Exploring Biomedicine - Module 3 BIOM10002
1/142
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
143 Terms
Similarities between Bacterial and mt DNA
double membrane, circular supercoiled molecule, undergoes reproduction via fission
mt DNA in humans
37 genes: 2 rRNA, 22 tRNA, 13 protein genes - some subunits of complexes are coded by nuclear genes. Maternally inherited, possessed in multiple copies
heteroplasmy
not every mitochondrial DNA in a given cell is the same - mitochondria typically have a mix of nonuniformly distributed normal and abnormal tissue
mtDNA protein transport systems
SAM, OXA1
Production of mitochondrial proteins
occurs via translation by ribosomes in the matrix
Eurkaryotic DNA features
protein-bound, linear, contains introns
Eukaryotic organelle features
contain nucleus, membrane bound organelles, 80S ribosome (subunits 40s and 60s, 1:1 rNA to protein)
Roles of the Mitochondria
producing ATP via oxidative phosphorylation, buffering calcium ions, Fe-S cluster biogenesis, regulation of cell dealth, immune signalling
Endosymbiosis
Modern mitochondria arose from oxygen breathing bacteria: large host cell and ingested bacterium become dependent on each other for survival
Faculative endosymbiosis
inclusion of an autonomous partner
Obligate endosymbiosis
central control, nuclear integration, cell-cycle synchronisation
Endosymbiotic Organelle
obligate codependency - cannot live independently
Nuclear DNA in mitochondria
only 13 proteins coded for in mt. all other required proteins come from outside mitochondria due to endosymbiosis transfer of mitochondrial genome
Nuclear encoded precursors
Synthesised on cytosolic ribosomes and delivered to mitochondria due to targeting sequences. Entry to mitochondria mediated by translocase enzymes.
Membrane proteins in Mitochondria
TOM: translocase of the outer membrane
TIM: Translocase of the inner membrane
SAM: sorting and assembling machinery
OXA1: oxidase assembly protein 1
SAM and OXA conserved proteins from bacterial origins
Mitochondrial Proteome
the entire set of proteins that can be expressed by the genome (including the mitochondrial genome) and is targeted to the mitochondria
Cellular Respiration
C6H12O6 + 6O2 = 6CO2 + 6H2O + ATP
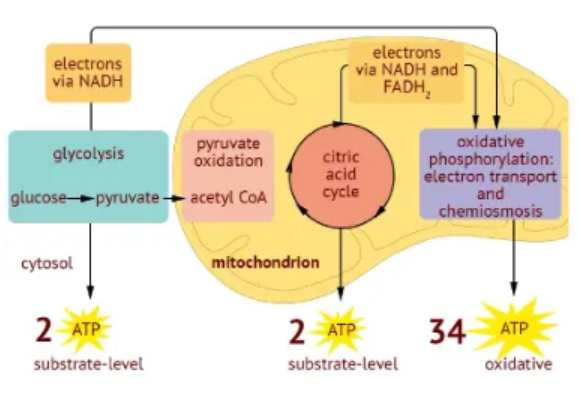
Glycolysis
converts the six-carbon glucose to 2 molecules of the three-carbon pyruvate + 2 net ATP, 2 NADH, and 2 H2O. Pyruvate travels to mitochondrial matrix and is converted to 2-carbon acetyl CoA.
Citric Acid Cycle
Oxidation of acetylCoA within 8 steps. End products after 2 rounds = 2 ATP, 6 NADH, 2 FADH2, 4CO2

Oxidative Phosphorylation
redox reactions generate energy (ETC) which is captured in a proton gradient to produce ATP (chemiosmosis). proteins pumped from intermembrane space to inner membrane driving synthase motor (Complex 5). Produces 32-34 ATP, 10 NAD+, 2 FAD, 6 H2O
Mitochondrial Diseases
long-term, genetic, oft-inherited disorders that occur when the mitochondria fail to produce enough energy for the body to function properly.
