Anatomy and Physiology - Lecture 5
1/102
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
103 Terms
What does the human skeleton initially consist of?
it initially consists of cartilage, which is later replaced by bone except in areas that require flexibility
What is skeletal cartilage made of?
its made of highly resilient, molded cartilage tissue that consists primarily of water, providing flexibility and cushioning
Does cartilage contain blood vessels or nerves?
no, cartilage contains no blood vessels or nerves
Perichondrium
a layer of dense connective tissue that surrounds cartilage like a girdle
it helps cartilage resist outward expansion and contains blood vessels for nutrient delivery
Chondrocytes
cartilage cells that are encased in small cavities called lacunae within a jelly-like extracellular matrix
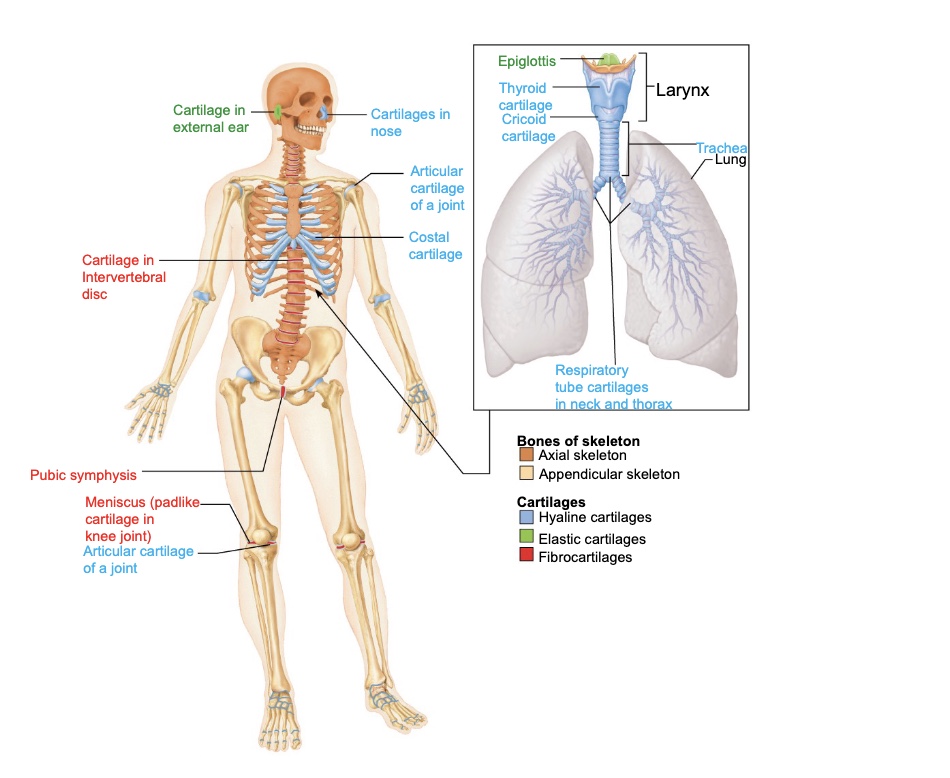
Three main types of cartilage in the body
hyaline cartilage
elastic cartilage
fibrocartilage
Hyaline Cartilage
it provide support, flexibility, and resilience
it is the most abundant cartilage type and its matrix contains only collagen fibers
it is found in articular joints, costal (ribs), respiratory (larynx, trachea), and nasal cartilages (tip of nose)
Elastic Cartilage
contains elastic fibers in addition to collagen, making it more flexible
found in only two places, the external ear and the epiglottis (the flap that covers the larynx when swallowing)
Fibrocartilage
made of thick collagen fibers that give it great tensile strength
found in the knee and the intervertebral discs between the vertebrae
Two ways cartilage grows
appositional growth
interstitial growth
Appositional Growth
cartilage-forming cells in the perichondrium secrete new matrix against the external face of existing cartilage, adding layers to the surface
Interstitial Growth
chondrocytes divide within lacunae and secrete new matrix from inside the cartilage, expanding it from within
What happens to cartilage as a person ages?
cartilage growth slows and often becomes calcified or replaced by bone tissue in adulthood
Why is cartilage important for skeletal development?
it serves as the template for bone formation and provides flexibility and cushioning in areas like joints and the rib cage
7 major functions of bones
support → form the framework that supports the body and cradles soft organs like muscles and tissues
protection → they enclose and safeguard vital organs such as the brain (skull), spinal cord (vertebrae) and heart and lungs (rib cage)
movement/anchorage → bones act as levers that muscles attach to; when muscles contract, bones move, enabling locomotion and manipulation of the environment
mineral and growth-factor storage →they serve as reservoirs for minerals, especially calcium and phosphorus, that can be released into the bloodstream to maintain mineral balance
blood-cell formation → In red bone marrow cavities of certain bones through a process called hematopoiesis.
triglyceride (fat) storage → Fat is stored in yellow bone marrow as an energy reserve for the body.
hormone production → osteocalcin is the hormone produced and it regulates insulin secretion, glucose levels, and overall metabolism; it also influences fat storage and energy use
How many names bones are in the human skeleton?
