patho accessory organs
1/97
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
98 Terms
normal functions of liver (summary)
1. synthesis: glucose, bile, plasma proteins, blood clotting factors
2. metabolism: steroids, drugs, carbs, fat, protein
3. storage: minerals,vitamins
4. filter blood, remove bacteria
what does the liver synthesize
glucose, bile, plasma proteins, blood clotting factors
describe the liver's role in estrogen/hormone metabolism
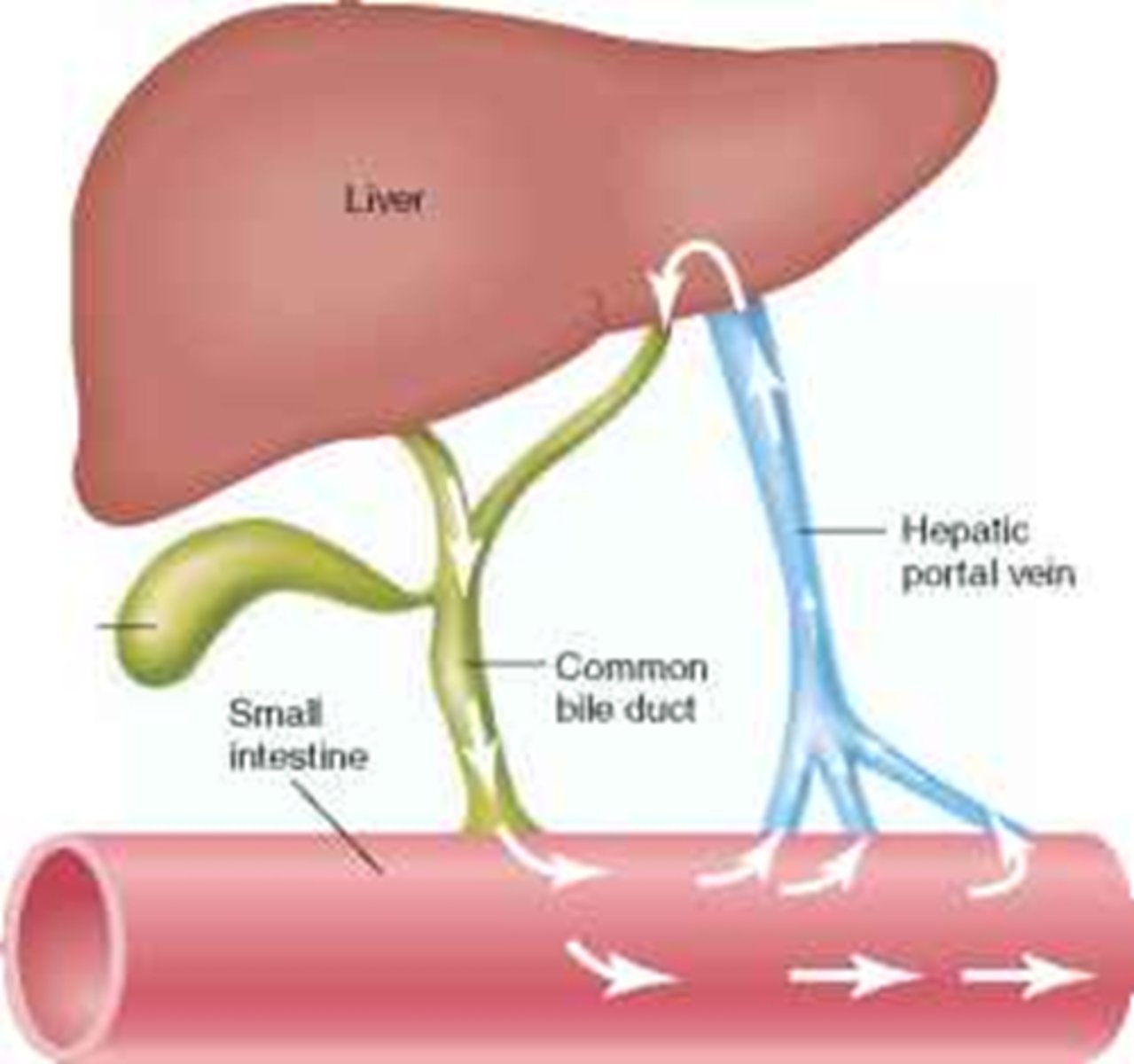
enterohepatic recycling: hormones (estrogen) are conjugated in the liver, secreted into bile->SI-> and reabsorbed
(increases half life)
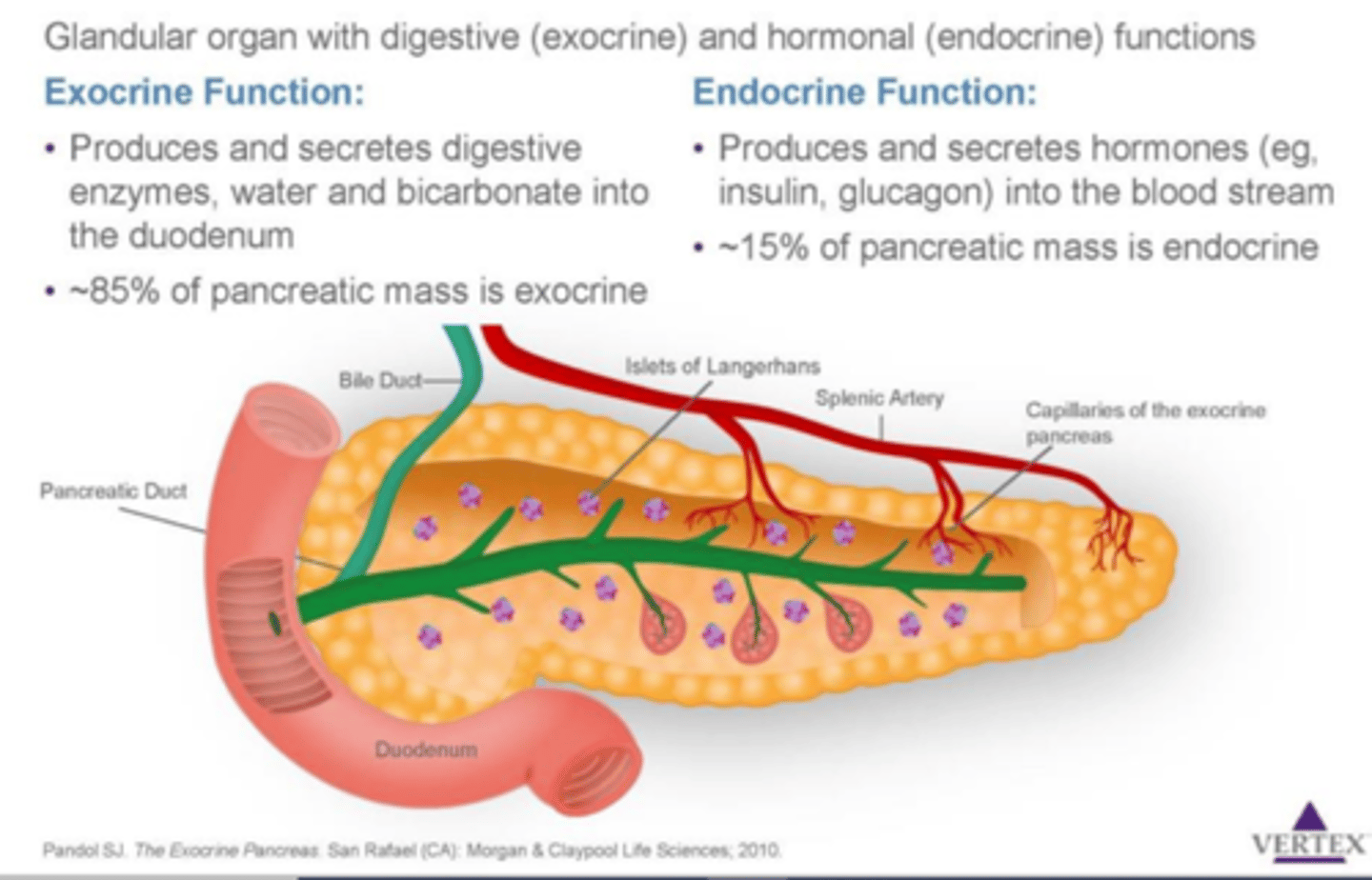
normal function of endocrine and exocrine pancreas
endocrine: supply insulin and glucagon
exocrine: digestive enzymes
t/f: the liver's primary role in metabolism is to make substances more polar for excretion
true
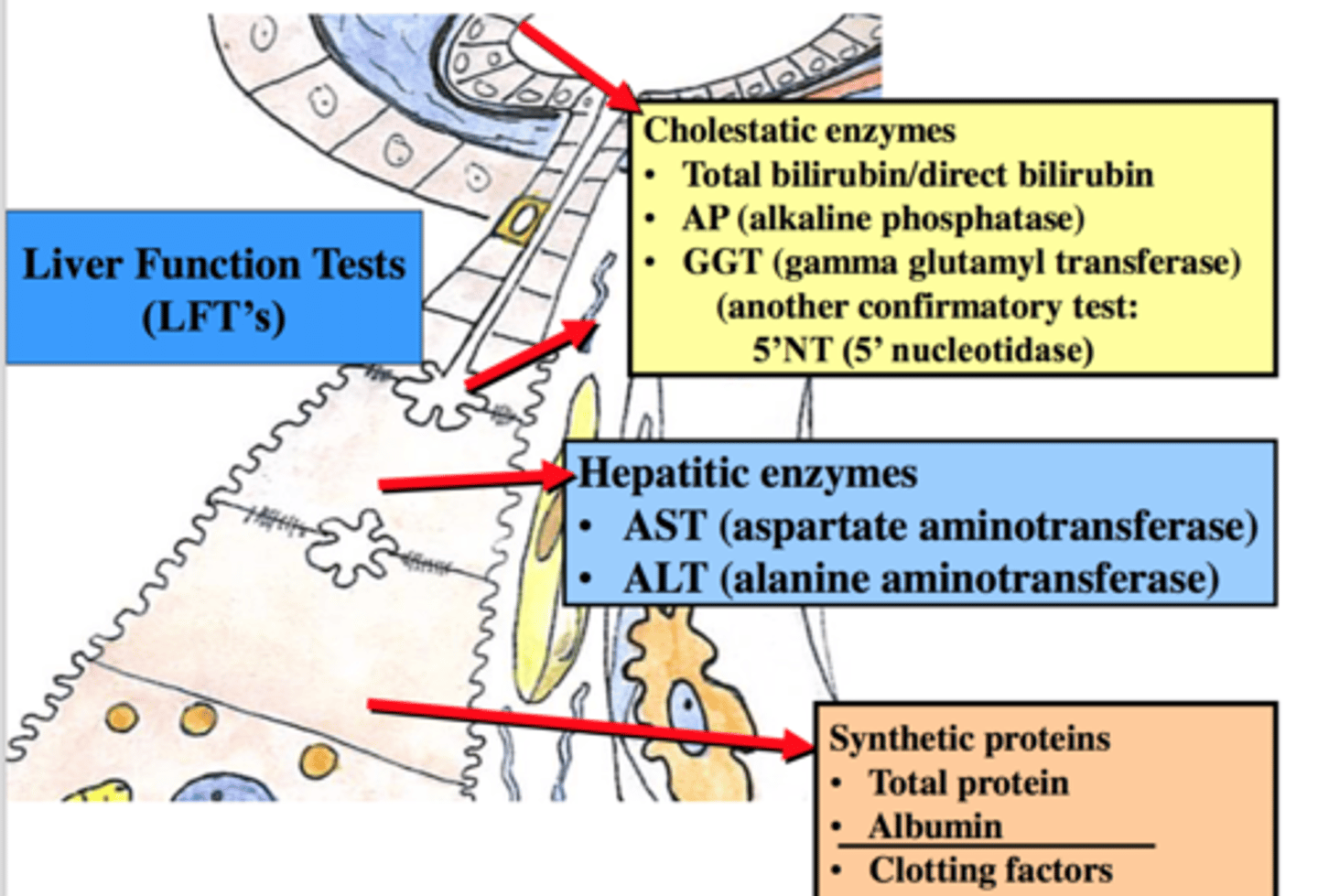
what is evaluated in lab to establish proper liver function
1. enzymes: damaged proteins will be in lymph/blood (ASL,AST)
2. bilirubin (should be low in blood)
3. proteins (iron, transferrin, coags)
4. coagulation tests (liver secretes coag factors)
5. hepatitis virus markers
