Chapter 20: Reproduction
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
64 Terms
Some Terminology (Next 7)
1. Gonads
2. Gametes
3. Gametogenesis
4. Gonadotropic Hormones
5. Gonadal Steroids
6. Meiosis
7. Mitosis
Gonads
☆ Testis & ovary
Gametes
☆ Sperm & egg
Gametogenesis
☆ Spermatogenesis (production of sperm) and oogenesis (production of egg)
Gonadotropic Hormones
☆ FSH (follicle-stimulating hormone), LH (luteinizing hormone)
Meiosis
☆ Chromosomes replicate and recombine, followed by two successive cell divisions resulting in 4 daughter cells, each with half the number of chromosomes (haploid) of the parent cell
- Occurs in gonads and creates gametes only
Mitosis
☆ Chromosomes replicate, followed by cell division that results in 2 daughter cells with the same number of chromosomes (diploid) of the parent cell
- Daughter cells are genetically identical
- Creates all bod cells besides gametes
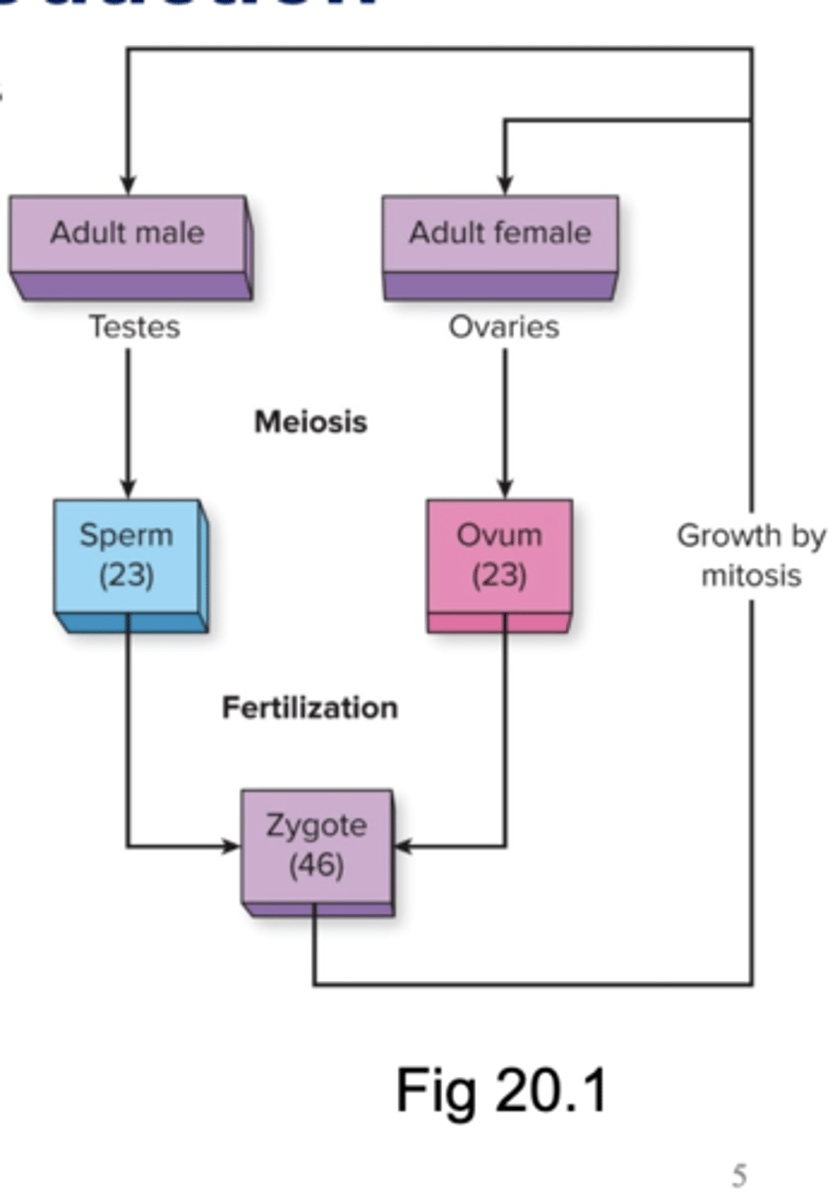
Sexual Reproduction Pt. 1
☆ In sexual reproduction, genes from two individuals are combined in random and novel ways with each new generation
- In each cell, there are 23 pairs of chromosomes, with one chromosome from each parent in each pair (46 chromosomes total in each cell)
- An individual's DNA is contained in these 46 chromosomes
- Except for sex chromosome, each pair contains two homologous chromosomes, meaning they look like each other and contain similar genes
- Cells that contains 46 chromosomes (23 pairs) are called diploid
- Cells that contains 23 chromosomes are called haploid
Sexual Reproduction Pt. 2
