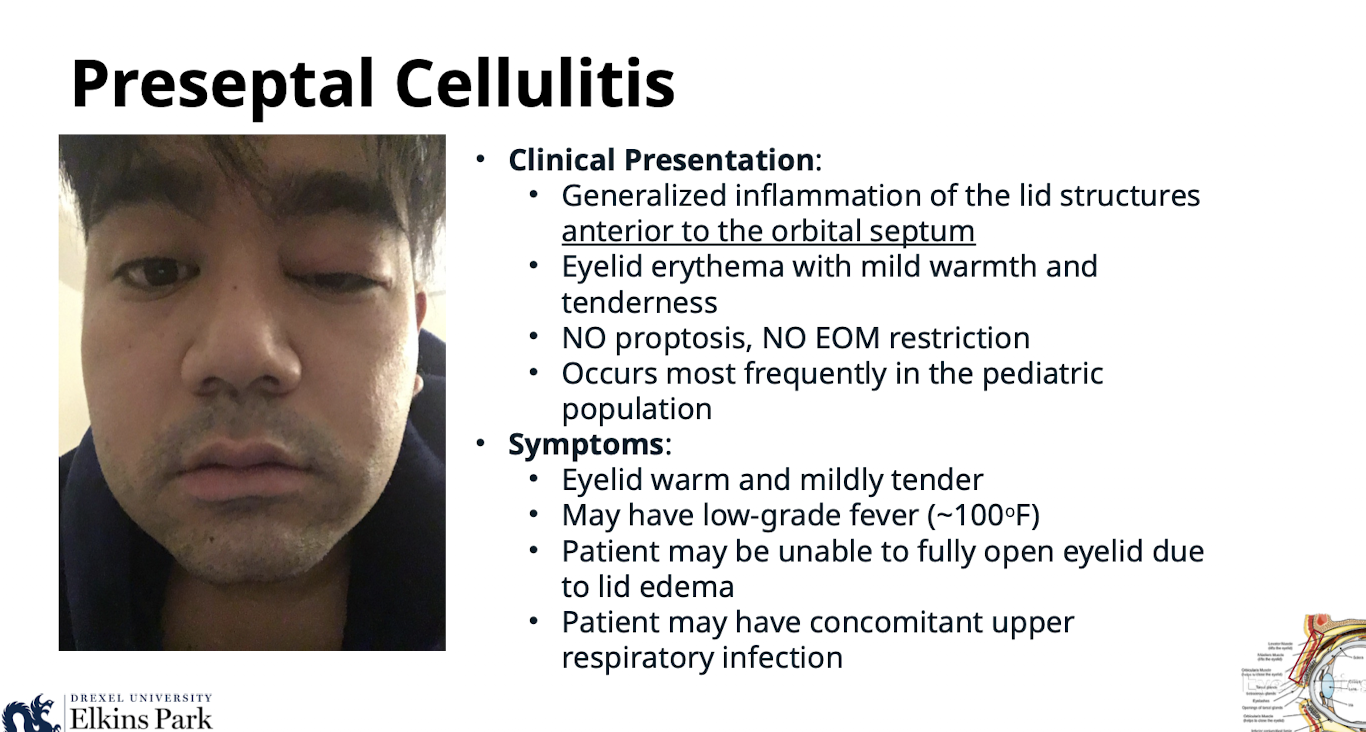
What is the clinical presentation of Preseptal Cellulitis?
Generalized inflammation of the lid structures anterior to the orbital septum; eyelid erythema with mild warmth and tenderness; NO proptosis; NO EOM restriction
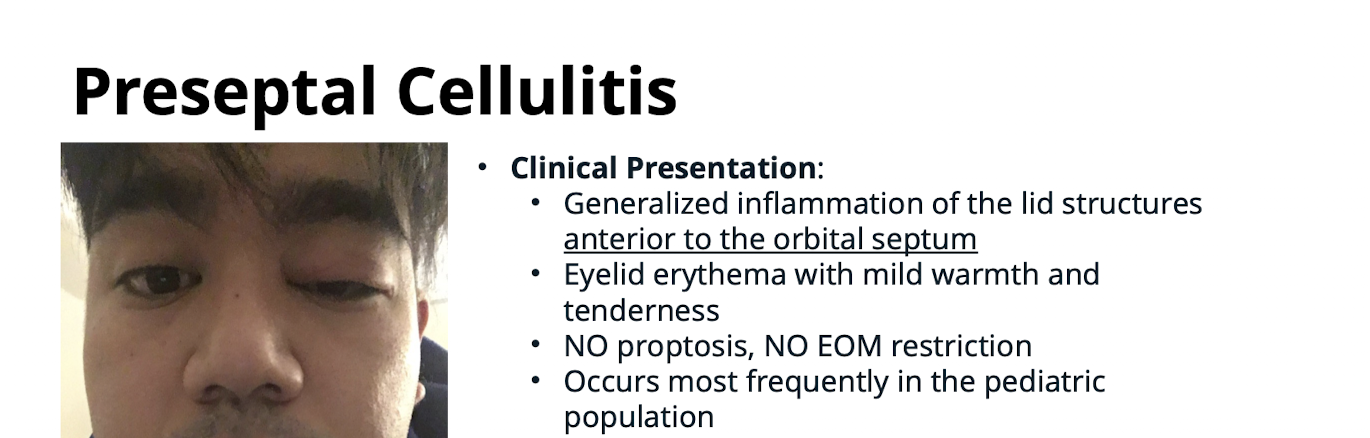
In which population does Preseptal Cellulitis occur most frequently?
The pediatric population
What are the symptoms associated with Preseptal Cellulitis?
Eyelid warm and mildly tender; may have low-grade fever (~100oF
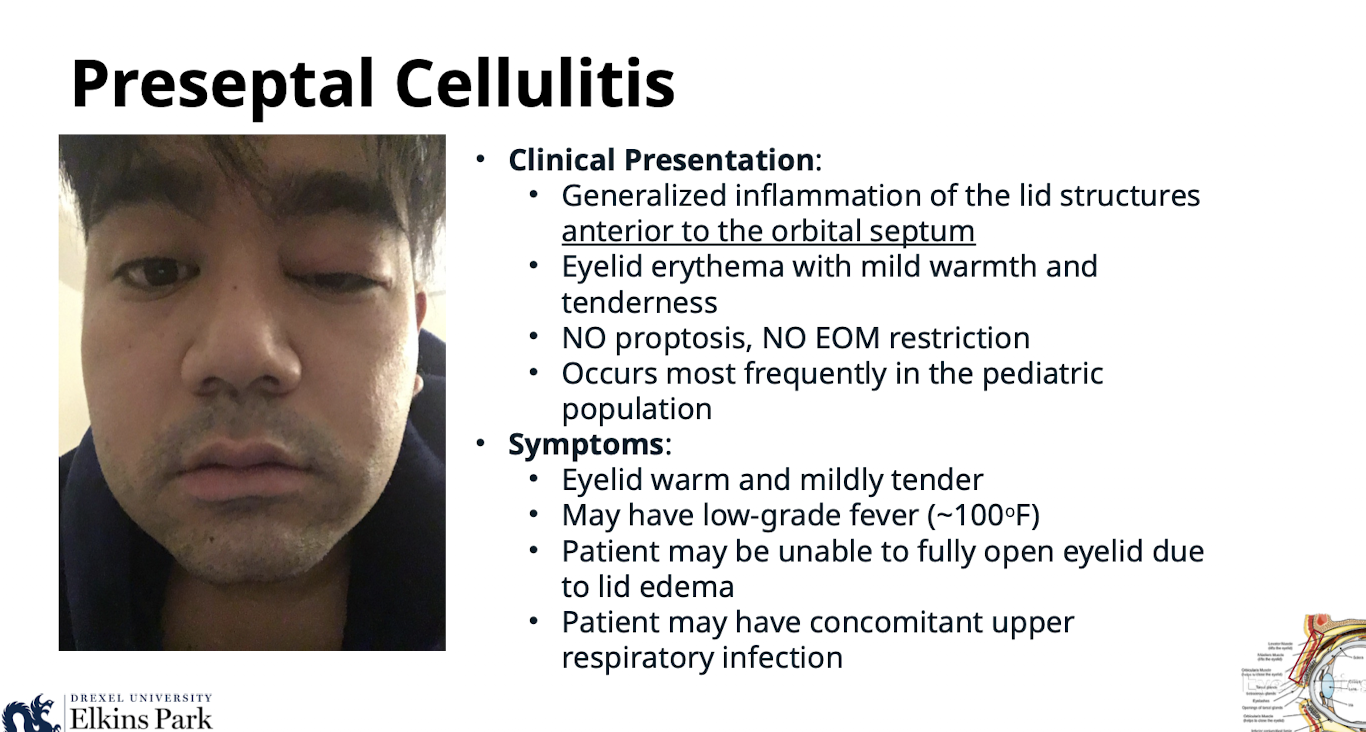
Why might a patient be unable to fully open the eyelid with Preseptal Cellulitis?
Due to lid edema
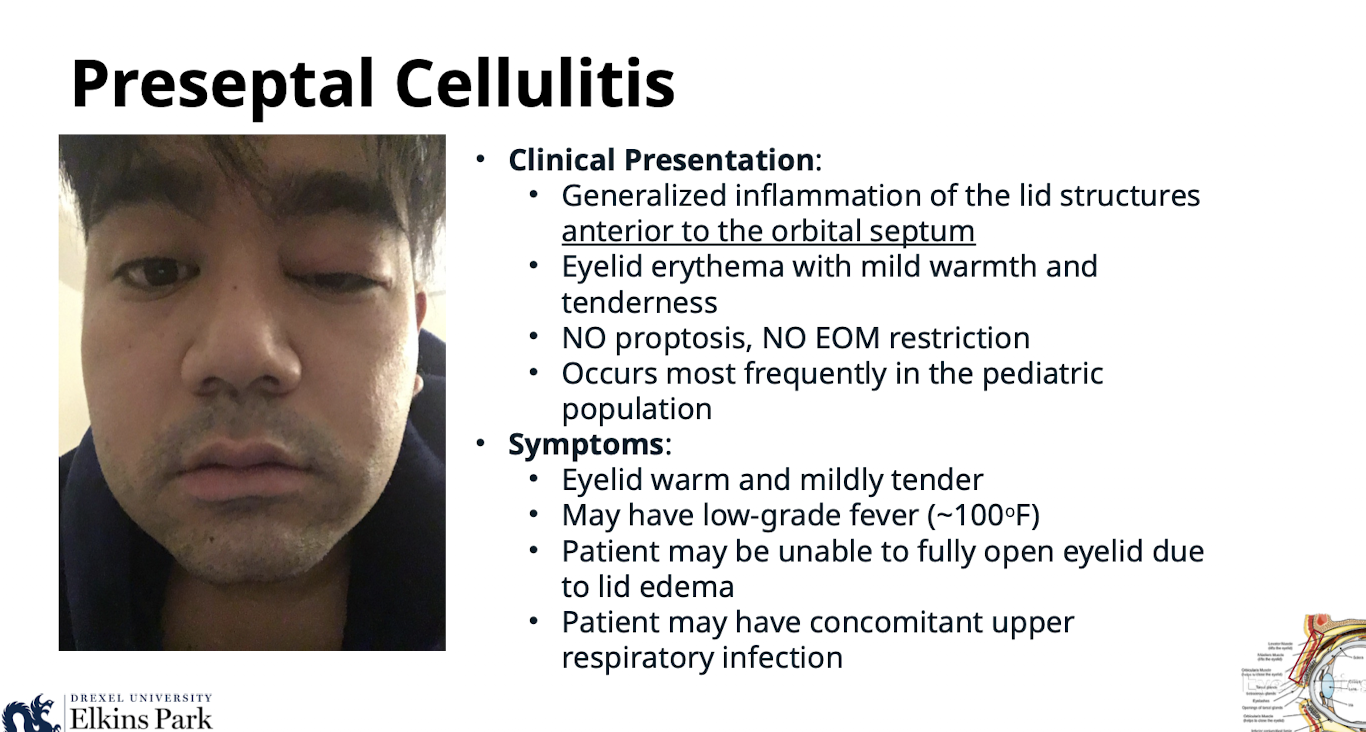
What additional symptoms might a patient with Preseptal Cellulitis have?
Concomitant upper respiratory infection
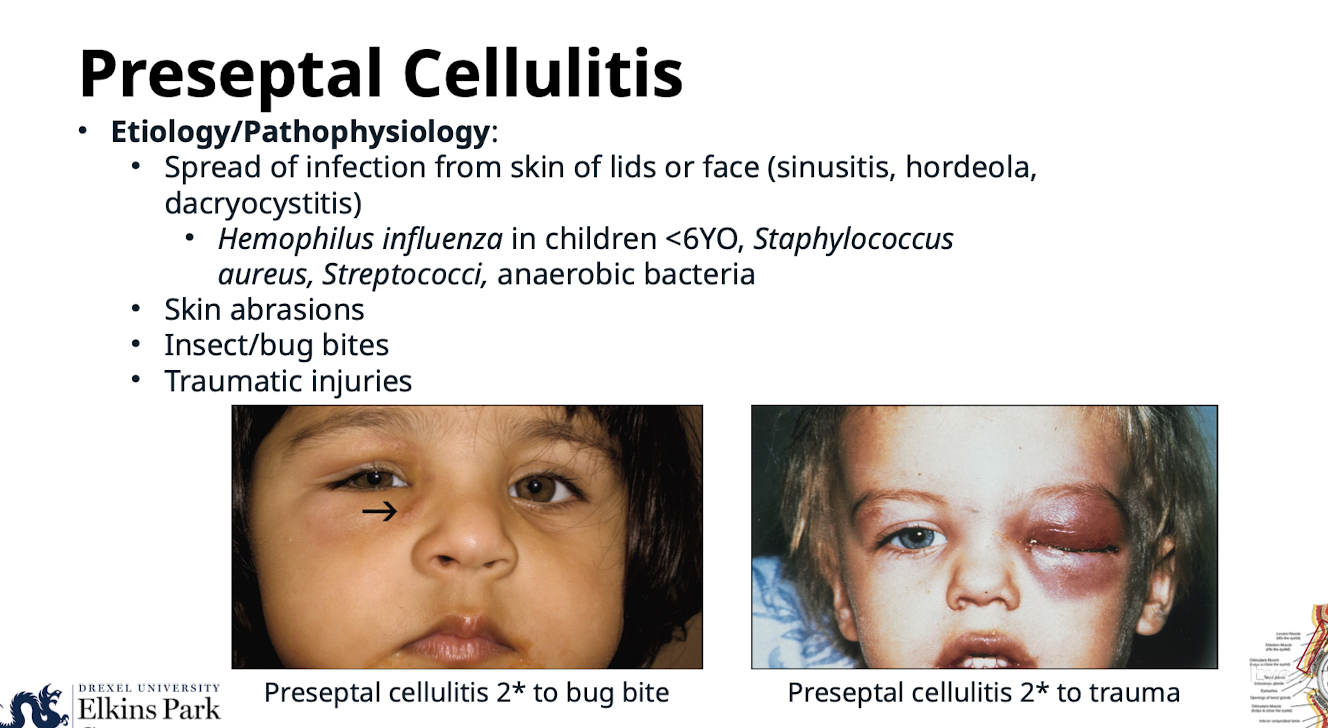
What is the Etiology/Pathophysiology of Preseptal Cellulitis?
Spread of infection from skin of lids or face (sinusitis; hordeola; dacryocystitis);
Hemophilus inuenza in children <6YO;
Staphylococcus aureus; Streptococci; anaerobic bacteria;
skin abrasions; insect/bug bites; traumatic injuries
What must be assessed accurately during the clinical examination for Preseptal Cellulitis?
Visual acuity; pupils; extraocular motilities. SHOULD be unaffected
What physical sign helps determine if there is orbital involvement in suspected cellulitis?
Resistance to retropulsion
Which lymph nodes should be palpated during the clinical examination for Preseptal Cellulitis to detect lymphadenopathy?
Preauricular; submandibular; sublingual
What must a fundus examination rule out when assessing Preseptal Cellulitis?
Optic nerve head swelling or venous engorgement
What medical emergency must be ruled out when diagnosing Preseptal Cellulitis?
Orbital cellulitis
What is the standard oral antibiotic treatment for Preseptal Cellulitis?
Augmentin 25-45mg/kg/day PO (for 7-10 days)
How is the Augmentin dose for children divided in Preseptal Cellulitis treatment?
Divided into two doses for children (max dose: 90mg/kg/day)
What non-oral treatments are used for Preseptal Cellulitis?
Warm compresses to the affected eyelid TID; antibiotic ointment (Polymixin B/bacitracin QID to affected eye if conjunctivitis is present); Tetanus toxoid if needed; Nasal decongestants if sinusitis present
When should a patient with Preseptal Cellulitis be referred for hospitalization?
If no improvement or worsening within 24-48 hours of initiating oral antibiotics
What is the clinical presentation of Orbital Cellulitis?
Eyelid edema; erythema; warmth and tenderness; Conjunctival injection; chemosis (ballooning of the conjunctiva, differentiates from preseptal cellulitis); Proptosis; Febrile and malaise; Restricted extraocular motilities/pain with eye movement
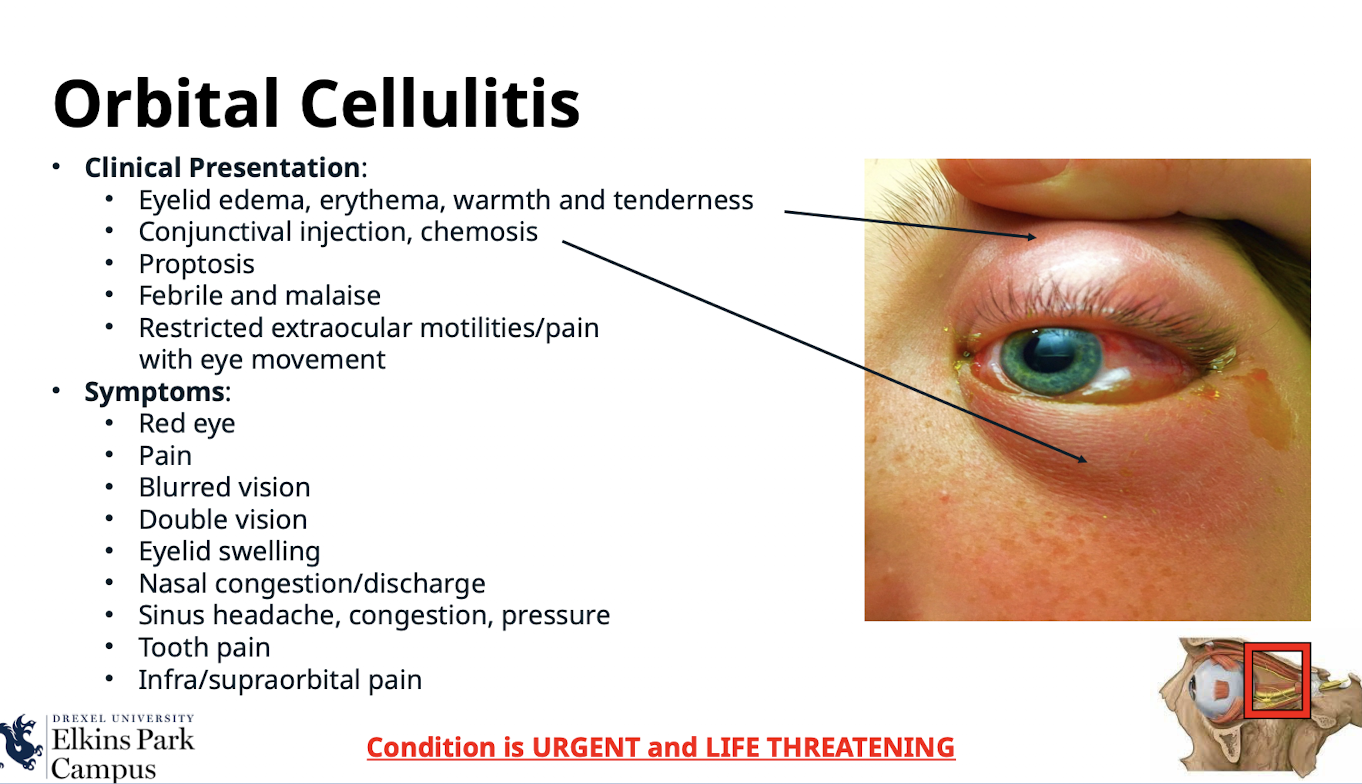
What are the common symptoms of Orbital Cellulitis?
