PHA 334 - Lecture #1 (Introduction)
1/124
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
125 Terms
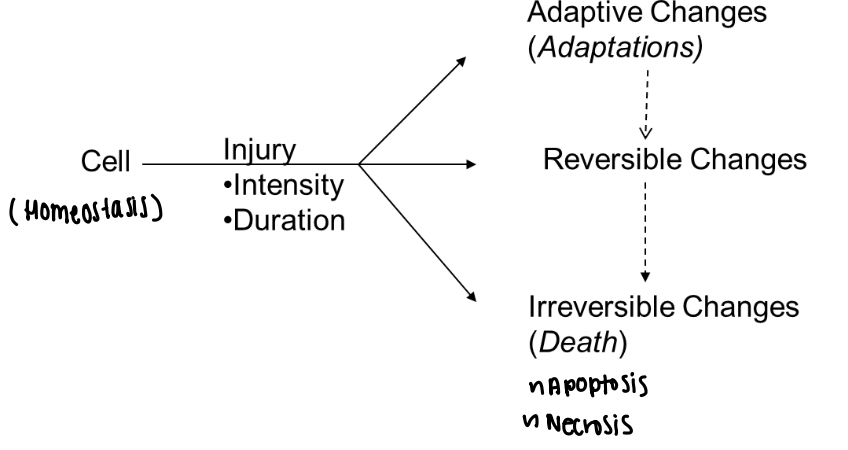
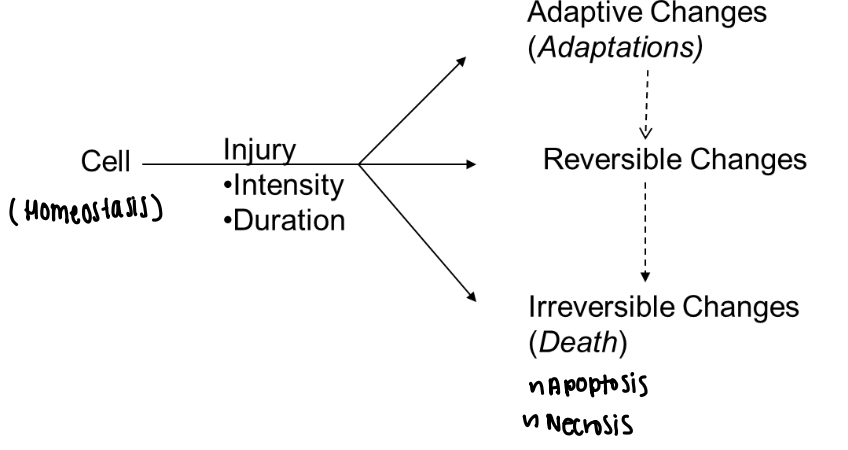
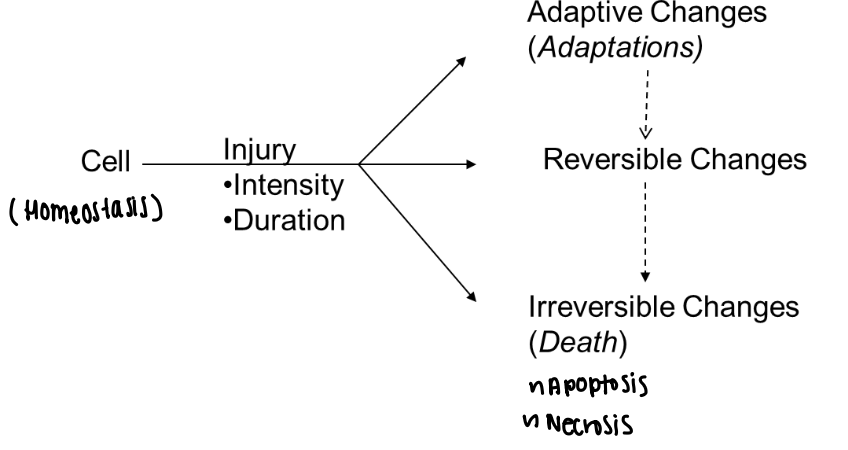
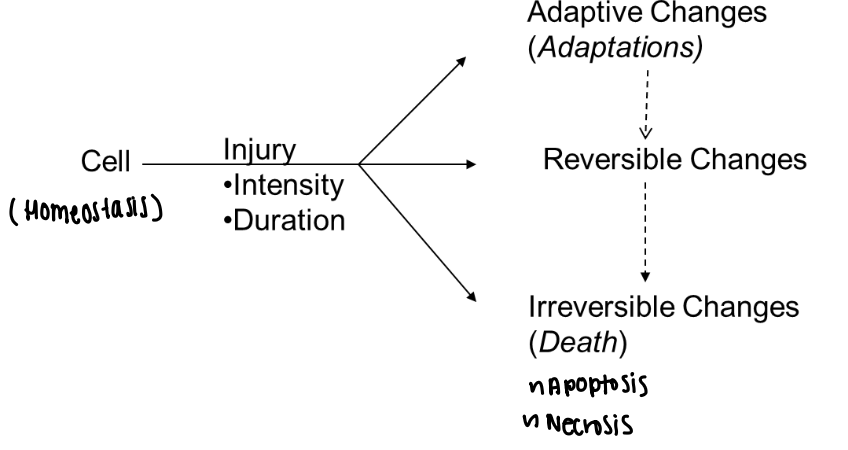
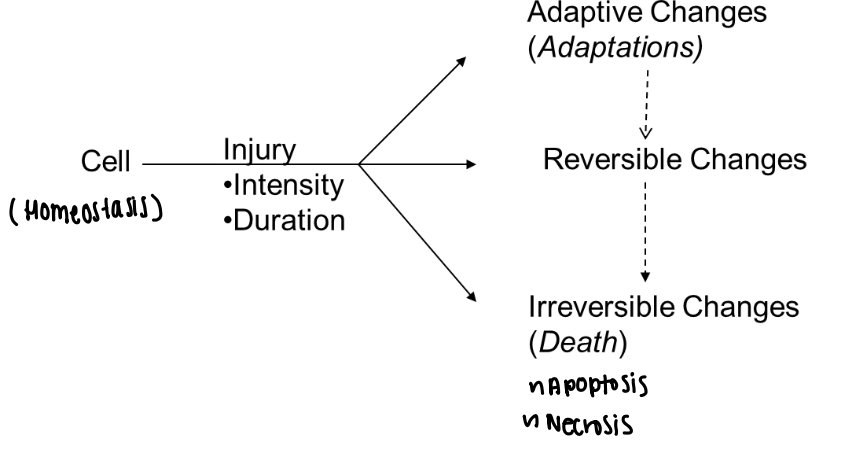
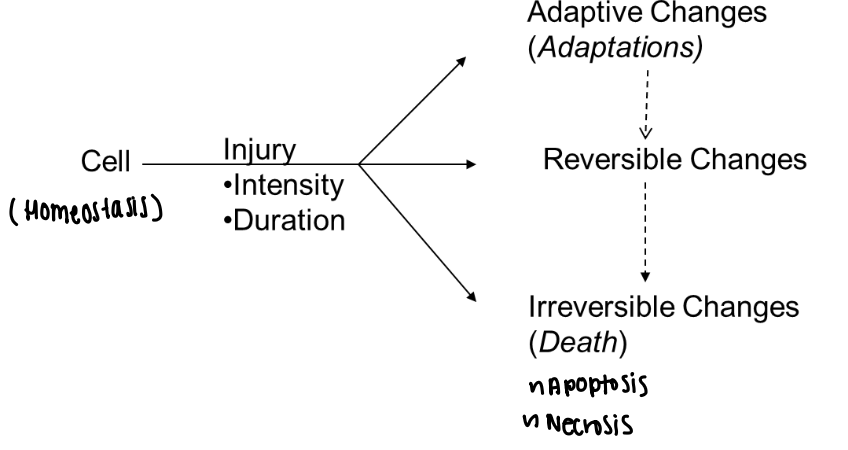
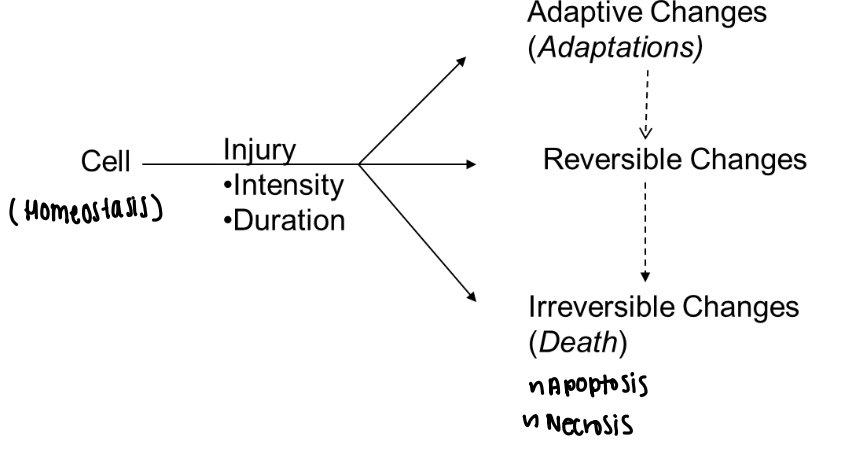
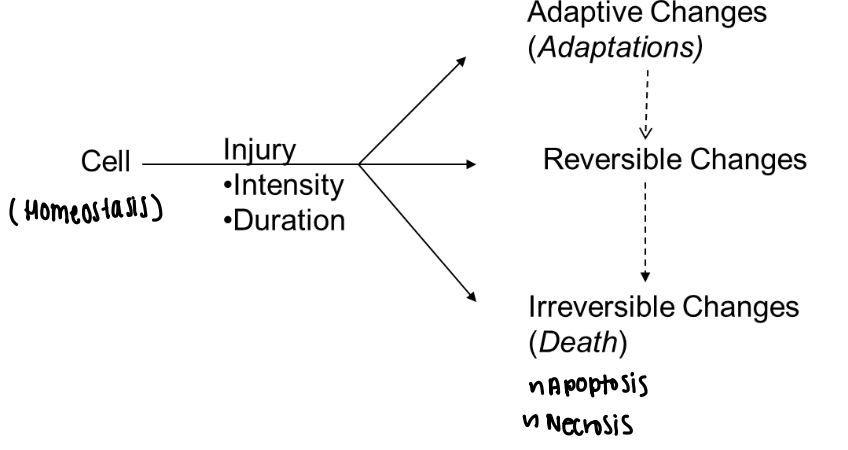
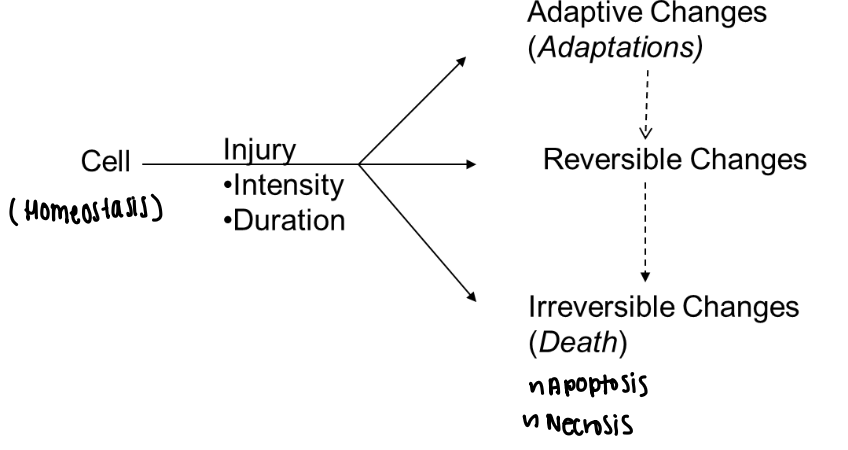
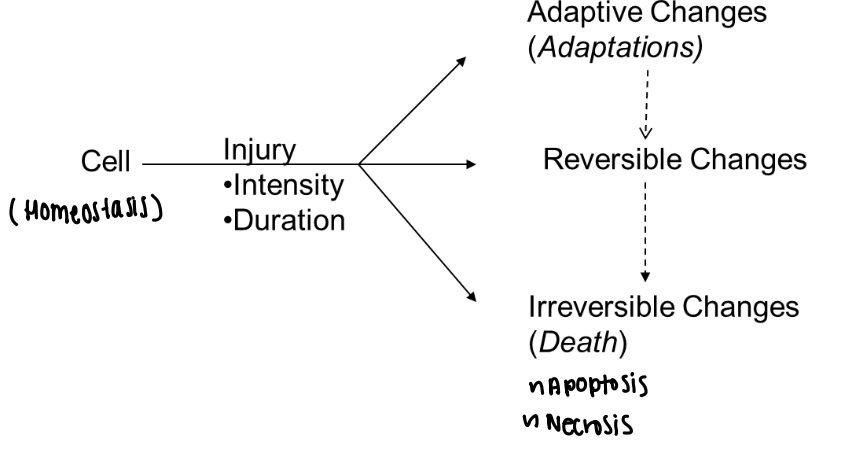
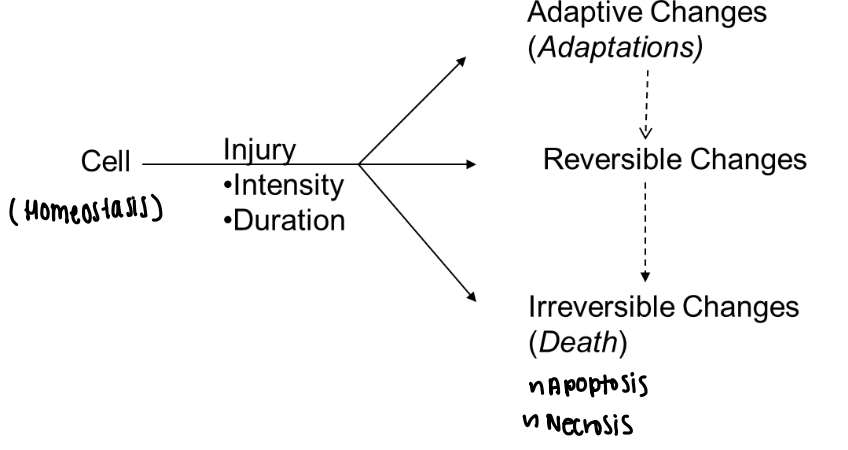
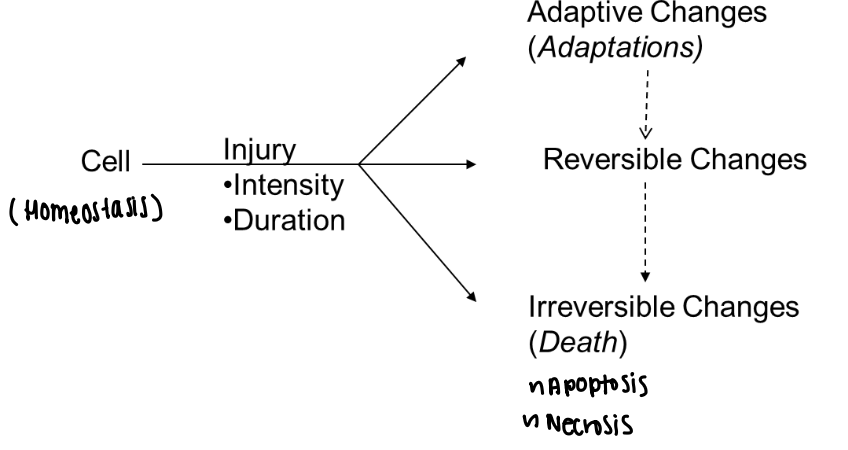
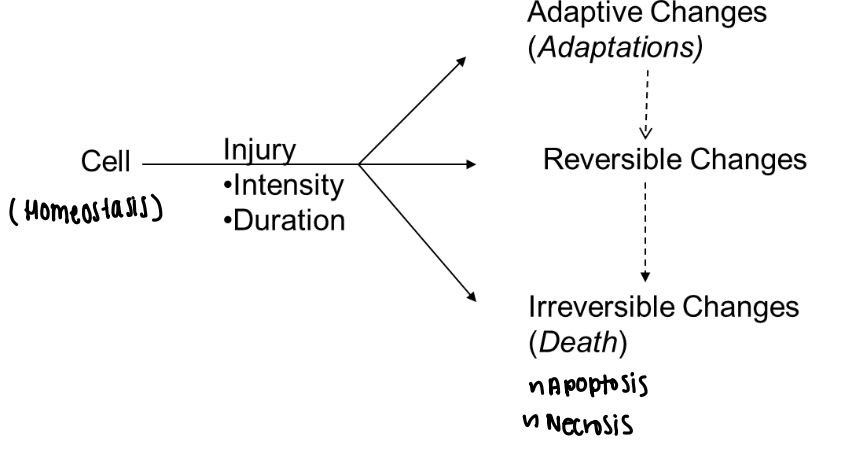
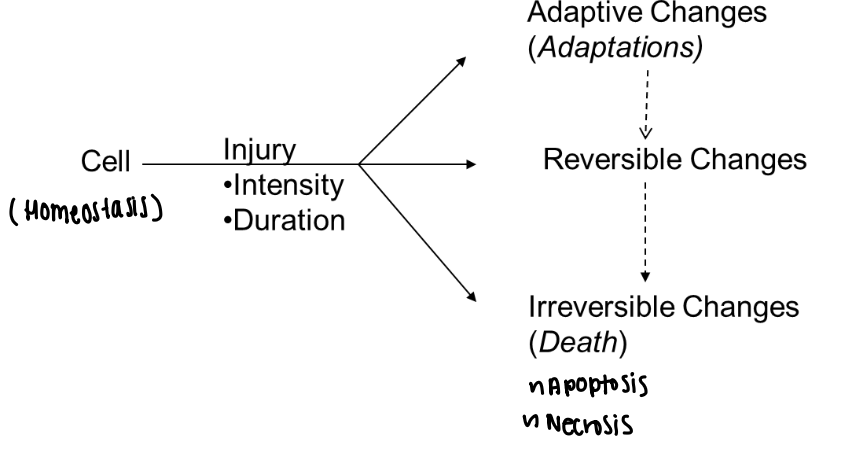
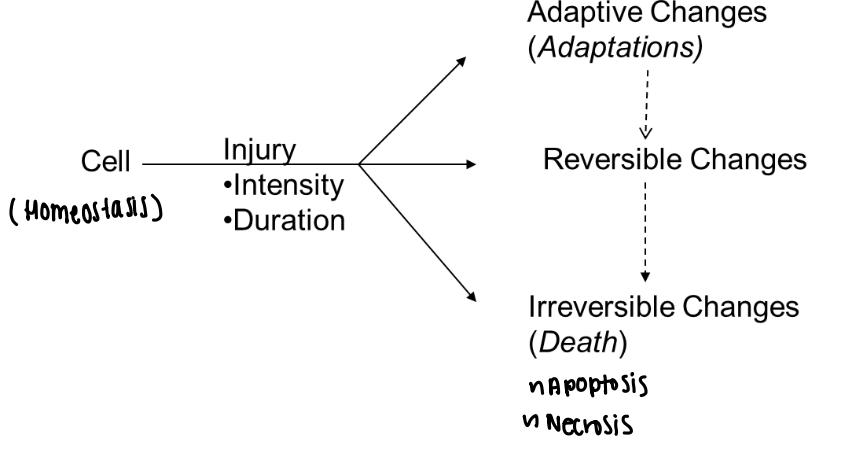
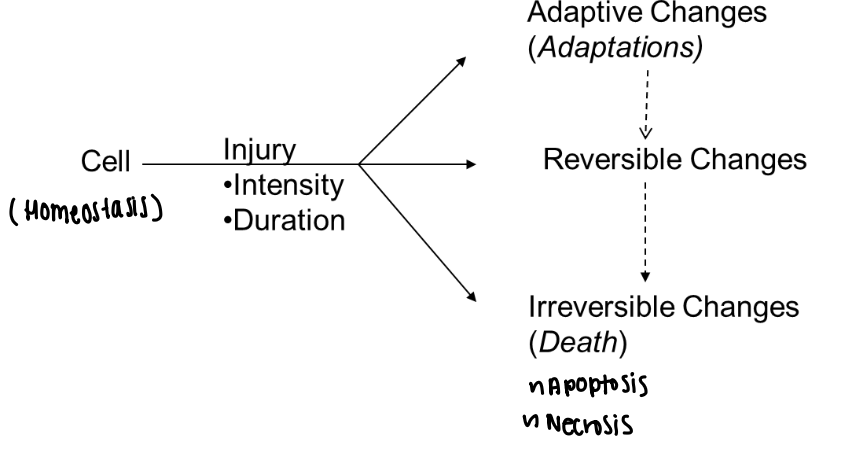
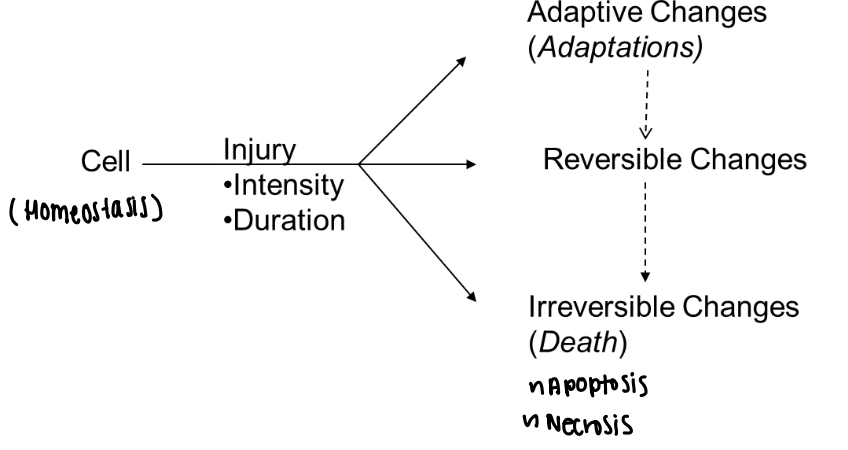
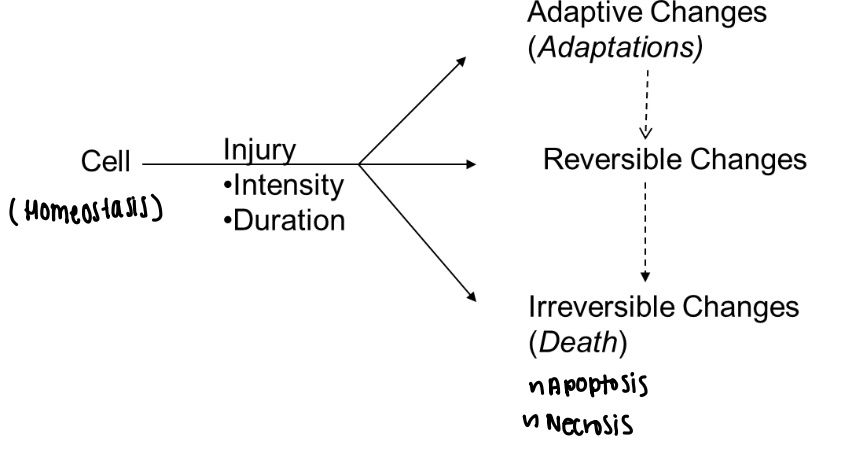
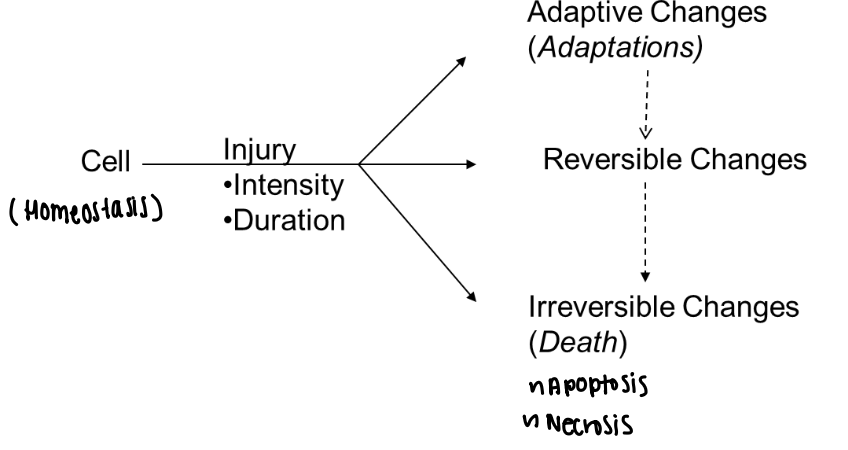
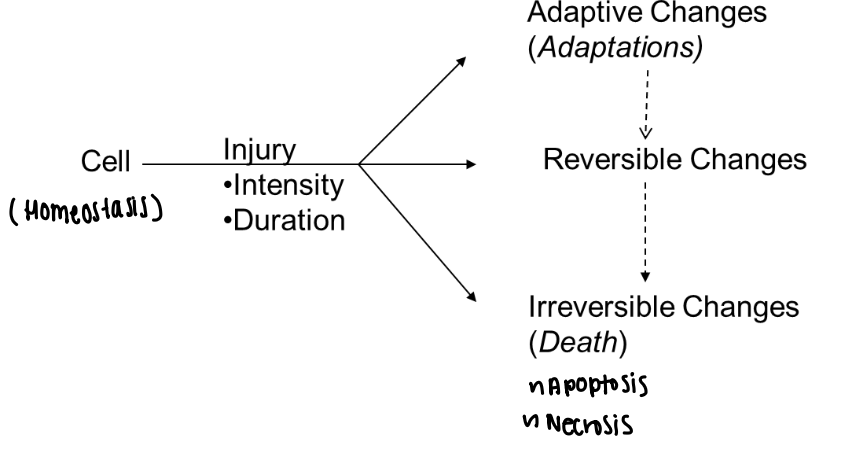