206
How is the skeleton divided based on location?
divided into two groups:
the axial skeleton
the appendicular skeleton
Axial Skeleton
the long axis of the body
includes the skill, vertebral column, and rib cage
it supports, protects, and carries other body parts such as the head, neck, and trunk
Appendicular Skeleton
the bones if the upper and lower limbs, plus the girdles (shoulder and hip) that attach them to the axial skeleton
it allows movement and manipulation of the enviroment
How are bones classified by shape?
Into four types:
long bones
short bones
flat bones
irregular bones
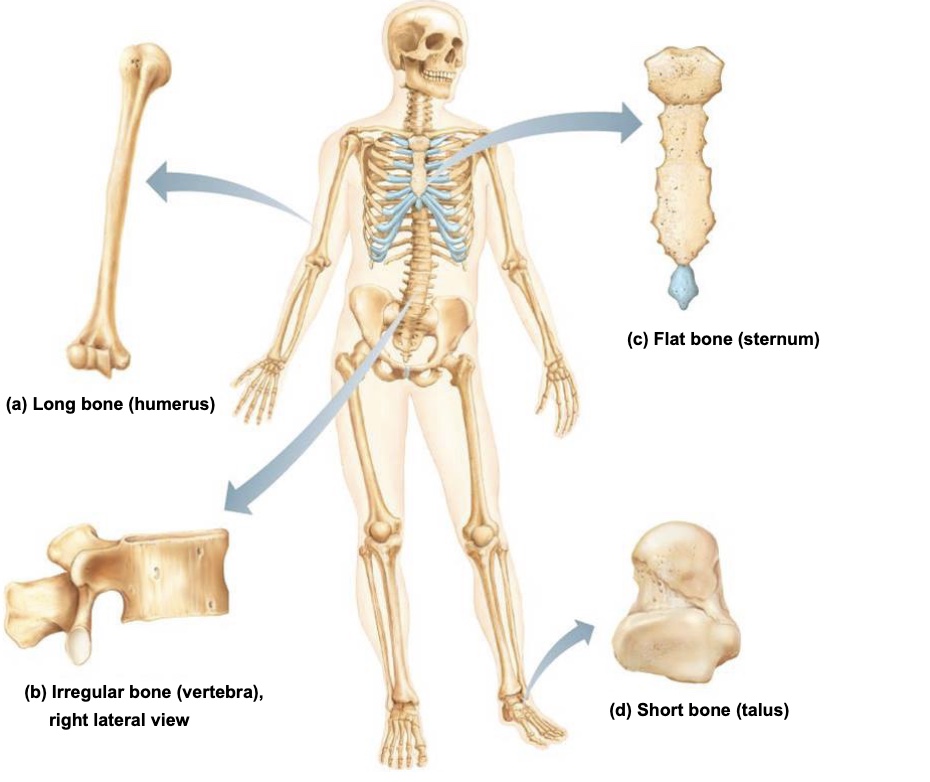
Long Bones
bones that are longer than they are wide
with a shaft and two ends
they are mostly limb bones (femur, humerus)
they act as levers for movement and support the weight of the bodt
Short Bones
cube-shaped bones found in the wrist (carpals) and ankle (tarsals); they provide stability and some movement
Sesamoid bones
special short bones that form within tendons to reduce friction and modify pressure (e.g the patella)
their number and size can vary among different peopl
Flat Bones
thin, flat, and slightly curved bones that protect internal organs and provide large surfaces for muscle attachment (e.g., sternum, ribs, scapulae, skull bone)