Red eye; Pain; Blurred vision; Double vision; Eyelid swelling; Nasal congestion/discharge; Sinus headache; congestion; pressure; Tooth pain; Infra/supraorbital pain
What is the most common etiology/pathophysiology of Orbital Cellulitis?
Direct extension from a paranasal sinus infection (especially ethmoiditis
What local infections can lead to Orbital Cellulitis?
Focal periorbital infection; Dacryoadenitis; Dacryocystitis; Dental infections
What surgical or systemic causes can lead to Orbital Cellulitis?
Sequela of orbital trauma; Sequela of orbital surgery or paranasal sinus surgery; Vascular extension (seeding from a systemic bacteremia); Secondary to orbital venous stasis and inflammation from a septic cavernous sinus thrombosis
What are the typical infectious organisms causing Orbital Cellulitis in adults and children?
Staphylococcus (adults); Streptococcus (adults); H. influenzae (children)
Which types of infections occur in immunocompromised patients (diabetics; HIV; chemotherapy patients) with Orbital Cellulitis?
Fungal infection; specifically Mucormycosis/zygomycosis or Aspergillus
What key history questions should be asked during the clinical examination for Orbital Cellulitis?
Ask about trauma; surgeries; ear/nose/throat infections; tooth pain/abscess; stiff neck or mental change
What finding related to visual acuity is common in the affected eye with Orbital Cellulitis?
Reduced visual acuity
What pupillary finding indicates compressive optic neuropathy in Orbital Cellulitis?
(+) Afferent Pupillary Defect (+APD)
What signs of orbital involvement are assessed during the clinical exam for Orbital Cellulitis?
Extraocular motilities restriction; Proptosis; Resistance to retropulsion; Conjunctival congestion/chemosis
What might a fundus exam show in a case of Orbital Cellulitis?
Swollen optic nerve head
Why is immediate referral to the emergency department necessary for Orbital Cellulitis?
Concern for infection of the CNS and meningitis
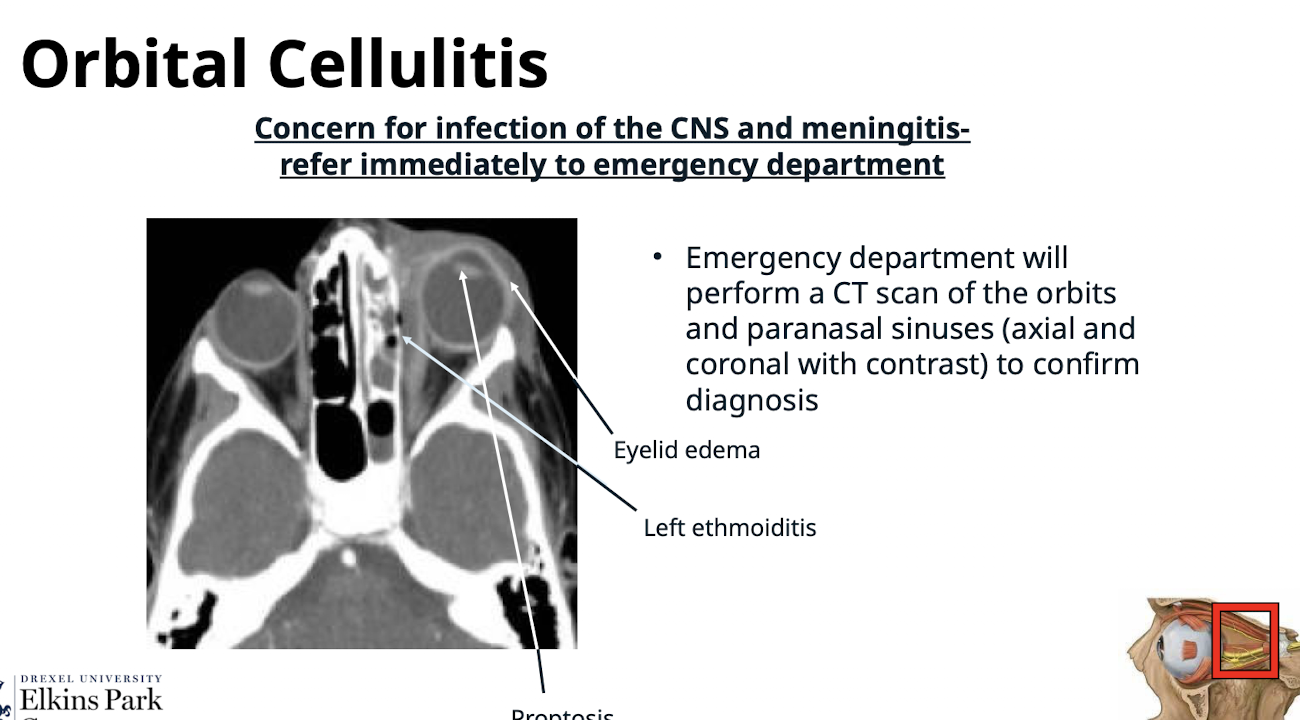
What imaging study is performed in the emergency department to confirm Orbital Cellulitis diagnosis?
A CT scan of the orbits and paranasal sinuses (axial and coronal with contrast)
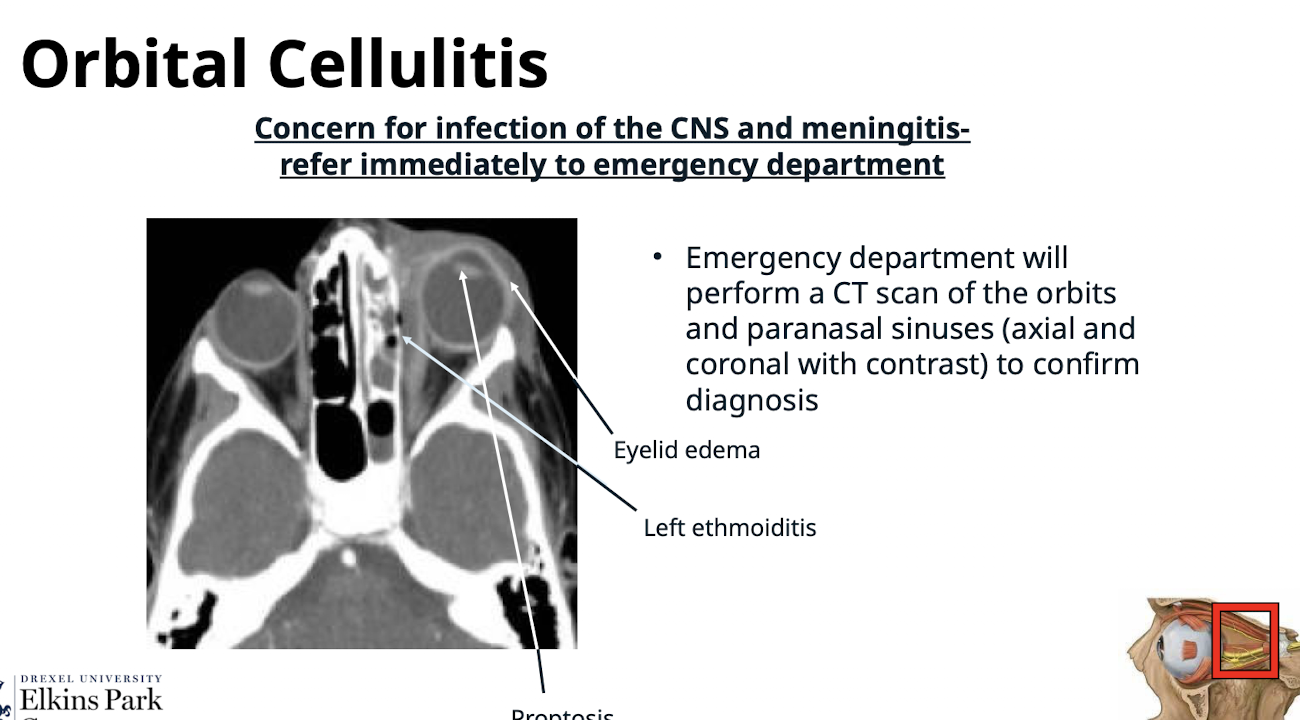
What is the mandatory treatment/management for Orbital Cellulitis?
Admit/refer to ED/hospital for IV antibiotics stat
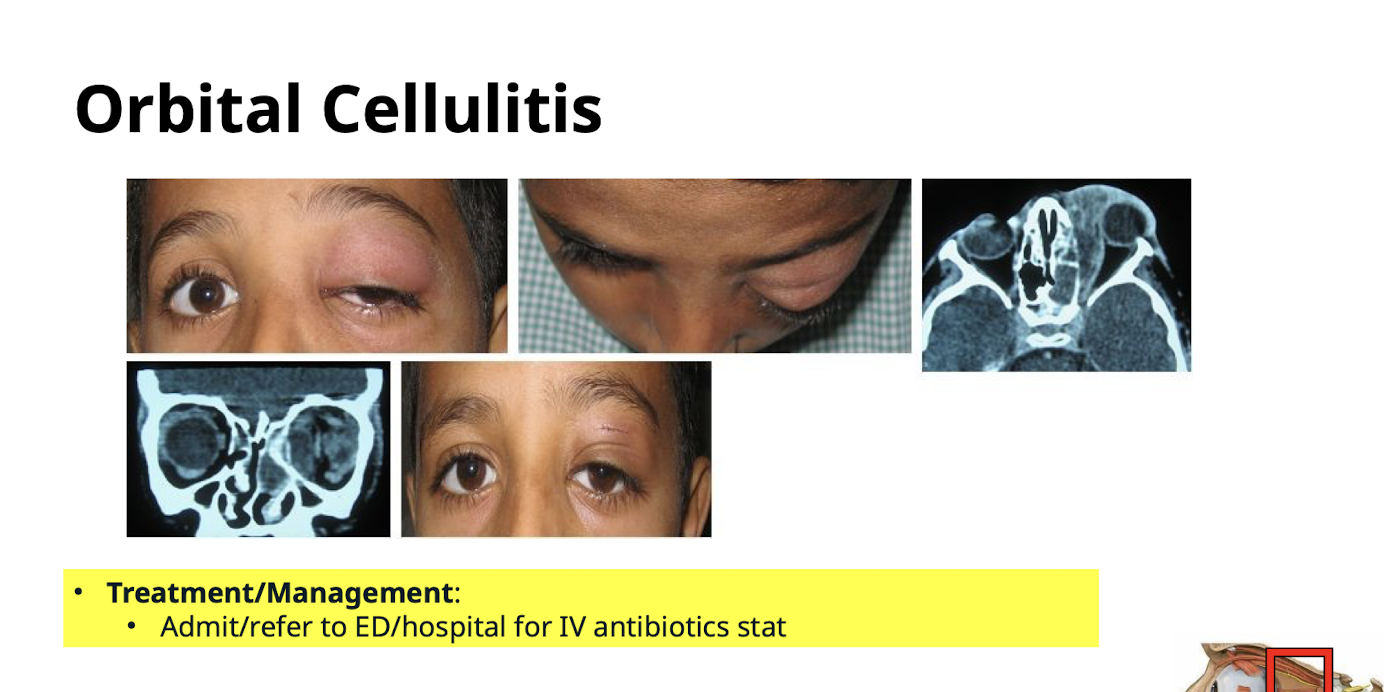
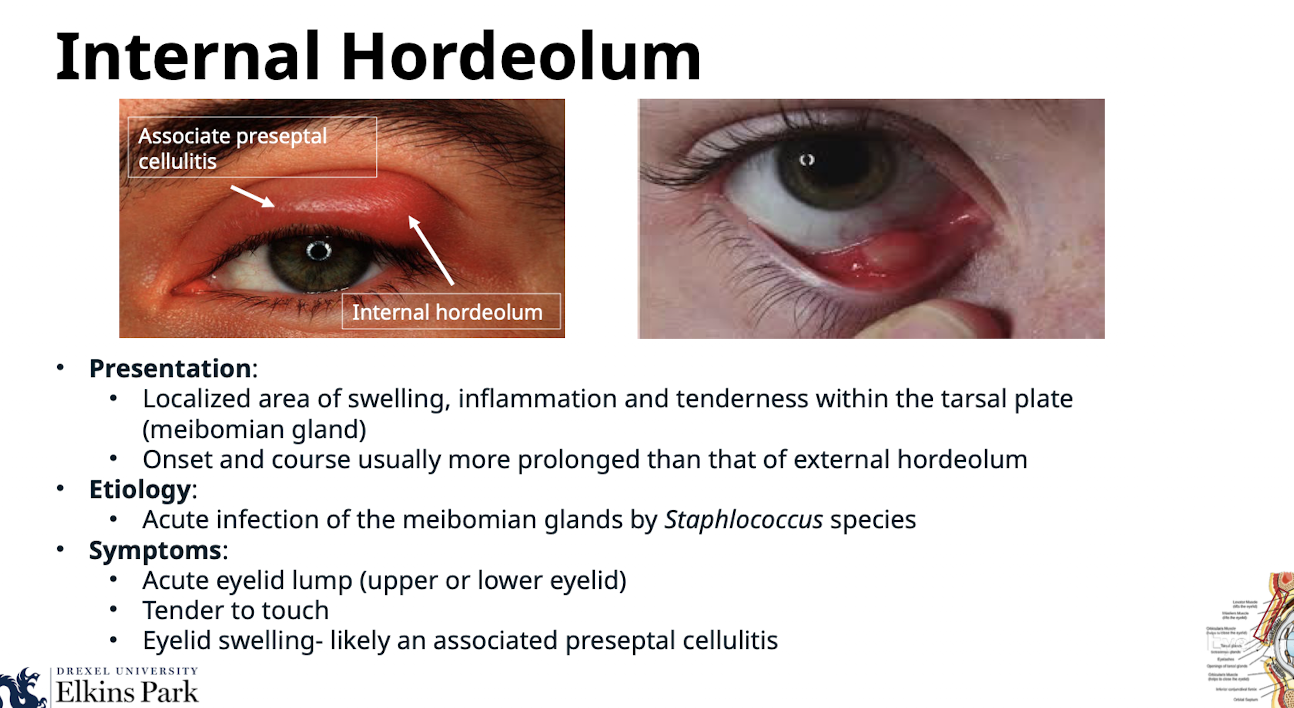
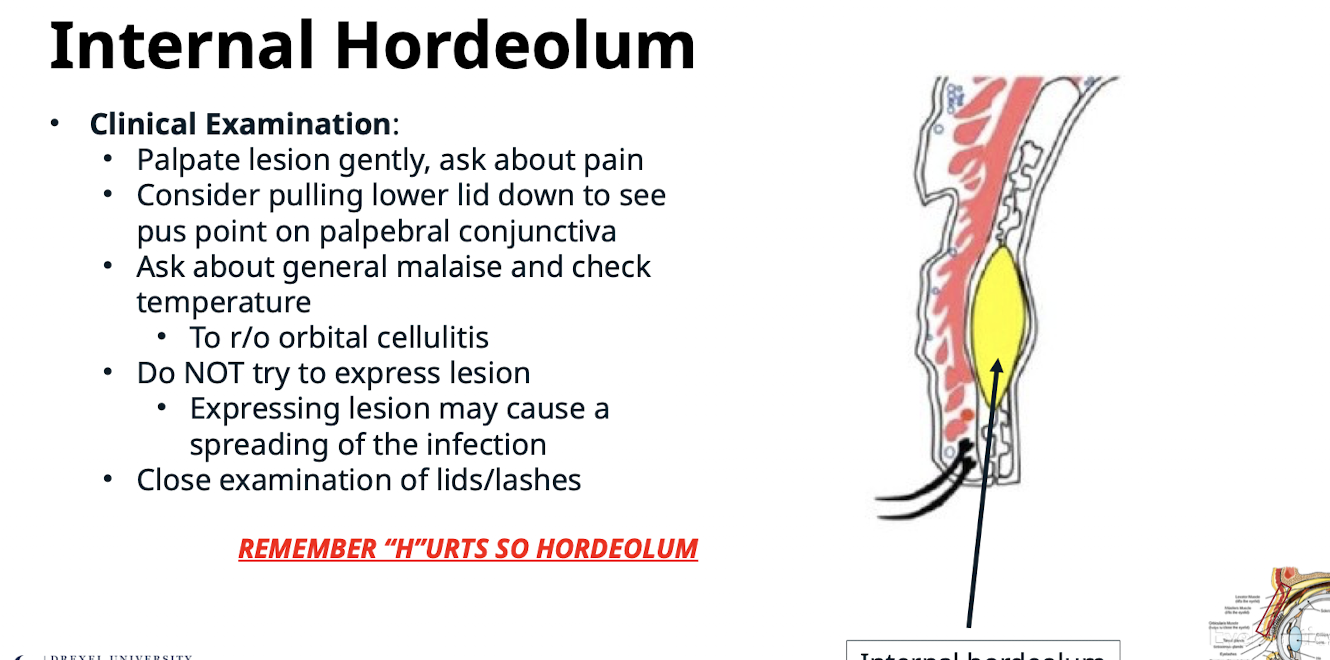
How does Internal Hordeolum present?
Localized area of swelling; inflammation and tenderness within the tarsal plate (meibomian gland); onset and course usually more prolonged than that of external hordeolum
What is the etiology of Internal Hordeolum?
Acute infection of the meibomian glands by Staphlococcus species
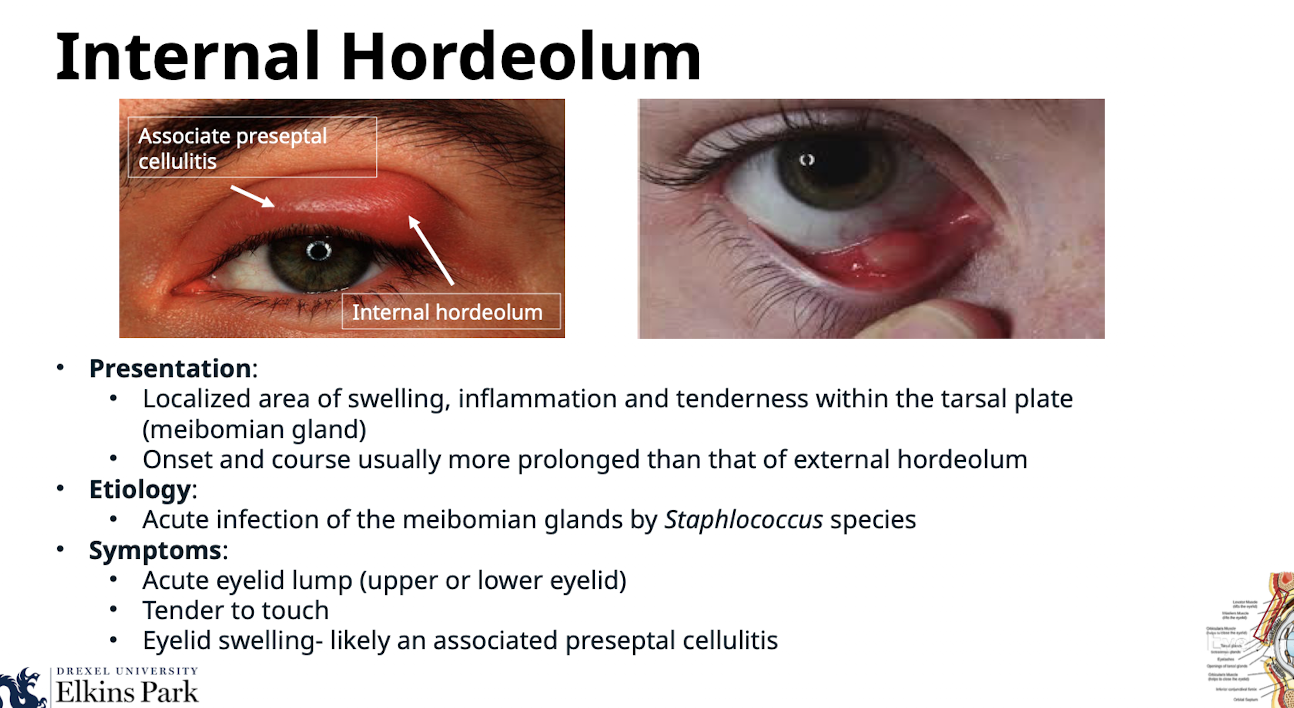
What are the symptoms of Internal Hordeolum?