☆ At puberty, meiosis in the gonads results in gametes (sperm, egg)
- Each gamete is unique and has 23 chromosomes (haploid)
☆ During fertilization, sperm cell and egg cell fuse to produce a fertilized egg (zygote), which is diploid
☆ Mitotic cell divisions underlie the growth of the zygote into an adult
- In mitosis, two genetically identical diploid "daughter" cells are produced
Sex Determination
☆ Pairs 1-22 are autosomal (numbered)
☆ Pair 23 is the sex chromosome
- X from mother
- X or Y from father
☆ Female: XX
☆ Male: XY
Reproductive Endocrinology
☆ During puberty, gonads secrete more sex steroid hormones, due to stimulation by gonadotropic hormones (FSH, LH) from anterior pituitary gland
- Testosterone
- Estrogen
- Progesterone
☆Three-Hormone Sequence:
GnRH --> FSH and LH --> gonads secrete sex hormones and undergo gametogenesis
☆ Secretion of gonadotropins and sex hormones in females is cyclical (menstrual cycle)
Male Reproductive System (Next 6)
1. Semen
2. Testes
3. Accessory Organs
Semen
☆ Composed of sperm and fluids from testes, the epididymis, the seminal vesicles, and the bulbourethral and prostate glands
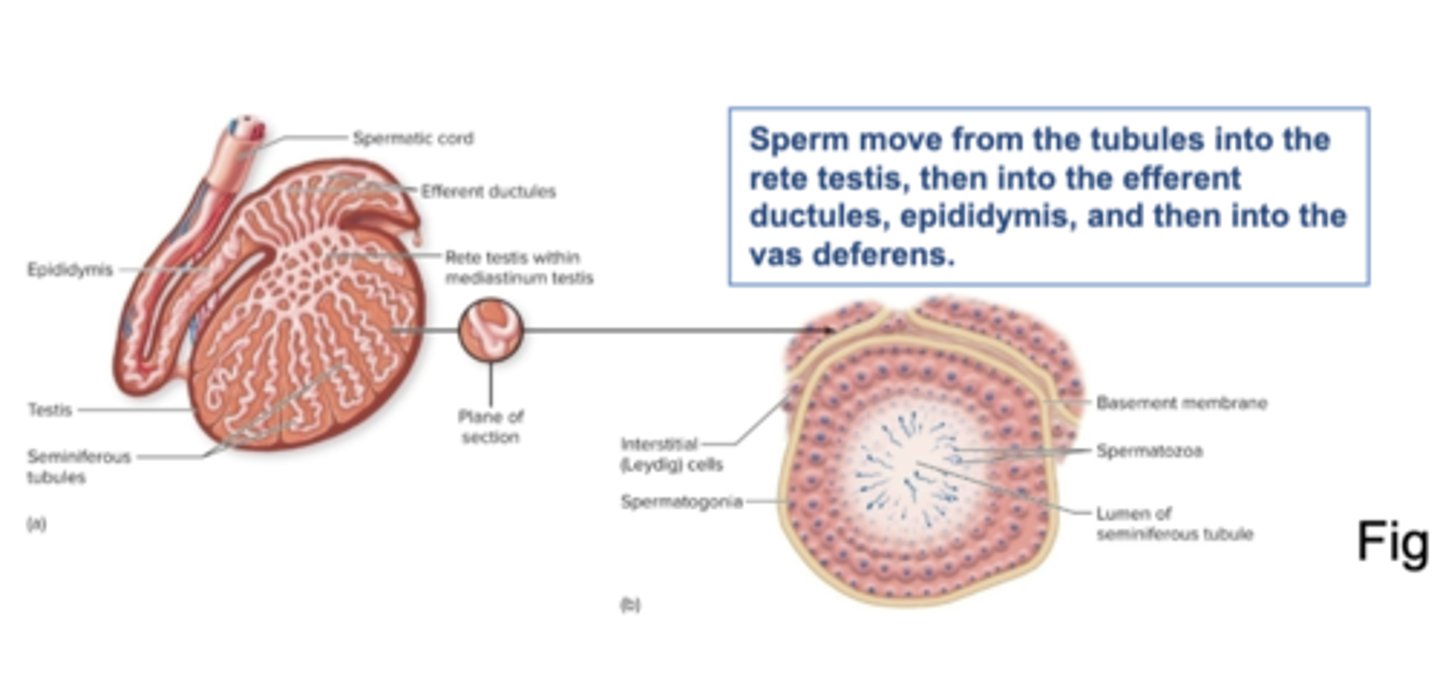
Testes
☆ Two main types of structures:
1. Seminiferous Tubules:
- Sertoli cells: spermatogenesis & secretion of inhibin (inhibits secretion of FSH)
2. Leydig or interstitial cells (between tubules):
- Secretion of testosterone
☆ Sperm move from the tubules into the rete testis, then into the efferent ductules, epididymis, and then into the vas deferens
Accessory Organs
1. Duct System
2. Glands