they protect internal organs and provide surfaces for muscle attachment
Bones that are part of both the axial and appendicular skeletons
the clavicle (appendicular) connects to the sternum (axial) linking the two skeleton regions
Three levels of bone structure
gross anatomy (visible structure)
microscopic anatomy (cellular level)
chemical composition (molecular level)
Two types of bone structure
compact bone
spongy bone
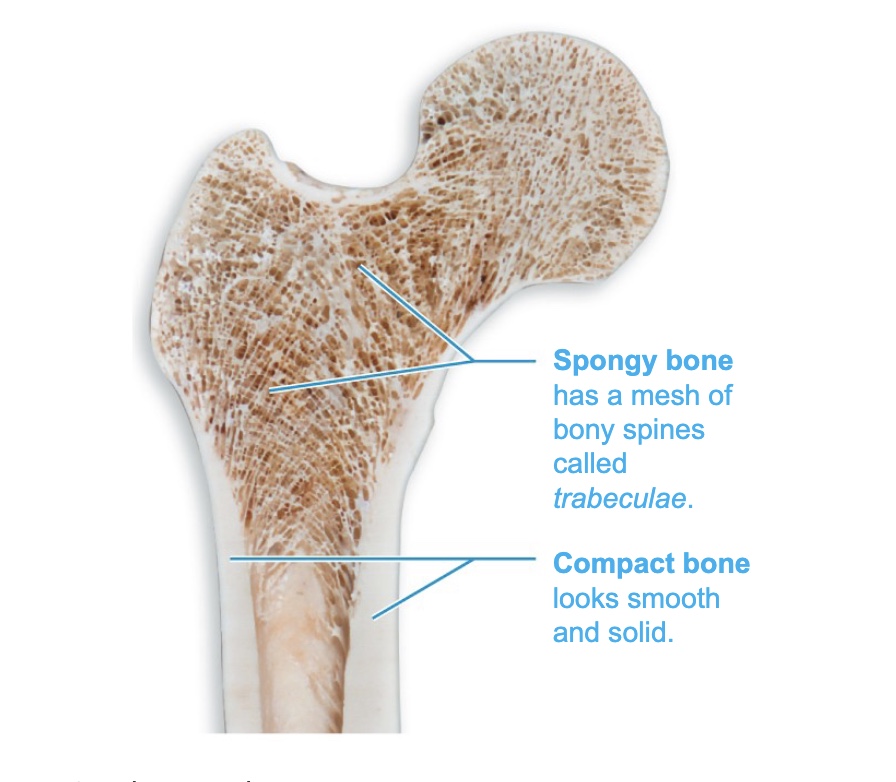
Compact Bone
the dense, outer layer of bone that looks smooth and solid
it provides strength and protection
Spongy Bone (cancellous bone)
a honeycomb-like network of small, needle-shaped or flat pieces called trabeculae, with open space filled with red or yellow bone marrow
Structure of short, irregular, and flat bones
they consist of thin plates of spongy bones covered by compact bone
periosteum on the outside and endosteum on the inside
bone marrow is scattered throughout the spongy bone rather than confined to a cavity
What covers the area of bone that forms a movable joint?
hyaline cartilage, which reduces friction and absorbs shock
Diaphysis of a Long Bone
the shaft or long axis of the bones
its made of bone surrounding a medullary (marrow) cavity
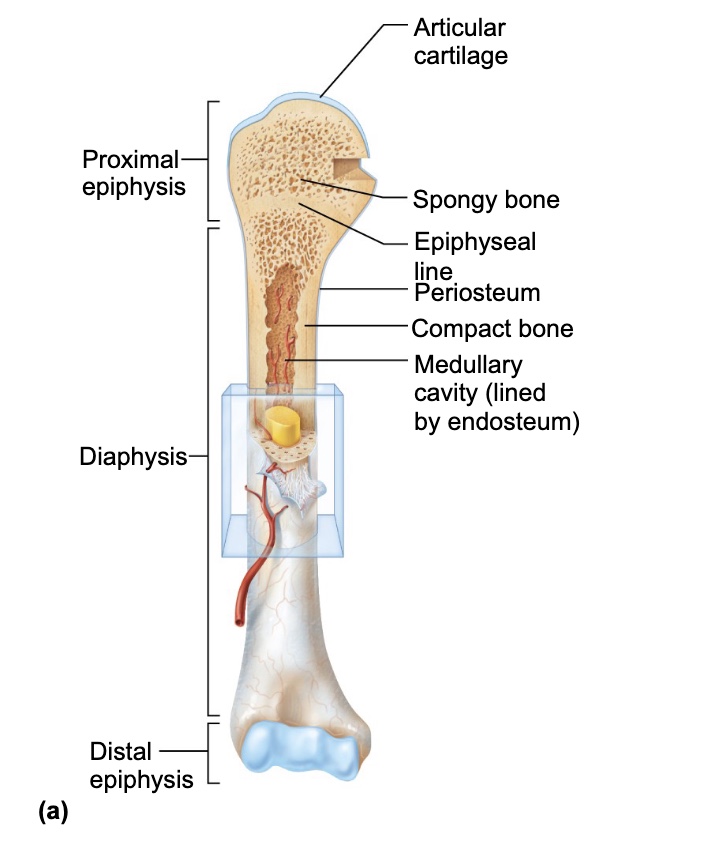
What does the medullary cavity contain?