Acute eyelid lump (upper or lower eyelid); Tender to touch; Eyelid swelling- likely an associated preseptal cellulitis
During the clinical examination for Internal Hordeolum, what should the clinician look for on the palpebral conjunctiva?
Consider pulling lower lid down to see pus point on palpebral conjunctiva
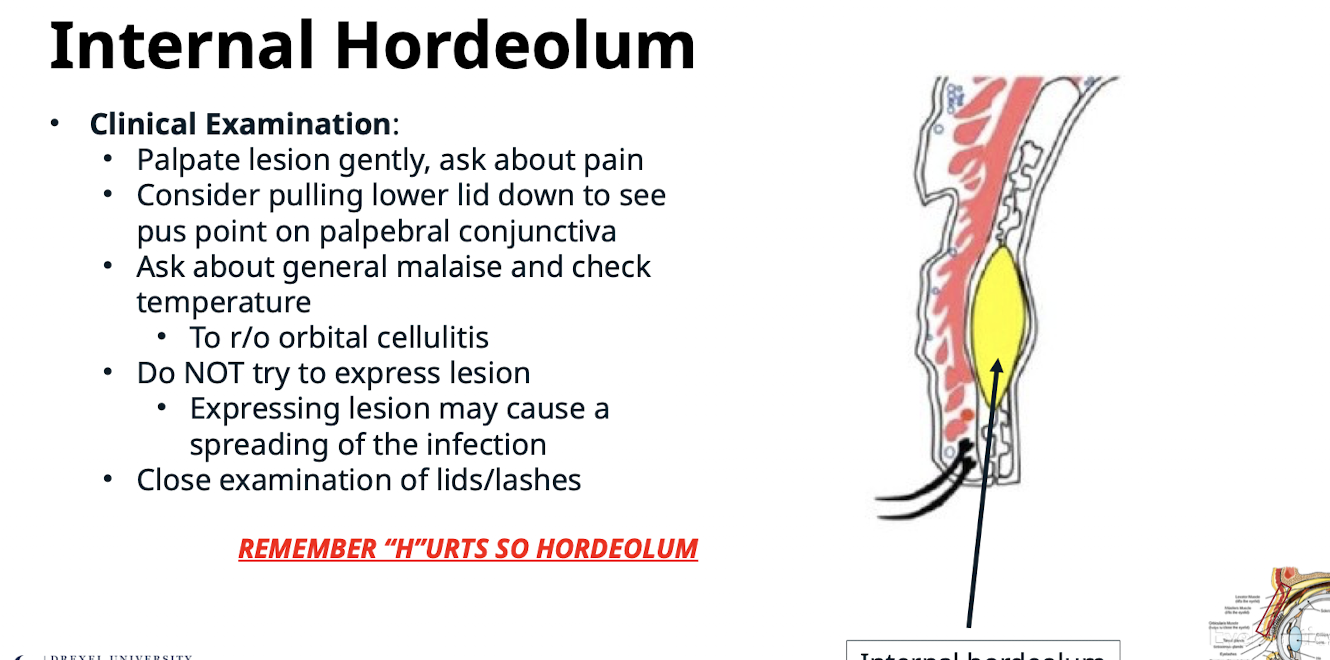
Why should the clinician check for general malaise and temperature in Internal Hordeolum?
To rule out orbital cellulitis
What clinical instruction is critical regarding expressing an Internal Hordeolum lesion?
Do NOT try to express lesion; expressing lesion may cause a spreading of the infection
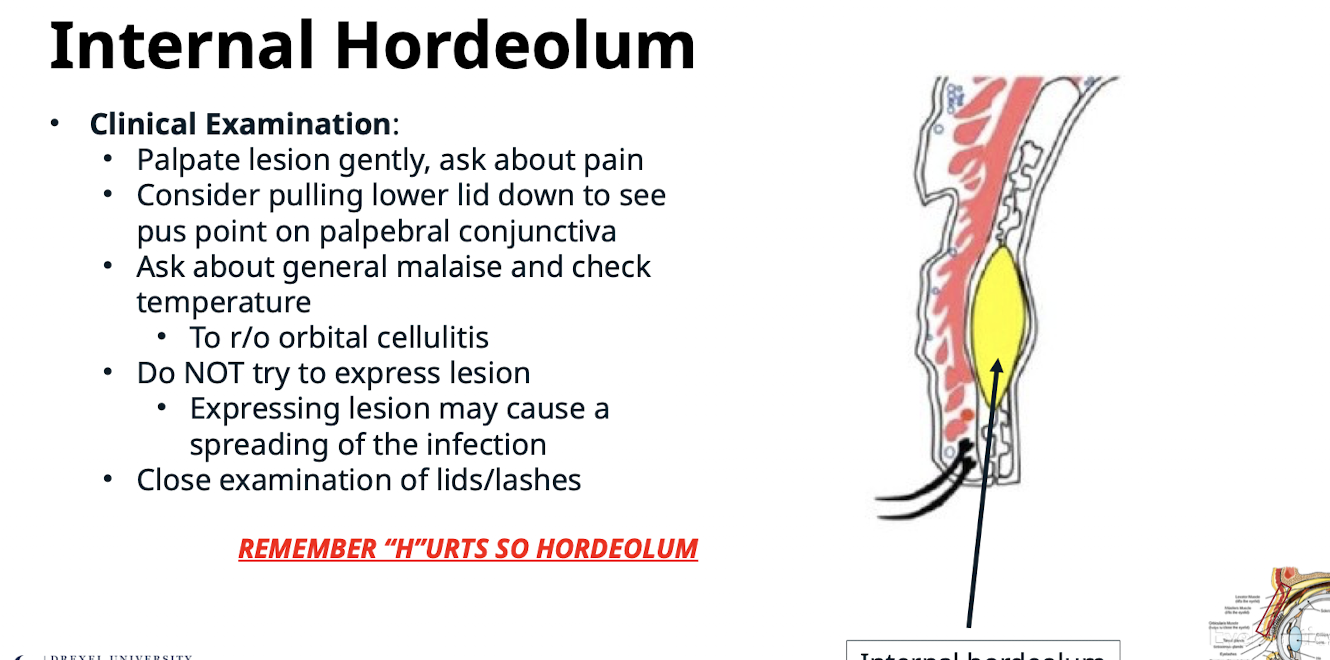
What is the mnemonic used to remember Internal Hordeolum?
REMEMBER “H”URTS SO HORDEOLUM. Chalazions do not hurt
What is the primary initial treatment for acute Internal Hordeolum infection?
Warm compresses for 10 min QID with gentle massage
How do warm compresses help treat an Internal Hordeolum?
Brings blood supply to lesion for immune defense; brings antibiotic in blood stream; helps to break up lesion in eyelid
What topical antibiotics are used for Internal Hordeolum?
Bacitracin ung q3h; Erythromycin ung q3h
What is the management for an internal hordeolum
Refer to ECP within 1 week for follw up
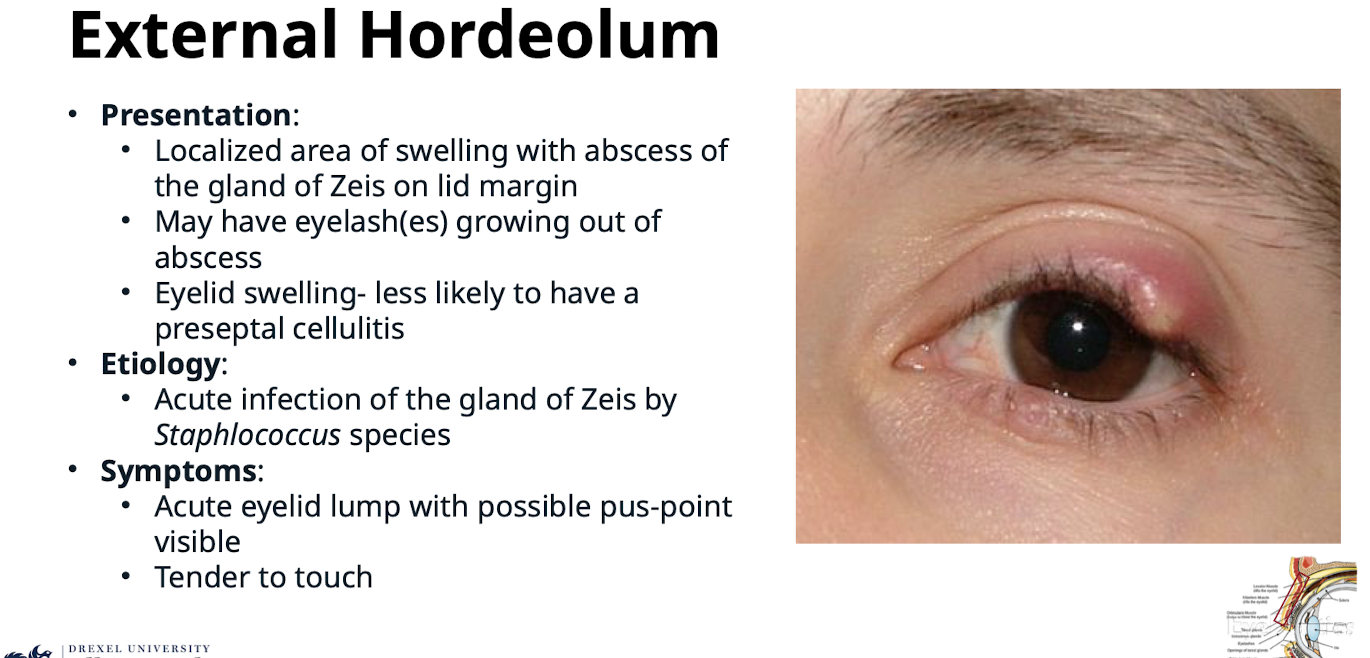
How does External Hordeolum present?
Localized area of swelling with abscess of the gland of Zeis on lid margin; may have eyelash(es) growing out of abscess; eyelid swelling- less likely to have a preseptal celluliti
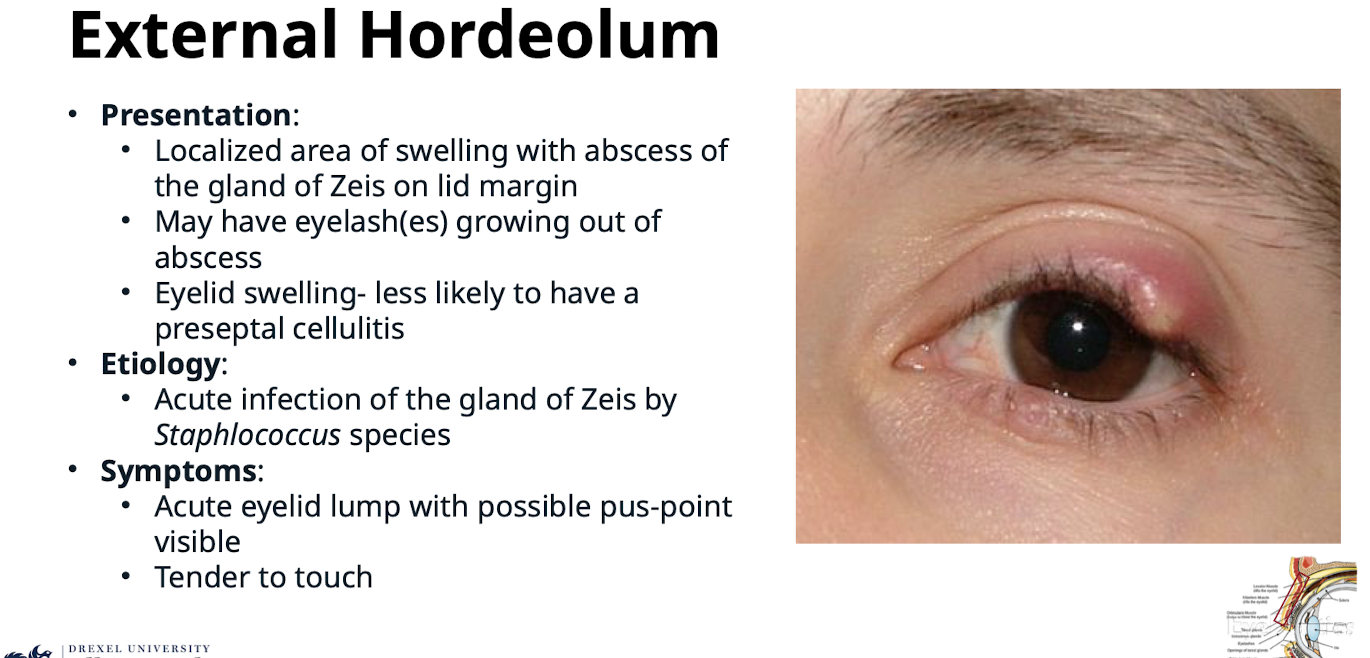
What is the etiology of External Hordeolum?
Acute infection of the gland of Zeis by Staphlococcus species
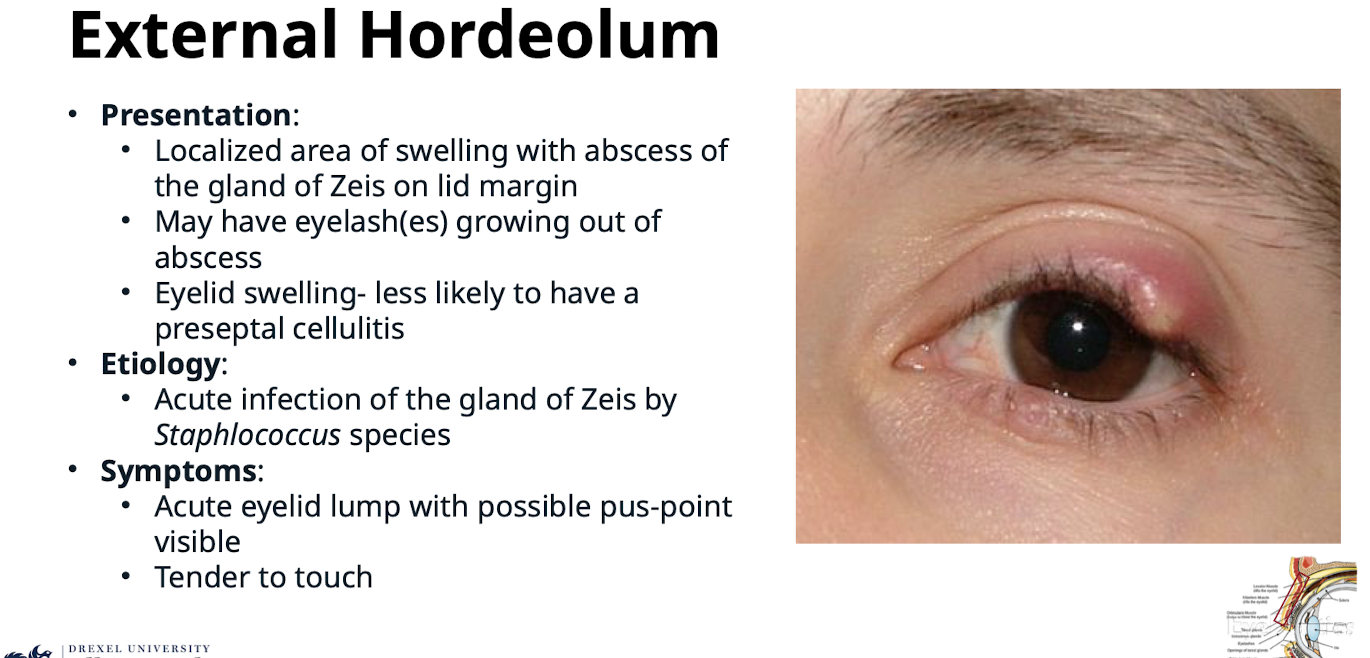
What are the symptoms of External Hordeolum?
Acute eyelid lump with possible pus-point visible; Tender to touch
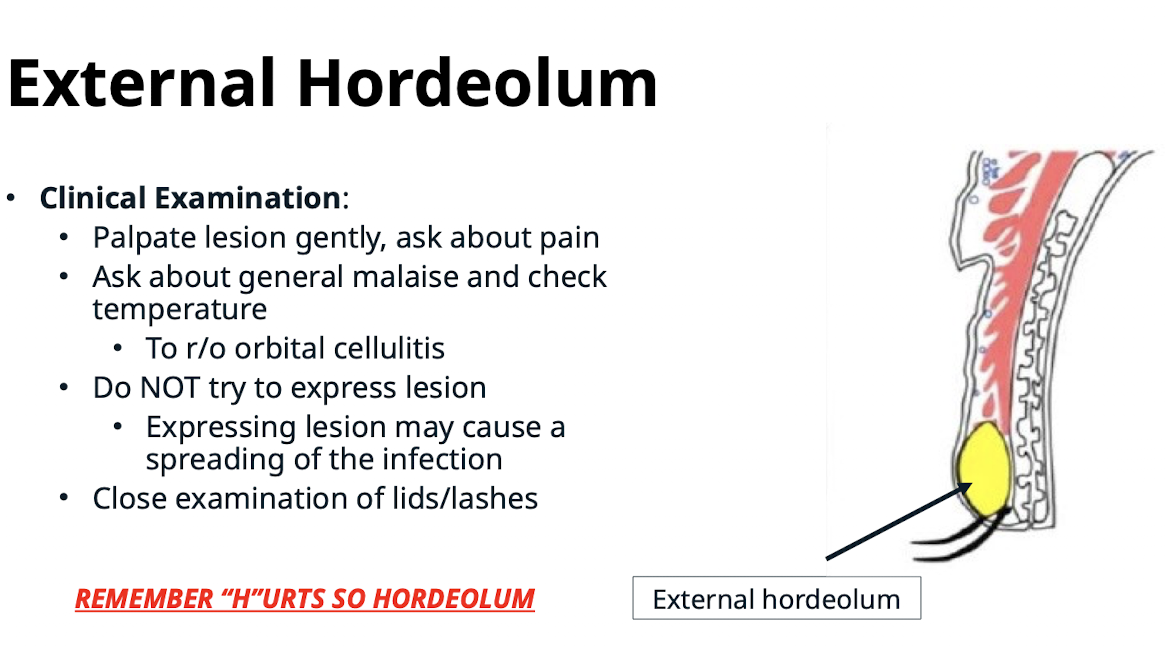
What instructions apply to the clinical examination and management of the lesion in External Hordeolum?