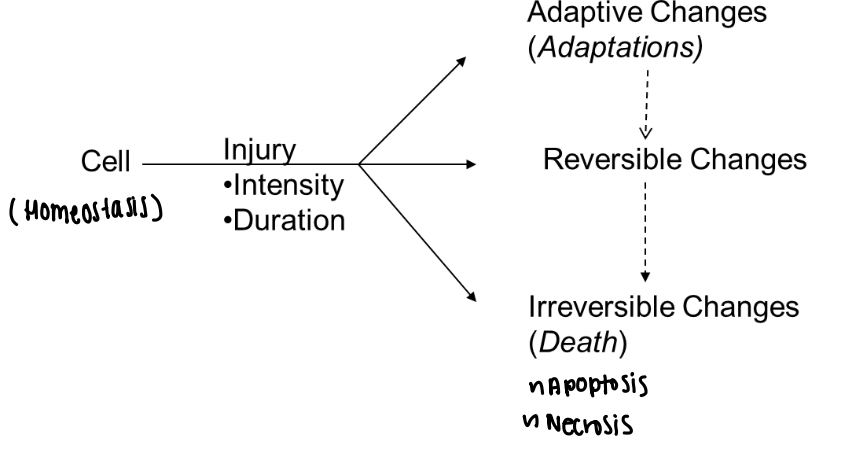
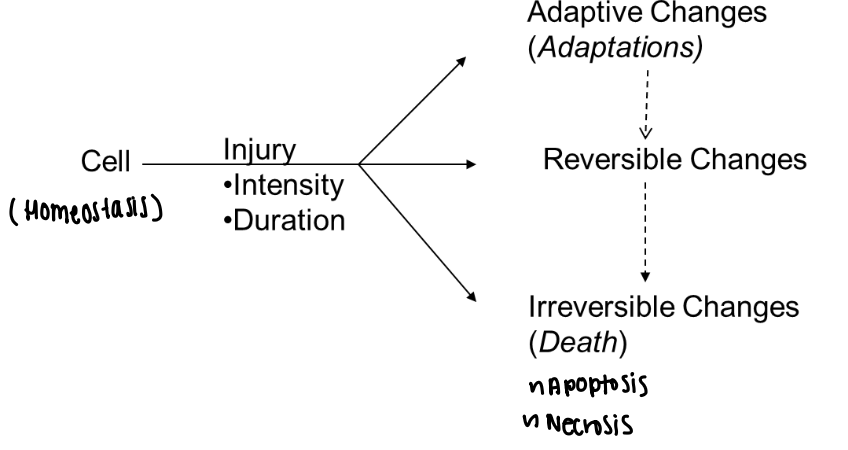
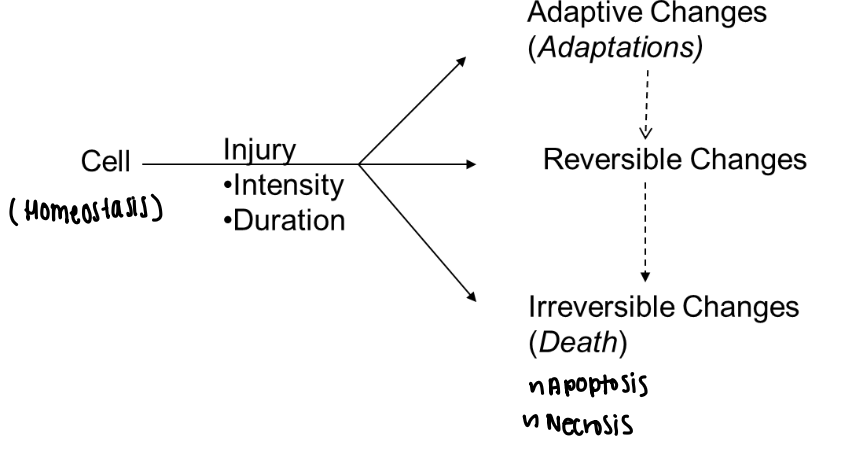
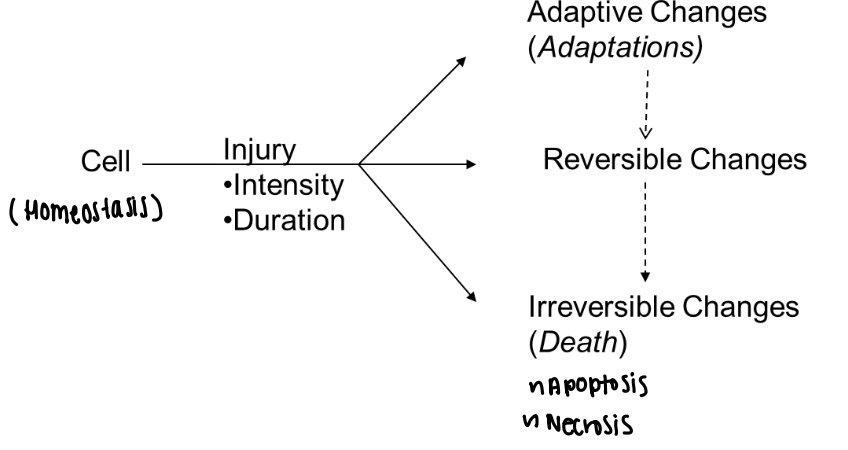
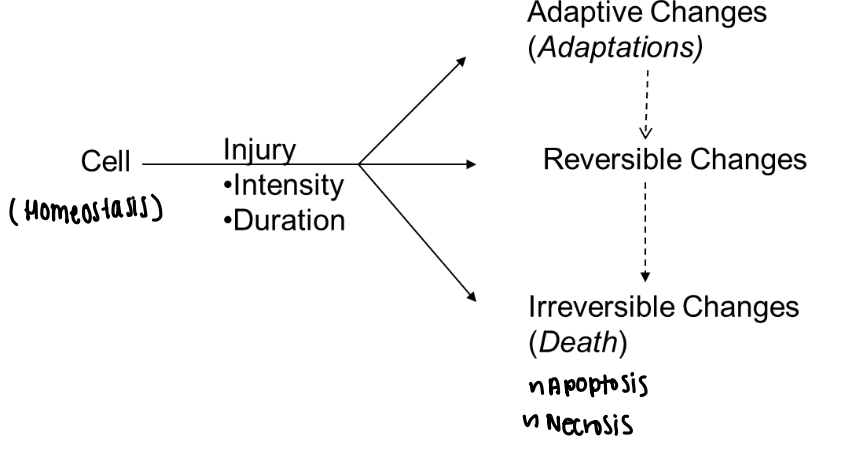
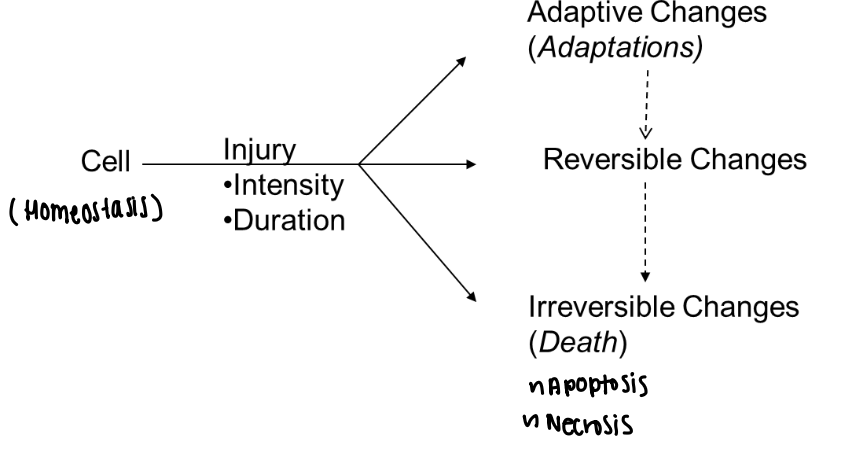
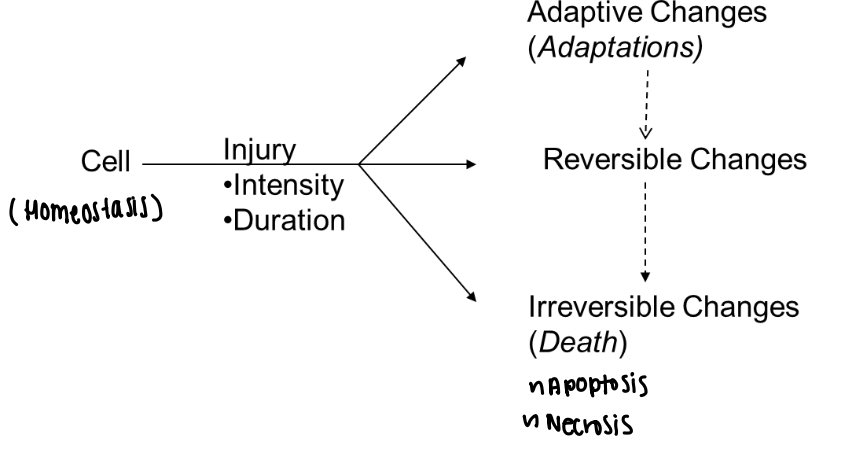
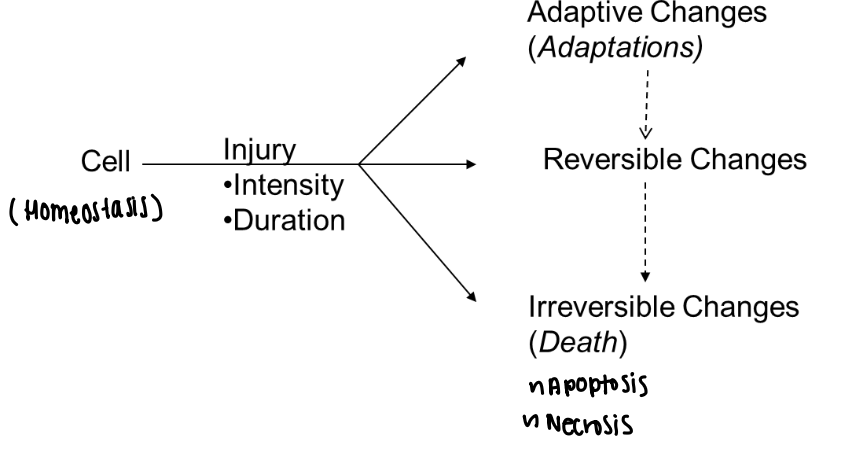
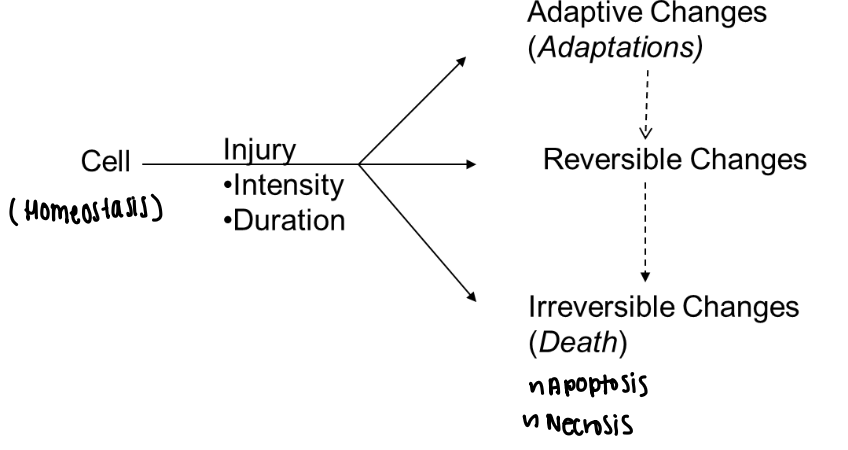
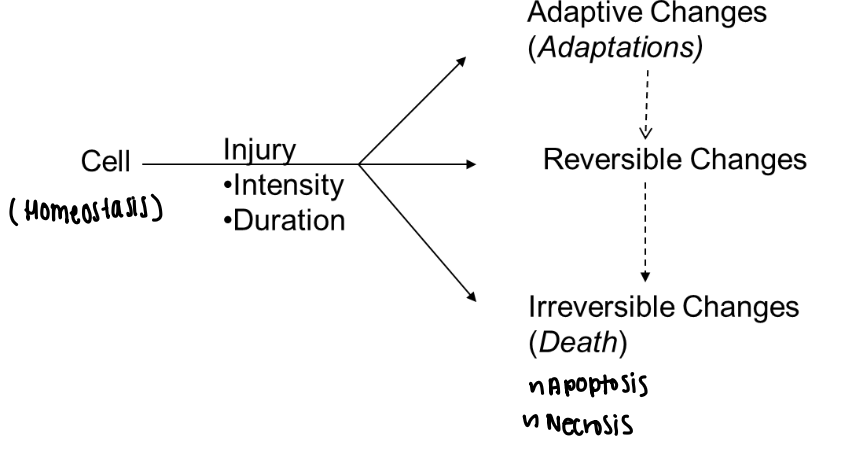
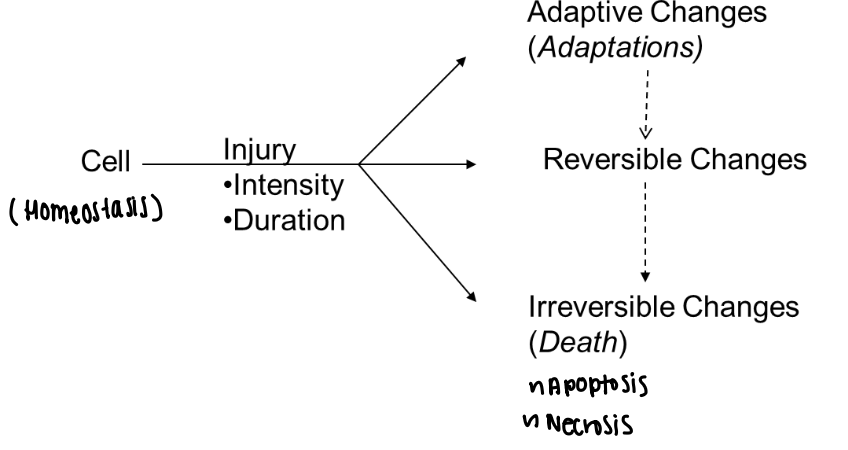
Cell injury
Damage to a cell caused by internal or external factors that disrupt homeostasis
External injurious agents
Factors outside the body that cause cell injury
Exogenous toxins
Toxic substances originating outside the body
Heavy metals
Exogenous toxins such as lead and mercury
Caustic agents
Exogenous chemicals such as acids and bases that cause tissue damage
Plant toxins
Natural toxins from plants such as poison ivy (exogenous toxins)