3. Secondary Sexual Structures
Duct System
☆ Epididymis, vas deferens, ejaculatory ducts, urethra
Glands
☆ Seminal vesicles, prostate gland, bulbourethral gland
☆ Secrete fluid component of semen, in which sperm is suspended
Secondary Sexual Structures
☆ Penis, scrotum
Hormonal Control of Male Reproductive Function
☆ Note the different effects of FSH an d LH, both secreted by the anterior pituitary gland
1. FSH stimulates spermatogenesis and secretion of inhibin by Sertoli cells in seminiferous tubules, while LH stimulates Leydig cells to secrete testosterone
2. Testosterone has varied effects
Testosterone Actions
☆ Spermatogenesis
☆ Stimulates anabolism --> growth of muscles and other structures
☆ Increased testosterone secretion during puberty --> growth of accessory organs, larynx
Spermatogenesis (Next 4)
☆ Appx. 300 million sperm cells produced each day in seminiferous tubules
☆ Spermatogonia are in outermost region of seminiferous tubules (diploid, 2n)
1. Mitosis
2. First Meiotic Division
3. Second Meiotic Division
4. Spermiogenesis
Mitosis
☆ Spermatogonia duplicate via mitosis
- One daughter cell becomes primary spermatocyte (2n)
First Meiotic Division
☆ Primary spermatocye divides into two identical secondary spermatocytes, each with 23 chromosomes (n) (with 2 identical chromatids per chromosome)
Second Meiotic Division
☆ Results in spermatids (n)
Spermiogenesis
☆ spermatids transform into spermatoza (sperm cells) (n)
Seminiferous Tubule and Sertoli Cells
☆ Sertoli cells in the tubule wall support spermatogenesis and protect developing sperm in the seminfierous tubules