Palpate lesion gently; ask about pain; Do NOT try to express lesion; expressing lesion may cause a spreading of the infection
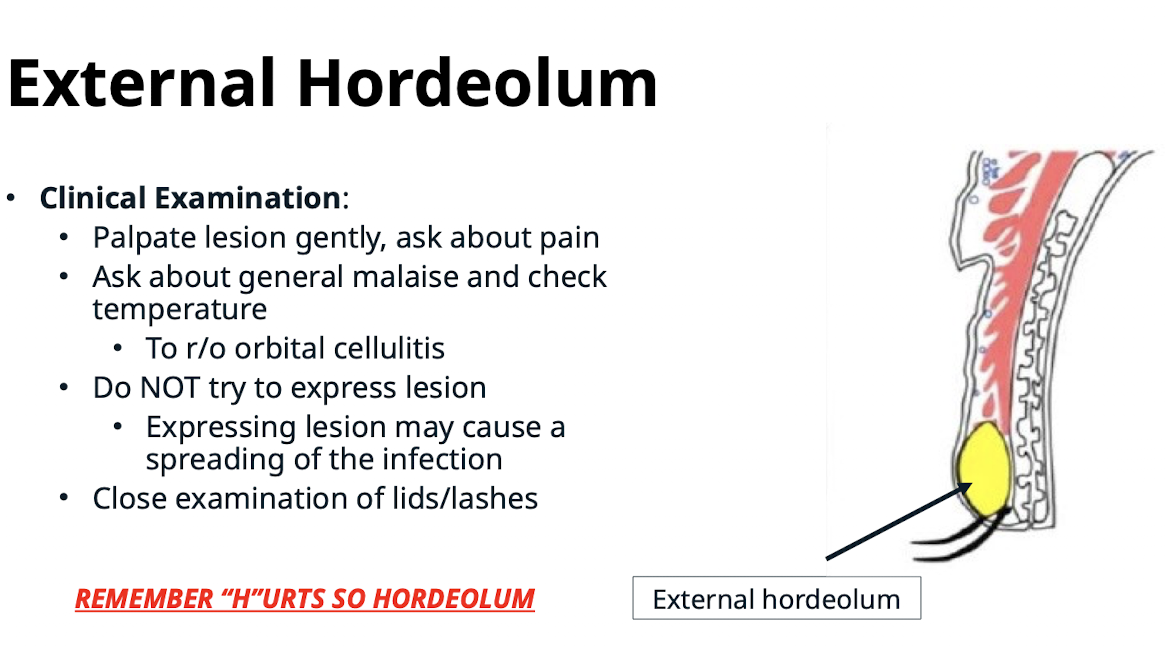
Why is it important to check temperature and general malaise in External Hordeolum?
To rule out orbital cellulitis
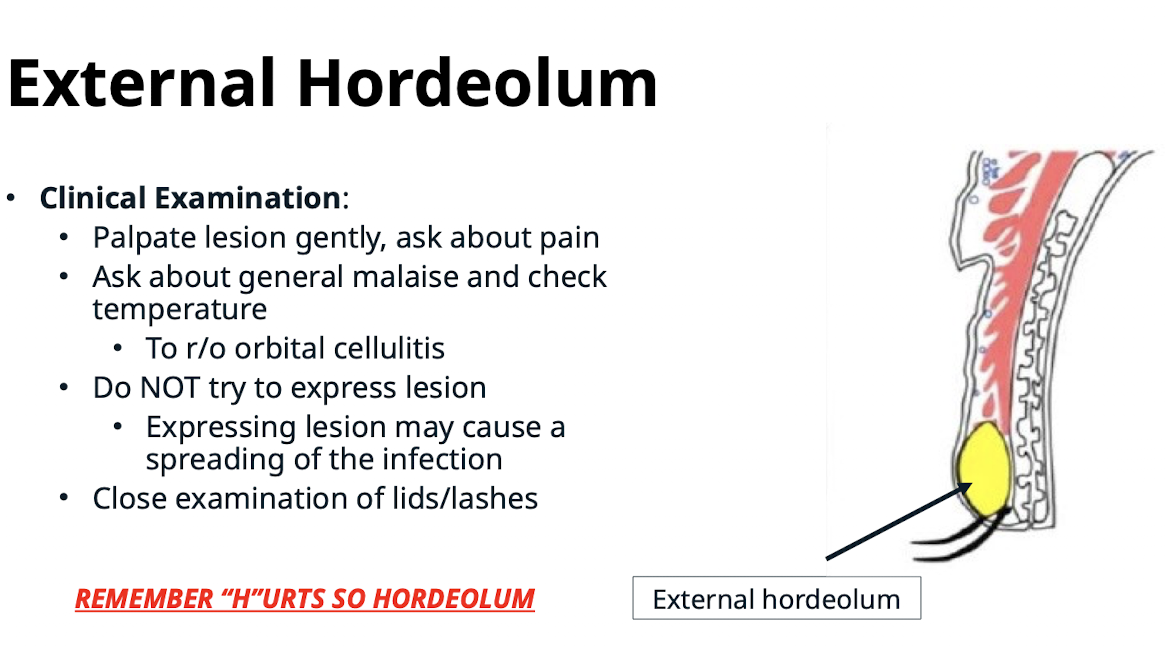
What is the mnemonic used to remember External Hordeolum?
REMEMBER “H”URTS SO HORDEOLUM
What are the treatment methods and management for acute External Hordeolum infection?
Warm compresses for 10 min QID with gentle message; Lash(es) Epilation of abscess (may cause lesion to drain); Topical antibiotics (Bacitracin ung q3h; Erythromycin ung q3h
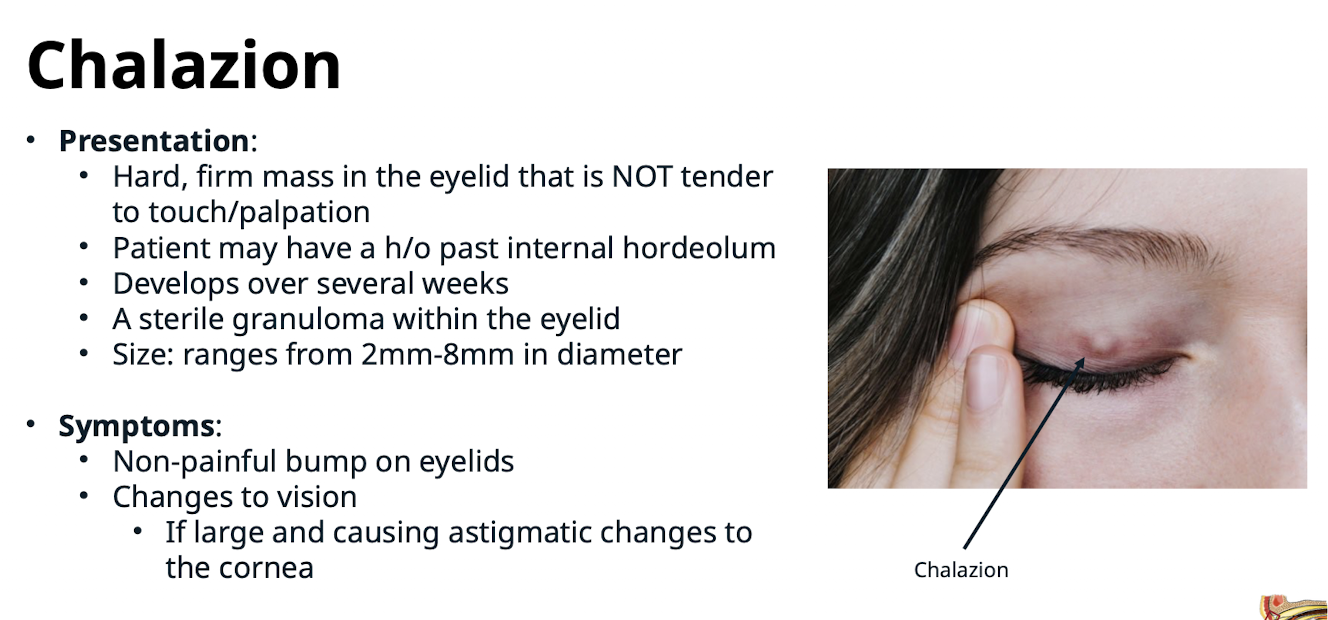
How does a Chalazion present?
Hard; firm mass in the eyelid that is NOT tender to touch/palpation; patient may have a history of past internal hordeolum; develops over several weeks; a sterile granuloma within the eyelid; Size: ranges from 2mm-8mm in diameter
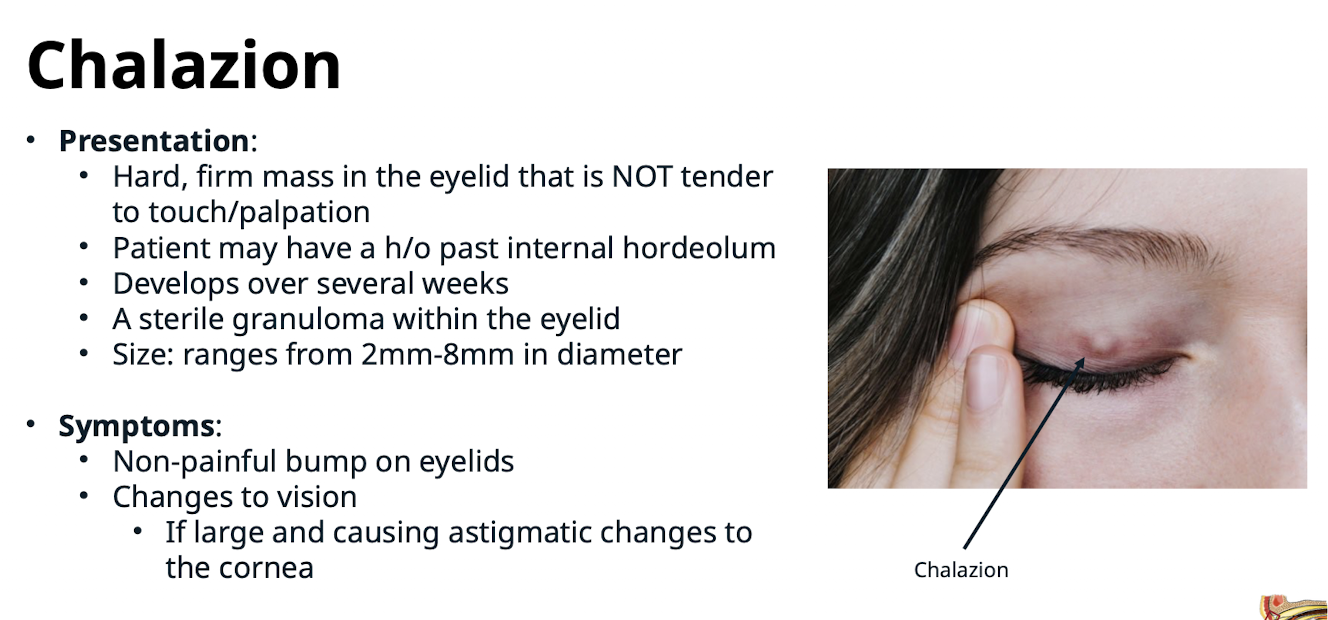
What are the symptoms of Chalazion?
Non-painful bump on eyelids; Changes to vision (if large and causing astigmatic changes to the cornea)
What is the key finding upon palpation of a Chalazion nodule?
There should be no pain
What conservative treatments are recommended for Chalazion?
Warm compresses* 5-10 minutes QID over affected eyelid followed by gentle digital message;
Topical Steroid/Steroid-Antibiotic Eyedrops/Ointments* – controversial bc it doesn’t really work (Maxitrol; FML; etc. BID-QID in the affected eye)
When should a patient with Chalazion be referred to Ophthalmology (Oculoplastics)?
If the lesion does not respond to conservative treatment
What are the surgical interventions for Chalazion?
Intralesional steroid injection; Incision and curettage
What is a potential side effect of Intralesional steroid injection for Chalazion? What is the management?
May lead to depigmentation of the injection site. Refer to ECP or Oculoplastics surgeon within 2-3 weeks
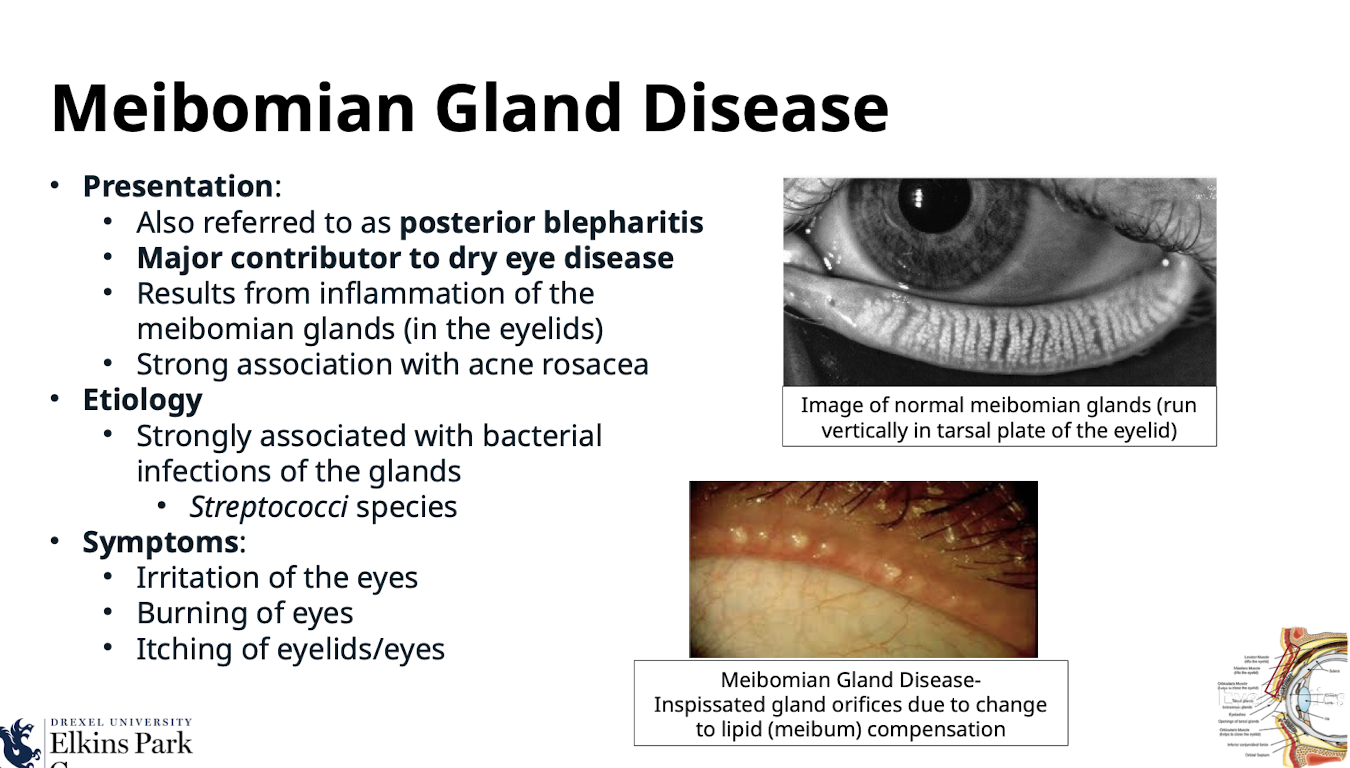
What is Meibomian Gland Disease also referred to as?
Posterior blepharitis
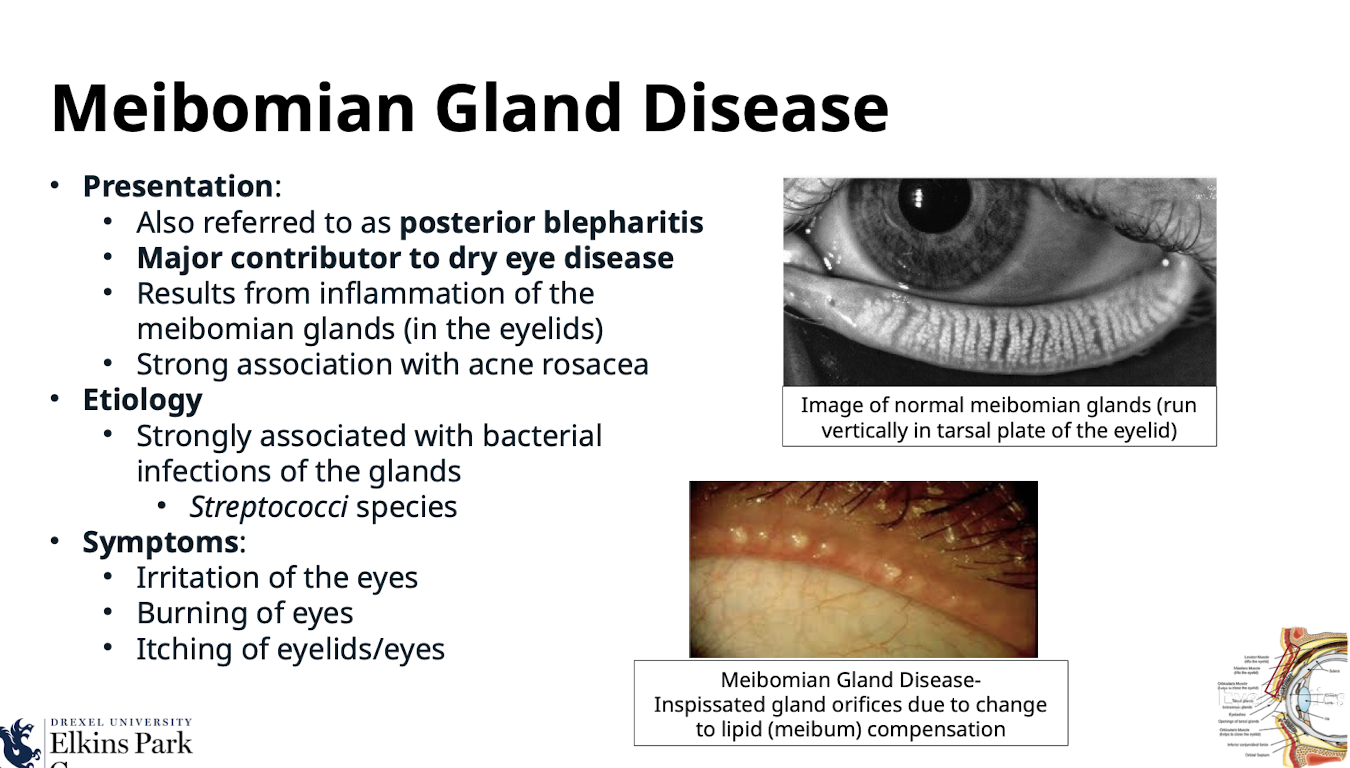
What is the clinical significance of Meibomian Gland Disease?
Major contributor to dry eye disease
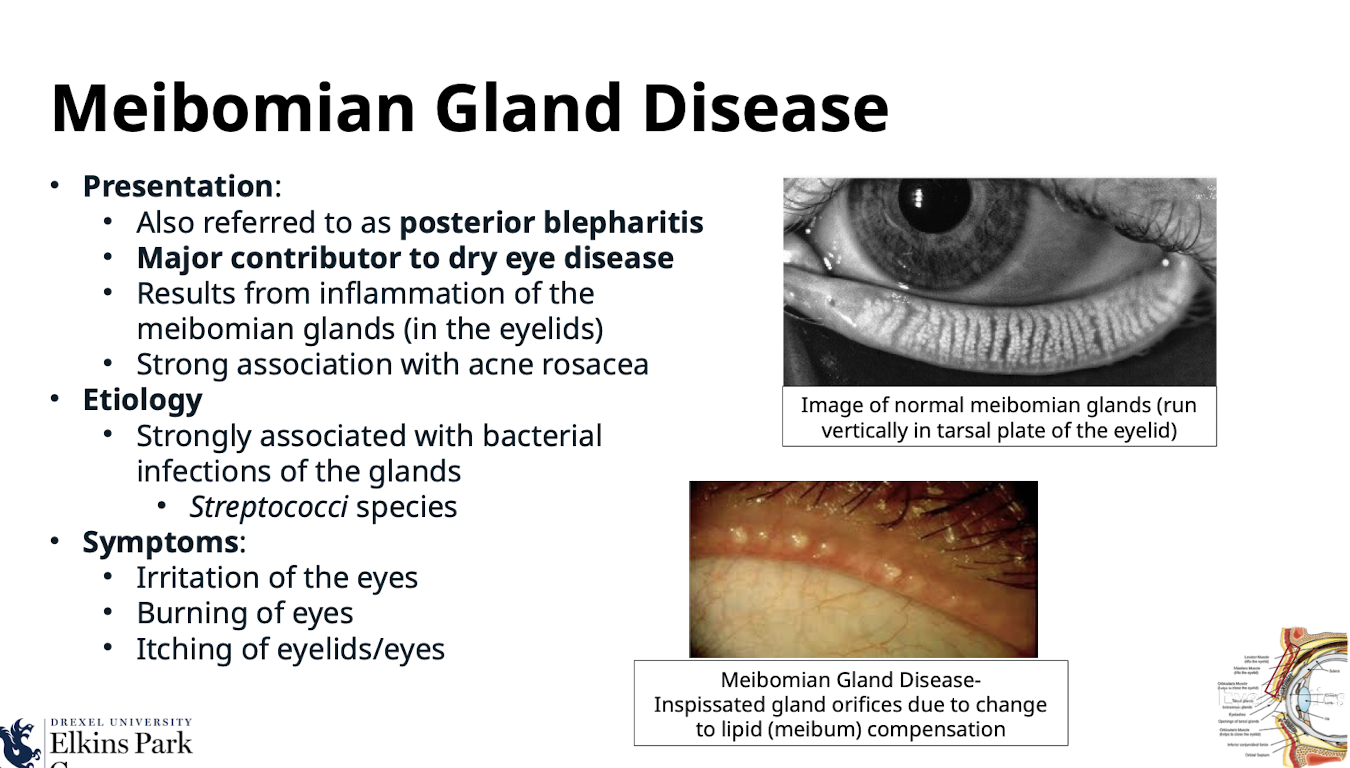
What condition is strongly associated with Meibomian Gland Disease?