Animal toxins
Toxins from animals such as venom from a snake bite (exogenous toxins)
Infectious agents
Pathogens that injure cells including bacteria, viruses, parasites, and fungi (exogenous toxins)
Radiation
External energy exposure that damages cellular DNA and proteins (exogenous toxins)
Physical trauma
Mechanical forces that cause tissue and cell injury
Pressure injury
Tissue damage caused by prolonged pressure such as sitting or lying down for a long time (Physical trauma)
Mechanical injury
Injury from strong physical force such as a blow or car accident (Physical trauma)
Thermal injury
Injury caused by extreme temperatures (Physical trauma)
Burns
Thermal injury caused by excessive heat (Physical trauma)
Frostbite
Thermal injury caused by extreme cold (Physical trauma)
Internal injurious agents
Factors within the body that cause cell injury
Ischemia
Decreased blood flow resulting in reduced oxygen and nutrient delivery (Internal injurious agents)
Hypoxia
Reduced oxygen availability to cells (Internal injurious agents)
Endogenous toxins
Toxic substances produced within the body (Internal injurious agents)
Free radicals
Reactive molecules that damage cellular components (Internal injurious agents)
Genetic factors
Mutations or abnormalities affecting cell structure or function (Internal injurious agents)
Immunologic factors
Autoimmune reactions that damage cells (Internal injurious agents)
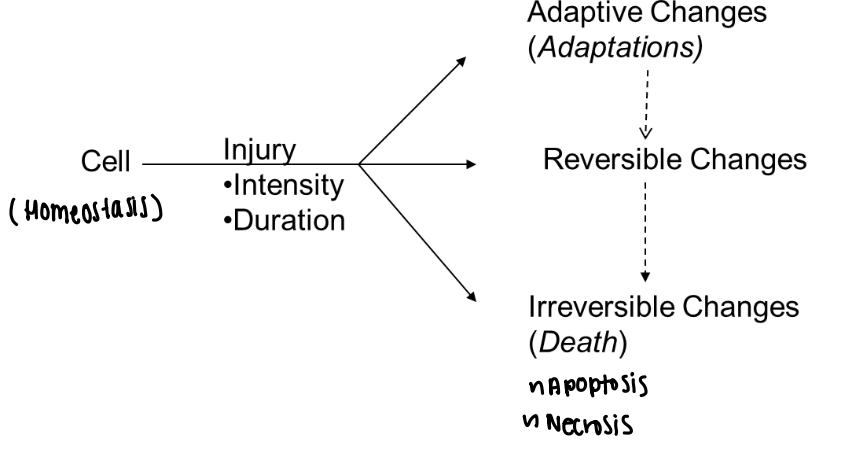
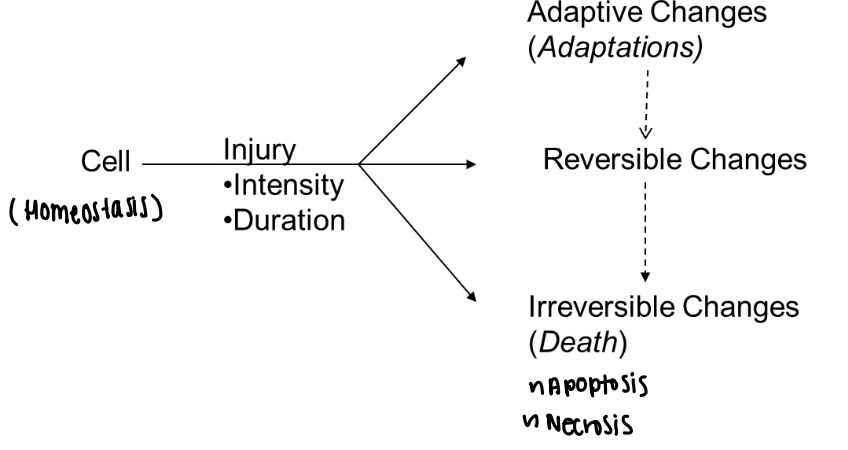
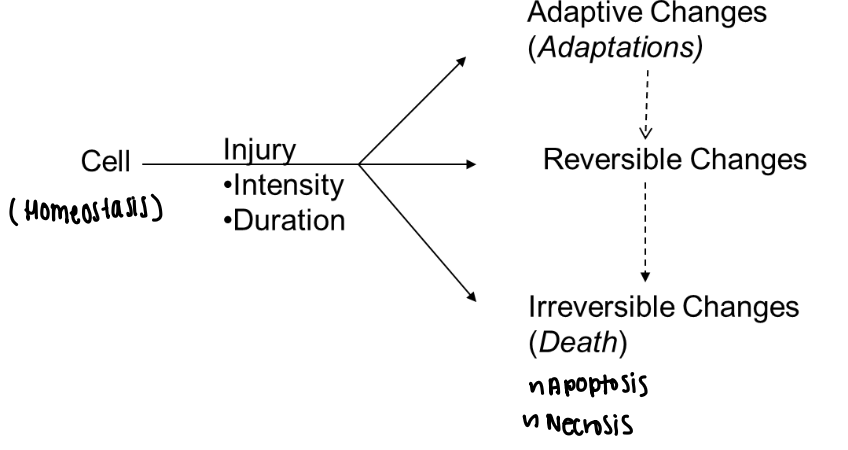
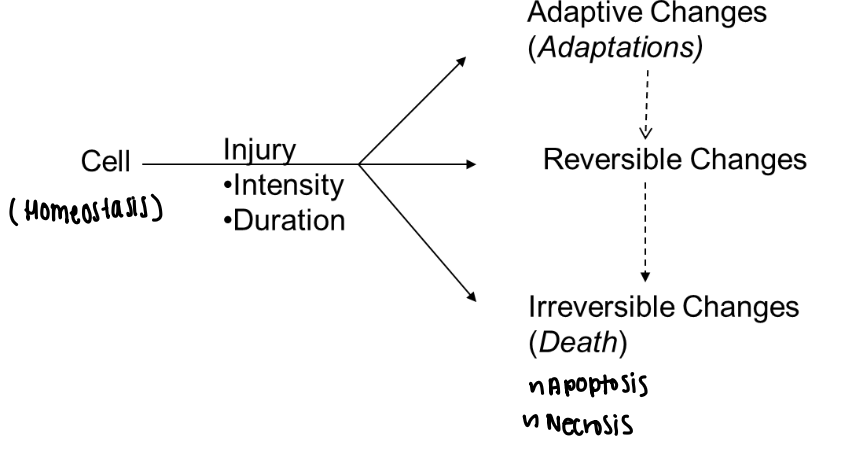
Cellular adaptations
Structural or functional changes that allow cells to survive injury
Hyperplasia
Increase in the number of cells due to abnormal stimulation
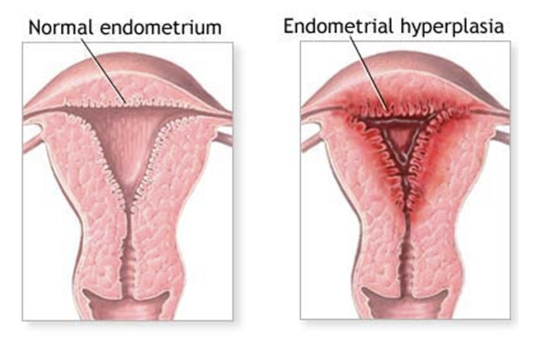
Hyperplasia example