6. autoimmune antibodies (type 2)
why do we need to check liver enzymes during drug dosing
anything we take orally will come in contact with the liver. if a drug dose is too high, it will damage liver during metabolism
liver injuries usually result in which responses
1. inflammation (hepatitis)
2. degeneration (hydropic or lipid)
3. necrosis (cell death)
4. fibrosis (scarring/cirrhosis)
t/f: the liver is only capable of necrosis
false. hepatocytes are regenerable and can divide (apoptosis)
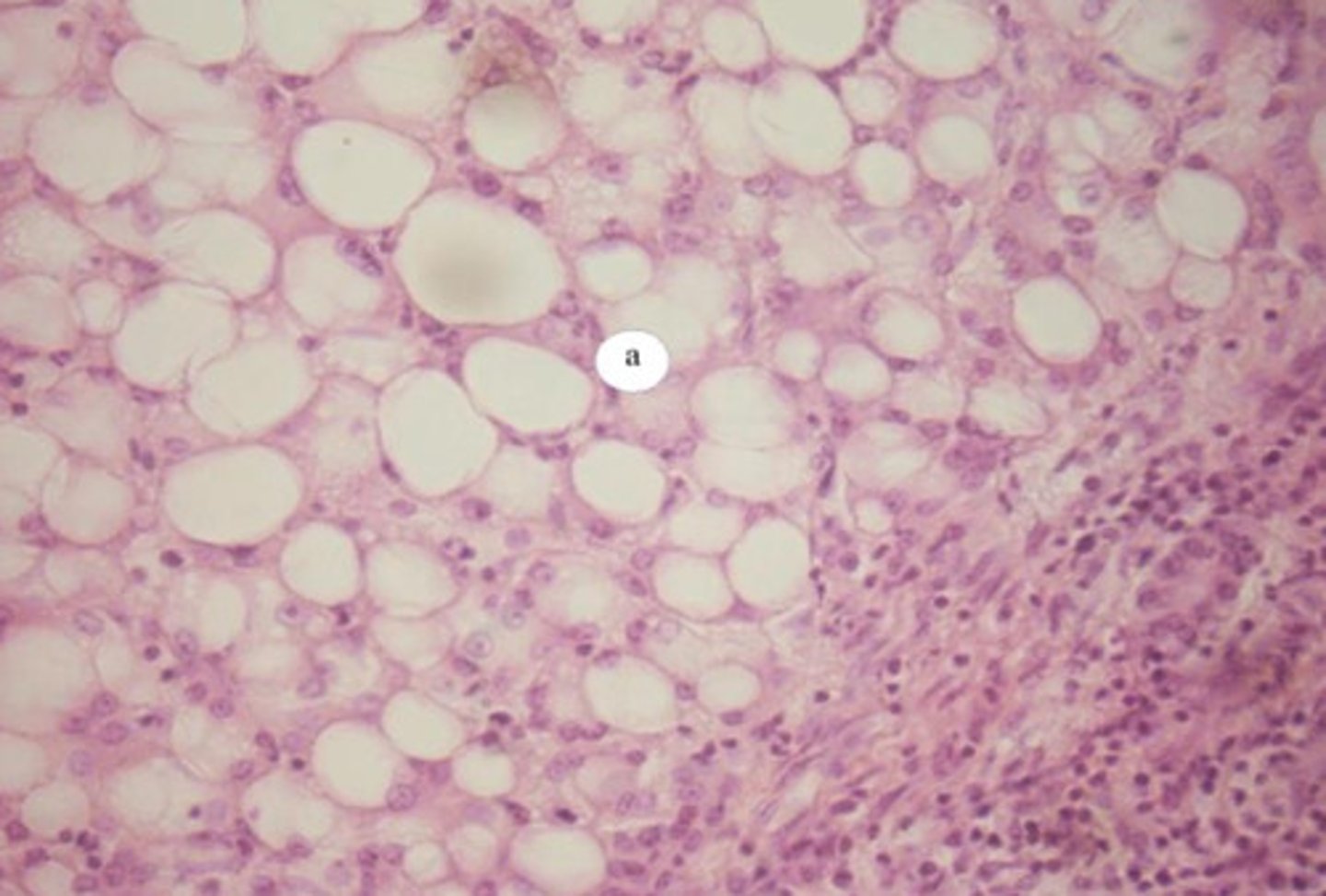
lipid degeneration of liver
lipids accumulate in liver (ex: during acute ethanol digestion)
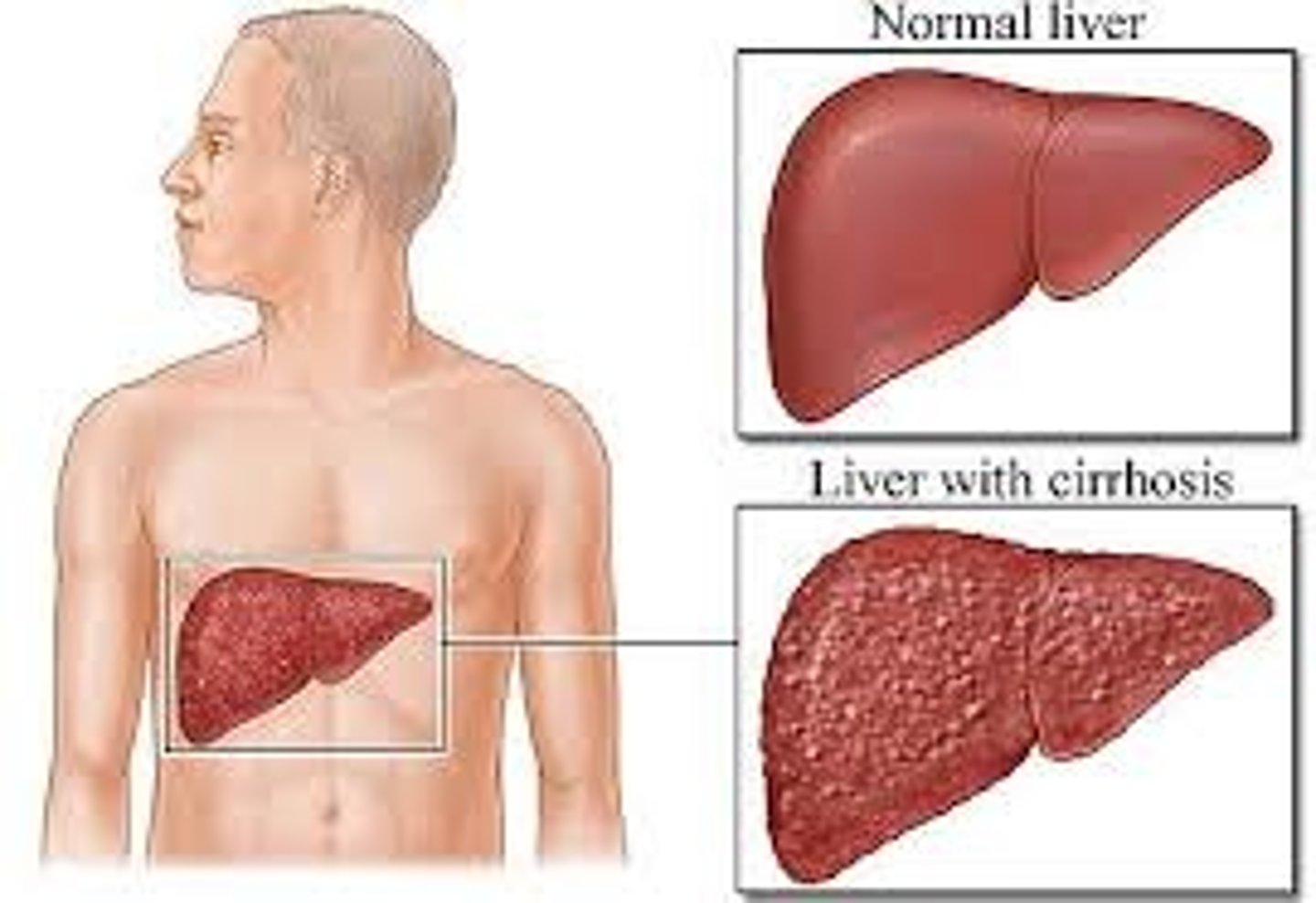
cirrhosis
general term for fibrotic scarring of the liver
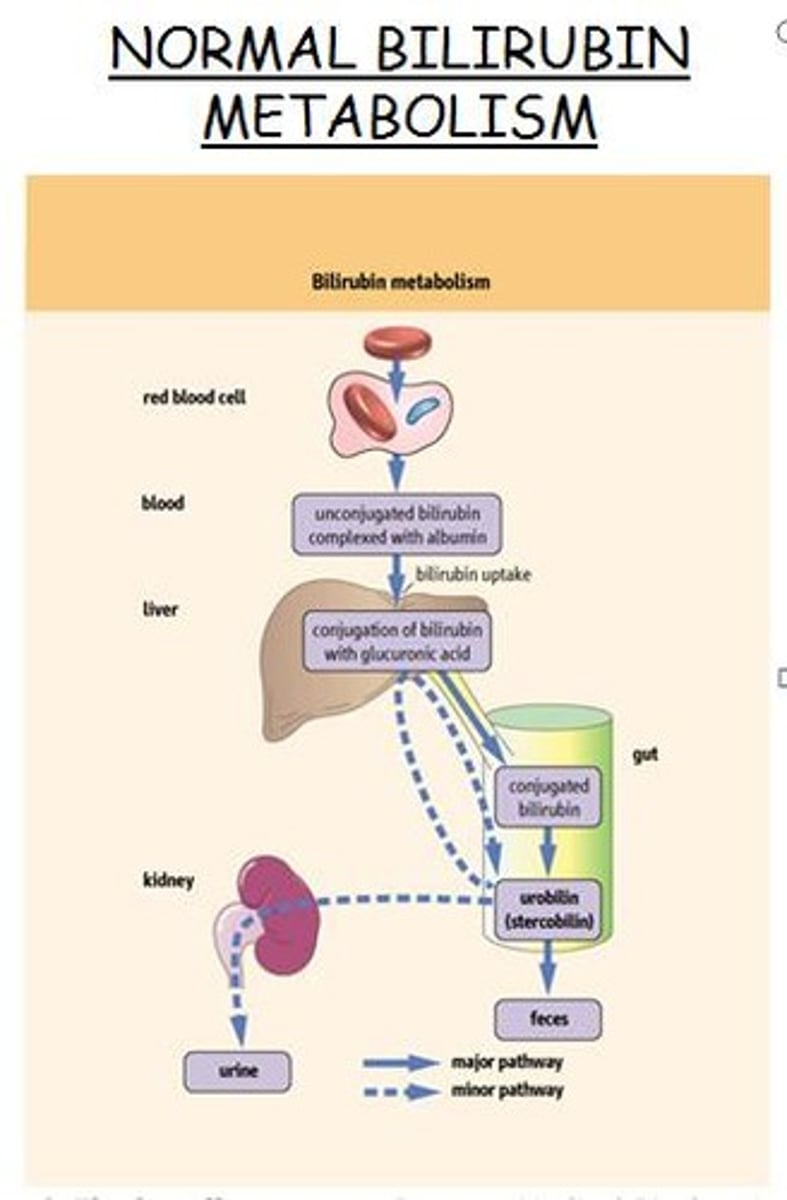
jaundice pathophys
yellow discoloration of skin and sclerae due to excess of blood bilirubin (iron protein breaks down and gives yellow color)

how does the liver normally function to prevent jaundice
uptakes and conjugates bilirubin compounds and places into bile for elimination
4 possible causes of jaundice
prehepatic:
1. excessive destruction of RBCs
intrahepatic:
2. impaired uptake of bilirubin by liver cells
3. decreased conjugation of bilirubin