Heterogeneity of MD
Clinical presentations and genetic causes of MD can be very different - >280 genes linked to MD.
Origins of MD
mutations can be inherited from parents or occur for the first time in a child - de novo
Clinical features of MD
encephalopathy, neuropathy, stroke-like episodes, hemiplegia, myoconic epilepsy, loss of muscle coordination, myopathy, deafness and blindness, lactic acidosis
Areas of MD effect
tissues heavily reliant on oxidative metabolism: central nervous system, peripheral nerves, the eyes, skeletal and cardiac muscle, endocrine organs
Primary MD
genes with a primary link to the function of the ETC, including mtDNA mutation
Secondary MD
genes with an indirect function on the ETC, or another mitochondrial function
Diagnosis of MD
initial biochemical tests - lactate and pyruvatem cerebrospinal fluid, amino/organic acids.
neuroimaging, electromyography, nerve conduction studies
genetic studies - albeit expensive. typically confirmation of well-suspected mitocondrial origin
muscle and tissue biopsies - less tolerated, less comprehensive
Functional Tests in MD
used to differentiate PMD and SMD as cannot be determined with lab tissue testing alone - RNA sequencing, quantitive proteomics, metabolomics
OMICS
analysis of large amounts of data representing an entire set of some kind e.g. genome, proteome, lipids, metabolome - systems perspective
mtDNA mutation
occurs due to random partitioning of mitochondria between dividing cells - daughter cells recieve non-identical copies of mtDNA. Heterogeneity leads to higher mutation rate.
Maternal mtDNA
Mitochondrial DNA is only recieved maternally as the mitochondria in sperm cells is destroyed post fertilisation
MELAS - Mitochondrial Encephalomyopathy, Lactic Acidosis, Stroke-like Episodes
a rare primary MD beginning in childhood, affecting the brain and nervous system, and the muscles. Caused by mutations in mtDNA gene MT-TL1 responsible for making tRNA to transport Leucine (UUR)
Sengers Syndrome
Secondary MD caused by mutation in acylglyerol kinease (lipid kinease) - responsible for import and assembly of mt carrier proteins and the TIM22 complex
Autosomal recessive - alleles must be homozygous
Respiratory Chain Enzymology Assays
identify malfunctioning electron transport chain complexes to support clinical evaluation of a defect in energy production.
Mitochondrial Replacement Therapy
A potential treatment for mitochondrial disease involves three-parent IVF, where a donor is used to supply healthy mitochondria to a parent couple.
Mito Cocktail
mixture of medications to optimise nutrition and general health - preventing deterioration of symptoms. ubiquinone, L-carnitine, B1 & B2, folic acid
Order of gastrointestinal tract
mouth - esophagus - stomach - small intestine (duodenum, jejunum, ileum) - large intestine - rectum - anus
Gastrointestinal tract
An open tube exposed to external environment, part of the digestive system. sections are anatomically quite similar but possess different characteristics, due to their function as specialised sections for uptake of different components
Nutritions and the GI tract
Stomach: water, ethyl alcohol, copper, iodide, fluride
Duodenum: calcium, phosphorus, magnesium ion, folate, some vitamins
Jejenum: many vitamins, iron, zinc, maganese, lipids, monosaccarides, amino acids
Ileum: other vitamins, depending on transit time
Large intestine: water, vitamin K, sodim, chloride, potassium
Composition of the Gut
muscosal tissue and smooth muscle. Protusions of villi allow for increased surface area
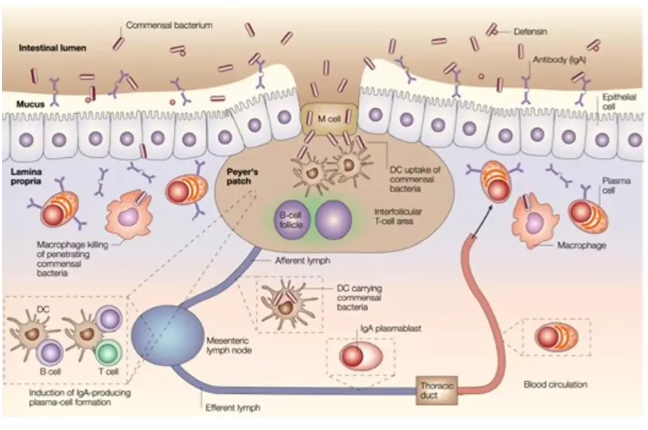
Peyer’s patches
specialised structures where immune cells are located in the gut that allow for fine-tuned interaction and monitoring