in adults, it contains yellow bone marrow (fat)
Epiphyses
the ends of long bones, made of compact bone externally and spongy bone internally
Epiphyseal Line
a remnant of the epiphyseal plate (growth plate) in adults where bone growth occurred during childhood
Periosteum
its a white, double-layered membrane covering the external surface of bones (except at joints)
it protects the bone, nourishes it, and serves as an attachment site for tendons and ligaments
two layers:
an outer fibrous layer of dense irregular connective tissue
an inner osteogenic layer containing stem cells
Sharpey’s Fibers (perforating fibers)
collagen fibers that secure the periosteum to the underlying bone matrix
Endosteum
a delicate connective tissue membrane lining the internal bone surfaces, including trabeculae and canals in compact bones
osteogenic cells that can differentiate into other bone cells, such as osteoblasts and osteoclasts are found here
Bone Markings
features on bone surfaces that serve as attachment sites for muscles, tendons, and ligaments
3 categories
projections (outward bulges)
depressions (grooves or indentation)
openings (holes or canals)
Hematopoietic tissue in bones
red bone marrow is found within trabecular cavities of spongy bone and diploe of flat bones, such as sternum
in newborns, medullary cavities and all spongy bone contain red bone marrow
in adults, red bone marrow is located in head of femur and humerus, but most active areas of hematopoiesis are flat bone diploe and some irregular bones (such as the hip bone)
yellow bone marrow can convert to red, if person becomes anemic
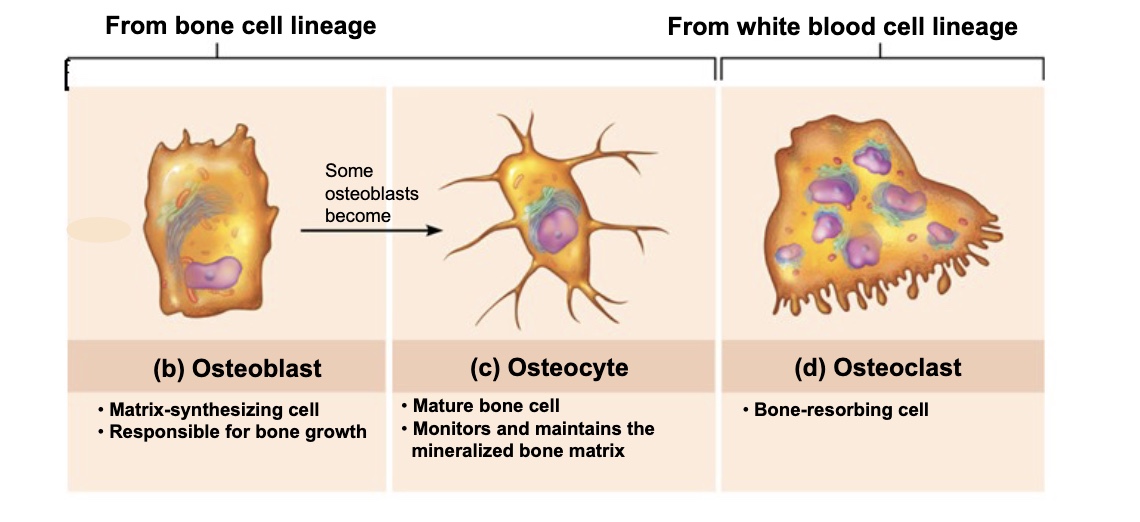
Osteogenic Cells
stem cells in the periosteum and endosteum that divide and differentiate into osteoblasts or bone-lining cells
Osteoblasts
bone-forming cells that secrete unmineralized bone matrix called osteoid, composed of collagen and calcium-binding proteins
they are important because they build new bone tissue and are actively mitotic, playing a key role in bone growth and remodelling
Osteocytes
mature bone cells found in lacunae that maintain the bone matrix and act as stress sensors
they detect mechanical stress or strain and signal osteoblasts and osteoclasts to remodel bone accordingly
Bone-lining Cells
flat bone cells on bone surfaces that help maintain the bone matrix; on the external surface they’re called periosteal cells, and on the internal surface, endosteal cells
Osteoclasts
large, multinucleate cells that break down bone tissue (bone absorption) and are derived from the same stem cells as macrophages
they are active in depressions called resorption bays; they gave ruffled borders that increase surface area for dissolving bone
Compact Bone
also called lamellar bone