intra/post:
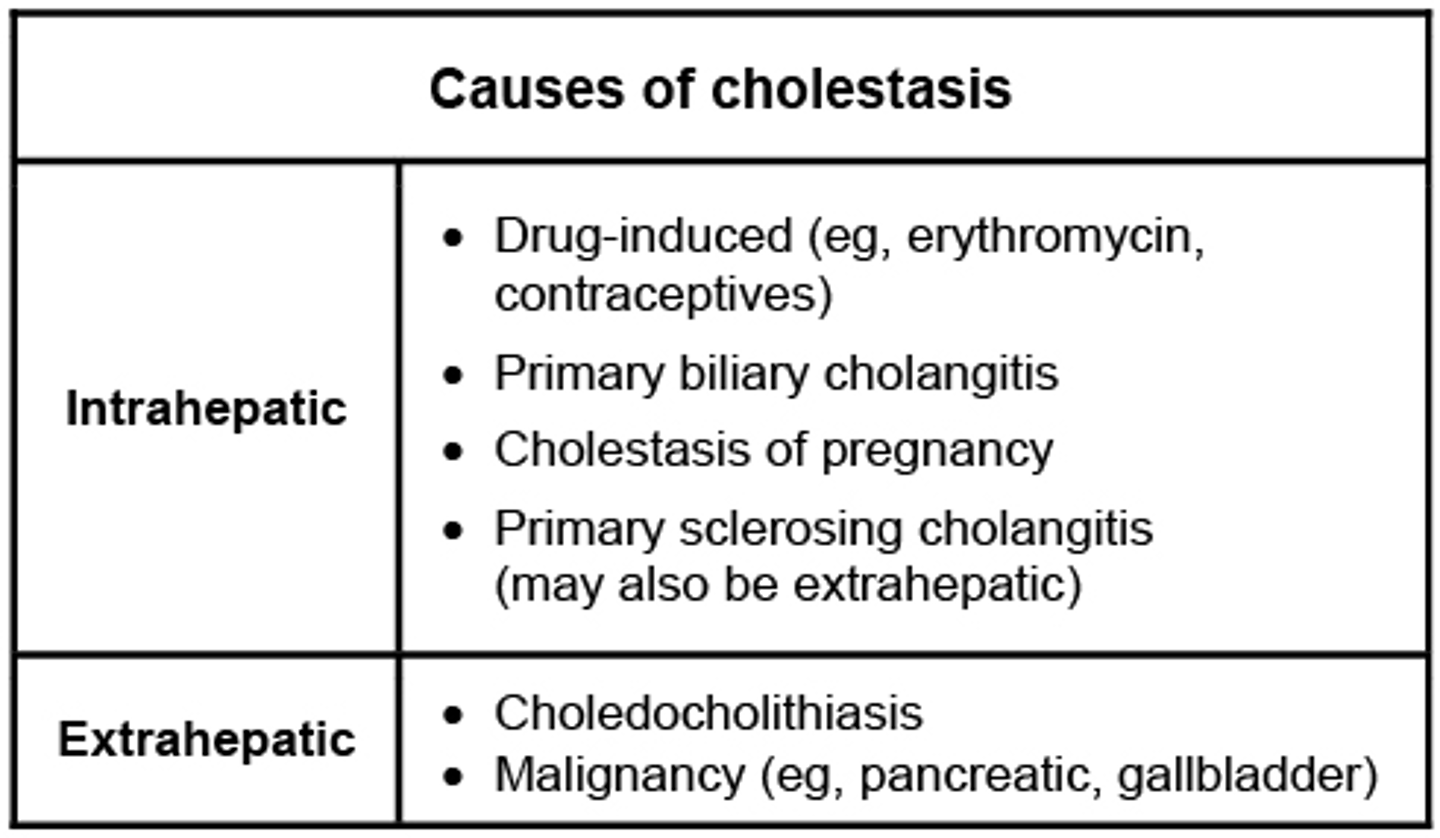
4. cholestasis (obstruction of bile flow)
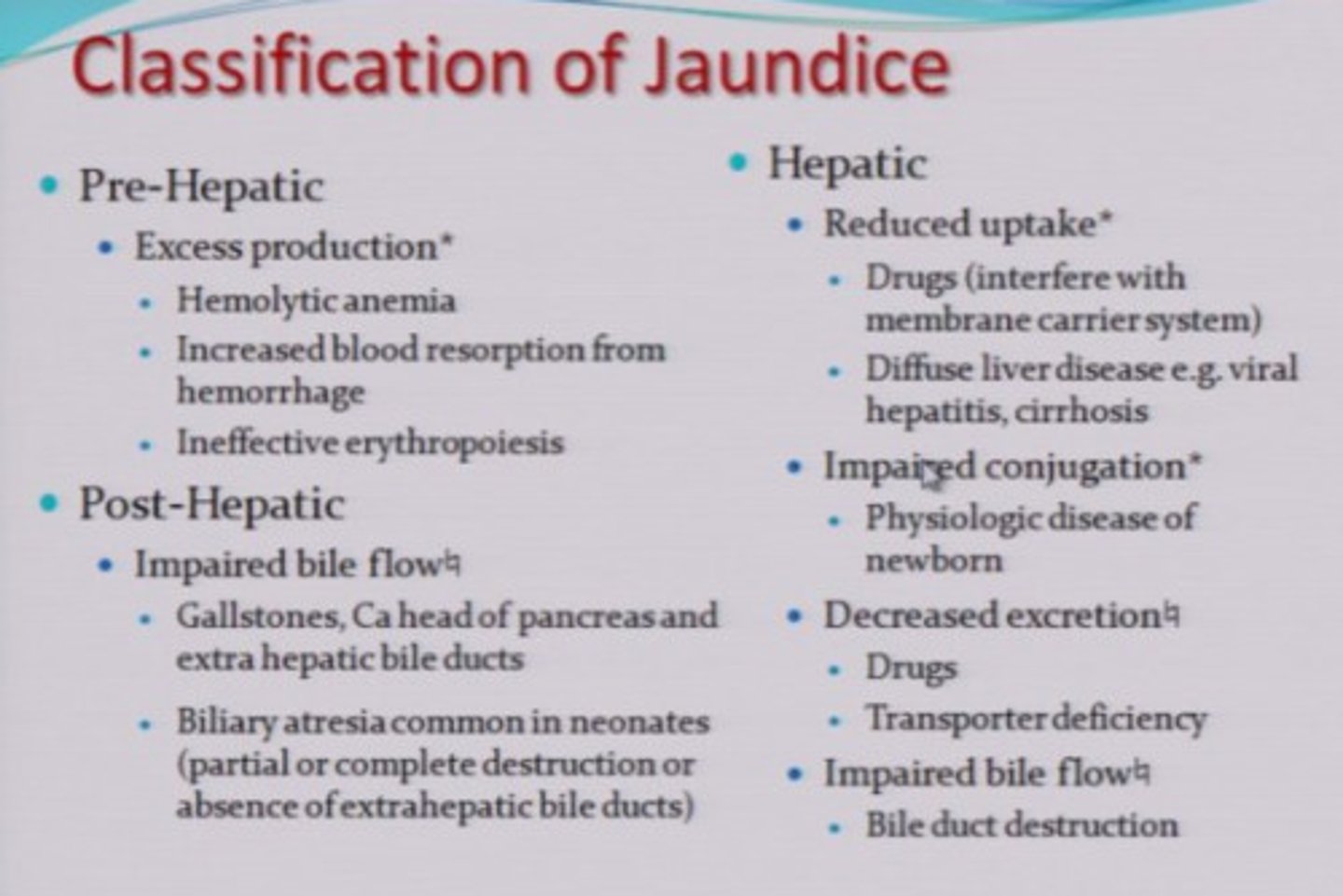
cholestasis
obstruction of bile flow in hepatic lobules or bile ducts
hematologic mechanism of jaundice (hemolytic jaundice)
excessive lysis of RBCs (ex: autoimmune) -> hepatocytes cannot conjugate bilirubin fast enough, it enters blood-> unconjugated hyperbilirubinemia= deposits in tissues= jaundice
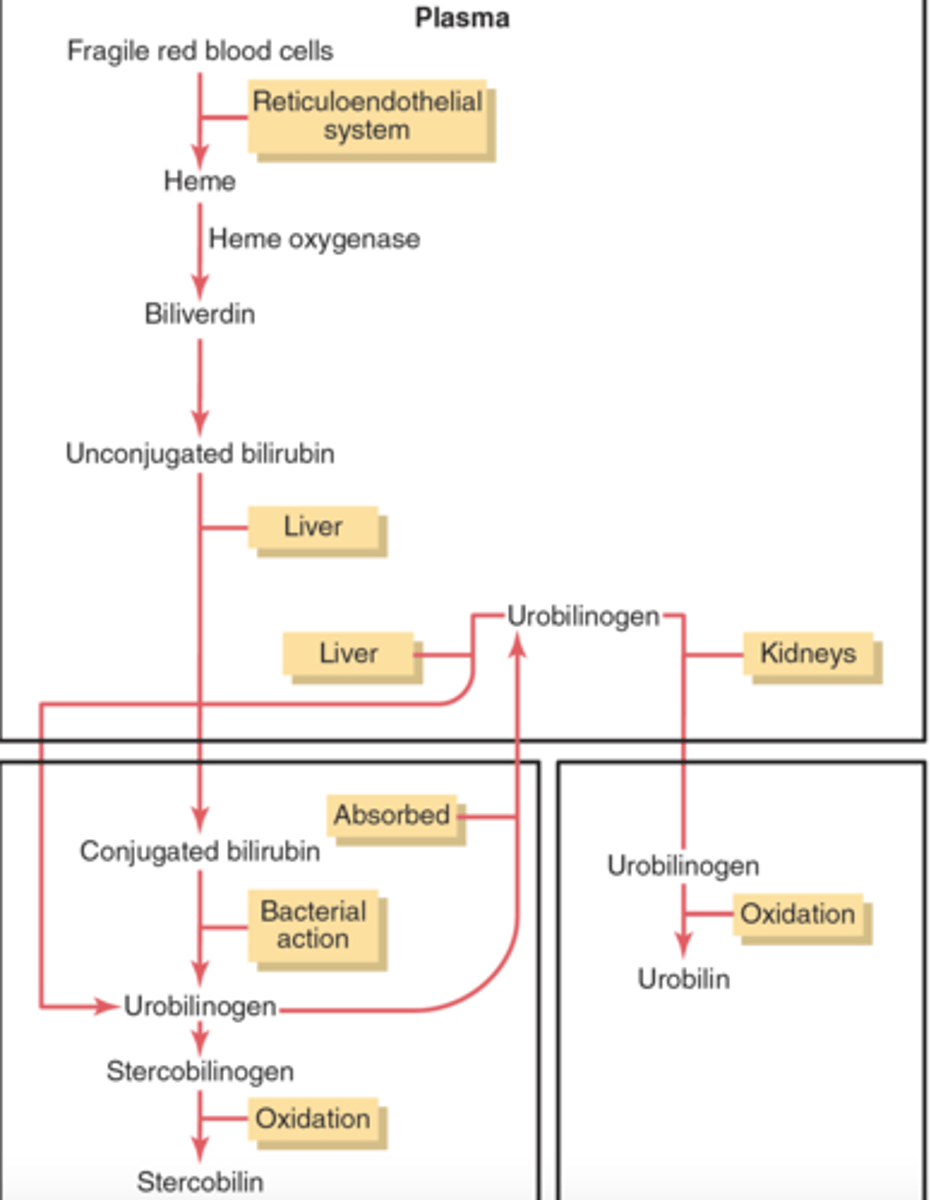
a pt is diagnosed with unconjugated hyperbilirubinemia. possible mechanisms?
1. hemolysis (liver cannot conjugate so much bilirubin)
2. intrahepatic obstruction: bilirubin is in liver but is not conjugated (ex: liver damage)
intrahepatic obstructive jaundice mechanism
damage or obstruction within liver-> liver is not uptaking/conjugating bilirubin properly-> bilirubin enters lymph/blood= jaundice
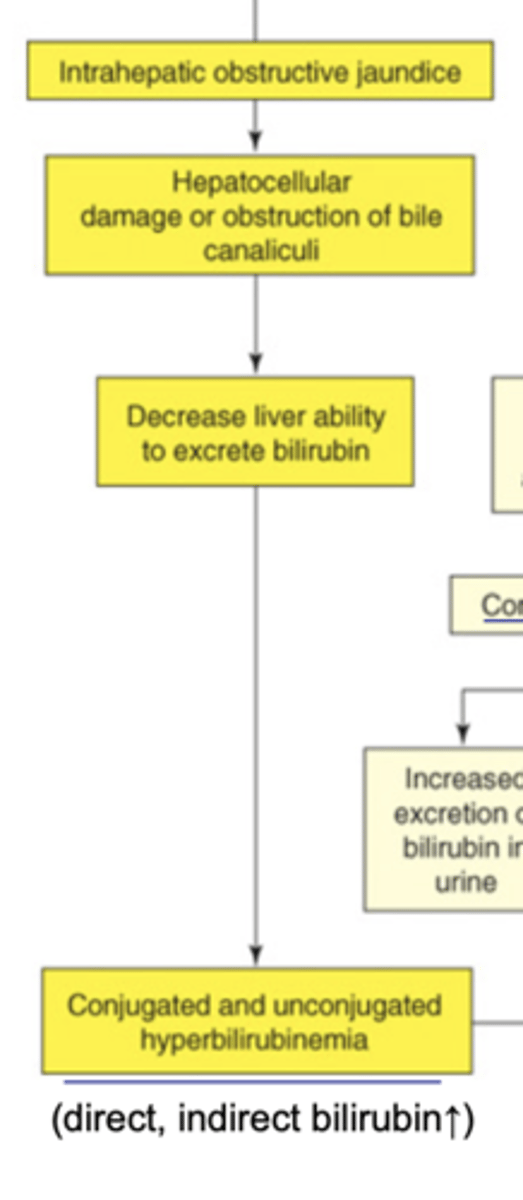
t/f: if the intrahepatic bile ducts are blocked, jaundice may be a result of both conjugated and unconjugated bilirubin
true. functional areas of the liver will be able to conjugate but the blockage/damage will result in unconjugated bilirubin via cell damage