Female Reproductive System (Next 5)
☆ Spermatozoan ejaculated into the female reproductive tract must move through the cervix and uterus before it can fertilize and ovulated egg
1. Ovaries
2. Accessory Organs
Ovaries
☆ Oogenesis
☆ Synthesize and secrete estrogen, progesterone, inhibin
☆ Ovarian (monthly) cycle:
- Developmental sequence w/ovulation of one ovum and some follicular cells per month
Accessory Organs (Female)
☆ Oviducts/Fallopian Tubes/Uterine Tubes
- Transport released ovum plus some follicular cells via ciliary action and smooth muscle contractions
- Usual site of fertilization
☆ Uterus
☆ Vagina
Uterus
☆ Usual site of implantation and fetal development
☆Perimetrium (outermost layer, connective tissue) includes peritoneum lining the pelvic cavity
☆ Myometrium is a thick smooth muscle layer
Endometrium includes epithelial layers are sloughed off during menstruation
☆ Narrows to form cervix, which opens vagina
Vagina
☆ Path for sperm to ovum
Uterus, Oviducts, and Ovaries
☆ Monthly, an ovary releases an ovum that moves from the ovaries into the oviduct
- Fertilized eggs are implanted in the uterus, where fetal development occurs
Oogenesis & Follicle Growth
1. Oogonia (2n) are surrounded by granulosa cells, which secretes hormones
- This hollow sphere is called a primordial follicle
2. Most oogonia die and the rest begin the first meiotic division at 7 months gestation, and are called primary oocytes (2n), contained in primary follicles
- 2 million at birth to 400,000 at puberty
- Around 400 are ovulated and the rest die