consists of:
→ osteon (Haversian system)
→ canals anf canaliculi
→ interstitial and circumferential lamellae
Osteon (Haversian system)
the structural unit of compact bone
it’s an elongated cylinder that runs parallel to the long axis of the bone, acting as a weight-bearing pillar
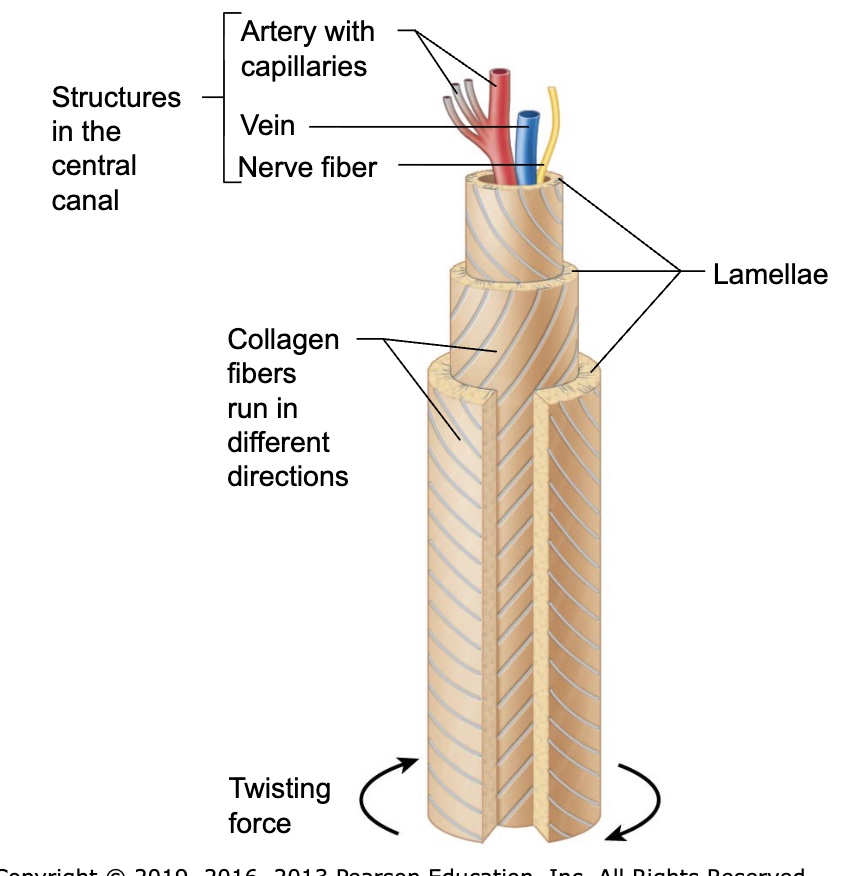
Lamellae
rings of bone matrix within an osteon that contain collagen fibers running in alternating directions to resists twisting forces
Central (Haversian) canal
the canal running through the core of an osteon, containing blood vessels and nerve fibers
Perforating (Volkmann’s) canals
canals that run perpendicular to the central canal, connecting blood vessels and nerves between periosteum, medullary cavity, and central canal
Lacunae
small cavities within bone that house osteocytes
Canaliculi
tiny channels that connect lacunae to each other and to the central canal, allowing nutrient and waste exchange between osteocytes
Interstitial Lamellae
remnants of old osteons that fill spaces between newer osteons
Circumferential Lamellae
layers of bone matrix that extend around the entire surface of the diaphysis, just deep to the periosteum, helping the bone resist twistin
Spongy Bone - Anatomy
appears poorly organized but is actually organized along lines of stress to help bone resist any stress
trabeculae, like cables on a suspension bridge, confer strength to bone
no osteons are present, but trabeculae do contain irregularly arranged lamellae and osteocytes interconnected by canaliculi
capillaries in endosteum supply nutrients
What two component make up bone?
organic and inorganic components
Organic components of bone
cells (osteogenic, osteoblasts, osteocytes, bone-lining cells, osteoclasts)
osteoid (the unmineralized organic matrix)
What is osteoid made of?
ground substance and collagen fibers, which provide flexibility and tensile strength
Why is collagen important in bone?
it resists stretching and provides flexibility, preventing bones from breaking under stress
What are sacrificial bonds in collagen?
small connections between collagen molecules that break under stress to absorbs energy and prevent fractures, then reform when the stress is removed
Inorganic components of bone
hydrocyapatite’s (mineral salts), mainly tiny crystals of calcium phosphate embedded in the collagen matrix
about 65% of bone madd is inorganic
What gives bone its hardness and strength?
the inorganic mineral salts, primarily calcium phosphate, provide hardness and resistance to compression
Ossification (osteogenesis)
the process of bone tissue formation that begins in the embryo and continues throughout life as bone grows, remodel, and repair
What are the three stages of bone development across life?