Endometrial proliferation due to prolonged estrogen exposure
Hypertrophy
Increase in cell size due to increased functional demand
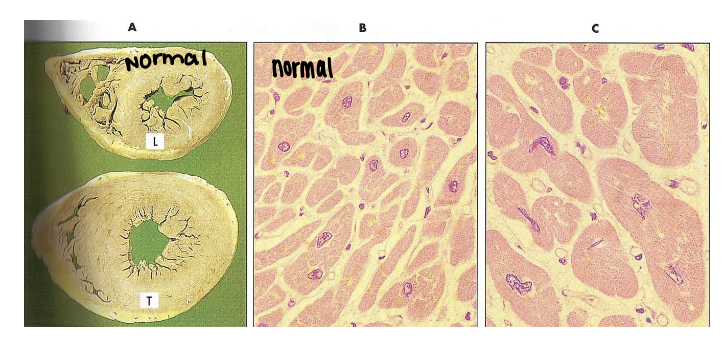
Hypertrophy example
Enlargement of the heart due to aortic stenosis
Atrophy
Decrease in cell size due to reduced blood supply, disuse, or denervation
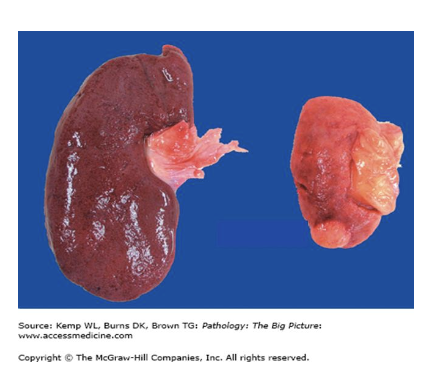
Atrophy example
Kidney atrophy due to renal artery atherosclerosis
Metaplasia
Reversible change from one differentiated cell type to another
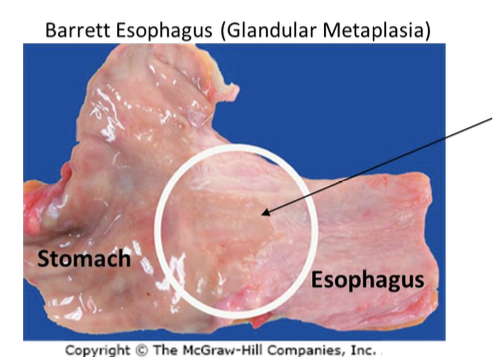
Metaplasia example
Replacement of esophageal squamous epithelium with glandular epithelium in acid reflux
Dysplasia
Disordered cellular growth with abnormal size, shape, and organization
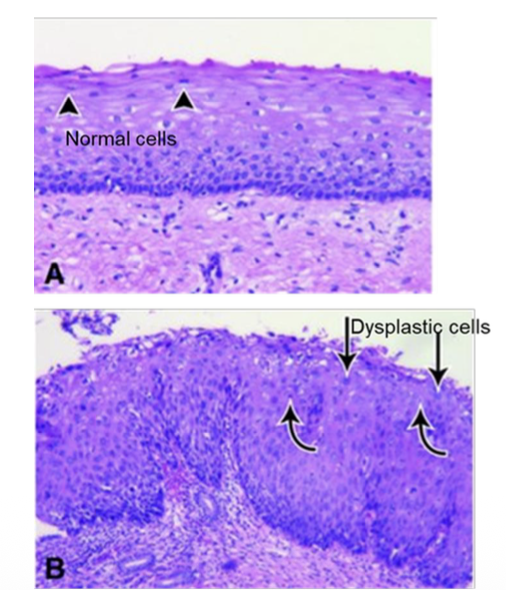
Dysplasia significance
Considered a precursor to cancer
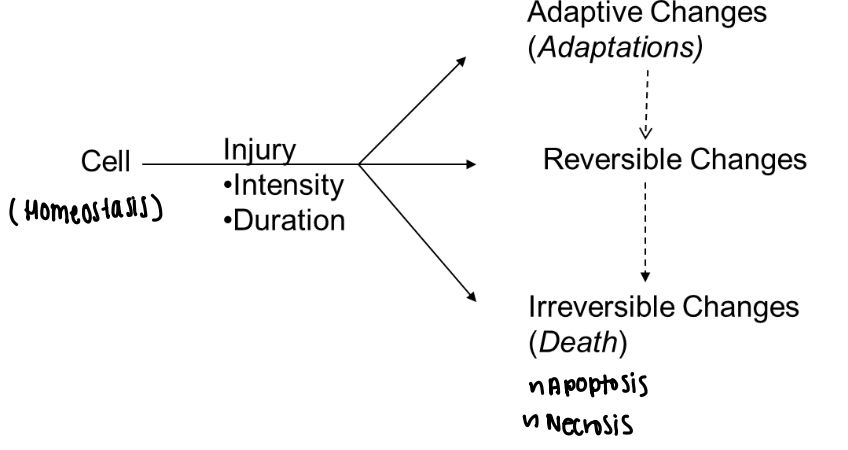
Reversible cell injury
Early cellular damage that can be reversed if the stressor is removed