extrahepatic obstructive jaundice mechanism
cholestasis (bile duct obstruction)-> conjugated bilirubin in bile is not excreted into SI-> backflow into lymph/blood/tissue= jaundice, light stools, possible more in urine
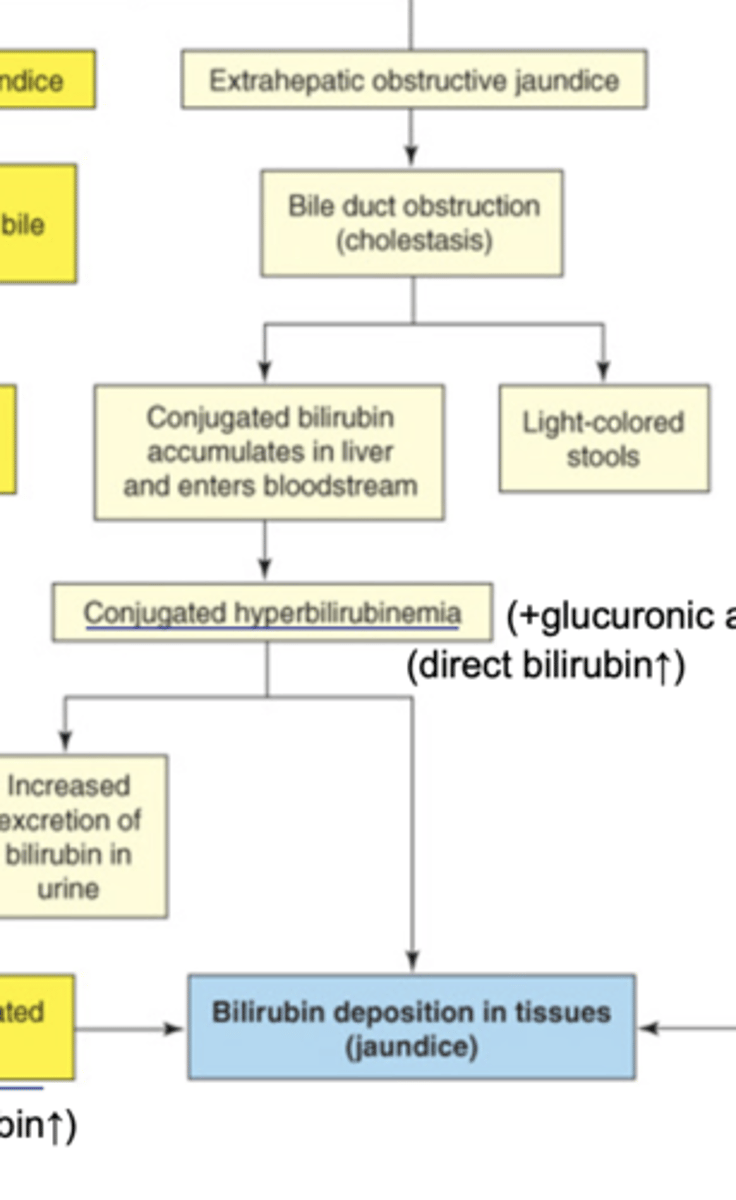
t/f: extrahepatic obstructions will always result in conjugated hyperbilirubinemia
true. liver has done its job of conjugation. extrahepatic obstructions will cause a backleak into lymph-> blood
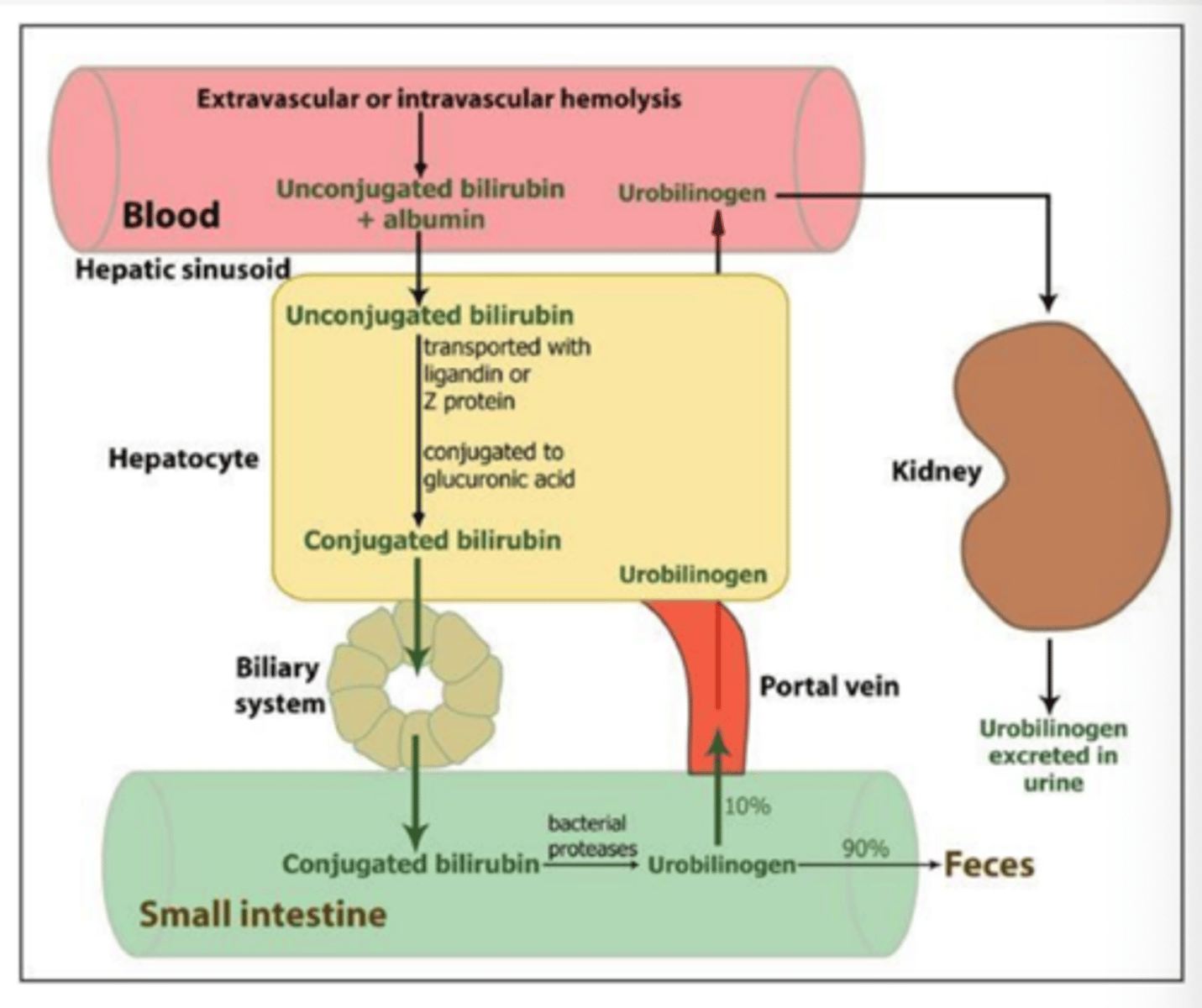
extrahepatic obstructions Sx in urine and feces
bile does not enter intestines= albino stools
increased excretion of bilirubin via urine= orange urine
causes of jaundice
pre-hepatic:
intra:
post:
pre: hemolysis of RBCs
intra: directly affect liver ability to remove bilirubin from blood or conjugate it [cancer, toxins, drugs, cirrhosis, neoplasms]
post: when bile flow is obstructed btwn liver and intestine [gallstones]
how does RBC breakdown lead to jaundice
RBCs contain hemoglobin which is broken down into bilirubin. large breakdown of RBCs lead to large bilirubin levels
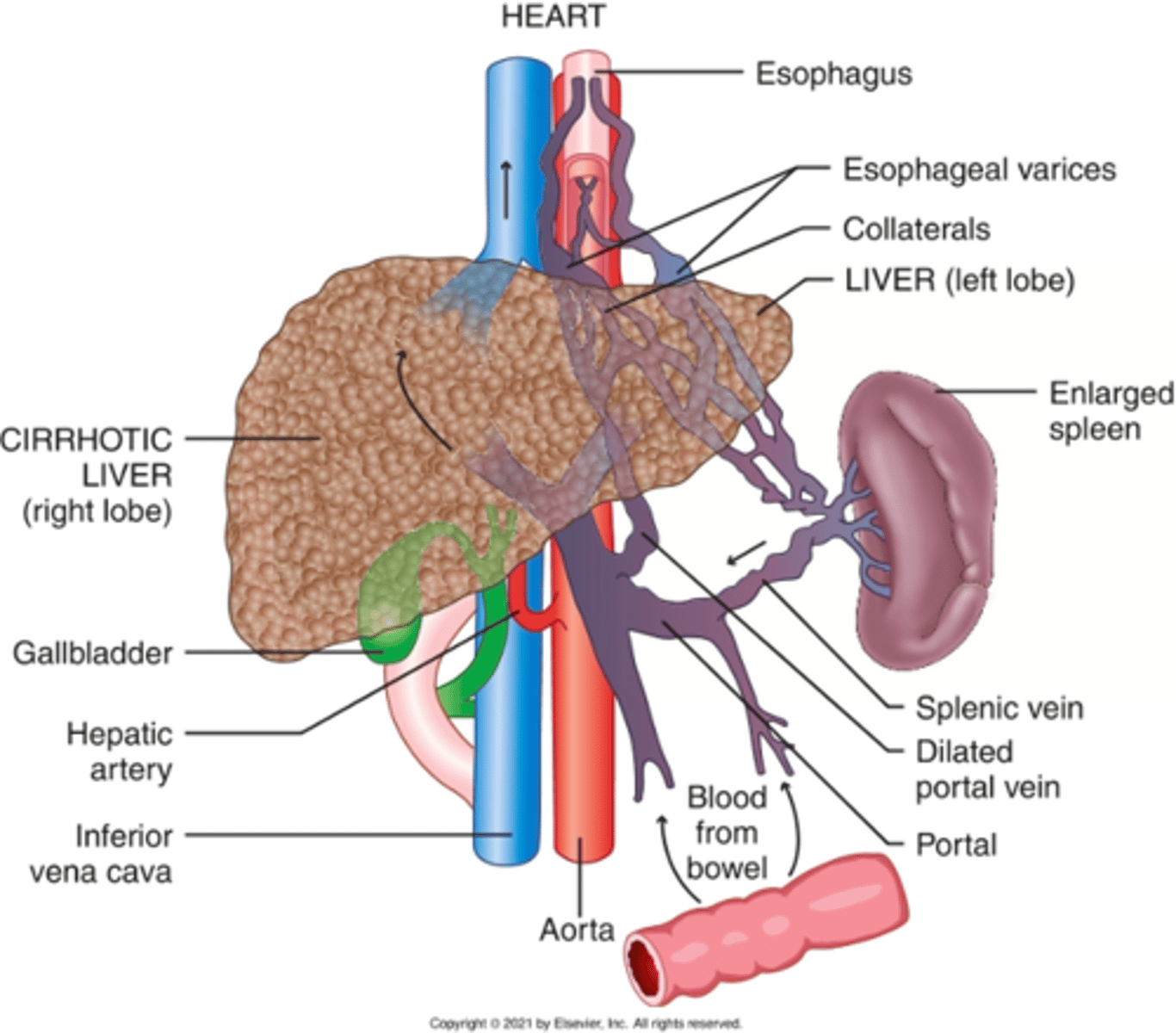
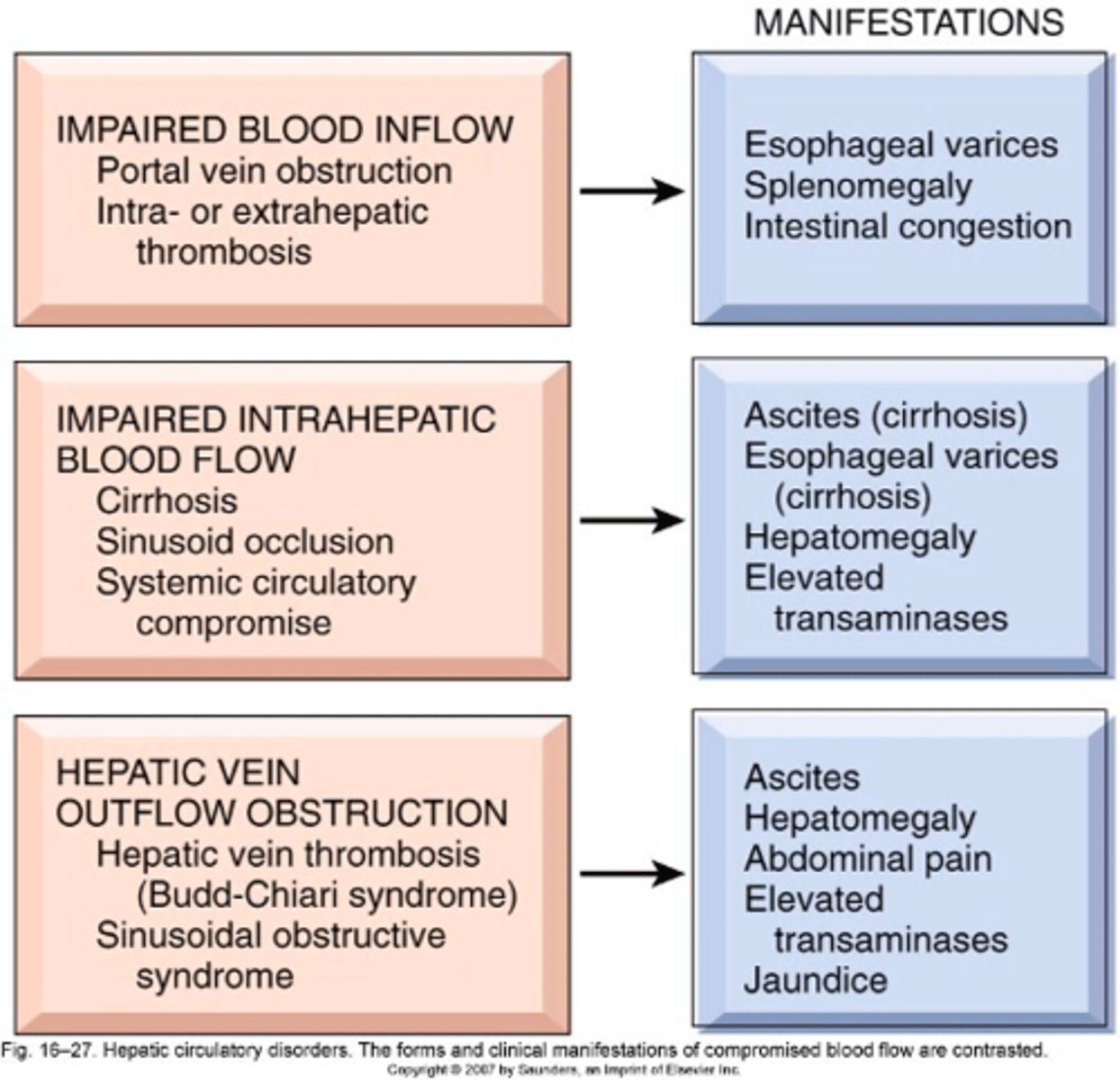
liver blood flow abnormality: pre-hepatic
where is blockage?
Sx?