formation of the bony skeleton in embryos
posnatal bone growth until earl adulthood
bone remodelling and repair throughout life
Two main type of ossification?
endochondral ossification
intramembranous ossification
Endochondral ossification
the process by which bone forms by replacing hyaline cartilage models
nearly all bones bones below the skull except the clavicles are formed by thus
it begins in the late second month of fetal development
What must occur before ossification can begin in cartilage?
the hyaline cartilage must be broken down to make way for bone formation
What is the primary ossification center?
the region in the center of the diaphysis where bone formation first begins
What triggers the transformation of perochondrium into periosteium?
blood vessels infiltrate the perchondrium, supplying nutrients and converting it into periosteum
What do mesenchymal cells in the periosteum differentiate into?
osteoblasts, which begin forming bone
Five main steps of endochondral ossification
bone collar forms around the diaphysis of the cartilage model
central cartilage in diaphysis calcifies and forms cavities
periosteal bud invades cavities, forming spongy bone
diaphysis elongates, and a medullary cavity forms
epiphyses ossify, leaving only articular cartilage and apuphyseal plates
What does periosteal bud consist of?
blood vessels, nerves, red marrow, osteogenic cells, and osteoclasts that invade the cartilage model
Intramembranous ossification
bone development from a fibrous connective tissue membrane, rather than from cartilage
Which bones form by intramembranous ossification
flat bones of the skull (frontal, parietal, occipital, temporal) and the clavicles
What type of cells form the fibrous membrane?
mesenchymal cells
What are the four major steps in intramembranous ossification
ossification center form as mesenchymal cells cluster and become osteoblasts
osteoid is secreted by osteoblasts then calcified
woven (immature) bone and periosteum form
woven bone is remodelled into lamellar bone, and red marrow appears
What is woven bone?
the initial, unorganized bone formed during ossification
it is later remodelled into mature lamellar bone
Postnatal Bone Growth
Long bones grow lengthwise by interstitial (longitudinal) growth of epiphyseal plate
Bones increase thickness through appositional growth
Bones stop growing during adolescence
some facial bones continue to grow slowly through life
Growth in Length of Long Bones
Interstitial growth requires presence of epiphyseal cartilage in the epiphyseal plate
Epiphyseal plate maintains constant thickness
– Rate of cartilage growth on one side balanced by bone replacement on other
• Epiphyseal plate consists of five zones:
1. Resting (quiescent) zone
2. Proliferation (growth) zone
3. Hypertrophic zone
4. Calcification zone
5. Ossification (osteogenic) zon
• Near end of adolescence, chondroblasts divide less often
• Epiphyseal plate thins, then is replaced by bone
• Epiphyseal plate closure occurs when epiphysis and diaphysis fuse
• Bone lengthening ceases
– Females: occurs around 18 years of age
– Males: occurs around 21 years of age
Resting (quiescent) zone
area of cartilage on epiphyseal side of epiphyseal plate that is relatively inactive
Proliferation (growth) zone
area of cartilage on diaphysis side of epiphyseal plate that is rapidly dividing
new cells formed move upward, pushing epiphysis away from diaphysis, causing lengthening
Hypertrophic Zone
area with older chondrocytes closer to diaphysis
cartilage lacunae enlarge and erode, forming interconnecting spaces