3. The first meiotic division finishes as the follicle develops, resulting in a secondary oocyte (n), which gets all of the cytoplasm, and a polar body
- This oocyte is in a mature or graafian follicle, which contains a fluid-filled cavity called an antrum
4. The second meiotic division starts and is arrested, to be completed upon fertilization
5. One graafian follicle develops and is ovulated each month
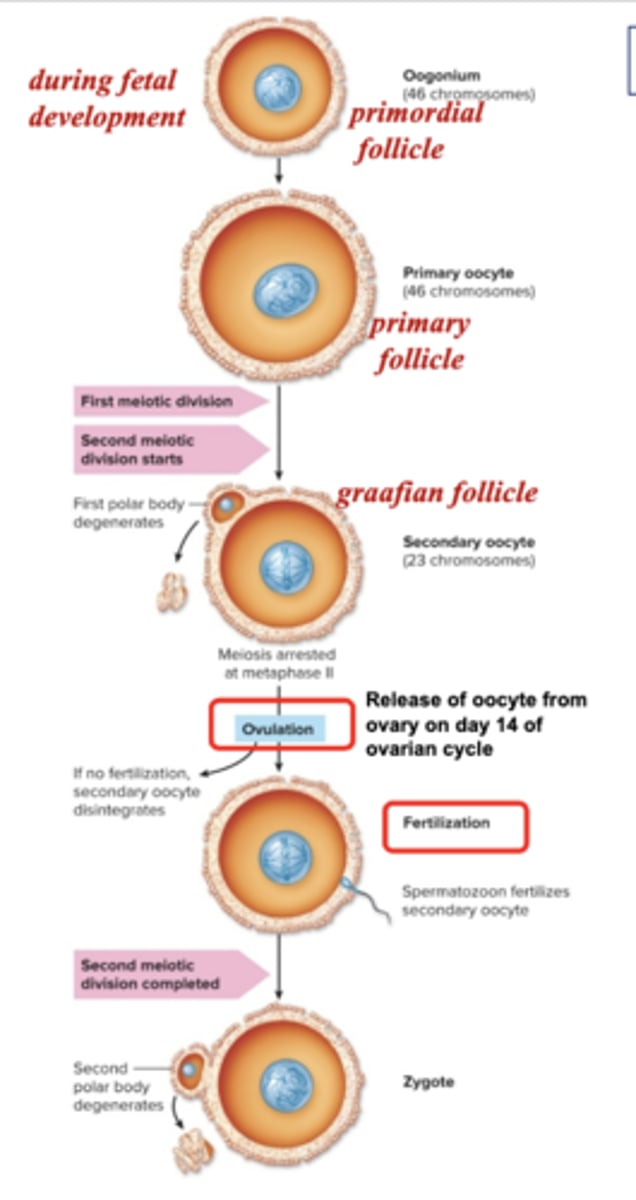
Follicles
☆ The zona pellucida is a thin, gel-like layer around the secondary oocyte
- It represents a barrie to fertilization of an ovulated oocyte by sperm
- The corona radiate is comprised of granulosa cells surrounding the zona pellucida
Menstrual Cycle
☆ 28 day ovarian cycle and endometrial cycle
☆ Cyclical variations in luteinizing hormone (LH), follicle-stimulating hormone (FSH), proesterogene, and estradiol (an estrogen)
☆Ovulation
☆ Menstruation
Ovulation
☆ Occurs at around day 14 of the cycle
Menstruation
☆ Shedding of epithelium of endometrium if ovulated egg is not fertilized; days 1-4 of cycle
Menstrual Cycle: Ovarian Cycle (Next 3)
☆ Follicular Phase
☆ Ovulation
☆ Luteal Phase
Follicular Phase
☆ Days 1-13
☆ Development of follicles under influence of FSH
☆ One follicle matures to Graafian follicle
☆ Increased estradiol secretion from granulosa cells
- Leads to LH surge (from ant. pit.) just prior to ovulation
Ovulation
☆ Day 14
☆ LH surge causes wall of graafian follicle to rupture at around day 14
☆ Secondary oocyte is released from ovary and sw
ept by cilia into oviduct, toward uterus
Luteal Phase
☆ Days 15-28