1. Hepatic artery damage (Ox): hypoxia, ischemia
2. Hepatic a. or Portal v. thrombosis/ obstruction
Effect:
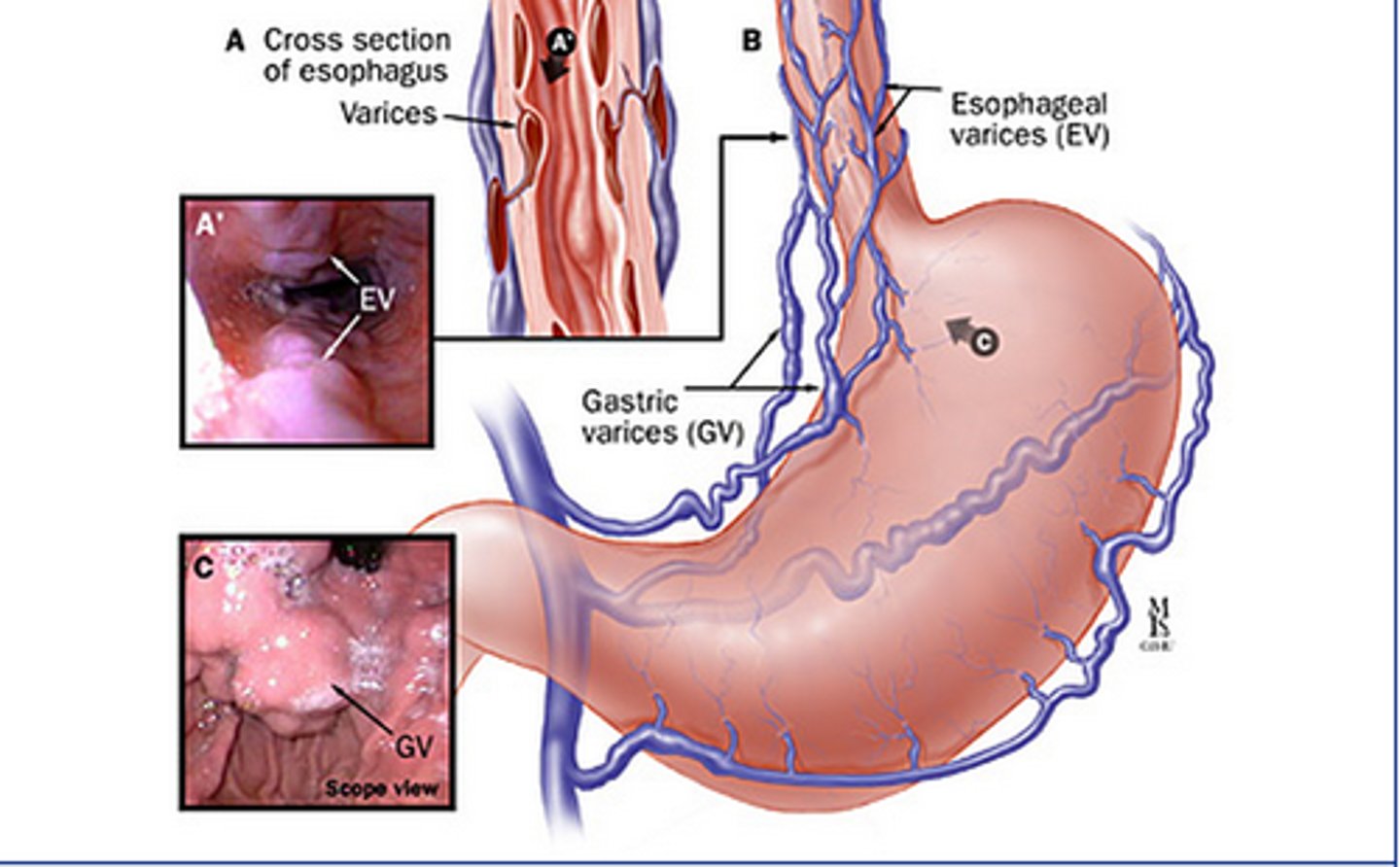
- Esophageal varices
- Splenomegaly
- Intestinal congestion/ varicose
Bc blood is getting shunted back/ away from liver in portal v. obstruction
(note no hepatomegaly bc not reaching liver)
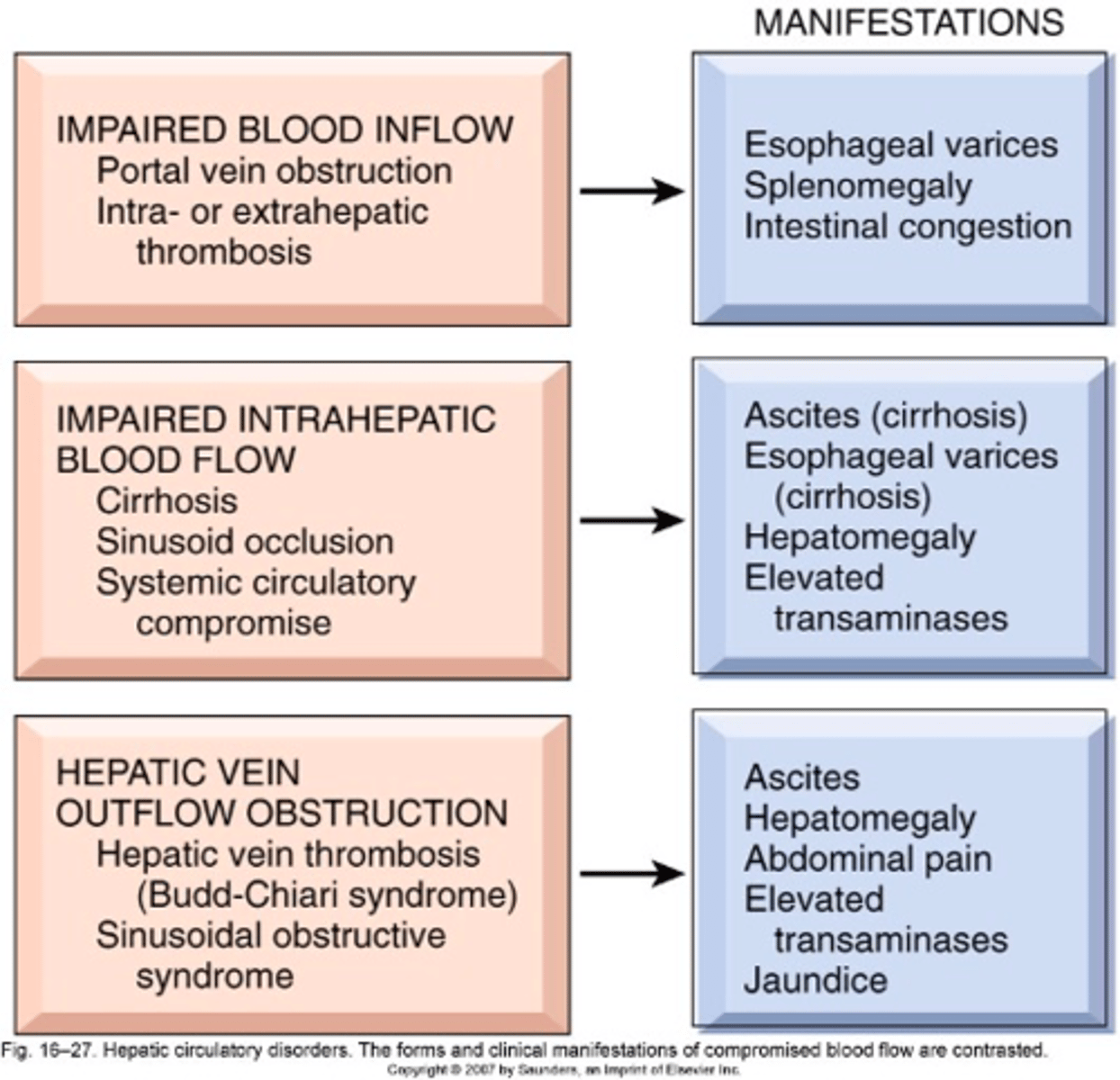
liver blood flow abnormality: intra-hepatic
where?
Sx?
1. Cirrhosis (poor blood movement)
2. Intrahepatic blood flow obstructions
3. Systemic circulatory compromise
Sx:
- Ascites (fluid is pushed out of liver bc of buildup)
- Esophageal varices (shunted)
- Hepatomegaly
- Elevated transaminases
Blood is not in all areas of liver; some back flow and some pooling in liver
liver blood flow abnormality: post-hepatic
where?
Sx?
1. Hepatic vein thrombosis
2. Obstructions
Sx:
- Ascites
- Hepatomegaly
- Abdominal pain
- Elevated transaminases
- Jaundice
Blood is not leaving liver-> backflow and leak into tissues
t/f: hepatomegaly is a common pathophysiology of portal vein obstruction
false. the portal vein brings blood from the GI tract to the liver. if it is obstructed then blood is not reaching the liver, therefore it will not enlarge
t/f: hepatomegaly is a common pathophysiology of hepatic vein obstruction
true. the hepatic vein carries deOx blood from the liver back to the heart. if it is obstructed then there is a backup of blood in the liver, causing enlargement
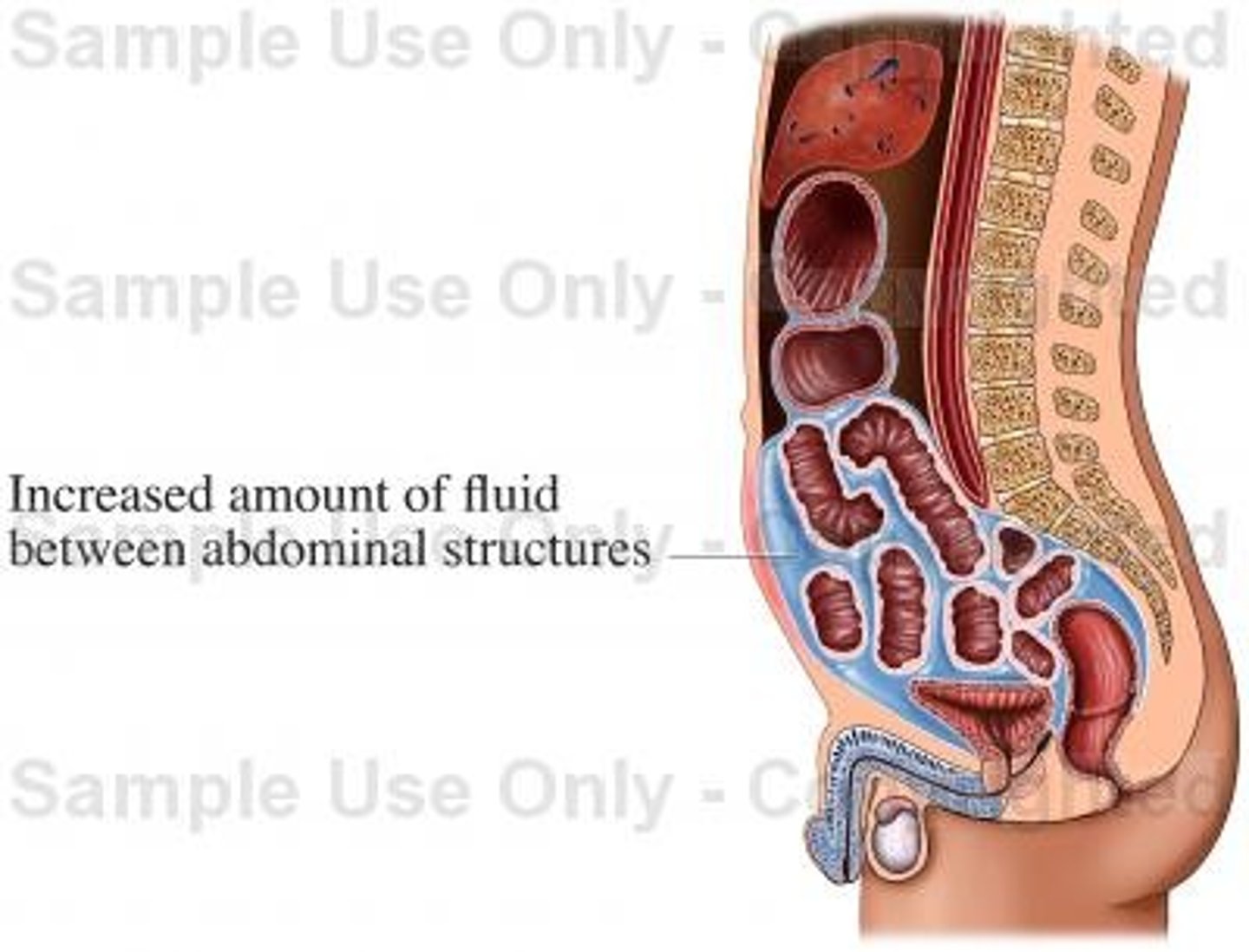
ascites
what is it?
when does it happen in impaired liver blood flow?
accumulation of fluid in the abdominal cavity
= occurs in intrahepatic and posthepatic obstructions (liver accumulates fluid-> ends up in tissue)
explain 2 ways how liver cirrhosis can lead to ascites
1. lymphatics/vessels are blocked from scarring= extra fluid ends up in tissue
2. low albumin production= edema
what does "congestion" mean in terms of blood flow
venous blood is pushed back into organs == dilates veins-> varicose

t/f: esophageal varices are common pathophysiologies of hepatic vein outflow obstructions
false. esophageal varices are pathophysiologies seen in impaired blood INflow and impaired INTRAhepatic blood flow. its usually due to the shunting of blood in the portal system back to organs.