Calcification Zone
surrounding cartilage matrix calcifies; chondrocytes die and deteriorate
Copyright
Ossification Zine
Chondrocyte deterioration leaves long spicules of calcified cartilage at epiphysis-diaphysis junction
Spicules are then eroded by osteoclasts and are covered with new bone by osteoblasts
Ultimately replaced with spongy bone
Medullary cavity enlarges as spicules are eroded
Growth in Width (Thickness)
• Growing bones widen as they lengthen through appositional growth
– Can occur throughout life
• Bones thicken in response to increased stress from muscle activity or added weight
• Osteoblasts beneath periosteum secrete bone matrix on external bone
• Osteoclasts remove bone on endosteal surface
• Usually more building up than breaking down which leads to thicker, stronger bone
that is not too heavy
Hormonal Regulation of Bone Growth
• Growth hormone: most important hormone inb stimulating epiphyseal plate activity in infancy and childhood
• Thyroid hormone: modulates activity of growth hormone, ensuring proper proportions
• Testosterone (males) and estrogens (females) at puberty: promote adolescent growth spurts
– End growth by inducing epiphyseal plate closure
• Excesses or deficits of any hormones cause abnormal skeletal growth
Bone Remodeling
• About 5–10% of our skeleton is replaced every year
– Spongy bone entirely replaced ~ every 3-4 years
– Compact bone entirely replaced ~ every 10 years
• Bone remodeling consists of both bone deposit and bone resorption
– Occurs at surfaces of both periosteum and endosteum
– Remodeling units: packets of adjacent osteoblasts and osteoclasts coordinate
emodeling process
Bone Resorption
• Resorption is function of osteoclasts
– Dig depressions or grooves as they break down matrix
– Secrete lysosomal enzymes and protons (H+) that digest matrix
– Acidity converts calcium salts to soluble forms
• Osteoclasts also phagocytize demineralized matrix and dead osteocytes
– Digested products are transcytosed across cell and released into interstitial fluid
and then into blood
– Once resorption is complete, osteoclasts undergo apoptosis
• Osteoclast activation involves PTH (parathyroid hormone) and immune T cell proteins
Copyright
Bone Deposit
• New bone matrix is deposited by osteoblasts
• Osteoid seam: band of unmineralized bone matrix that marks area of new matrix
• Calcification front: abrupt transition zone between osteoid seam and older
mineralized bone
Control of Remodeling
Hormonal controls
– Parathyroid hormone (PTH): produced by parathyroid glands in response to low
blood calcium levels
Stimulates osteoclasts to resorb bone
Calcium is released into blood, raising levels
PTH secretion stops when homeostatic calcium levels are reached
– Calcitonin: produced by parafollicular cells of thyroid gland in response to high
levels of blood calcium levels
Effects are negligible, but at high pharmacological doses it can lower blood
calcium levels temporarily
Response to mechanical stress
– Bones reflect stresses they encounter
Bones are stressed when weight bears on them or muscles pull on them
– Wolf’s law states that bones grow or remodel in response to demands placed
on them
Stress is usually off center, so bones tend to bend
Bending compresses one side, stretches other side
– Diaphysis is thickest where bending stresses are greatest
– Bone can be hollow because compression and tension cancel each other out in center of bone
Bone Repair
Fractures are breaks
– During youth, most fractures result from trauma
– In old age, most result from weakness of bone due to bone thinning