☆ Transform of follicle into corpus luteum (CL, yellow body) due to LH
- CL secretes estradiol, progesterone (peaks during this phase)
- If no fertilization, estradiol and progesterone decrease and CL turns into corpus albicans, causing menstruation
Hormonal Changes During Menstrual Cycle
☆ Small increases in the secretion of LH & FSH --> follicular maturation in the follicular phase and an increase in the synthesis and secretion of ovarian steroid hormones
☆ LH surge --> ovulation & luteal phase
- High progesterone concentration
Menstrual Cycle: Endometrial Cycle (Next 3)
☆ Menstrual Phase
☆ Proliferative Phase
☆ Secretory Phase
Menstrual Phase
☆ Days 1-14
☆ As ovarian hormones secretion decreases, uterine blood vessels constrict rhythmically, depriving the tissue of blood
☆ Endometrium undergoes necrosis and is sloughed off, resulting in menstrual flow
☆ Myometrium contract as well (causing of cramps)
Proliferative Phase
☆ Days 5-14
☆ Growth and maturation of endometrium under influence of estradiol from the follicle
Secretory Phase
☆ Days 15-28
☆ Increases progesterone and estradiol from CL stimulate endometrial thickening, for implantation
- If no implantation, estrogen and progesterone levels drop and shedding occurs
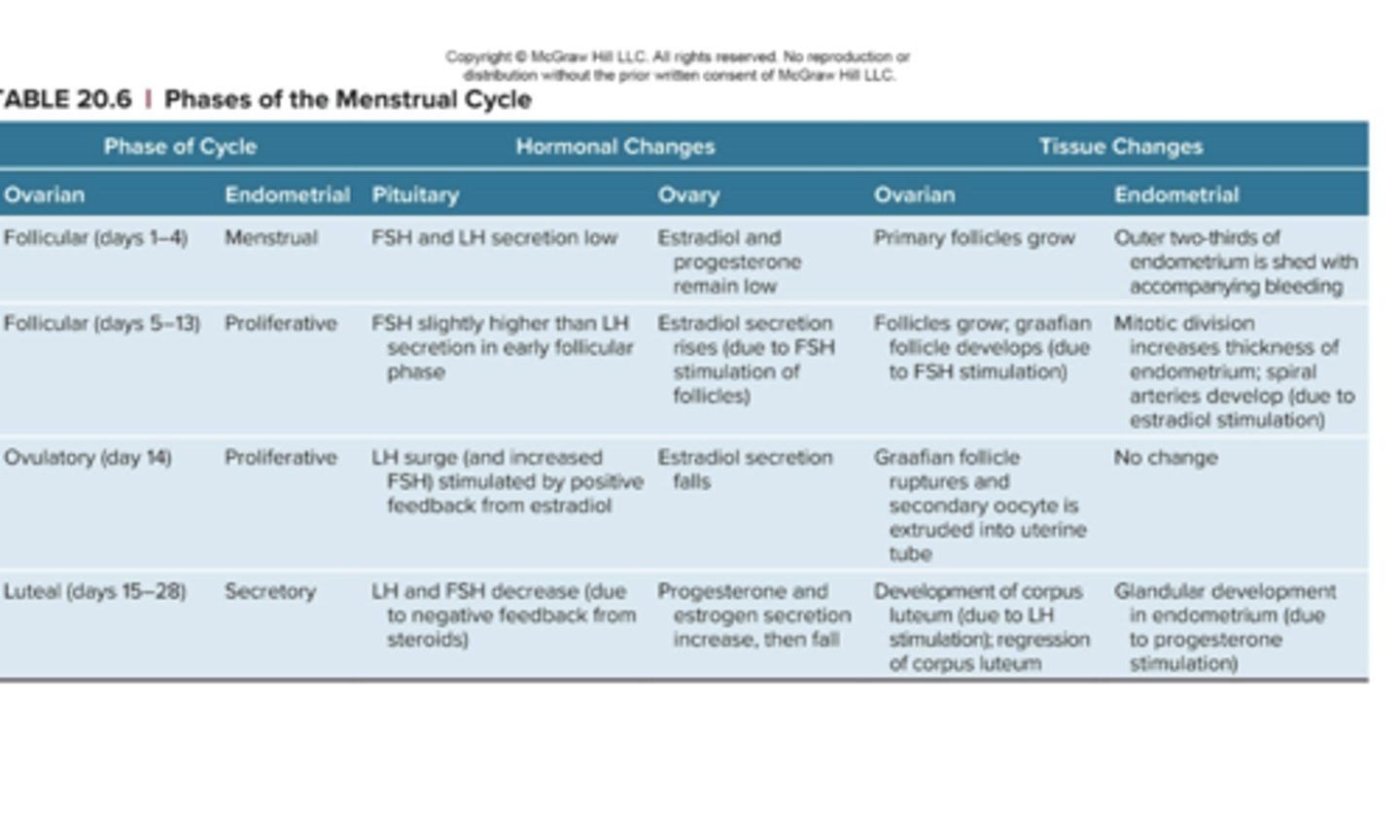
Phases of the Menstrual Cycle Table
Fertilization Pt. 1
- Mature sperm is stored in epididymis
- Appx. 300 million sperm is ejaculated during intercourse
- Fluid pressure of ejaculate propels sperm into uterus
- Only around 100 survive to enter each oviduct (acidic vaginal environment, energy requirements of travel), and about 10% can fertilize an ovum