t/f: ascites is a common pathophysiology of impaired blood inflow to the liver as a result of the blood being shunted to tissue
false. ascites is a common Sx of intrahepatic and posthepatic blood flow obstructions (NOT prehepatic). in prehepatic there is no hepatomegaly so the fluid isnt being pushed out into the tissues
pathologic conditions affecting the hepatobiliary system
1. injury from drugs and toxins (first pass, goes to liver first)
2. infection, inflammation, immune
3. metabolic disorders (ex: ethanol)
4. neoplasms (metastasis, not usually primary)
phase 1 vs phase 2 liver metabolism
P1: oxidations via cytochrome P450s
= make drug less active and more polar
P2: conjugation rxns
= caps free radicals
= makes molecule more water-soluble
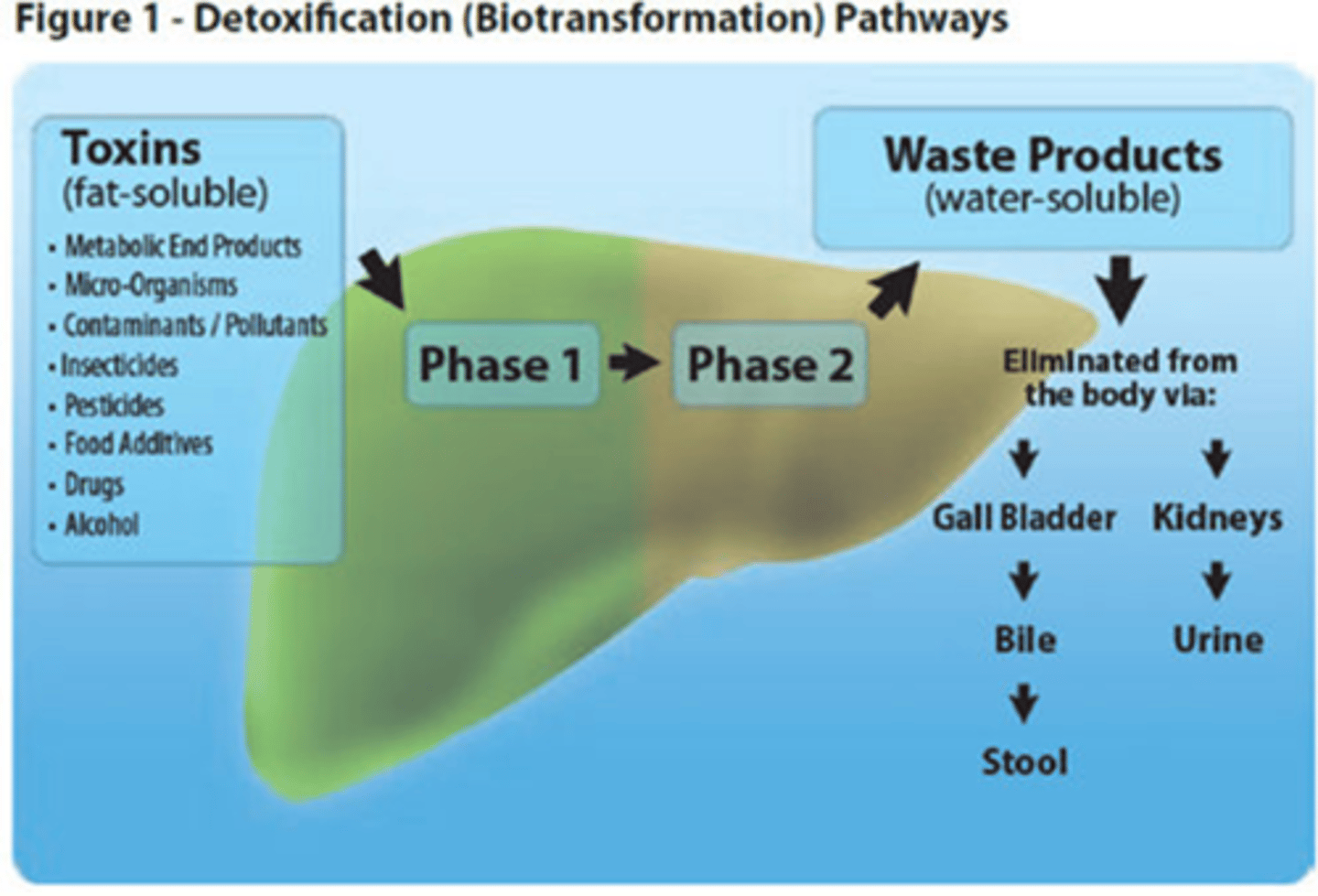
which phase of metabolism often results in free radical production
P1 (momentarily; P2 usually caps the free radical)
t/f: phase 1 reactions are more abundant than phase 2
true. phase 2 reactions can get behind/ run out of conjugation molecules, leading to more free radicals= necrosis, inflammation
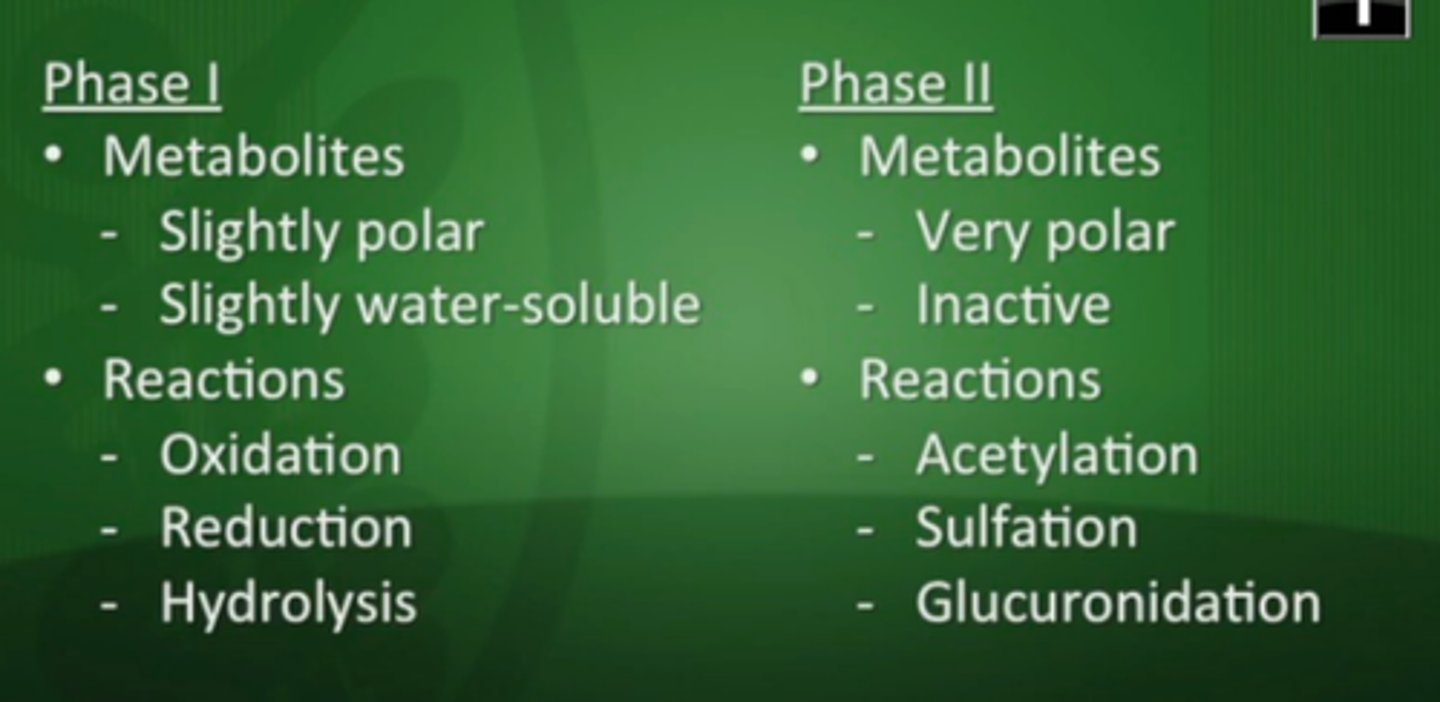
which phase of metabolism makes a drug more water soluble?
P2
which phase of metabolism makes a drug more polar?
P1
why is it important to monitor liver enzymes for certain medications
liver enzyme metabolism depends on genetics, could be diff for every patient
t/f: improper drug metabolism can lead to cirrhosis
true. production of free radicals will lead to damage= chronic inflammation= scarring
what can lead to an imbalance between phase 1/phase 2 rxns, leading to free radicals and liver damage
1. high drug concentrations
2. genetics
3. polypharmacy (more active drugs)
t/f: P1 reactions often give rise to free radicals and are inactivated by P2 reactions
true
host factors that contribute to drug-induced liver disease
1. genetics (missing CYPs)
2. age (very young and old= lower fxn)
3. underlying chronic liver disease (scarring= worse metabolism)
3. diet/alcohol (induce or suppress metabolism)
4. polypharmacy (higher affinity drug is metabolized before low affinity= more active drug)
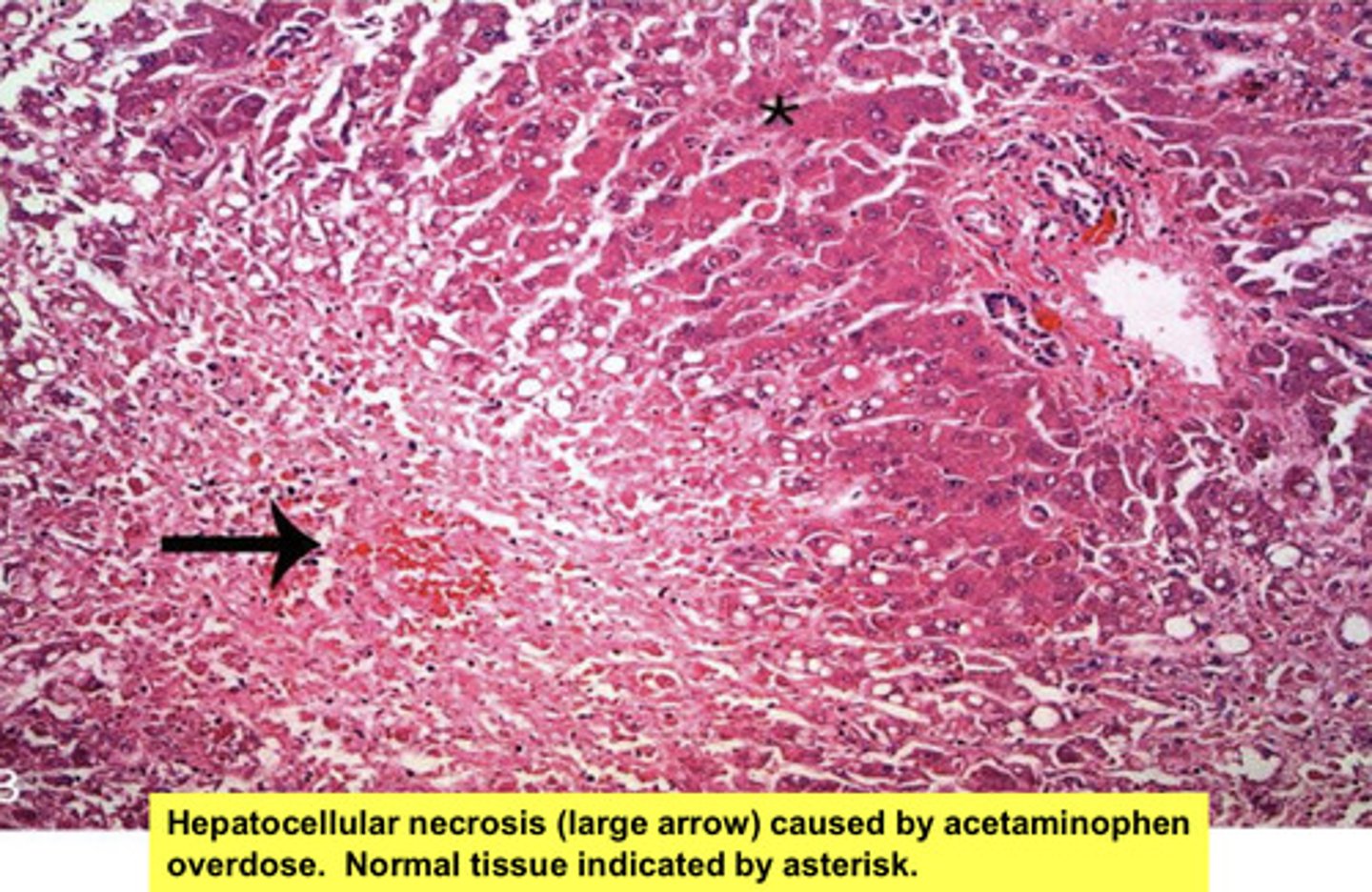
4 drug-induced liver diseases
1. direct hepatotoxic injury: free-radical byproducts from metabolism
2. idiosyncratic rxns: genetic
3. cholestatic rxns: stasis; stuff isnt moving out of liver
4. chronic hepatitis: scarring, inflammation, poor function
what are idiosyncratic reactions of the liver
genetic; unpredictable response to drug
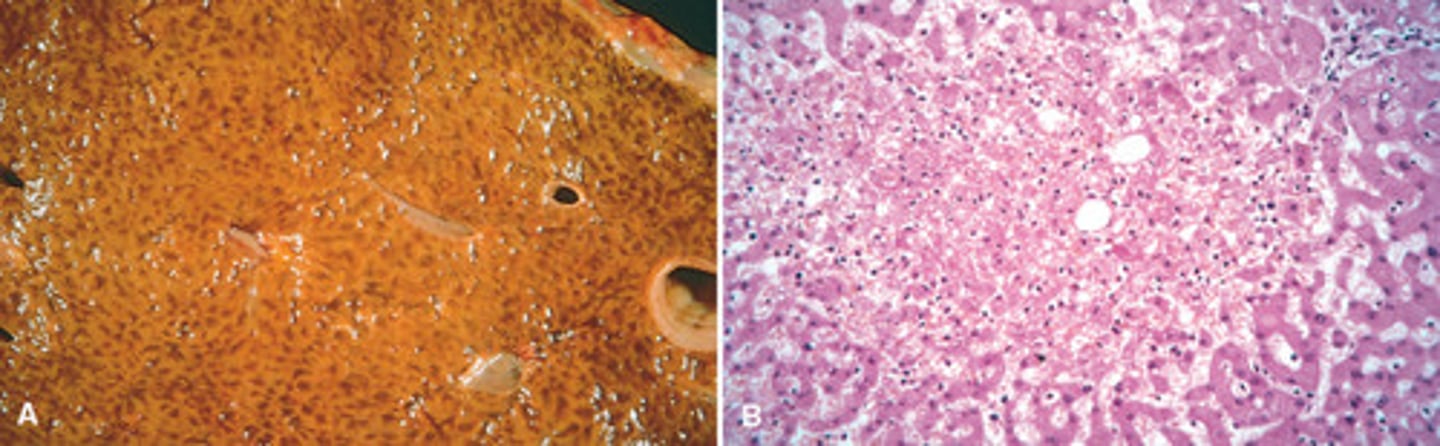
what does hepatocellular necrosis look like
pale, yellow scarring, coagulative necrosis, inflammation
Kupffer cell
resident macrophage in liver
liver fibrosis
Scar tissue forms, result of chronic inflammation
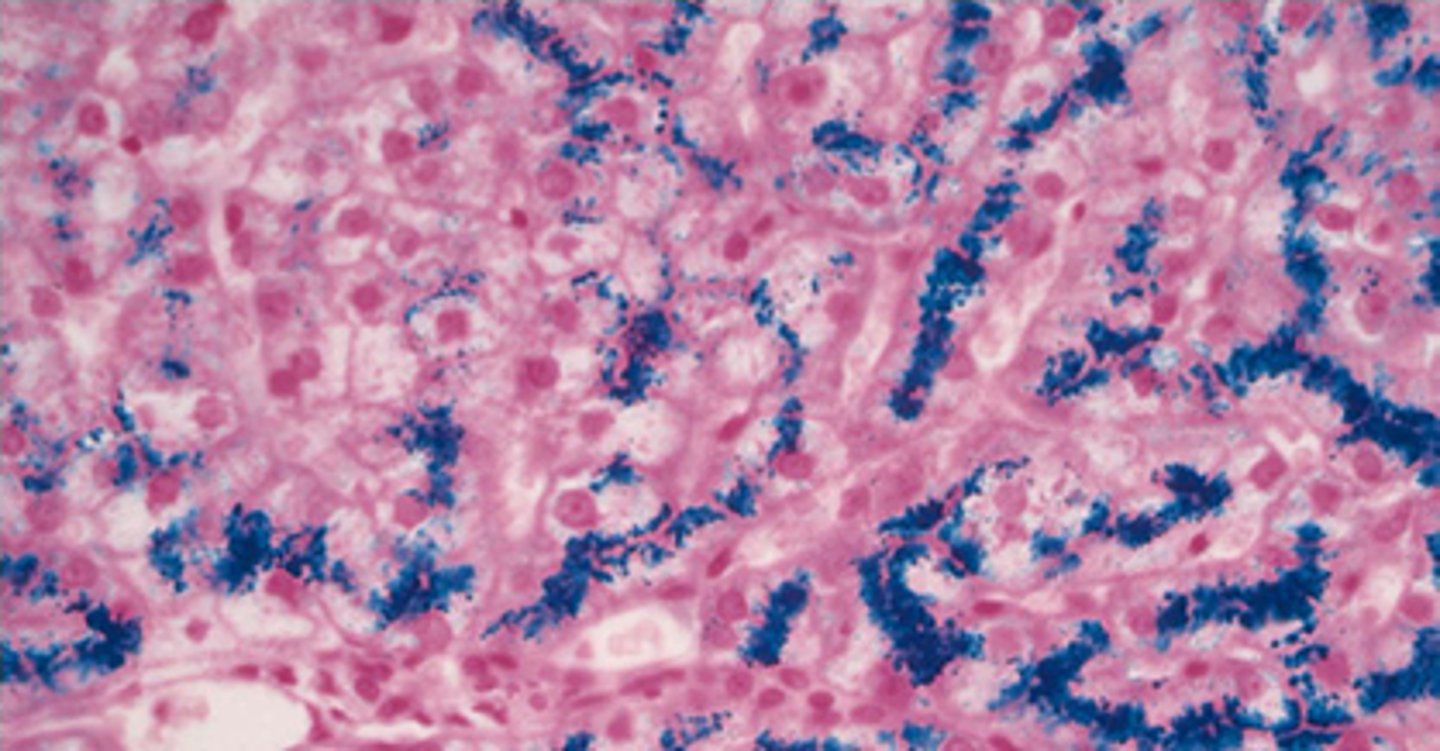