Fracture Classification
Three “either/or” fracture classifications
– Position of bone ends after fracture
Nondisplaced: ends retain normal position
Displaced: ends are out of normal alignment
– Completeness of break
Complete: broken all the way through
Incomplete: not broken all the way through
– Whether skin is penetrated
Open (compound): skin is penetrated
Closed (simple): skin is not penetrated
• Can also be described by location of fracture, external appearance, and nature of break
Fracture Treatment and Repair
• Treatment involves reduction, the realignment of broken bone ends
– Closed reduction: physician manipulates to correct position
– Open reduction: surgical pins or wires secure ends
– Immobilization of bone by cast or traction is needed for healing
Time needed for repair depends on break severity, bone broken, and age
of patient
Repair involves four major stages:
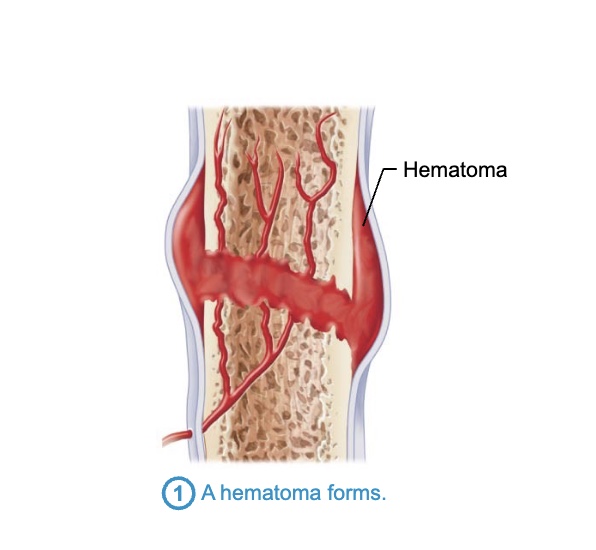
1. Hematoma formation
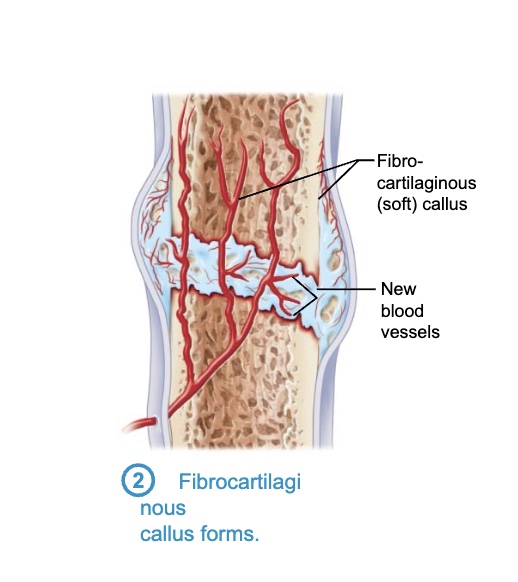
2. Fibrocartilaginous callus formation
3. Bony callus formation
4. Bone remodeling
Copyright
Hematoma formation
– Torn blood vessels hemorrhage, forming mass of clotted blood called a
hematoma
– Site is swollen, painful, and inflamed
Fibrocartilaginous callus formation
– Capillaries grow into hematoma
– Phagocytic cells clear debris
– Fibroblasts secrete collagen fibers to span break and connect broken ends
– Fibroblasts, cartilage, and osteogenic cells begin reconstruction of bone
Create cartilage matrix of repair tissue
Osteoblasts form spongy bone within matrix
– This mass of repair tissue is called fibrocartilaginous callus
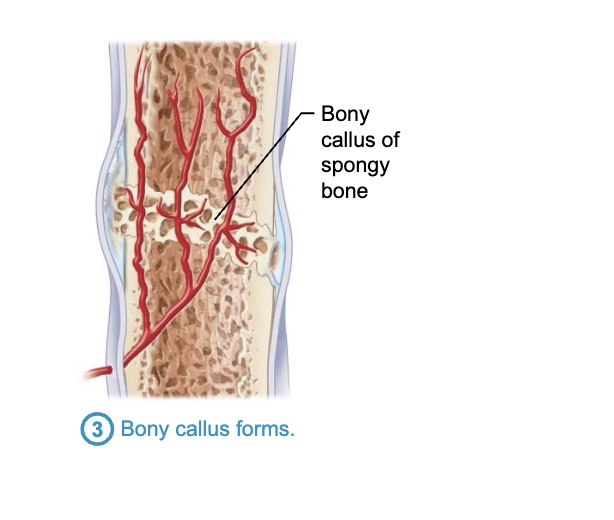
Bony callus formation
– Within one week, new trabeculae appear in fibrocartilaginous callus
– Callus is converted to bony (hard) callus of spongy bone
– Bony callus formation continues for about 2 months until firm union forms
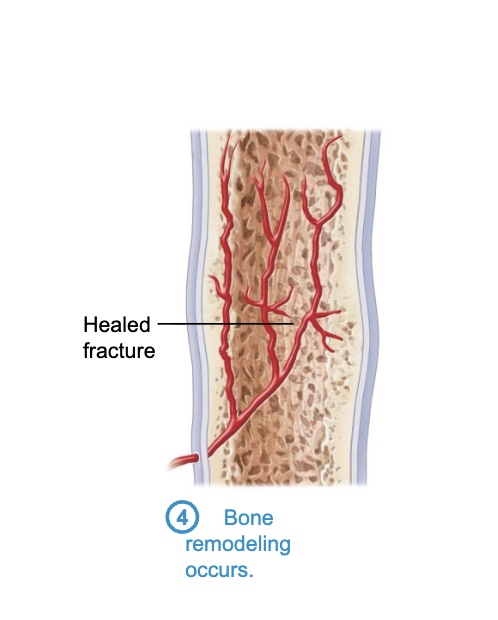
Bone remodeling
– Begins during bony callus formation and continues for several months
– Excess material on diaphysis exterior and within medullary cavity is removed
– Compact bone is laid down to reconstruct shaft walls
– Final structure resembles original structure
Responds to same mechanical stressors
Bone Disorders
• Imbalances between bone deposit and bone resorption underlie nearly every disease
that affects the human skeleton.
• Three major bone diseases:
– Osteomalacia and rickets
– Osteoporosis
Osteomalacia and Rickets
• Osteomalacia
– Bones are poorly mineralized
– Osteoid is produced, but calcium salts not adequately deposited
– Results in soft, weak bones
– Pain upon bearing weight
• Rickets (osteomalacia of children)
– Results in bowed legs and other bone deformities because bones ends
are enlarged and abnormally long
– Cause: vitamin D deficiency or insufficient dietary calcium
Osteoporosis
• is a group of diseases in which bone resorption exceeds deposit
• Matrix remains normal, but bone mass declines
– Spongy bone of spine and neck of femur most susceptible
Vertebral and hip fractures common
Risk factors f
– Most often aged, postmenopausal women
Affects 30% of women aged 60–70 years and 70% by age 80
Estrogen plays a role in bone density, so when levels drop at menopause,
women run higher risk
– Men are less prone due to protection by the effects of testosterone
– Insufficient exercise to stress bones
– Diet poor in calcium and protein
– Smoking
– Genetics
– Hormone-related conditions
Hyperthyroidism
Diabetes mellitus
– Consumption of alcohol or certain medications