☆ Capacitation
☆ After its release in the female reproductive tract, a spermatozoan is propelled by the thrashing movements of its flagellum, or tail
Capacitation
☆ Ability to fertilize egg
- Stimulated in whip-like action of tail to propel sperm forward toward Oocyte
Fertilization Pt. 2
☆ Fertilization occurs in oviduct, due to short viability and slow transport of egg
☆ Time window: 5 days before 1 day after ovulation, due to sperm's ability to fertilize for 4-6 days, and egg viability for 24-48 hr
☆ Acrosome in head of sperm binds with zona pellucida of egg, triggering acrosome reaction:
- Alteration of head membrane and release of acrosomal enzymes, to digest a path through the zona pellucida to the oocyte
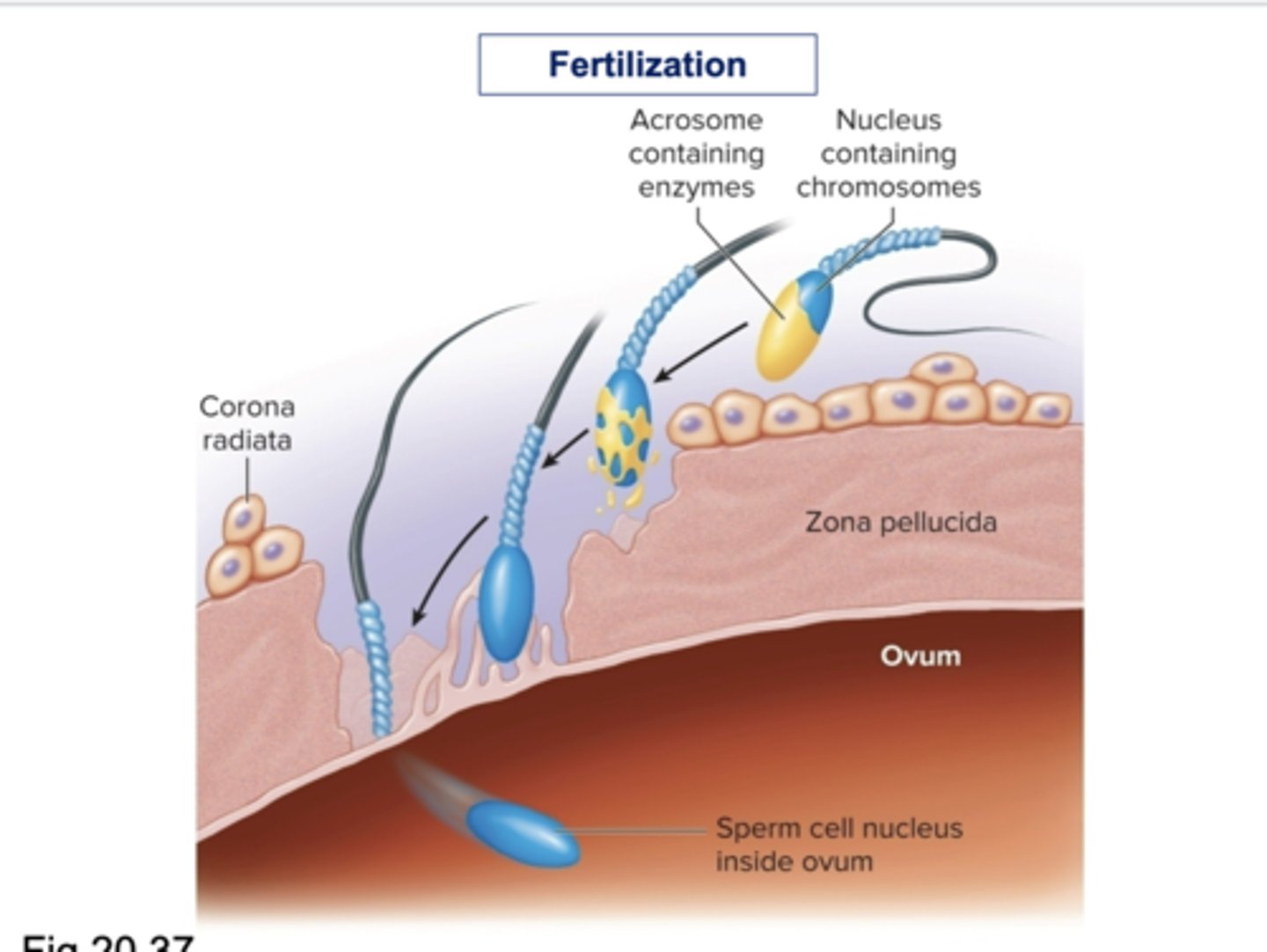
Fertilization Image
Early Development
☆ Zygote (fertilized egg) completes its second meiotic division --> diploid
☆ Undergoes cleavage = mitotic cell division 2 smaller cells
☆ Continued mitosis eventually results in morula (16 cells) at 50-60 hours after fertilization, which enters uterus 3 days after ovulation
☆ By day 4, 32-64 cells, then converted to blastocyst = inner cell mass (to become fetus) + outer chorion (to become placenta)
☆ On day 6, embryo attaches to uterine wall = implantation
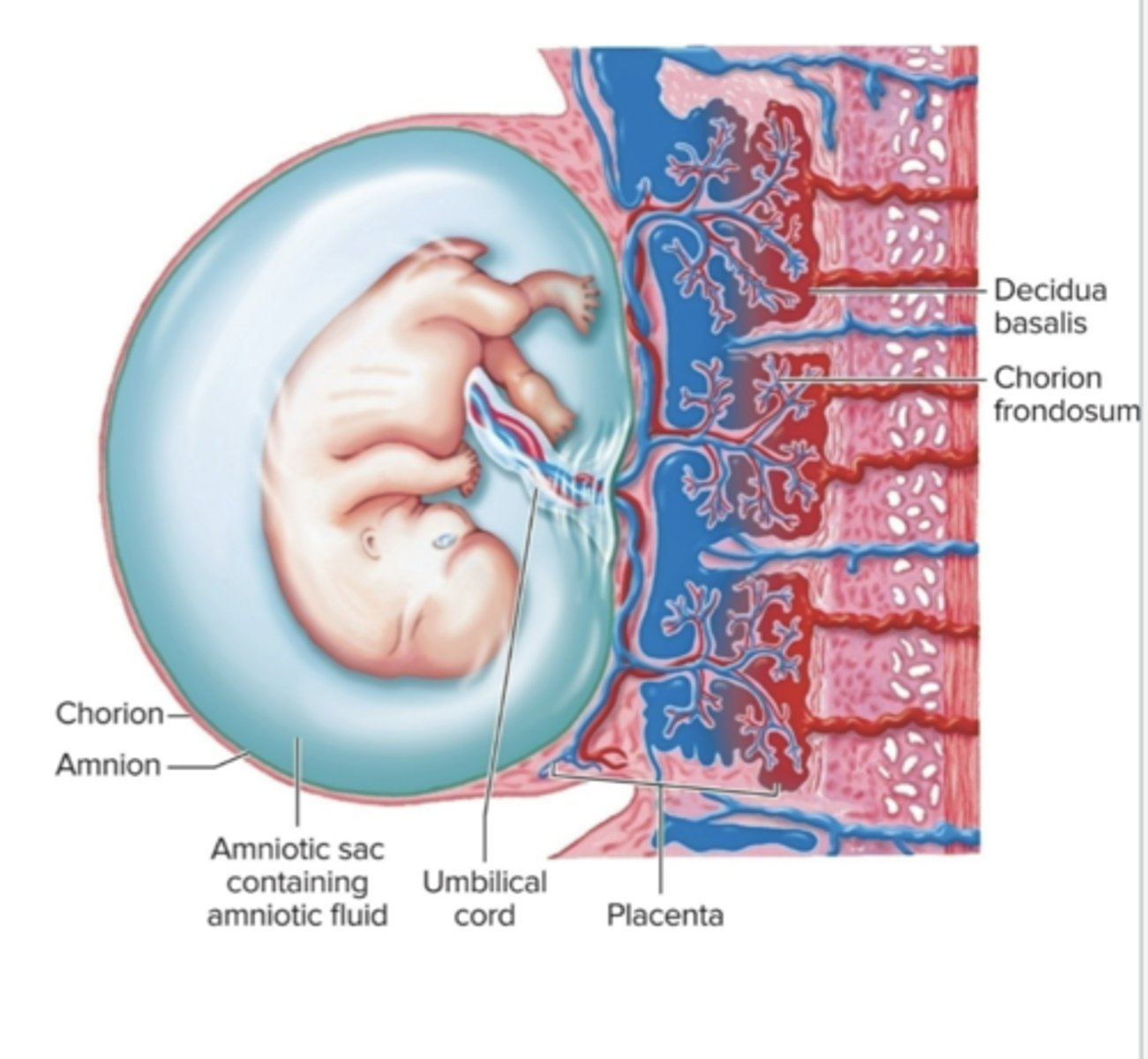
Placenta Pt. 1
Placenta: organ of exchange of gases, nutrients, and waste between mother and fetus; develops in uterus
- Interlocking fetal and maternal tissue with extensive blood supply
- Umbilical arteries (2) and vein (1) are in umbilical cord