This can occur through hydropic sweeling
Hydropic swelling (Reversible cell injury)
Accumulation of water in the cell due to failure of ion pumps
Organelle swelling (Reversible cell injury)
Swelling of mitochondria and endoplasmic reticulum during reversible injury
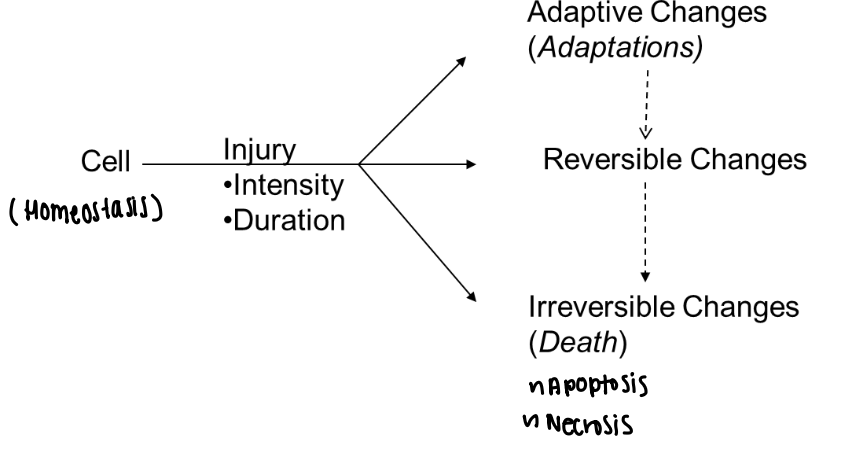
Irreversible cell injury
Damage beyond recovery that leads to cell death
• The exact ‘point of no return’ is not defined; however, irreversible injury is characterized by:
– Severe swelling or rupture of cell
– Breakdown of organelles
– Nuclear changes
– Can lead to necrosis: one type of cell death in the living body
Irreversible injury features
• The exact ‘point of no return’ is not defined; however, irreversible injury is characterized by:
– Severe swelling or rupture of cell
– Breakdown of organelles
– Nuclear changes
– Can lead to necrosis: one type of cell death in the living body