hemochromatosis
what is it?
stain?
excess iron deposits throughout the liver-> damage and dysfunction
prussian blue stain
nutmeg pattern of hemorrhagic necrosis
damage to liver vessels leads to mixing of extravasated RBCs with pale areas of the liver (necrotic cells)
causes of hepatitis
1. autoimmune
2. rxns to drugs/toxins
3. infectious (malaria, mono, salmonella...) (target bloodstream which goes through liver)
4. viruses
endogenous/aseptic hepatitis etiologies
1. autoimmune
2. liver is indirectly inflamed not bc its infected but bc theres inflammation in other areas of the body (changes in bloodstream)
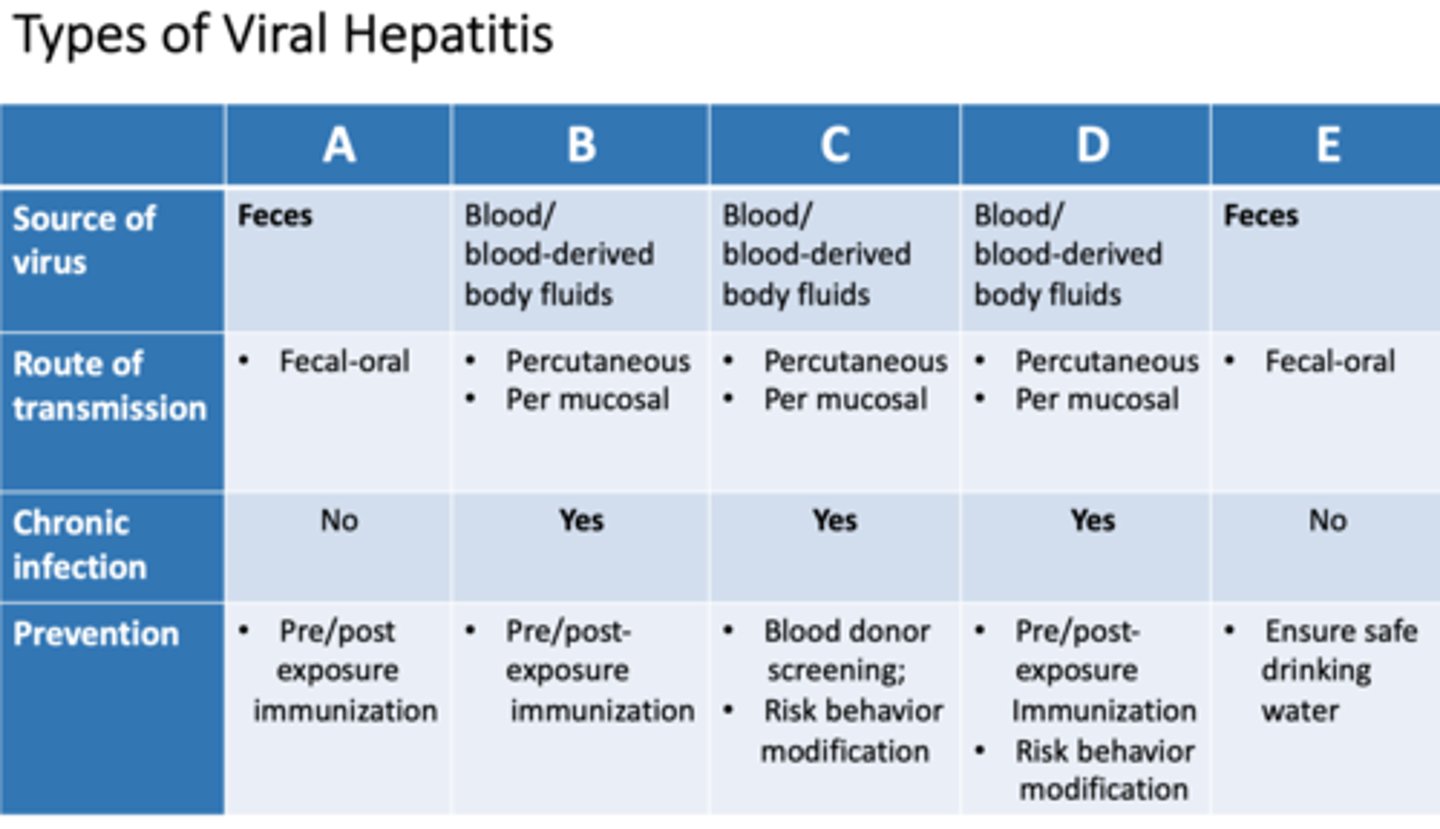
hepatotropic viruses are?
examples?
viruses that need hepatocytes as host cell
= A,B,B-delta, C,E [virus mutated in different form]
![<p>viruses that need hepatocytes as host cell</p><p>= A,B,B-delta, C,E [virus mutated in different form]</p>](https://knowt-user-attachments.s3.amazonaws.com/4602f190-fcc8-4964-8479-9ac054c35b88.png)
2 mechanisms of cellular injury in viral hepatitis
1. direct cellular injury (virus uses cell as host)
2. induction of immune response against virus (collateral damage)
t/f: hepatotropic viruses always reside in the liver and often cannot survive in other environments
false, large blood flow in liver, viral particles can get into bloodstream
which WBCs are present in hepatitis
lymphocytes
t/f: hepatitis infections often trigger hepatocyte apoptosis, leading to a lower inflammation reaction
true
sequence of events in hepatitis infection (from incubation to recovery)
1. incubation phase (after exposure)
2. prodromal (preicteric phase): no specific symptoms, but feel sick
3. icteric phase: specific symptoms (jaundice, fever, inflammation)
4. recovery phase (complete/recovery or incomplete/healing)
in which phase of a hepatitis infection can you see specific symptoms such as jaundice
icteric phase
chronic active hepatitis
acute exacerbations of hepatitis have subsided, but there is no recovery-there is low level activity of virus
fulminant hepatitis
initially infected cell has ruptured next to non-infected neighbor cell-> release of intracellular enzymes-> digest non-infected neighbor-> more necrosis/inflammation
(indirect type of damage)
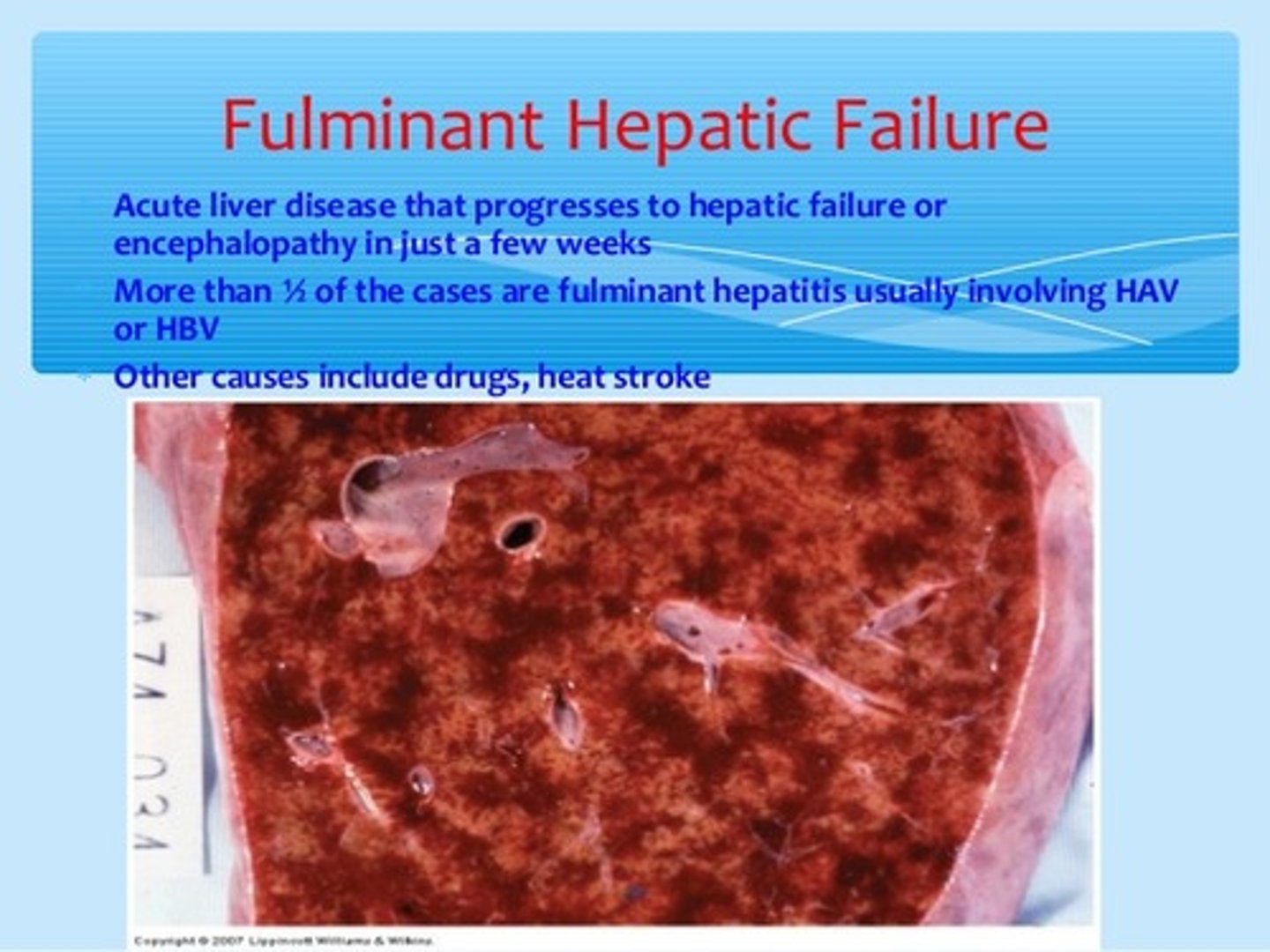
in which form of viral hepatitis is there indirect injury to hepatic cells that are not infected by a virus
fulminant hepatitis
HepA
-found where in infected individuals?
found in feces, bile, sera of infected individual
HepA
transmitted by?
fecal-oral route
=contaminated shellfish, unsanitary conditions, food/water contamination
t/f: hepatitis A recovery is usually spontaneous and highly resolvable
true. HepA is benign, self-limited, resolves spontaneously
Summarize the HepA chart
incubation/acute disease/recovery?