Acne rosacea
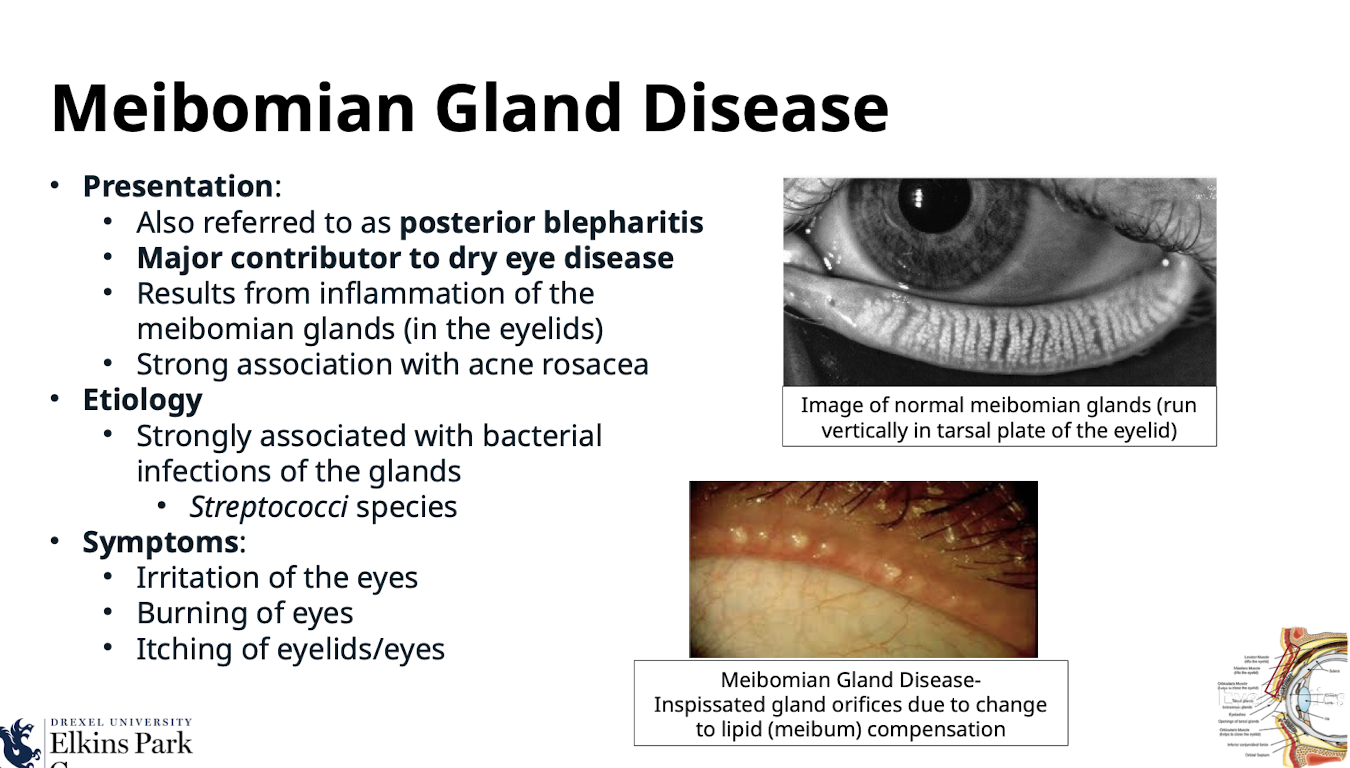
What is the etiology of Meibomian Gland Disease?
Results from inflammation of the meibomian glands (in the eyelids); strongly associated with bacterial infections of the glands
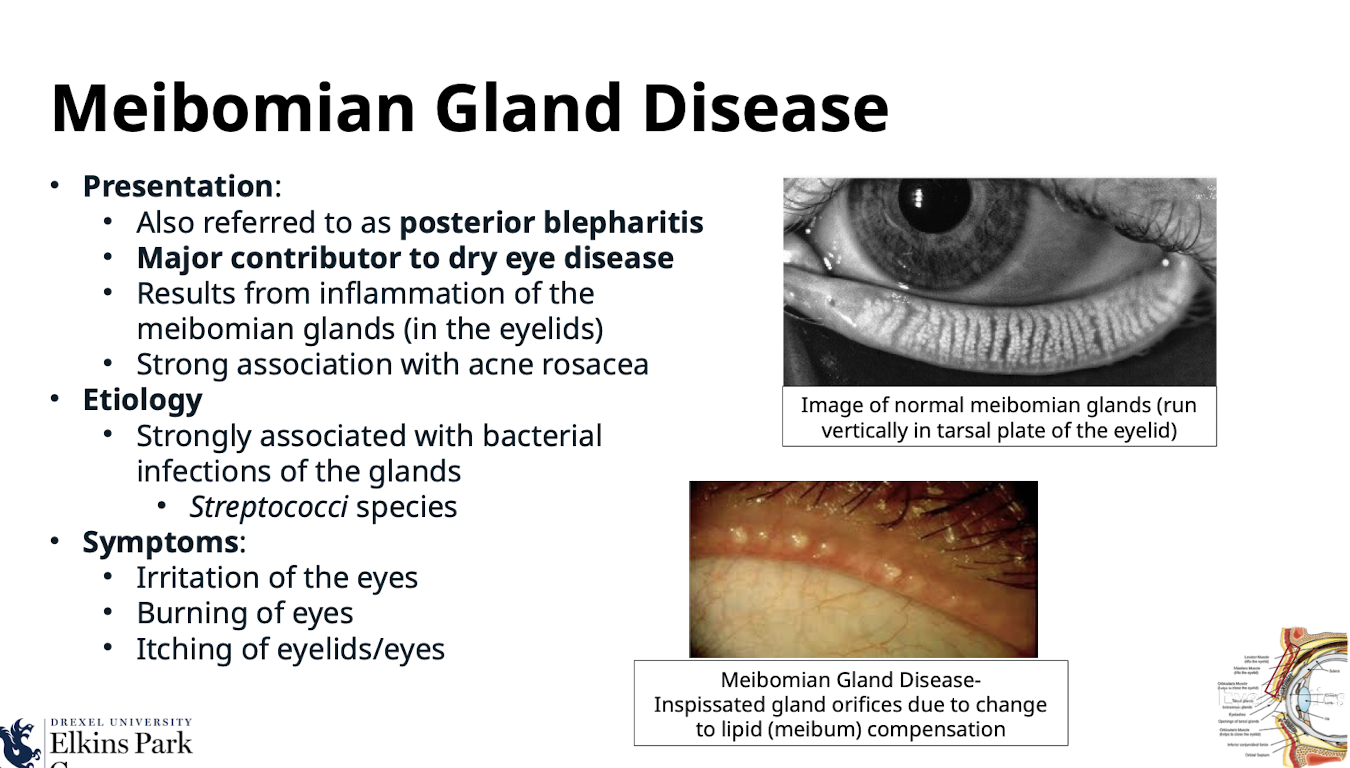
What bacterial species are associated with Meibomian Gland Disease?
Streptococci species
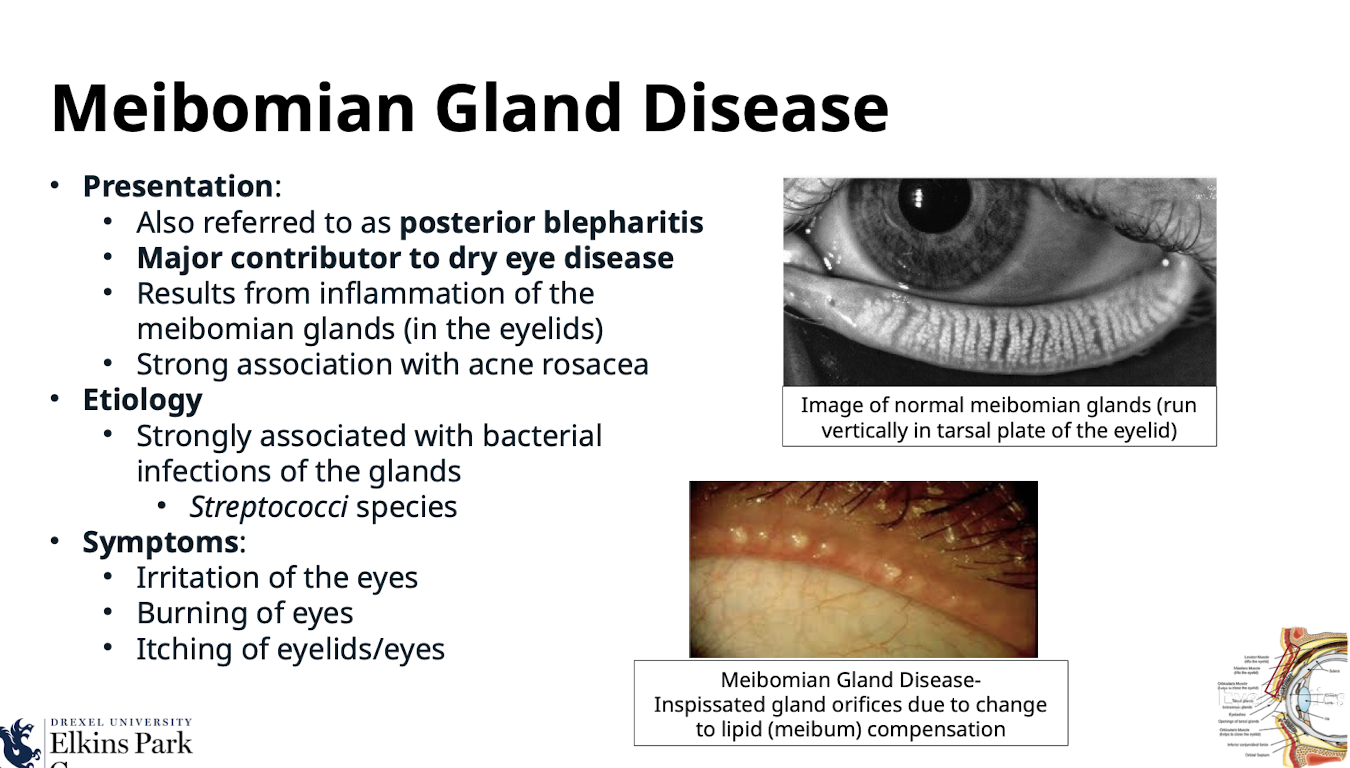
What are the symptoms of Meibomian Gland Disease?
Irritation of the eyes; Burning of eyes; Itching of eyelids/eyes
What features are seen on the eyelid margins in Meibomian Gland Disease?
Eyelid margins are hyperemic with/without eyelid telangiectasia; Meibomian gland orifices are inflamed
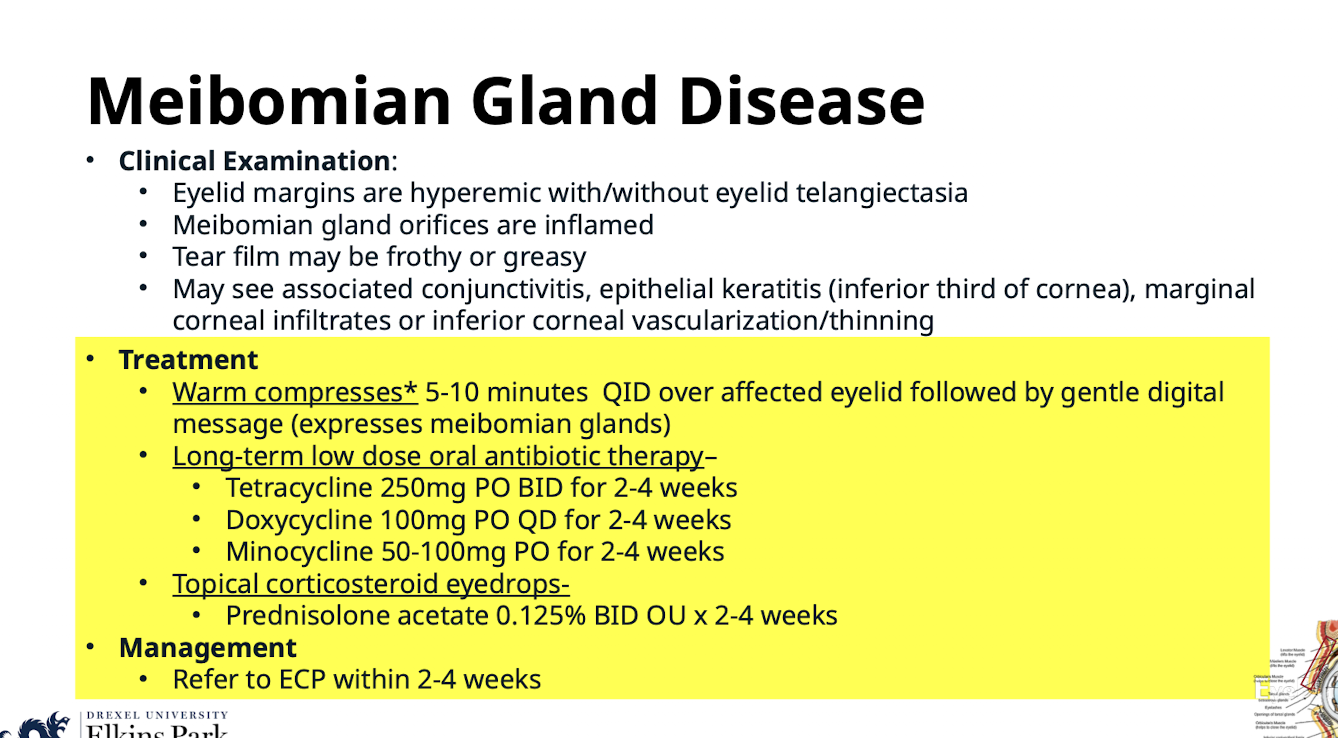
What does the tear film look like in Meibomian Gland Disease?
May be frothy or greasy
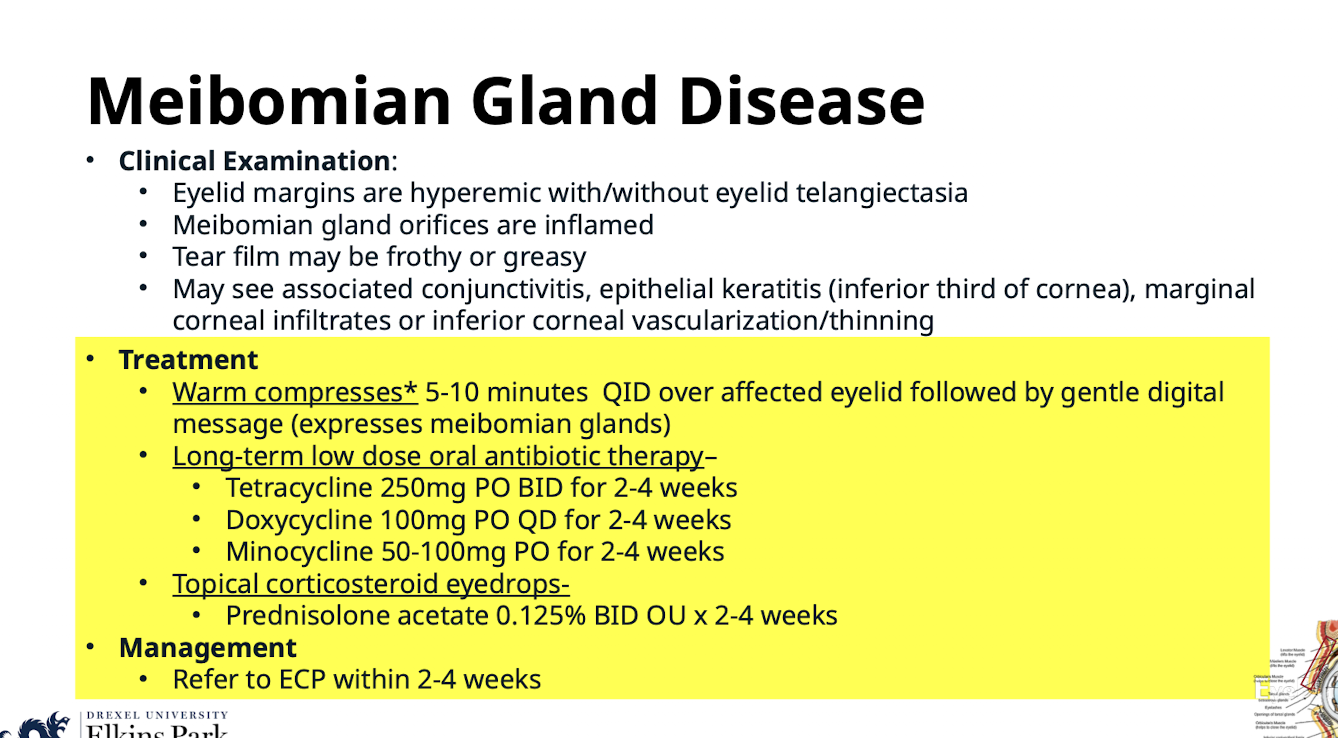
What associated ocular complications may be seen with Meibomian Gland Disease?
Associated conjunctivitis; epithelial keratitis (inferior third of cornea); marginal corneal infiltrates or inferior corneal vascularization/thinning
What conservative treatment expresses meibomian glands in MGD?
Warm compresses* 5-10 minutes QID over affected eyelid followed by gentle digital massage (expresses meibomian glands)
What long-term low dose oral antibiotics are used to treat Meibomian Gland Disease?
Tetracycline 250mg PO BID for 2-4 weeks;
Doxycycline 100mg PO QD for 2-4 weeks;
Minocycline 50-100mg PO for 2-4 weeks
What topical corticosteroid eyedrops are used for MGD treatment? What is the management of MGD
Prednisolone acetate 0.125% BID OU x 2-4 weeks. Refer to ECP within 2-4 weeks
How does Anterior Blepharitis present?