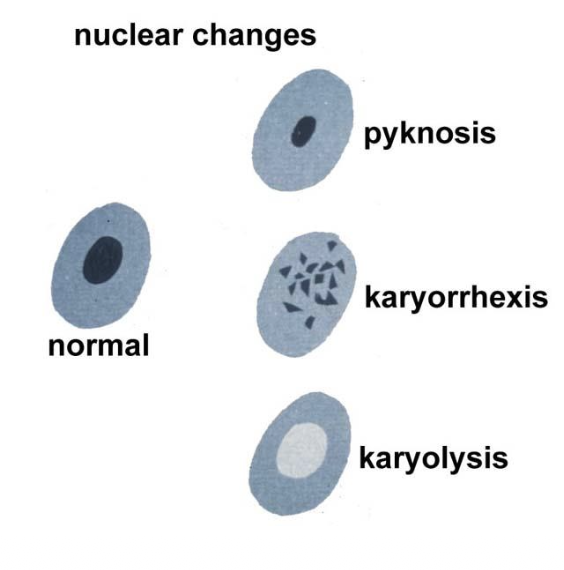
Pyknosis (Irreversible injury)
Nuclear shrinkage and chromatin condensation
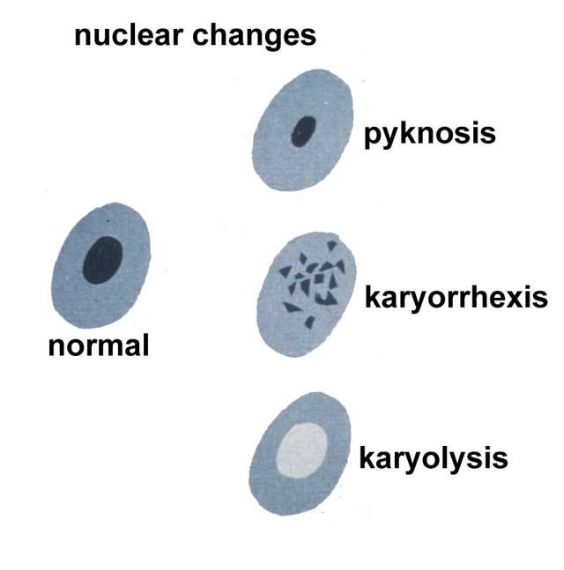
Karyorrhexis (Irreversible injury)
Nuclear fragmentation
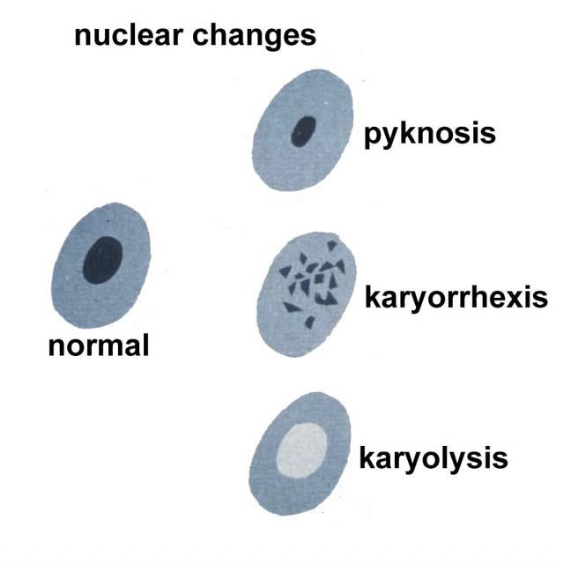
Karyolysis (Irreversible injury)
Loss of the nucleus
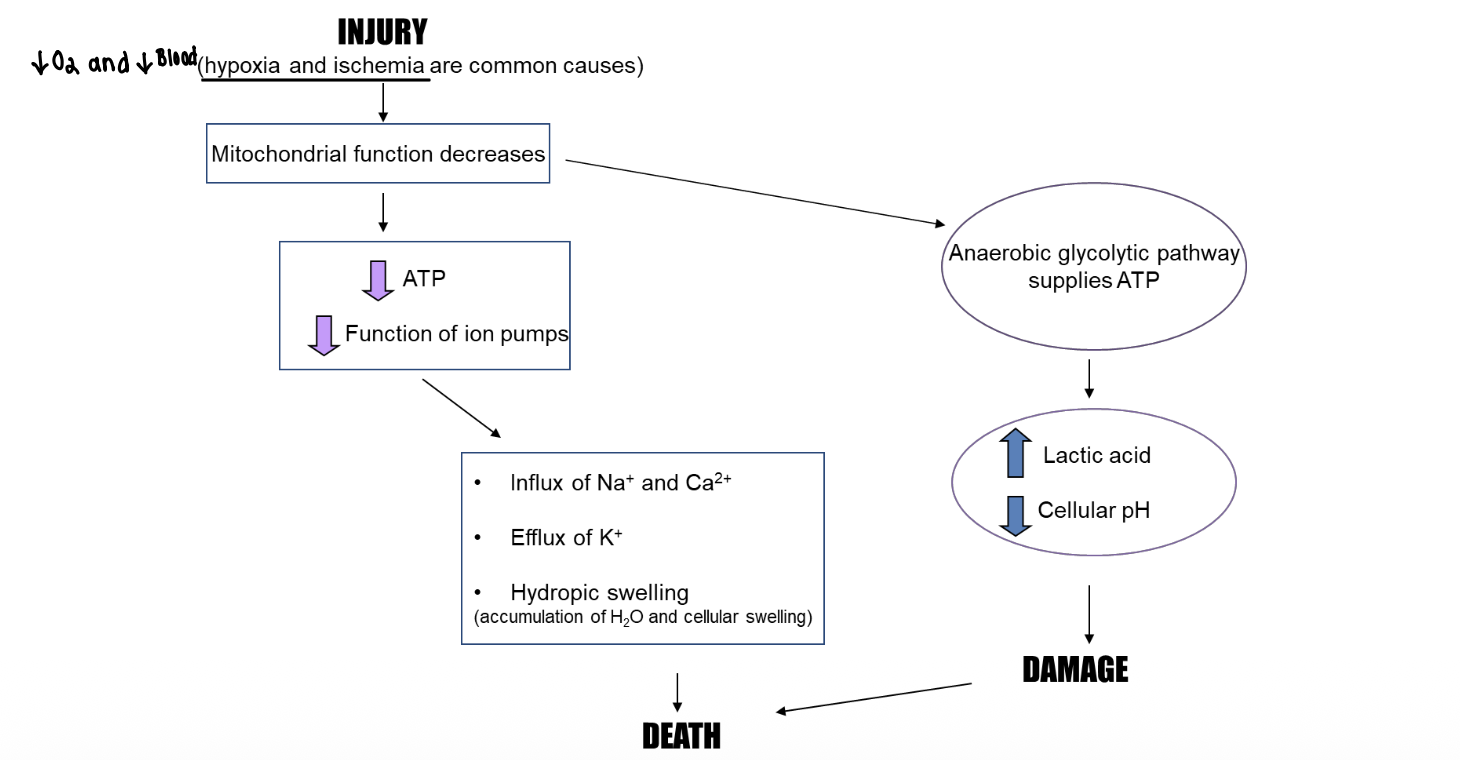
Ischemic cell injury mechanism (Necrosis)
Decreased oxygen leads to decreased ATP production
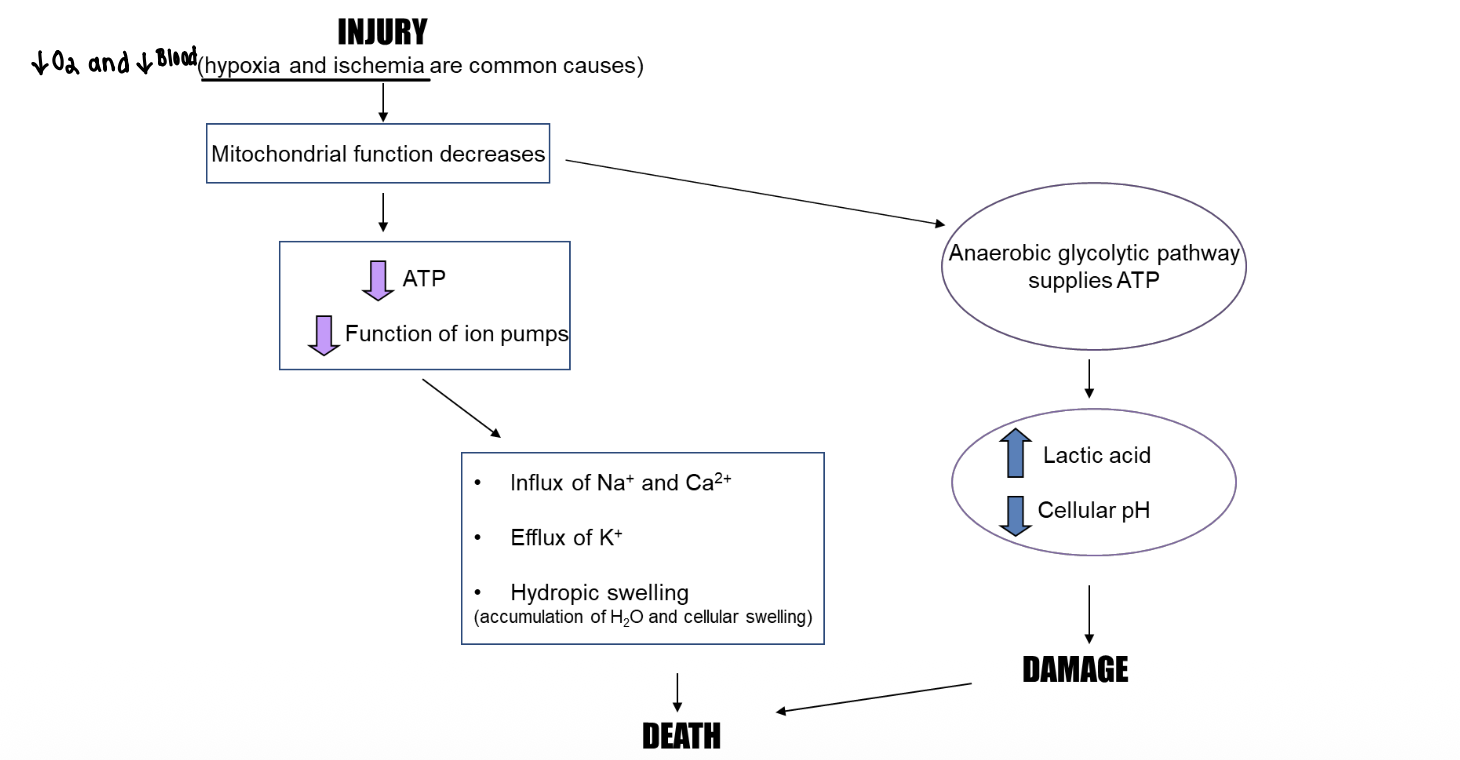
ATP depletion effect (Necrosis)
Failure of Na⁺/K⁺ and Ca²⁺ pumps (causing Influx of Na and Ca/efflux of K)
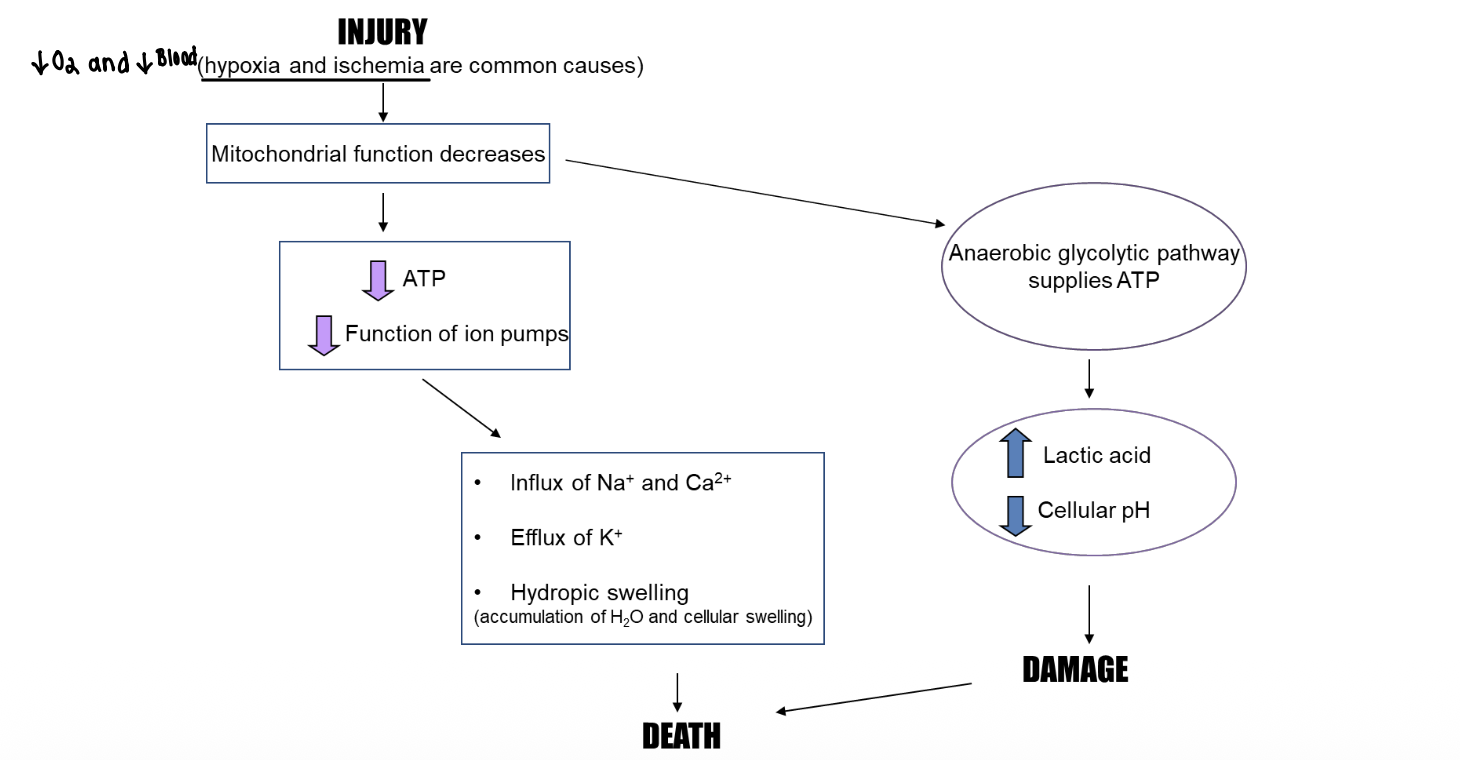
Ion imbalance (Necrosis)
Influx of Na⁺ and Ca²⁺ and efflux of K⁺
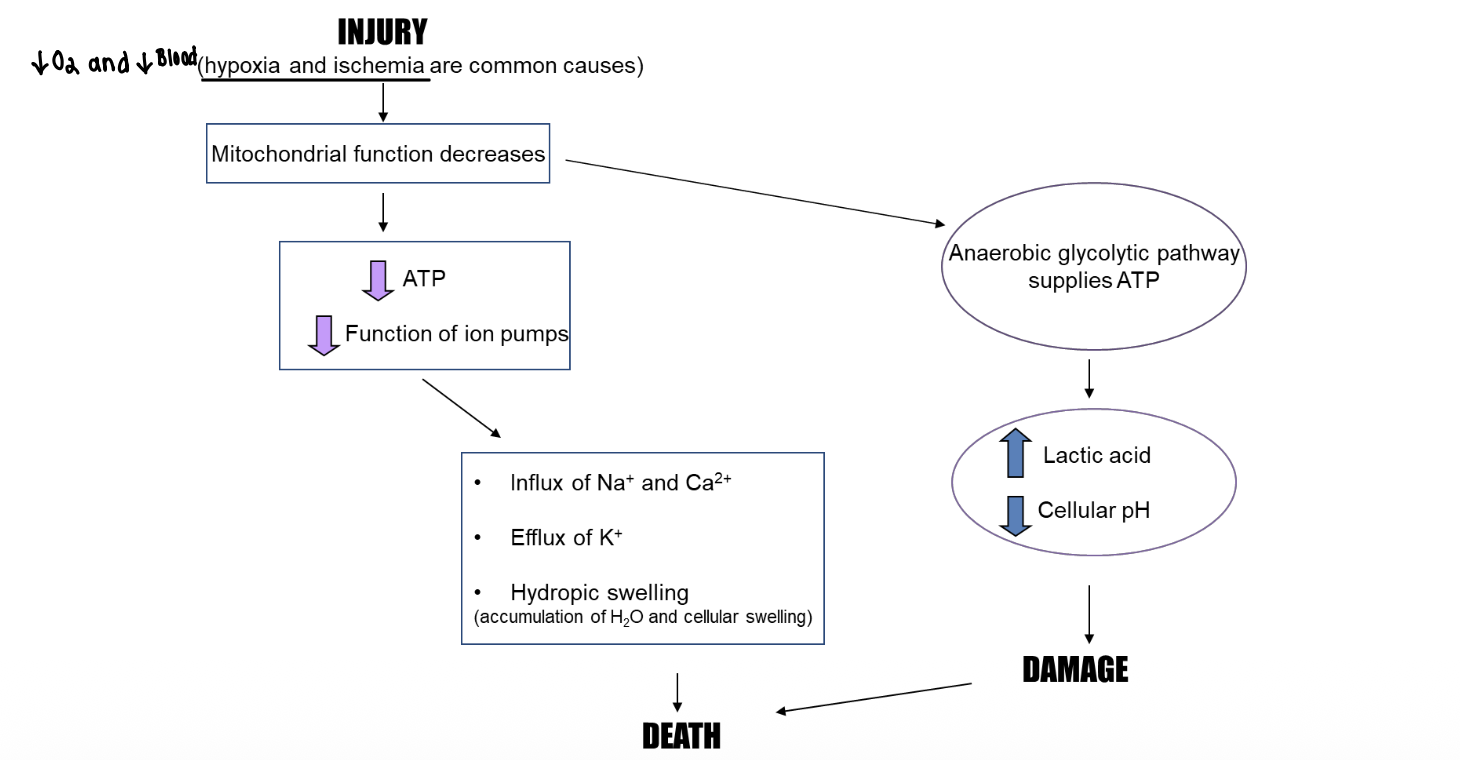
Cell swelling mechanism (Necrosis)
Water follows sodium into the cell causing hydropic swelling
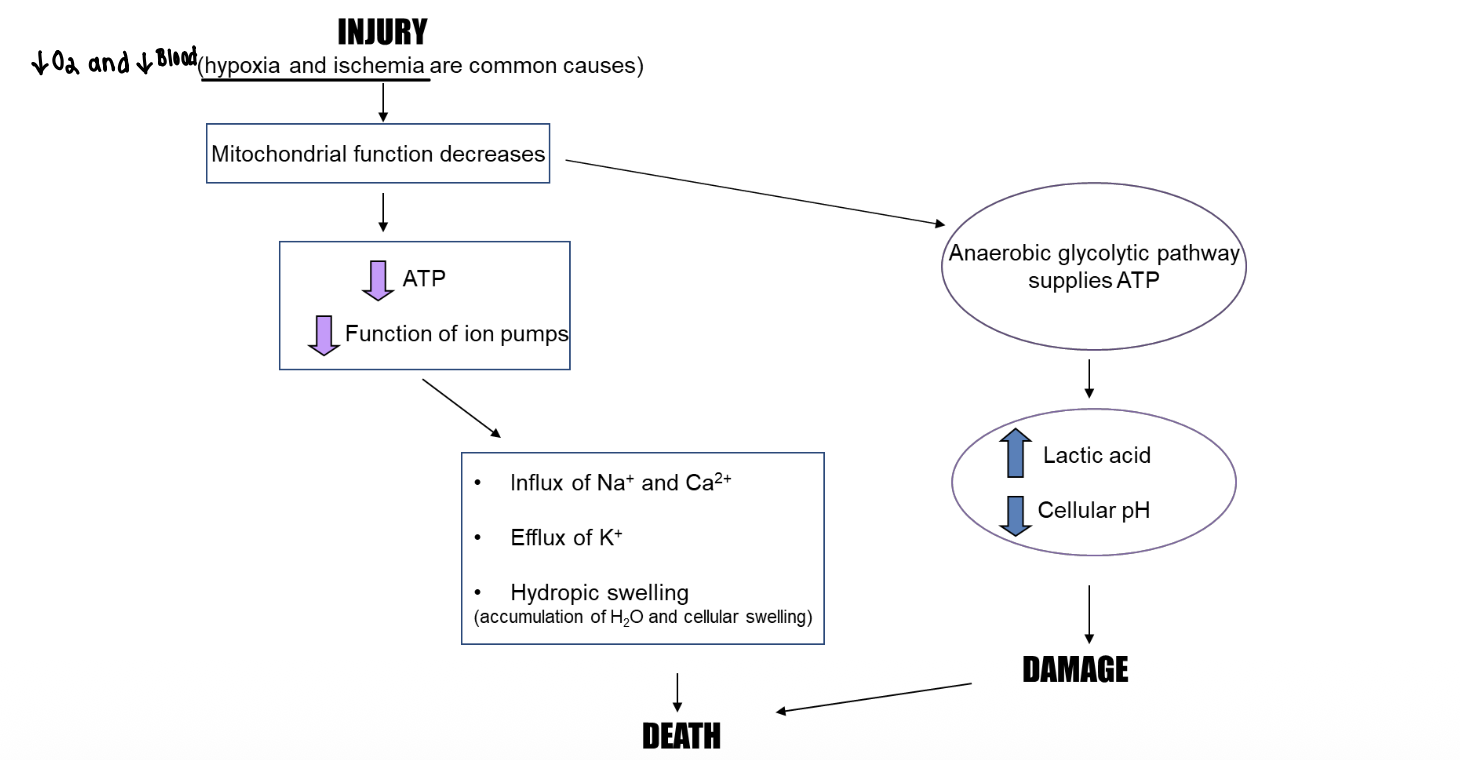