Microbiota in the gut
many non-damaging and tend to occupy the space without causing damage to the host - can be aerobic or anaerobic. Largest diversity in the large intestine
Functions of gut microbiota
Protective: production of anti-microbial factors, receptor competition, nutrient competition, pathogen displacement
Structural functions: barrier fortification, stimulation of IgA production, apical tightening of tight junctions
Metabolic functions: control epithelial cell differentiation/proliteration, metabolism of dietary carcinogens, synthesise vitamins, ferment non-digestible residue, ion absorption
Harmful Gut Microbes
Bacteria: salmonella enterica, e. coli
Viruses: norovirus, rotovirus
Parasites: giardia intesinalis, entamoeba histolytica
Pathogenic Traits
promoting colonisation in sterile locations, excessive occupation of specific niches, antagonising host defences, facilitating spread of microbes
Mechanism of Infection
Encounter - arrival of microbe to site
Entry - binding to receptor, triggering uptake mechanisms
Replication - utilising host resources for multiplication
Spread - release of new progeny, causing damage
Gastrointeritis
any inflammation of the gastrointestinal tract. Symptoms include diarrhoea, vomiting and abdominal cramping. Typically self-limiting (repairs itself with time). Can be infectious or non-infectious (caused by host response)
Invasive Gastroenteritis
infection causes inflammation of the gut that results in breaching of the epithelial lining. Leads to vomiting, fever, abdominal pain and bloody diarrhoea due to blood vessel damage
M cells
specialized epithelial cells in the intestine that act as a crucial part of the immune system by sampling antigens and pathogens from the gut and transporting them to underlying immune cells.
Sources of Invasive Gastroenteritis
Food safety risks - faecal-oral transmission and poor food handling
Salmonella
subspecies of bacteria which cause salmonellosis. Causes either enteric fever or non-typhoidal salmonella
Enteric fever
non-self-limiting, more severe than NTS. Incubation period of 7-14 days. Requires antibiotic treatment. Vaccination available in endemic areas
Non-typhoidal salmonella
Natural hosts of food animals, reptiles and insects - zoonotic. Incubation period of 6-12 hours. Typically self-limiting
Salmonella infection
occupy the extracellular niche of gut luminal space. Can breach epithelial layer through multiple routes and drain to lymph nodes,causing systematic infection. Able to replicate intracellularly and in typically sterile sites
Non-invasive gastroenteritis
inflammation of the gut without the breaching of the mucosal layer. caused by bacterial toxins which are released over the course of infection. Typically self-limiting
Clostridiodes Difficile
A hospital pathogen that typically florishes following wide use of antibiotics. Entirely toxin medicated. Toxins A & B are taken up by colonic epithelial cells, causing cell death, damage, inflammation and fluid accumulation.
Bacillus Cereus
Spore forming bacterium commonly found in soil/on vegetables. causes emetic or diarrhoeal foodborne illness dependent on type of bacterual toxins
Bacillus Cereus - Emetic Toxins
cause emetic syndrome involving ingestion of pre-formed toxin that leads to the destruction of the mitochondria within infected cells. heat-stable and pH resistant. Activates receptors that stimulate the major nerve controlling stomach function
Bacillus Cereus - Enterotoxins
Cause diarrhoeal syndrome involving the production of enterotoxins following ingestion. Pore-forming toxins, e.g. Hbl and Nhe, cause holes in host cell membranes, inducing cell death and leading to fluid accumulation in the ileum.