A chronic inflammatory condition of bilateral eyelids/lashes; involves the eyelid skin; lashes and associated glands
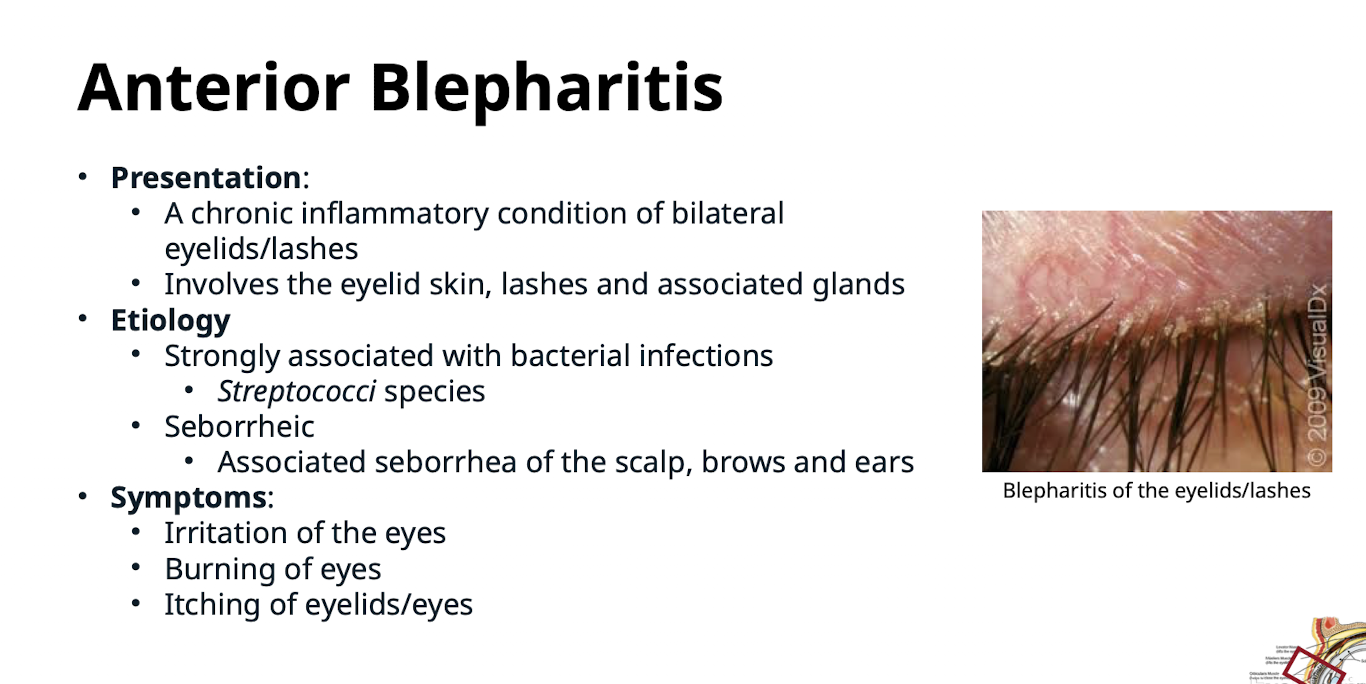
What are the two main etiologies of Anterior Blepharitis?
Strongly associated with bacterial infections (Streptococci species); Seborrheic (associated seborrhea of the scalp; brows and ears)
What are the common symptoms of Anterior Blepharitis?
Irritation of the eyes; Burning of eyes; Itching of eyelids/eyes
What classic finding is seen on the eyelids during the clinical examination for Anterior Blepharitis?
The eyelids are “red-rimmed” (hyperemia of the eyelid skin) with scales or collarettes seen clinging to the lashe
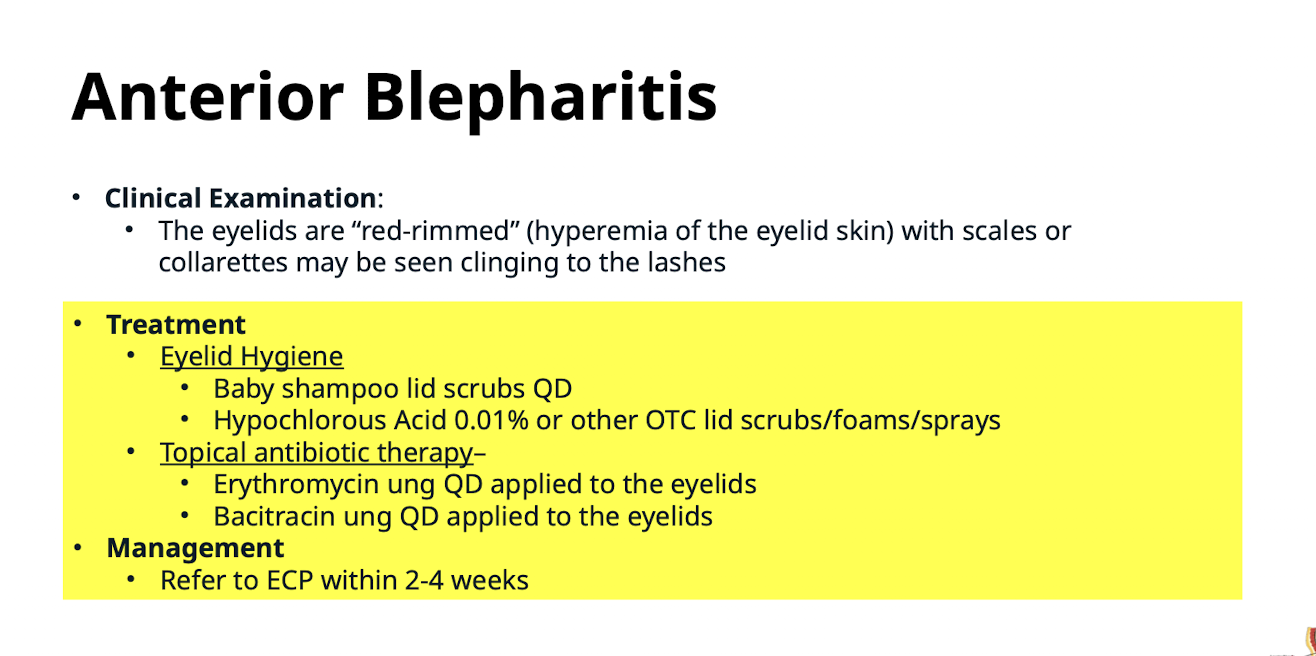
What constitutes Eyelid Hygiene treatment for Anterior Blepharitis?
Baby shampoo lid scrubs QD;
Hypochlorous Acid 0.01% or other OTC lid scrubs/foams/sprays
What topical antibiotic therapy and management is used for Anterior Blepharitis? Refer to ECP within 2-4 weeks
Erythromycin ung QD applied to the eyelids;
Bacitracin ung QD applied to the eyelids
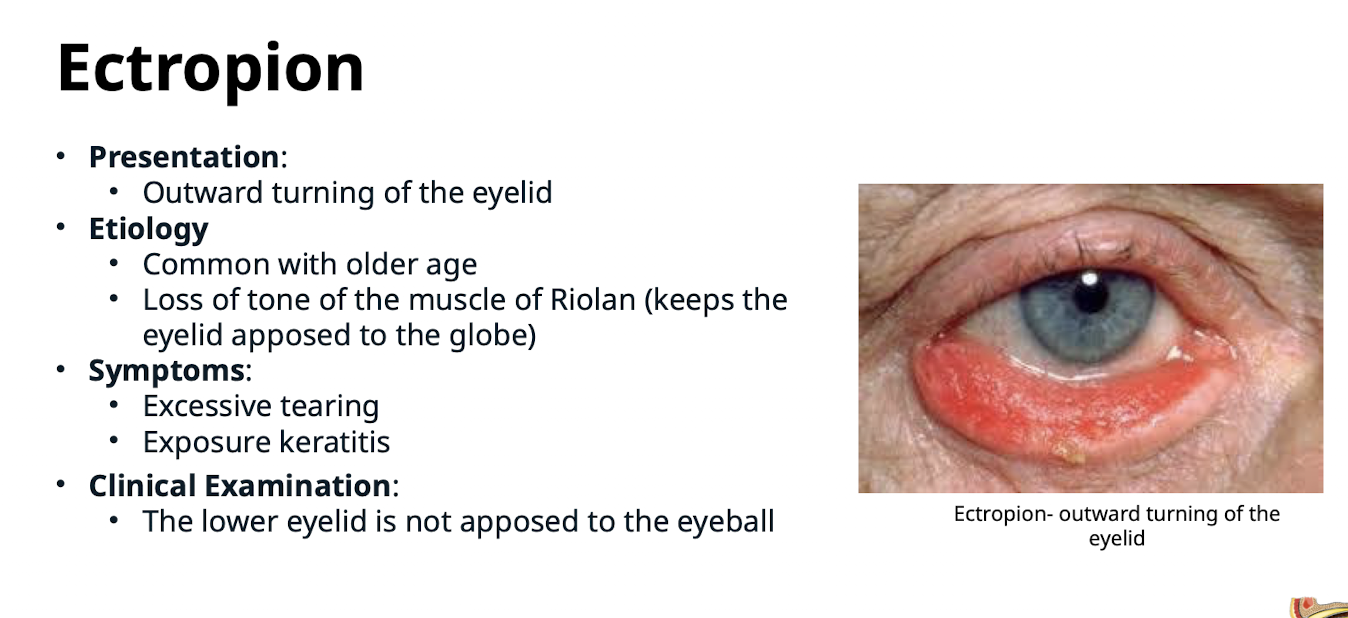
How is Ectropion defined?
Outward turning of the eyelid
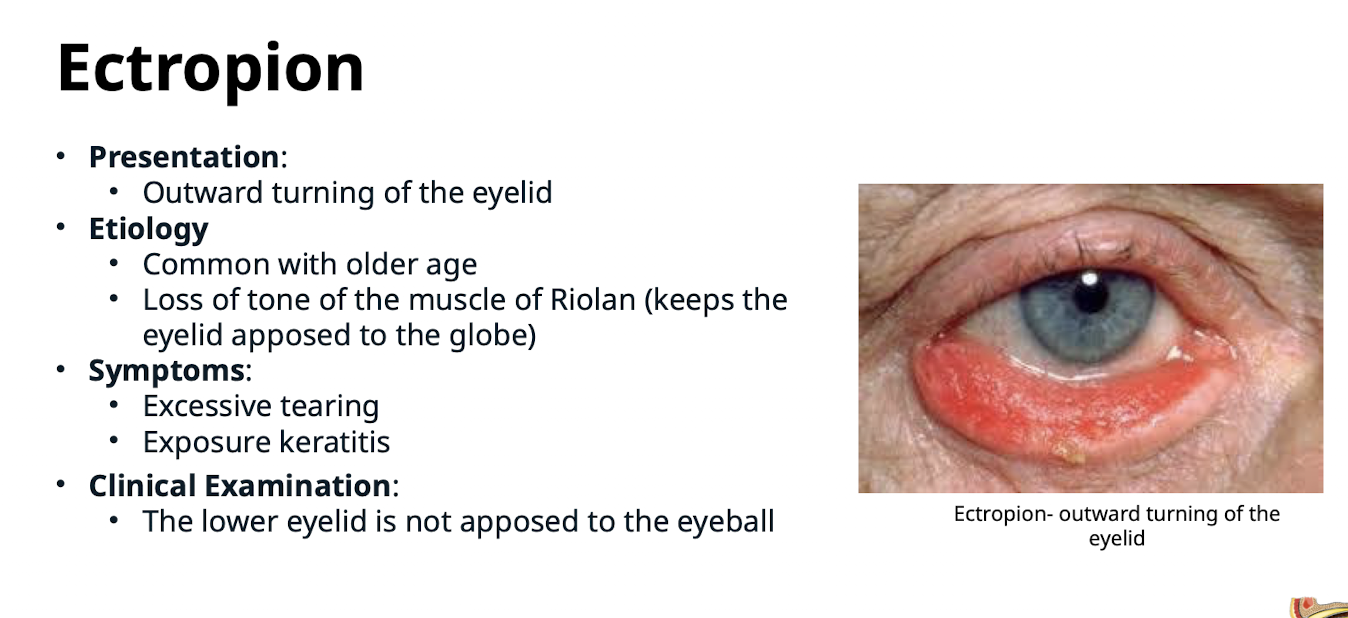
What is the primary cause of Ectropion in older age?
Loss of tone of the muscle of Riolan (which keeps the eyelid apposed to the globe)
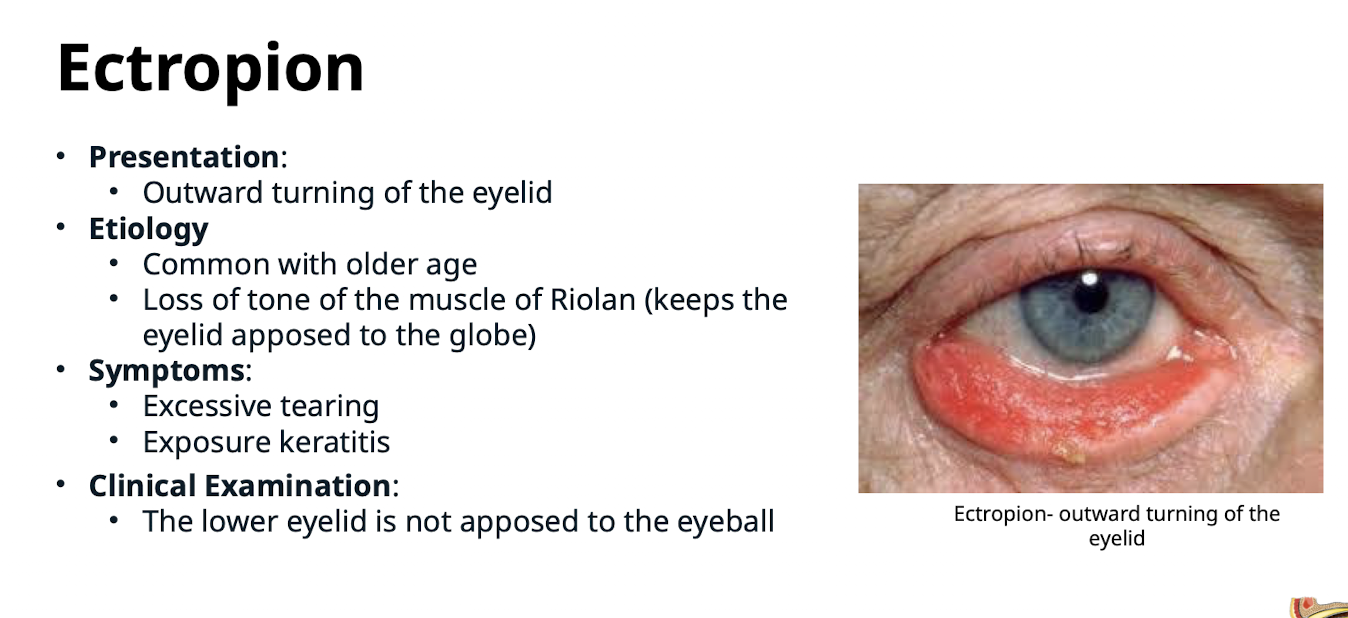
What are the symptoms of Ectropion?
Excessive tearing; Exposure keratitis
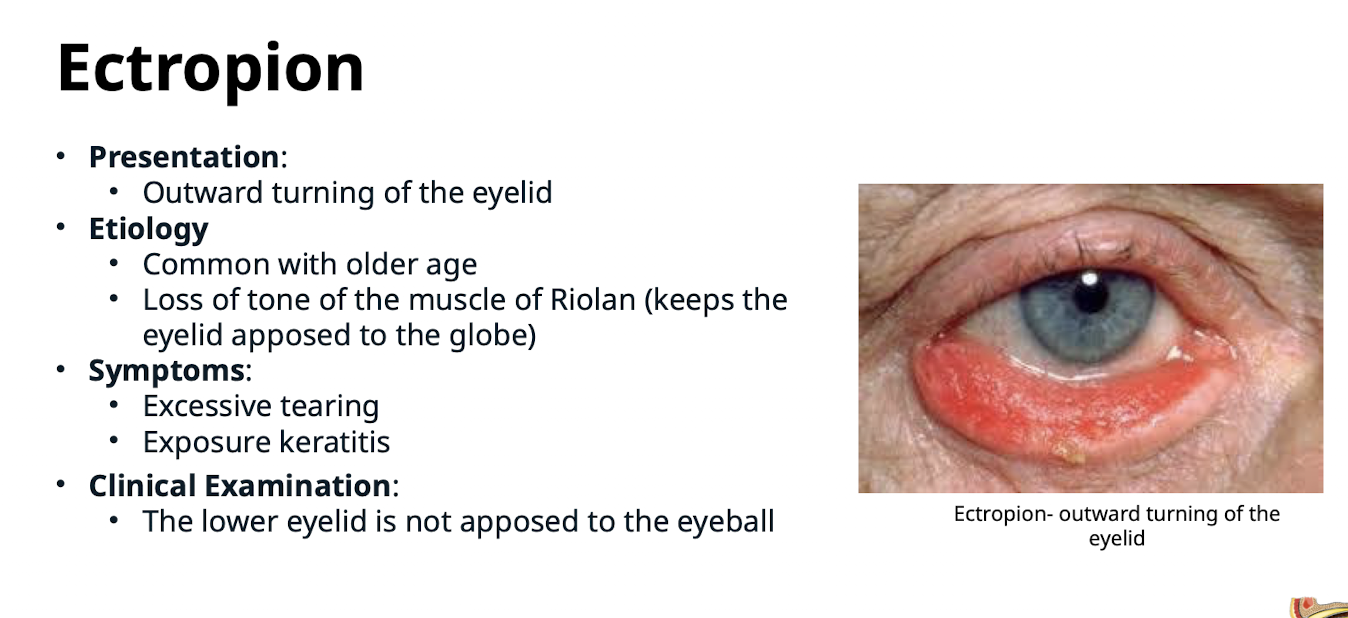
What is the key finding in the clinical examination of Ectropion?
The lower eyelid is not apposed to the eyeball
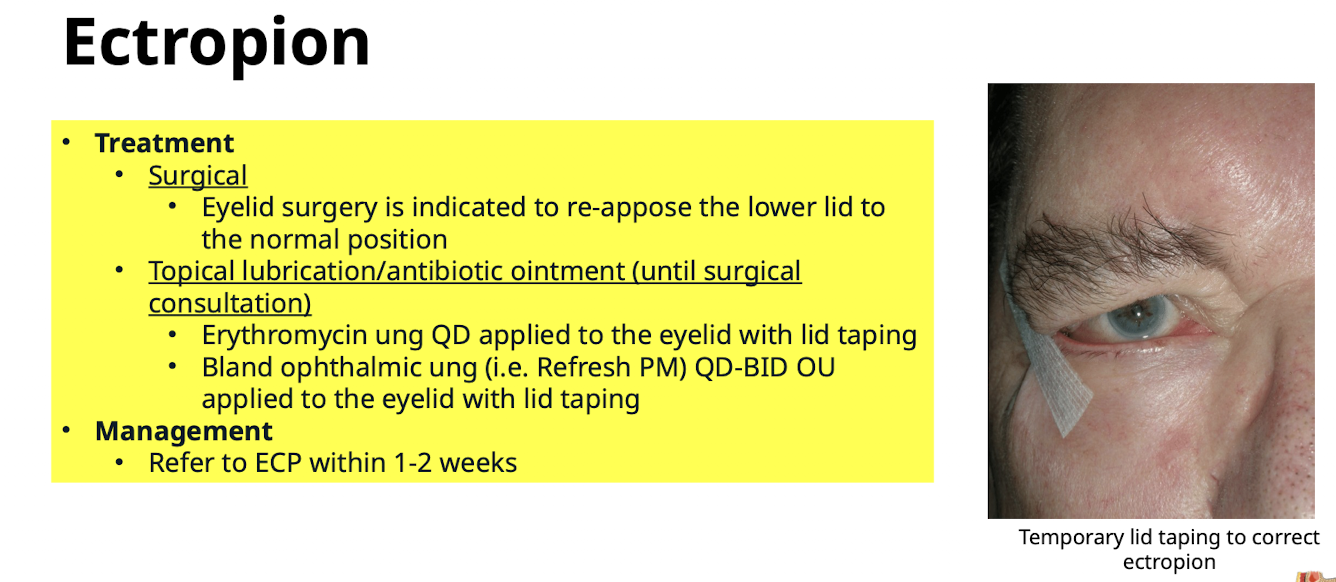
What is the definitive treatment for Ectropion?