☆ The fetus is in the fluid-fulled amniotic sac
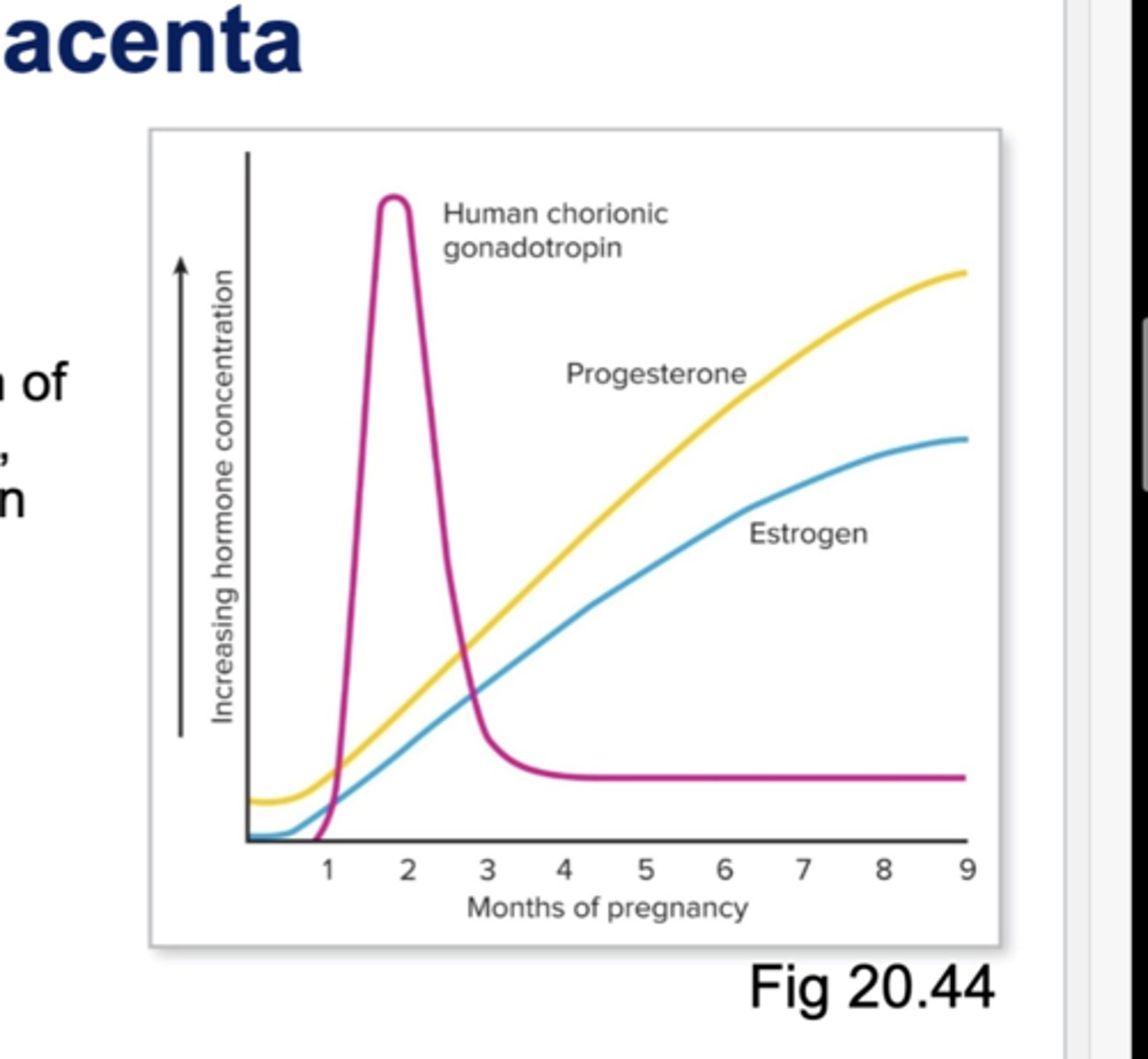
Placenta Pt. 2
☆ In weeks 1-10, blastocyst cells secrete human chorionic gonadotropin (hCH)
- Maintains Cl and secretion of estradiol and progesterone, and to prevent menstruation
☆ CL regresses in week 5-6, and then placenta secretes progesterone and estrogen to maintain pregnancy
Labor & Parturition (Next 6)
☆ Labor
☆ Parturition
☆ Progesterone
☆Estrogen
☆ Cervix
Labor
☆ Powerful uterine contractions to expel fetus
Parturition
☆ Childbirth (delivery)
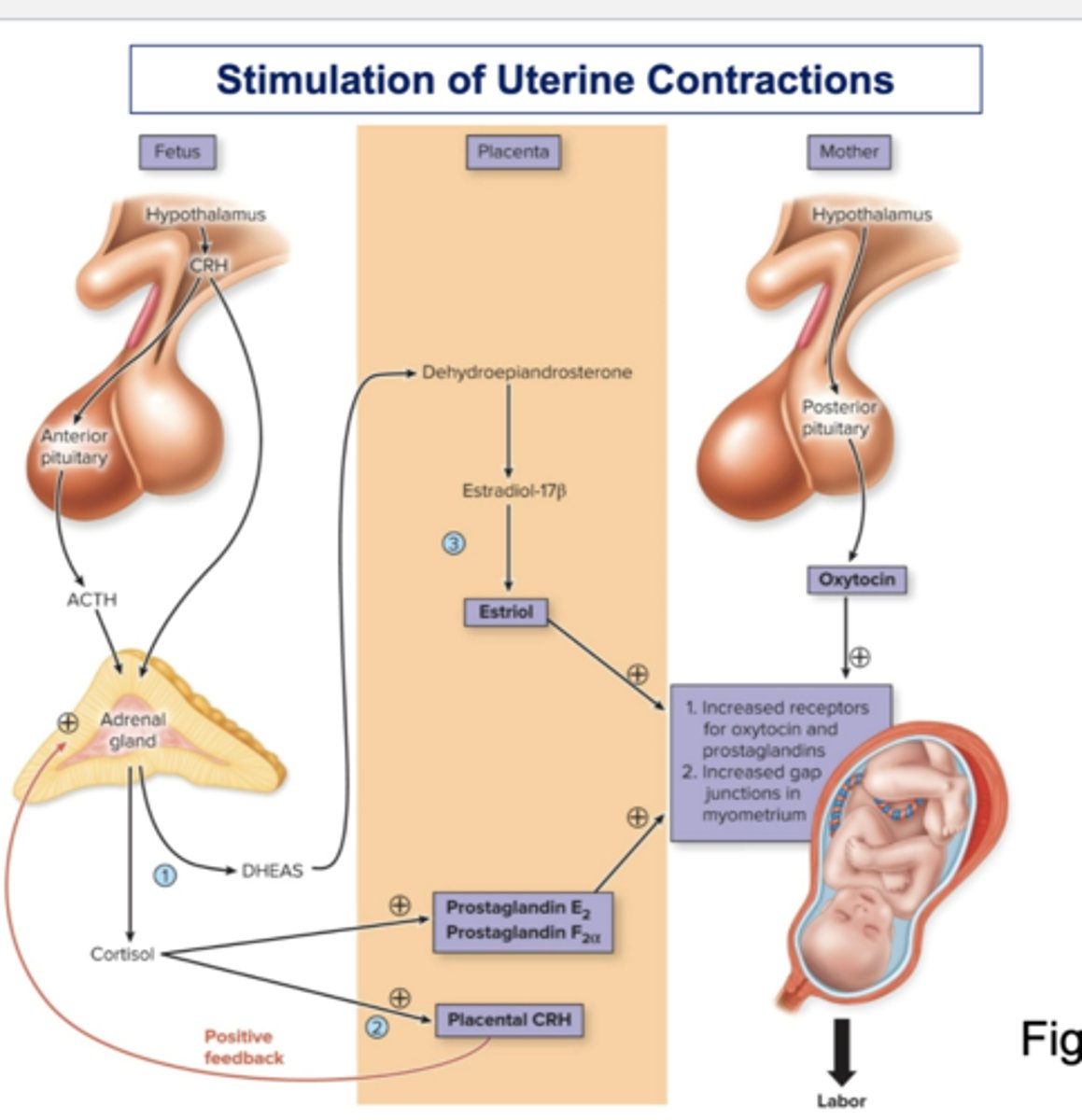
Uterine Contractions
☆ Stimulated by oxytocin (uterus & hypothalamus/posterior pituitary) and prostaglandins (fatty acids, uterus)
Progesterone
☆ Secretion decreases
Estrogen
☆ Causes smooth muscle cells to form gap junctions, so that myometrium contract as single unit
Cervix
☆ Is made of soft and flexible estrogen, prostaglandins, and relaxin (ovary)
Stimulation of Uterine Contractions Image
Lactation Production
☆ Production and secretion of milk after birth
☆ Mammary glands in breasts produce and secrete milk
- Surrounded by myoepithelial cells (contractile cells for milk ejection) and adipose tissue
- They become secretory in early pregnancy due to progesterone, estrogen, and prolactin
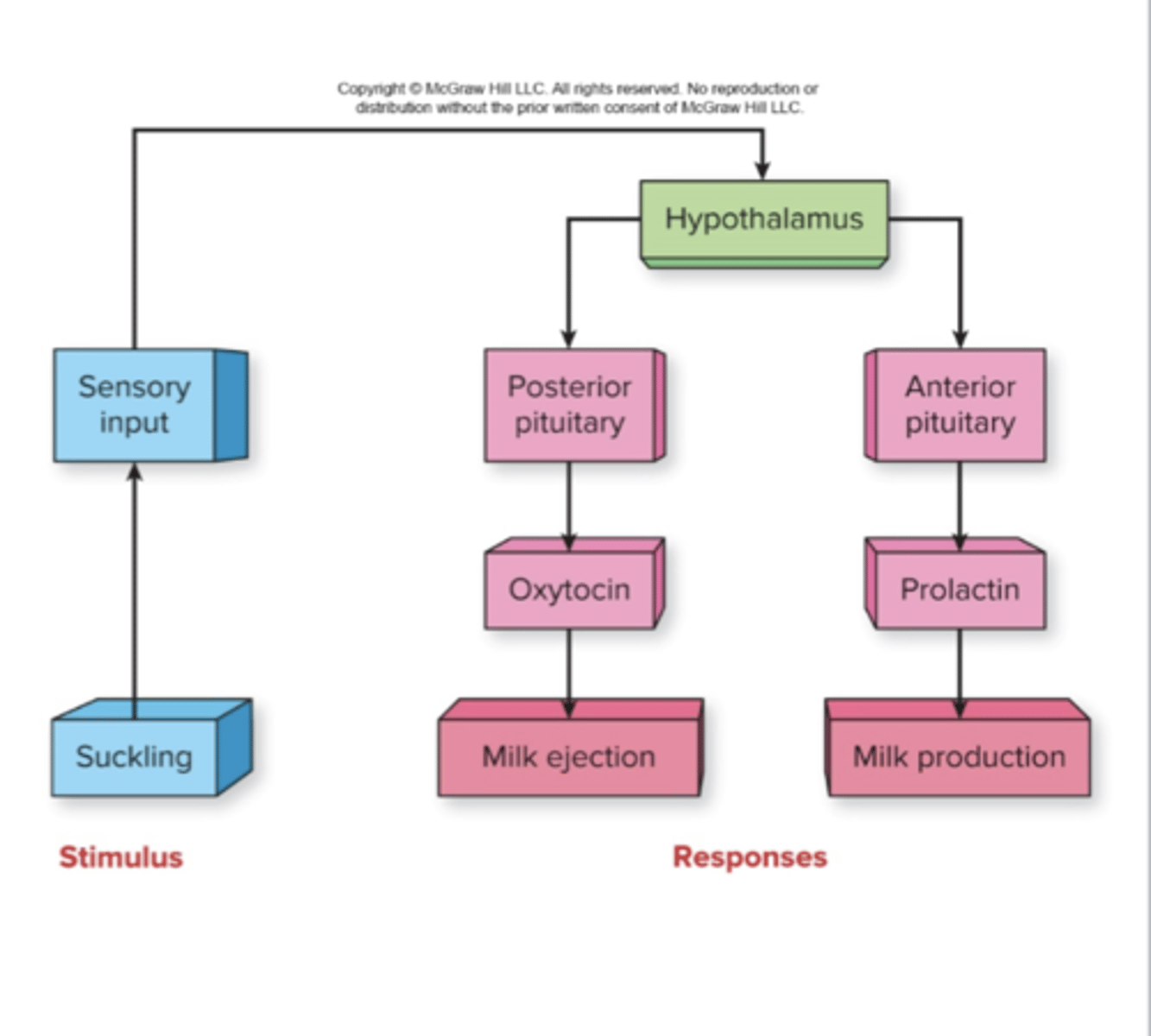
Lactation Hormones
☆ Hormones:
- After parturition, increases prolactin stimulates mammary glands to produce milk
- Sucking also causes secretion of prolactin and oxytocin, which result in secretion of milk into ducts, and ejection of milk, respectively