Homeostasis
The maintanence of a stable internal environment involving the regulation of temperature, pH, ions, and solvents (polar molecules), all of which can disrupt hydrogen bonds and cause denaturation.
Feedback loops
require the transmission of an input from a receptor to a control center, which directs to effector to produce a certain output. Negative Feedback is self regulatory and helps to maintain a level, while positive feedback amplifies a response.

Process of homeostasis
stimulus produces change in variable
change detected by receptor
information sent along afferent pathway to control centre
information sent along effect pathway to effector
response of effect influences magnitude of stimulus
Blood glucose - Negative Feedback
When blood glucose levels are too low, the pancreas is stimulated to release glucagon which allows stored glycogen in the liver to be released into the blood.
When blood glucose levels are too high, the pancreas is stimulated to release insulin which allows glucose to be removed from the blood via the liver storing it as glycogen
Blood Pressure - Negative Feedback
When mean arterial pressure increases, the heart is stimulated to decrease heart rate and force of heart muscle contraction, and blood vessels are stimulated to dialate. This causes a decrease in MAP.
When mean arterial pressure decreases, the heart is stimulated to increase heart rate and force of heart muscle contraction, and blood vessels are stimulated to contract. This causes a increase in MAP.
Visceral information
Sensory or motor information related to internal organs and smooth/cardiac muscle. Information that is subconscious. Includes homeostatic reflexes.
Somatic Information
sensory or motor information related to the body wall and movement of limbs/joints - conscious information and voluntary movement
Ligands
hormones and neurotransmitters - chemical signalling molecules involved in
Neurotransmitters
Ligands released in small packets at the synapse. They are action discrete - restricted to receptors at the synapse.
Noradrenaline
a neurotransmitter released by the sympathetic nervous system to evoke fear, flight or fight responses. Activates adrenergic receptors.
Endocfrine hormones
released into the circulatory system. Action may occur on any cell in the body with a receptor for the particular ligand.
Adrenaline
a hormone secreted by the adrenal gland under sympathetic control. Activates adrenergic receptors.
Thyroid hormone
a hormone secreted by the thyroid gland under hypothalamic regulation. Increases energy expenditure (heat production).
Circadian Rhythm
24-hour cycles that are part of the body’s internal clock that run in the background carrying out essential functions and processes, resulting in changes of levels of arousal and attention
Changes in body temperature
Body temperatures are higher in the day and fall towards the sleep period. When temperature falls below a certain point, sleep is initiated.
Plasma glucose levels and cortisol levels also follow similar patterns.
Methods of heat exchange
radiation - heat transfer via electromagnetic waves
evaporation - heat transfer via conversion of water to vapour
convection - heat exchange with surrounding medium
conduction - heat exchange with another object
Non-shivering Thermogenesis
sympathetic regulation that occurs by increased use of energy within the body in cold environments. e.g. generation of heat via brown adipose tissue (BAT) where mitochondrial burn fuel to directly produce heat rather than creating ATP
Shivering thermogenesis
somatic regulation that occurs by contractions of muscles within cold environments. i.e. signalling via the hypothalamus for rapid muscle contraction, burning ATP and creating heat
Four Thermoregulatory Strategies
non-shivering thermogenesis, shivering thermogenesis, vasoconstriction/dilation, water evaporation
Fever
an adaptive response to infection that involves the alteration of core body temperature via reflex.
Infection agents activate the immune response, which results in the release of inflammatory mediators.
Prostaglandin is produced and carried by the blood to the hypothalamus.
An alteration in neuronal activity adjusts for the altered set point.
Pyrogens
agents that incite the fever response.