Incubation (4 weeks): viral particles appear in liver first (prodromal phase)
Acute (4-8w): viral particles in liver, feces (bile), blood = symptoms (icteric phase)
Recovery(8-12): no viral particles in feces/blood; levels slowly drop in liver
-not carrier, not chronic
which antibodies serve as memory cells for hepatitis A
IgG (but IgM made initially)
how is HepB transmitted
infected blood, sexual contact, body fluids, contaminated needles, maternal transmission (third trimester)
t/f: HBV is more serious than HAV
true
t/f: HAV can be transmitted to the fetus if the mother is infected during the third trimester
false. HBV can
Acute HepB with recovery
incubation period?
acute period?
transmission?
Incubation (2 months): virus is in blood first (that's how its transmitted)
Acute (2-4 months): virus enters liver
=no transmission after 4 months if recovered. possible transmission if carrier
what is different in chronic HepB chart compared to acute hep B with recovery
Acute disease in chronic is less intense, lasts longer, low level of inflammation
Virus remains in blood (unlike acute which is gone after 4 months)= possible transmission, symptomatic
HepB carrier state
Same as chronic but active acute disease is lower=no symptoms but they are infectious (virus is still in blood)
can patients with chronic hepatitis B transmit the virus if they do not have acute exacerbations
yes. virus is still in blood. same for carriers with no symptoms
in HepB infections, what is the most frequent outcome? least?
most= subclinical or acute-> recovery
least= carrier (5-10) or chronic (4%)
most people with CHRONIC HepB viruses develop which outcomes
cirrhosis, carcinoma, or recovery
Hep__ is responsible for most cases of post-transfusion hepatitis
HepC
t/f: most HepC cases result in chronic hepatitis
true (50-80%)
t/f: most HepB cases result in chronic hepatitis
false. only 4%
how is HepC transmitted
contaminated blood sources (IV drug use)
similarities in HepB and HepC incubation
both take about 2 months to incubate and virus begins in blood (unlike A, 4 weeks and starts in liver)
which Hep viral infection is marked by intense acute exacerbations during chronic inflammation
HepC
most HepC outcomes are? least?
most= chronic (85%)
=resolution (15%)
=fulminant (rare)
t/f: most pts with chronic HepC exhibit cirrhosis
false. 20% exhibit cirrhosis and 80% are stable (but majority of HepC pts do have chronic inflammation)
which form of hepatitis has the most risk for hepatocellular carcinoma
HepC
t/f: cirrhosis results in a smaller liver
true. collagen fibers contract the liver, but it is heavy and dense
t/f: most chronic hepatitis cases are autoimmune
FALSE. 20% of chronic hep cases are autoimmune
t/f: in most autoimmune hepatitis, another autoimmune disease is present
true. ex:UC, SLE, RA
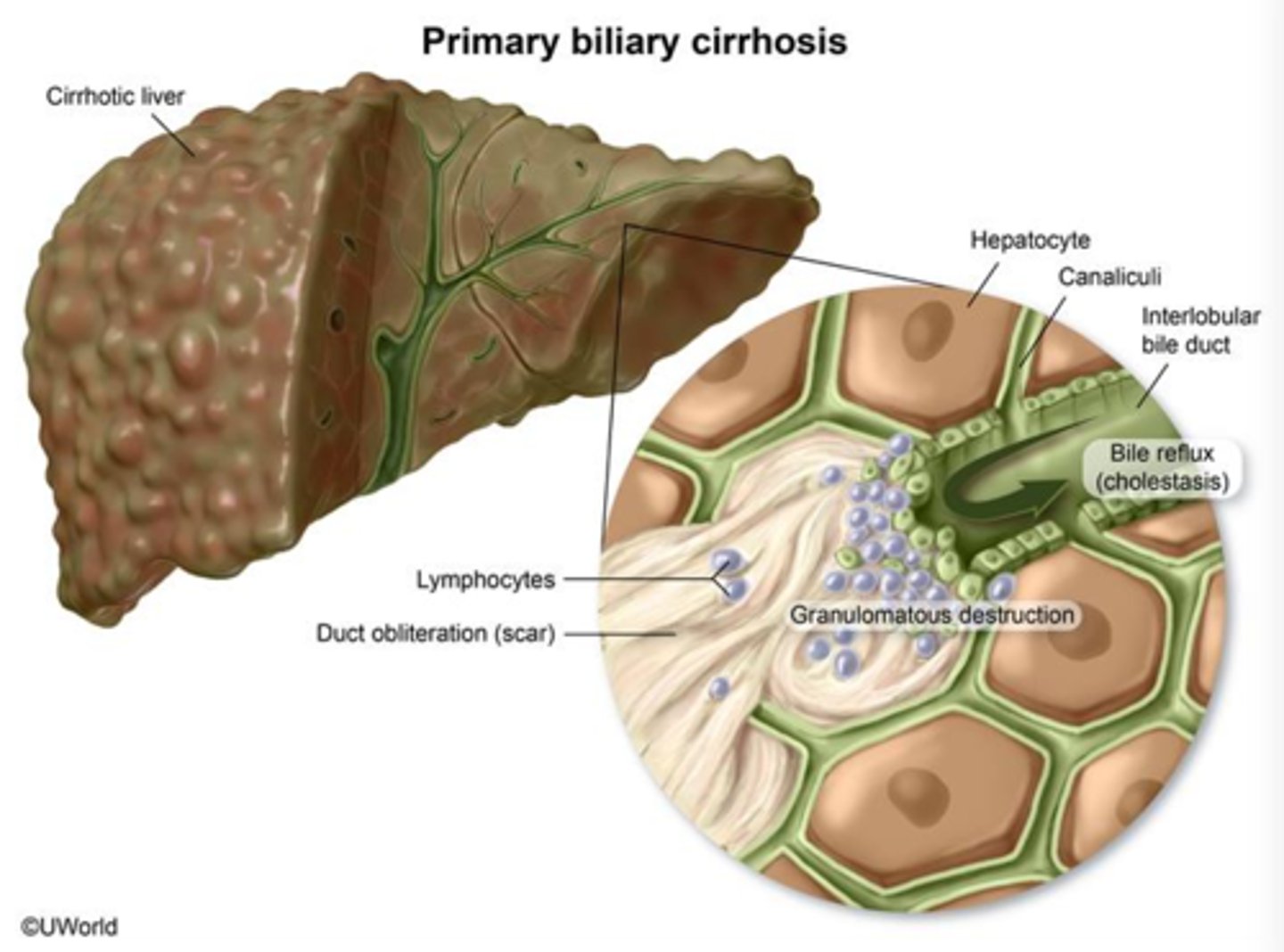
primary biliary cirrhosis
-autoimmune: auto antibodies target bile ductal epithelial cells (not hepatocytes)
-inflammatory destruction of intrahepatic bile ducts
primary sclerosing cholangitis
Inflammation and fibrosis of intrahepatic and extrahepatic bile ducts that presents with obstructive jaundice
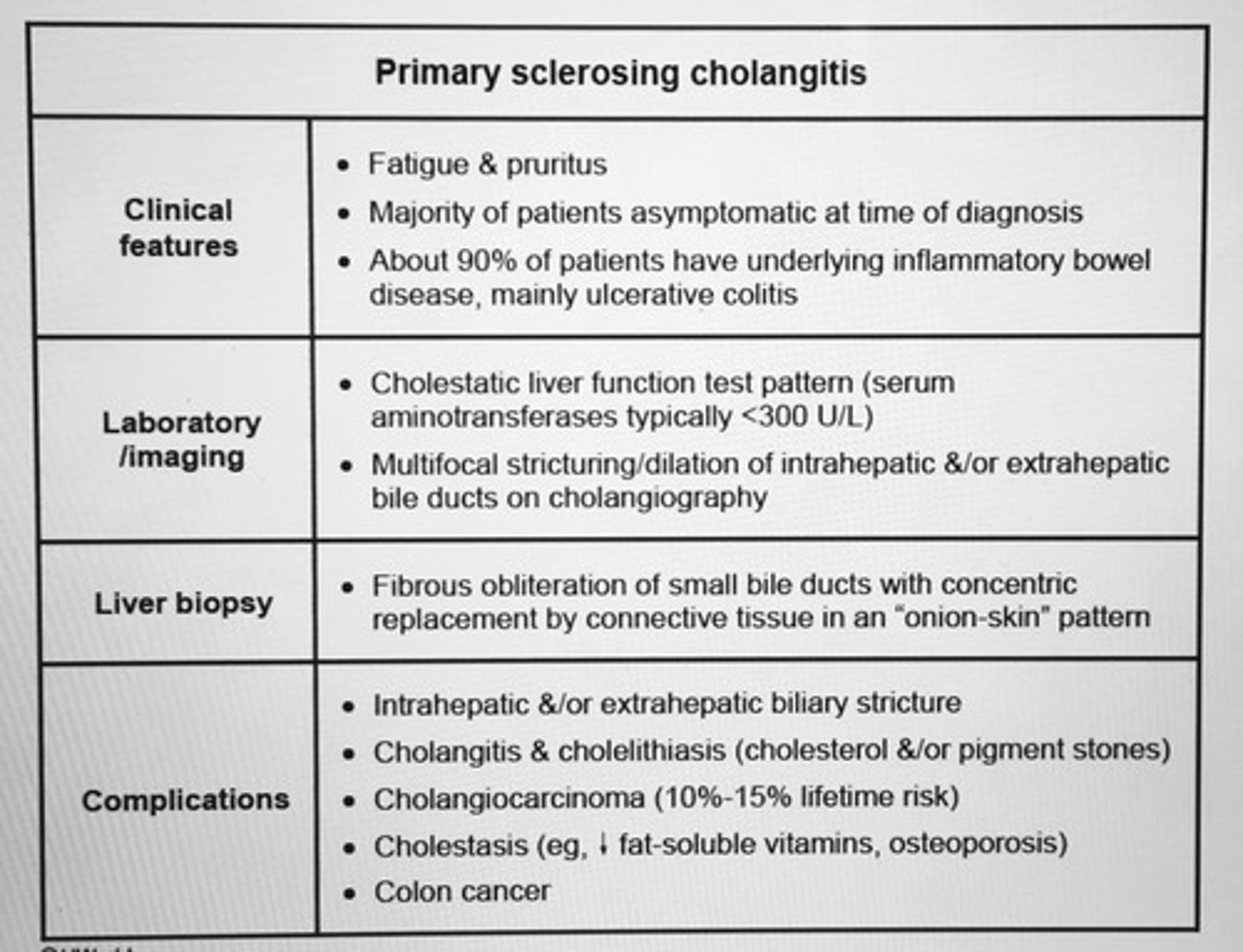
in which biliary disease is there hardening due to scarring
primary sclerosing cholangitis
symptoms of intrahepatic biliary disease
inflammation of bile ducts= disruption of bile flow-> backflow of bilirubin into lymph and blood
-pruritis/itching
-weight loss
-fatigue
-dark urine, pale stools
-jaundice
which type of hyperbilirubinemia do you expect to see in intrahepatic biliary diseases
conjugated, liver has conjugated the bilirubin but there is problem in bile duct flow
treatment of intrahepatic biliary disease
liver transplantation. you cannot separate out affected bile ducts
t/f: liver transplantations are considered a cure for intrahepatic biliary disease because you are removing the obstructed bile ducts
false. biliary disease is often auto immune, so the transplanted liver will be targeted by host's immune system
how is alcohol metabolized in the ADH system? where?
-via alcohol dehydrogenase
- in hepatocyte cytoplasm
EtOH-> acetaldehyde-> acetic acid