Surgical; Eyelid surgery is indicated to re-appose the lower lid to the normal position
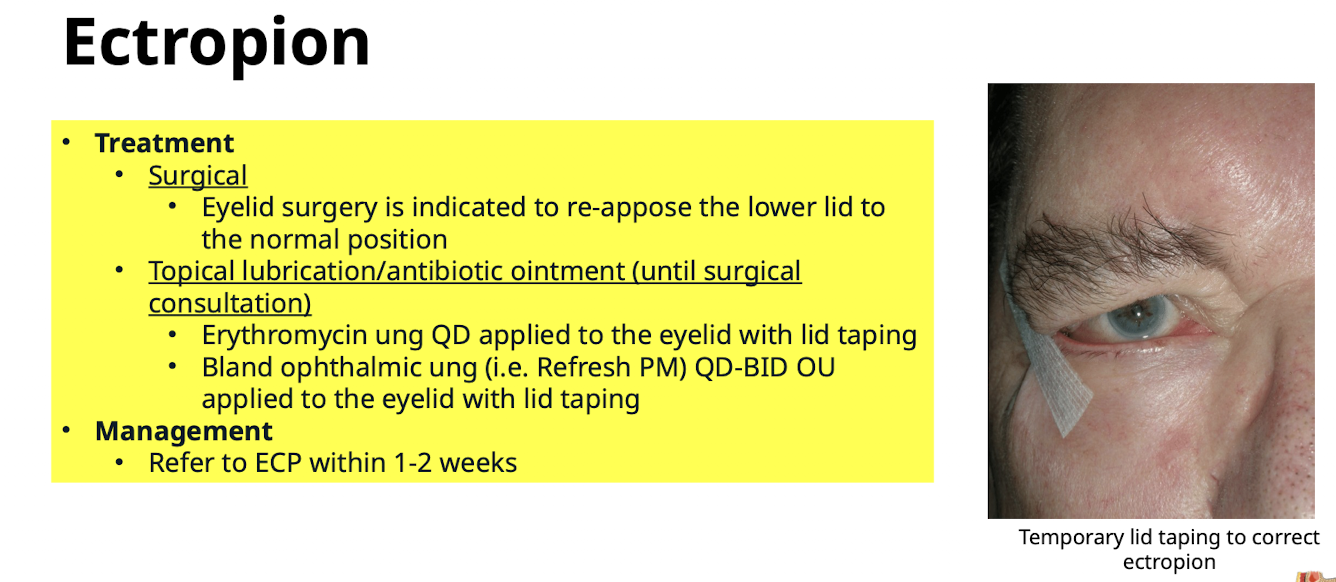
What temporary measures are used for Ectropion treatment until surgical consultation? What is the management?
Topical lubrication/antibiotic ointment (Erythromycin ung QD or Bland ophthalmic ung (i.e. Refresh PM) QD-BID OU) applied to the eyelid with lid taping. Refer to ECP within 1-2 weeks
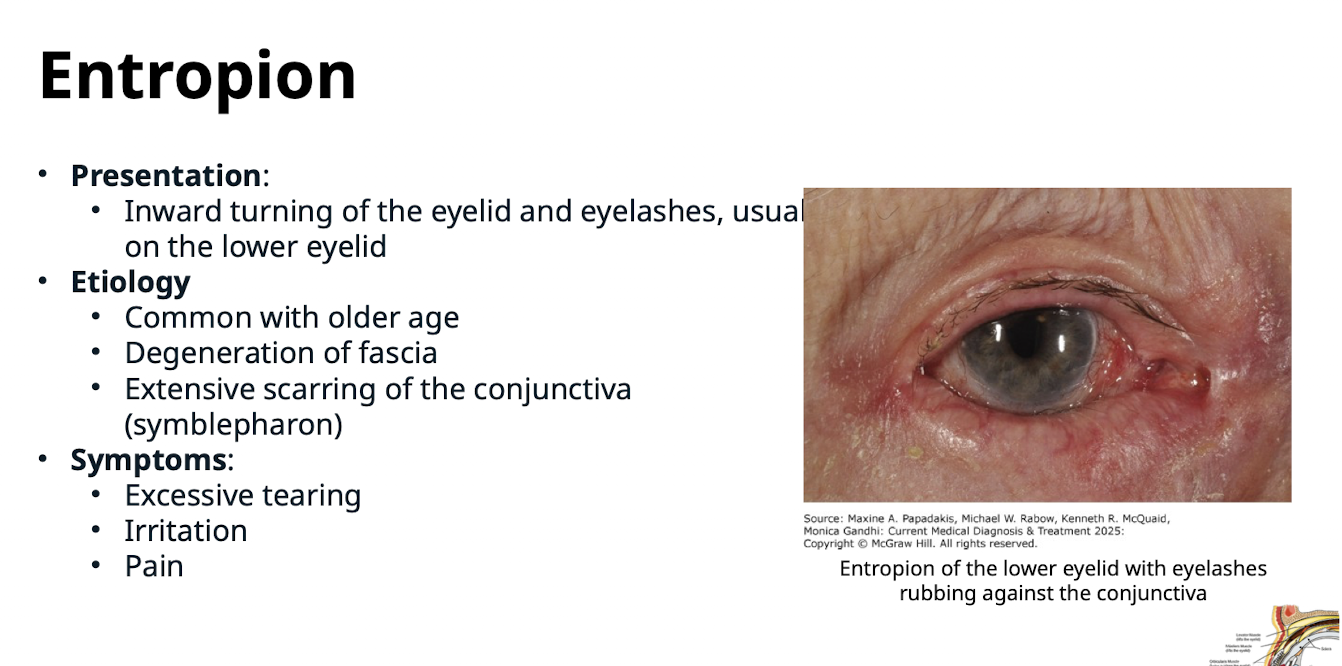
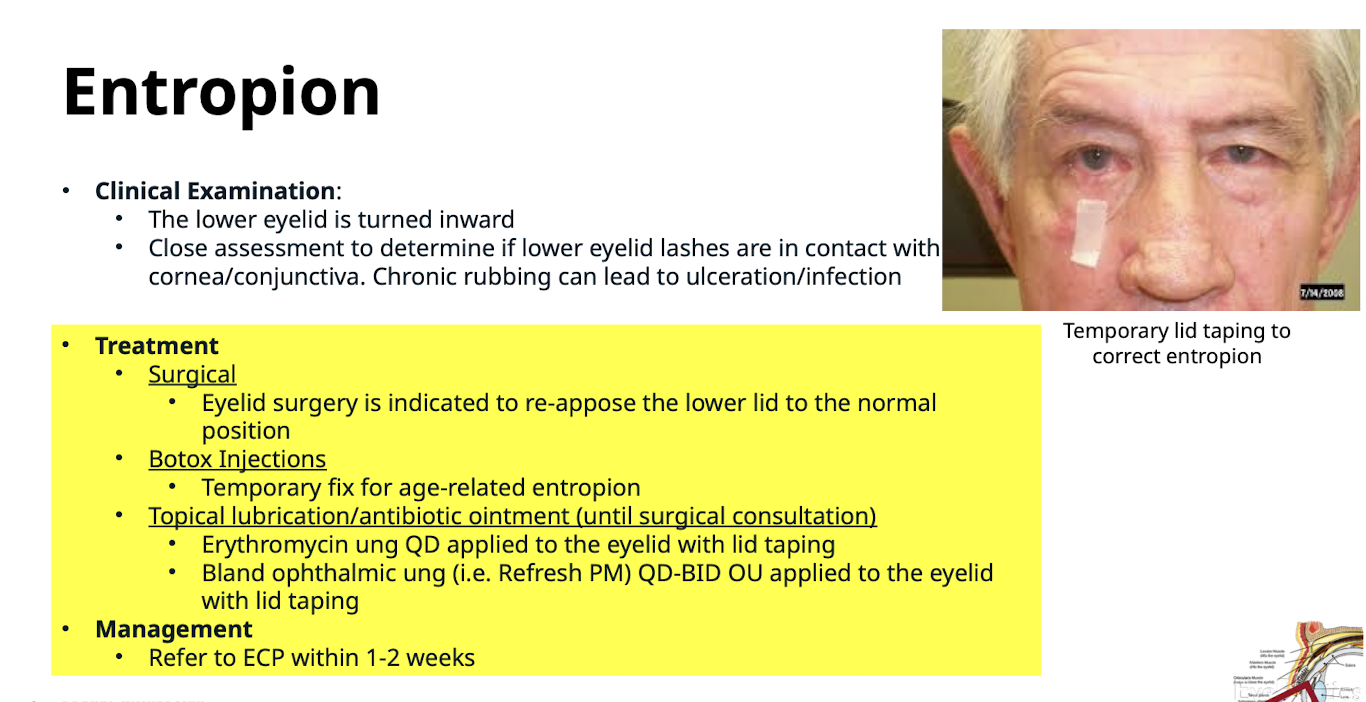
How is Entropion defined?
Inward turning of the eyelid and eyelashes; usually on the lower eyelid
What are the etiologies of Entropion?
Common with older age; Degeneration of fascia; Extensive scarring of the conjunctiva (symblepharon)
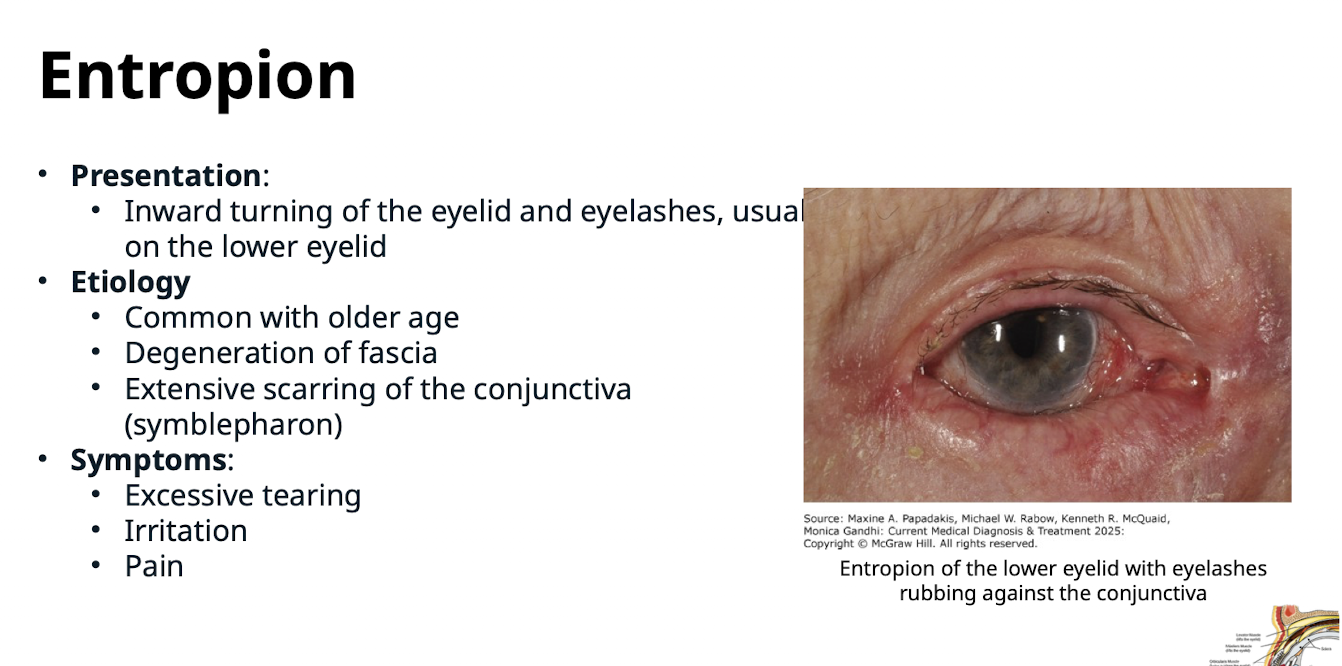
What are the symptoms of Entropion?
Excessive tearing; Irritation; Pain
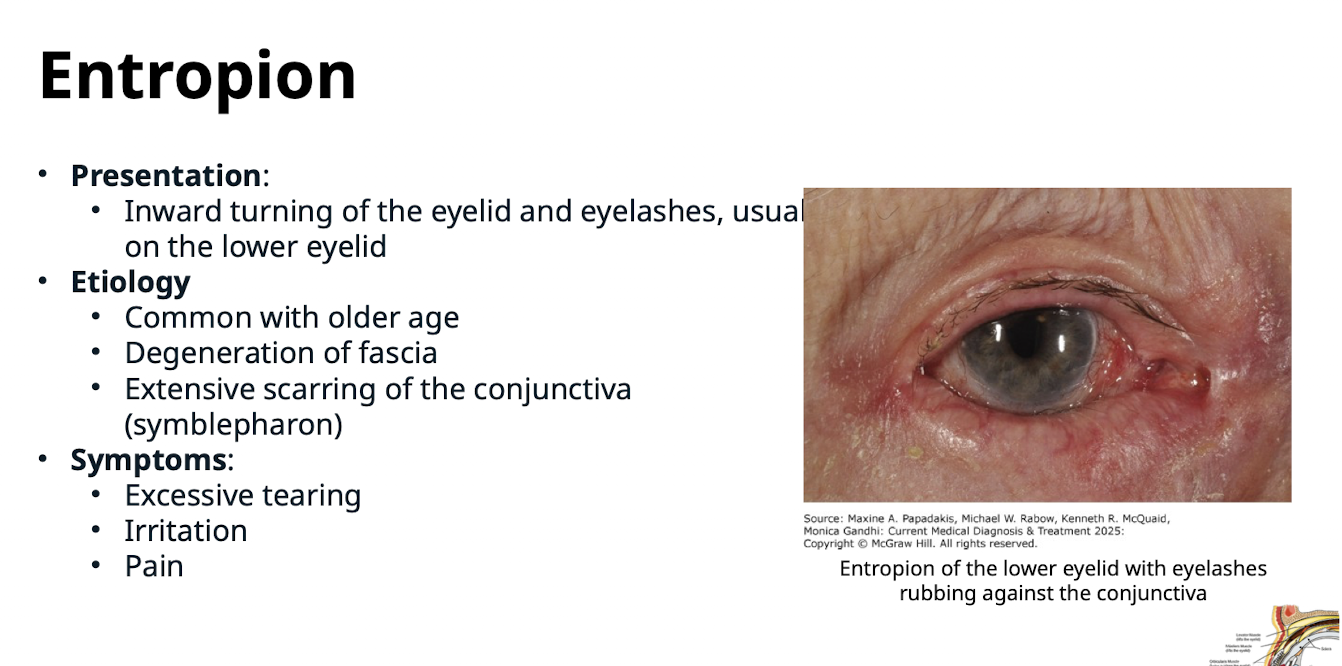
What risk is associated with chronic rubbing of lashes against the cornea/conjunctiva in Entropion?
Ulceration/infection
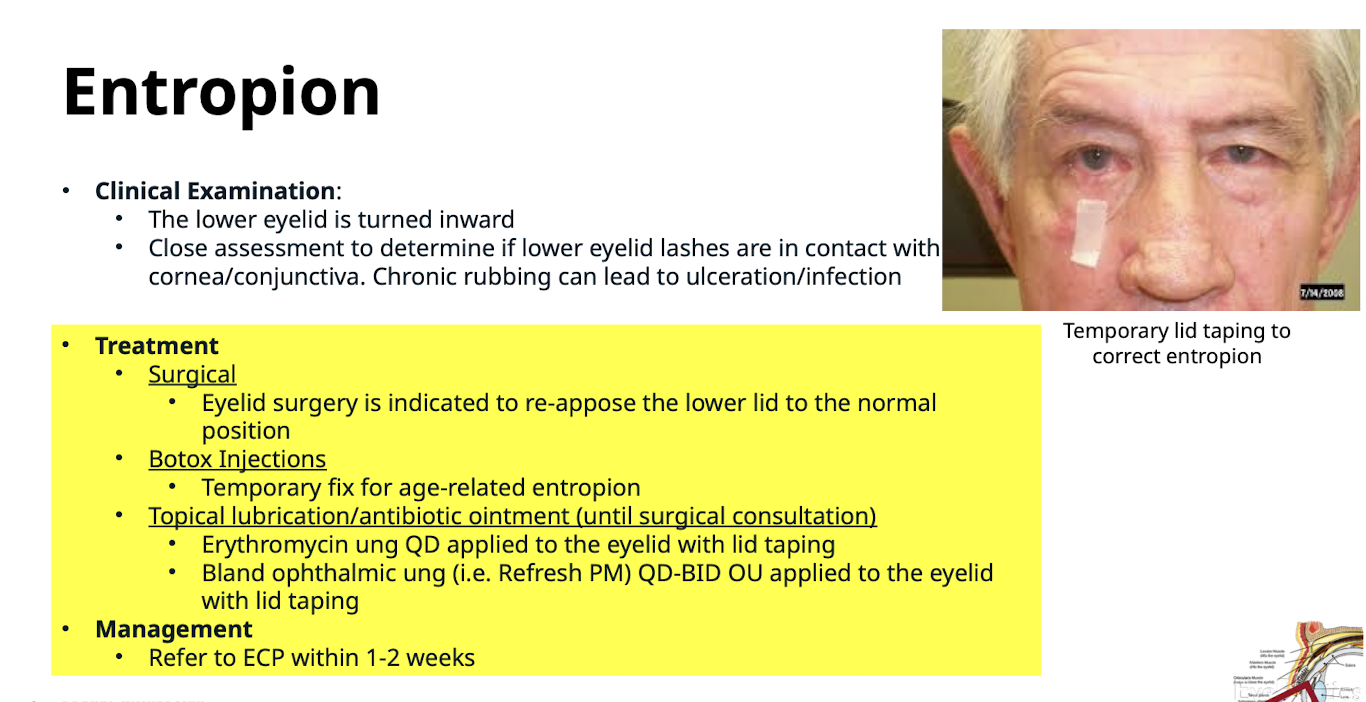
What are the treatment methods for Entropion? What is the management? Refer to ECP within 1-2 weeks
Surgical (to re-appose the lower lid to the normal position);
Botox Injections (temporary fix for age-related entropion); T
opical lubrication/antibiotic ointment (Erythromycin ung QD or
Bland ophthalmic ung (i.e. Refresh PM) QD-BID OU) applied to the eyelid with lid taping
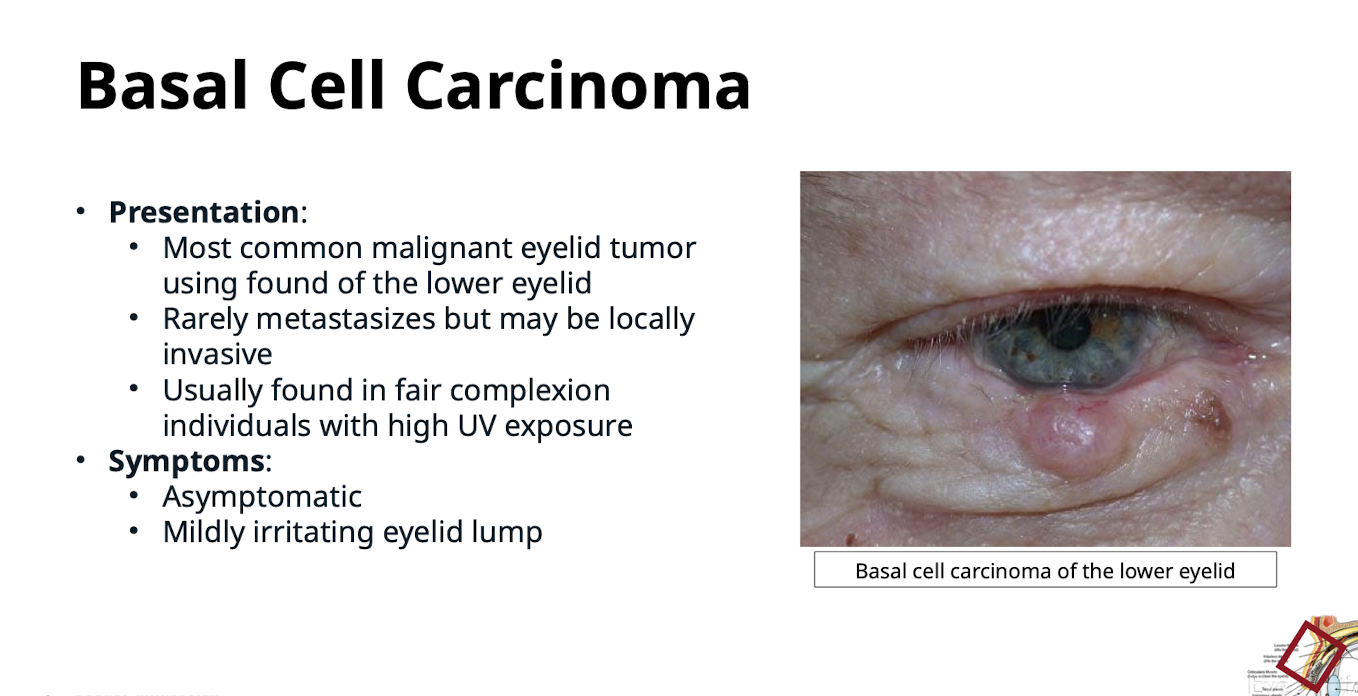
What is the most common malignant eyelid tumor?