Impact of fever
Fever helps slow viral replication rate by raising the body’s temperature above their optimal operating temperature.
Certain proteins within the immune system operate better at higher temperature than normal, allowing for an adaptive advantage as they are selectively activated during infection.
Sepsis
an uncontrolled inflammatory response, resulting in excess high temperature that can lead to organ damage.
Responses to temperature
Changes in core body temperature are sensed in the hypothalamus and evoke unconscious visceral responses.
Changes in ambient temperature lead to conscious awareness of thermal discomfort, resulting in behavioural responses.
GI Semi-Permeability
Pros: efficient nutrient absorption, controlled permeability, immune surveillance, microbial homestasis, detoxification
Cons: vulnerability to barrier dysfunction - “leaky gut”, entry point for pathogens, allergen exposure, limited defence
Intestinal Epithelial Cells
form the first physical barrier (tight junctions). produce mucins and antimicrobial enzymes (defensins, lysozymes). act as sentinels with pattern-recognition receptors
Globlet cells
Secrete mucus, forming a protective layer on epithelial surfaces to limit microbial contact
Dendritic cells
Sample antigens from the lumen (e.g. via M cells), present antigens to T cells in Peyer’s patches
Macrophages
Phagocytose pathogenic bodies and maintain gut microbiota balance
M cells
specialised epithelial cells found in Peyers patches that assist in antigen sampling and transport to immune cells
The respiratory system
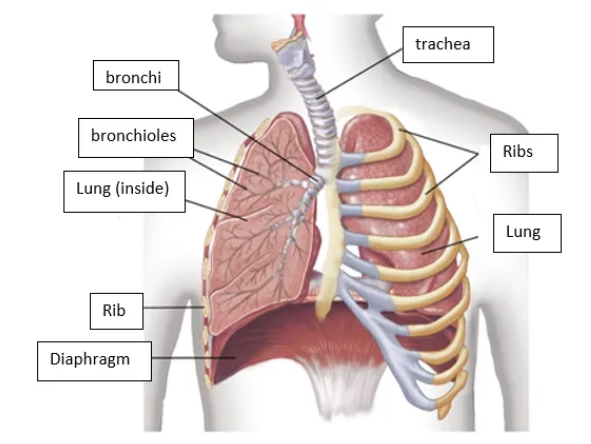
Purposes of the Respiratory System
transfer oxygen from the environment to red blood cells
transfer carbon dioxide from blood to the air
regulate acid-base balance
The Bronchial System
formed from 22 divisions of the trachea. composed of cartilge, connective tissue, and smooth muscle
Asthma
a disease of the conducting system which leads to variable airflow obstruction, characterised by inflammation and thickening of the airway membrane
Triggers of asthma
air pollution - bushfire smoke, allergens - house dust mite, grass pollens, exercise, viral infections, cigarettes
Spirometry
A measurement of lung performance. Inspiration and expiration are measured on a graph of volume vs time. Asthma is characterised by reduced airflow on expiration
FEV1 value
The amount of air blown out in one second - a measure of how quickly air can leave the lungs. Typically 70-80% of forced vital capacity.
FEV1 in asthma is reduced to <80% of what is predicted.
Forced Vital Capacity
Total volume of air that can be forcibly exhaled after a deep inhalation.
Allergic Asthma
Most cases are eosinophilic, with allergic cells appearing in sputum. Blood eosinophil count can be used to approximate sputum eosinophil count.
Allergens are inhaled and make contact with the respiratory epithelium.
They are picked up by dendritic signalling cells and presented to naive T cells, creating a cell-mediated immune response, as well as to B cells to produce antibodies.
Histamine released by mast cells leads to restriction of the airways and recruitment of eosinophils.
Non-Allergic Asthma
Pollutants such as fungi or cigarette toxins activate innate lymphoid cells which leads to bronchial hyperreactivity and the recruitment of eosinophils.