Basal Cell Carcinoma (BCC)
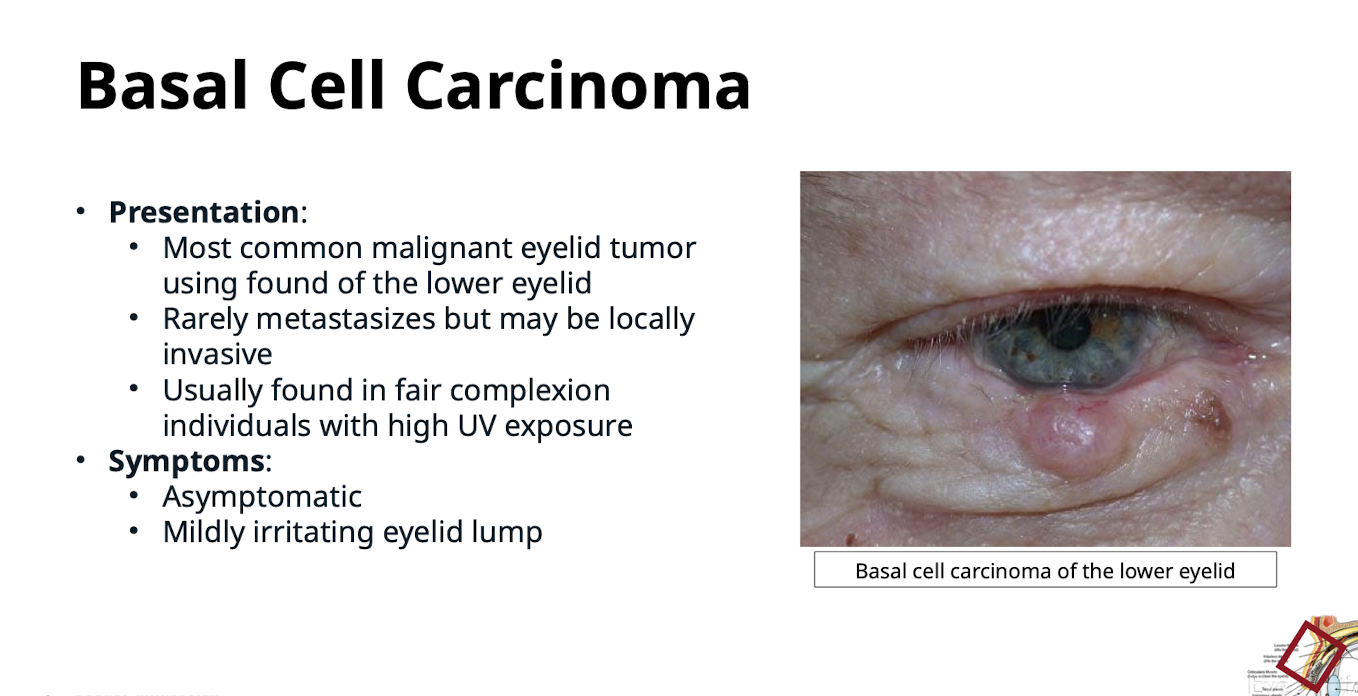
Where is Basal Cell Carcinoma typically found on the eyelid?
Usually found of the lower eyelid
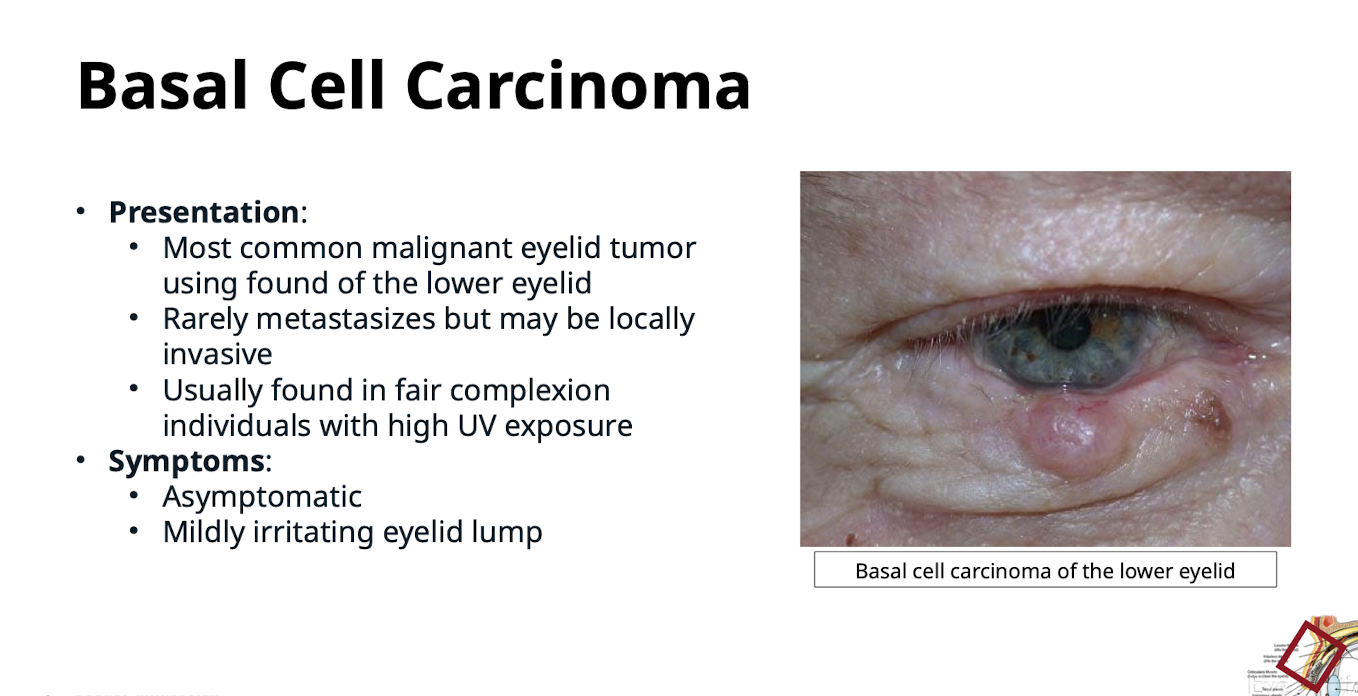
Describe the metastatic potential and invasiveness of Basal Cell Carcinoma.
Rarely metastasizes but may be locally invasive
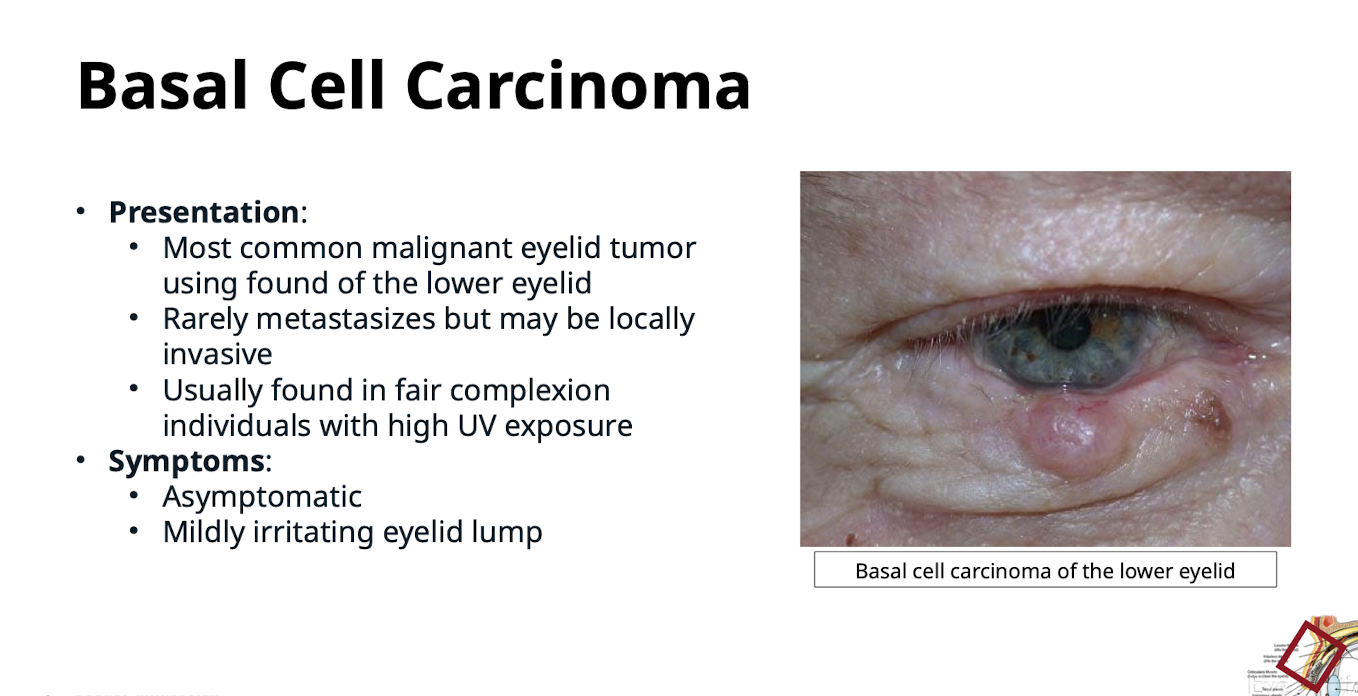
Who is at risk for a BCC of the eye and what are the symptoms?
Inidviduals of fair complexion and individuals with high UV exposure.
Usually asymptomatic or a mildly irritating eyelid lump
How does Squamous Cell Carcinoma (SCC) often appear on the eyelid?
Often appears like a basal cell carcinoma; has a variable presentation
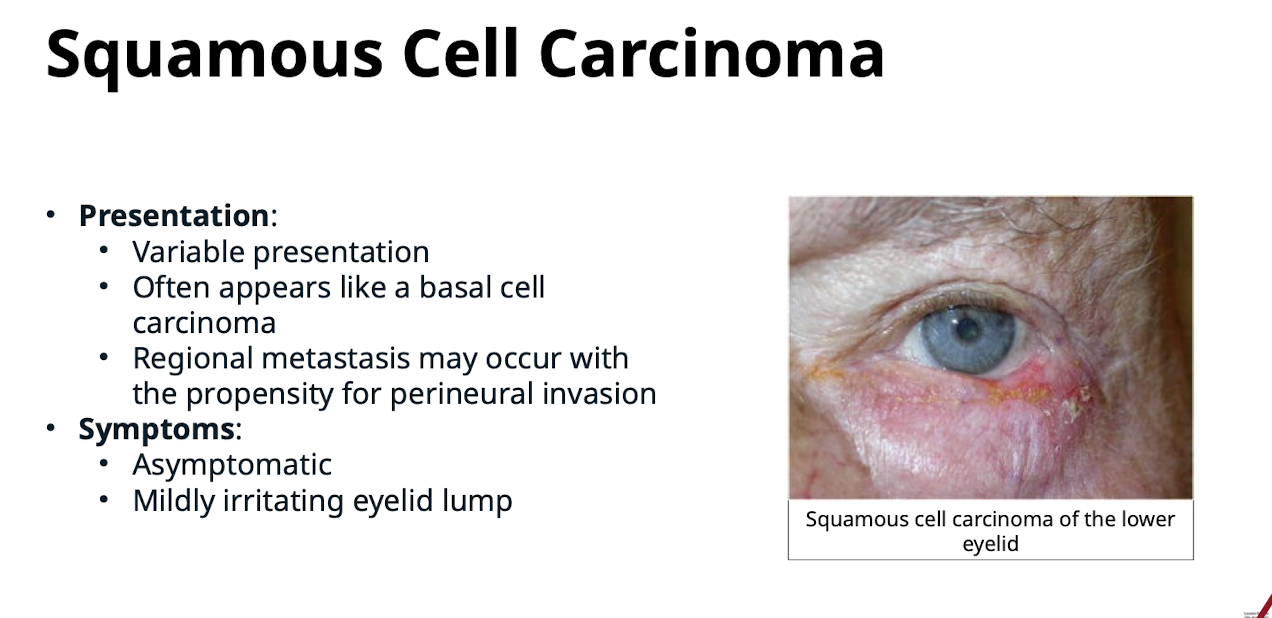
How do you tell the difference between a benign lump and malignant lump?
Does it change the shape of the eyelid margin? If eyelashes don’t grow out of it its bad, is it growing/changing
Describe the metastatic behavior of Squamous Cell Carcinoma. What are the symptoms?
Regional metastasis may occur with the propensity for perineural invasion. Usually asymptomatic or a mildly irritating eyelid lump
What is Sebaceous Cell Carcinoma also known as?
Meibomian gland carcinoma
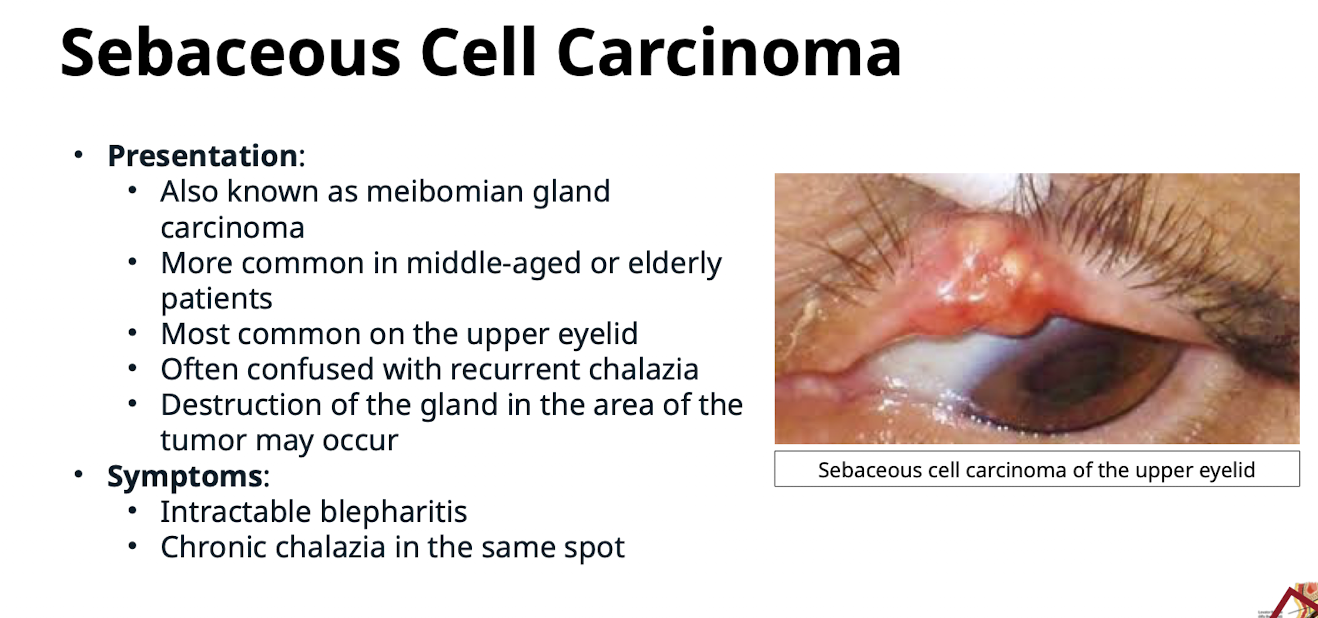
Where is Sebaceous Cell Carcinoma most common? What demographic?
On the upper eyelid. Middle aged or elderly patients
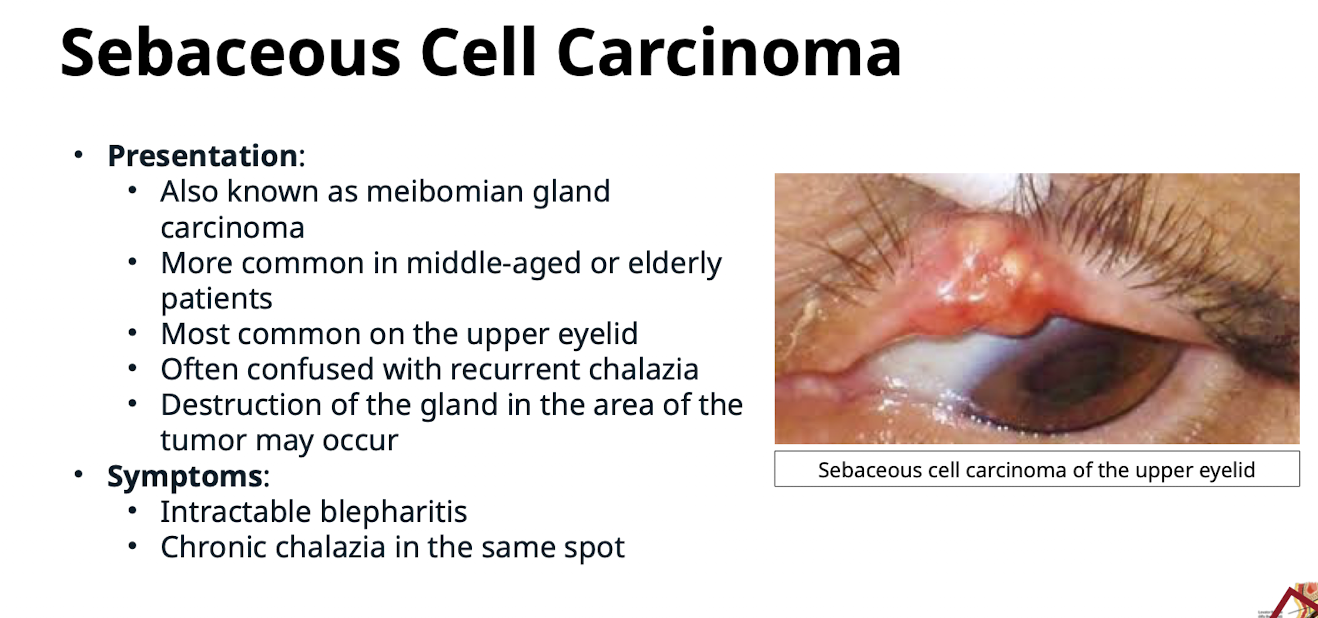
With what common eyelid condition is Sebaceous Cell Carcinoma often confused?
Recurrent chalazia. Destruction of the gland in the area of the tumor may occur.
What symptoms are associated with Sebaceous Cell Carcinoma?
Intractable blepharitis; Chronic chalazia in the same spot
What history elements are important when examining an eyelid tumor?
Duration; Rapid or slow growth; Bleeding
How is metastasis evaluated during the clinical examination for eyelid tumors?
Palpate preaurical; submaxillary and cervical lymph nodes
What local signs indicate concern for malignancy in an eyelid tumor?
Loss of eyelashes; changes in the eyelid architecture
What surgical techniques are used to treat eyelid tumors?
Excision and biopsy; May need to employ Mohs surgical technique
What is the management plan for suspected eyelid tumors?
STAT referral to Oculoplastics surgeon
Anything lid related that needs cutting is oculoplastics not general ophthalmology