Anaerobic metabolism consequence (Necrosis)
Lactic acid accumulation and decreased cellular pH
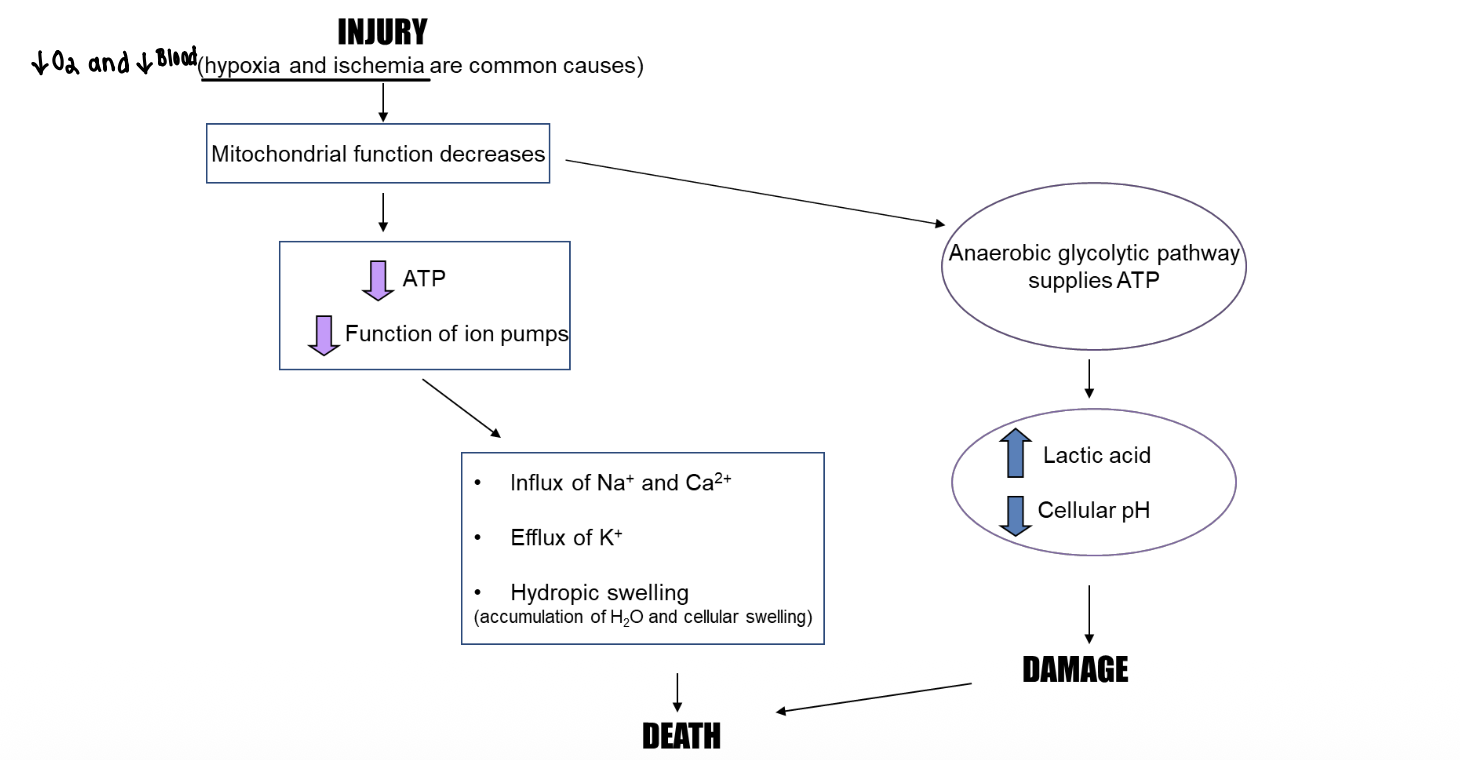
Final outcome of ischemic injury (Necrosis)
Organelle damage leading to necrosis
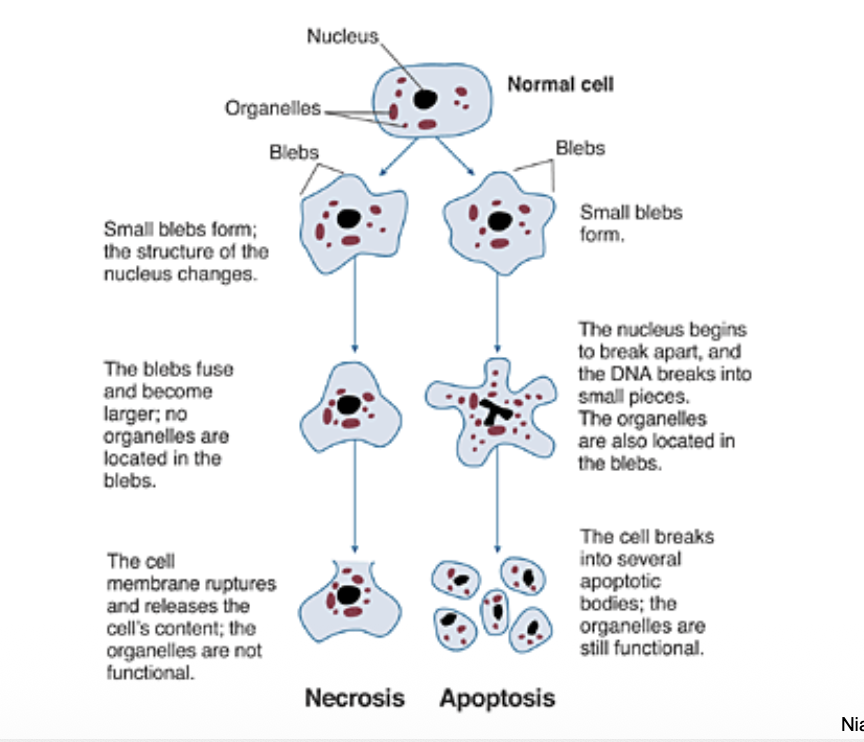
Necrosis (Irreversible injury)
Uncontrolled cell death caused by severe injury
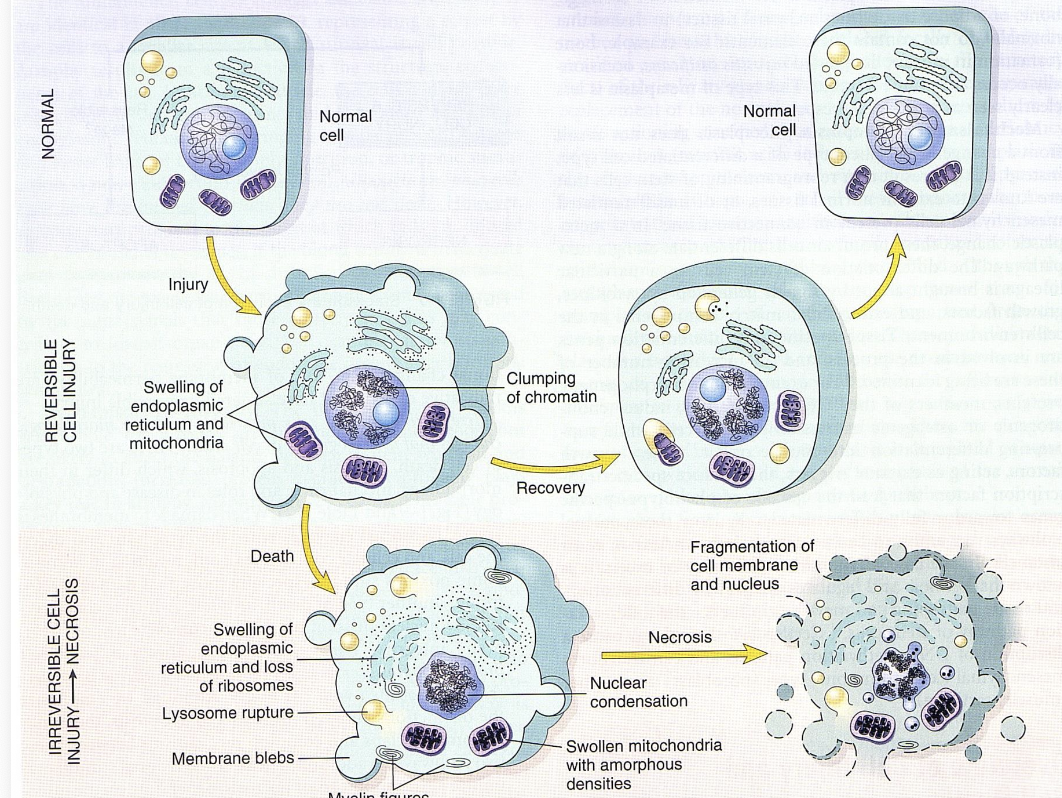
Necrosis characteristics
• Damage to cell causes rupture of cell membrane
• Intracellular contents are expelled into the extracellular space
• This triggers inflammation
• Necrosis usually involves large numbers of cells
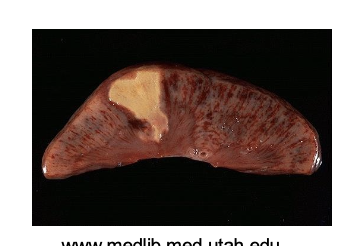
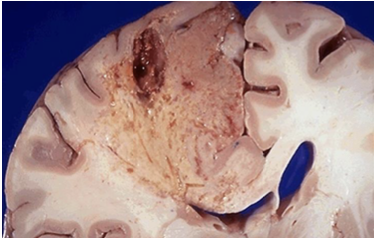
Coagulative necrosis (Form of Necrosis)
Protein denaturation with preserved tissue architecture
Caused by: local ischemia, mild burns produced by heat, electricity
Coagulative necrosis causes (Form of Necrosis)
Local ischemia or mild burns
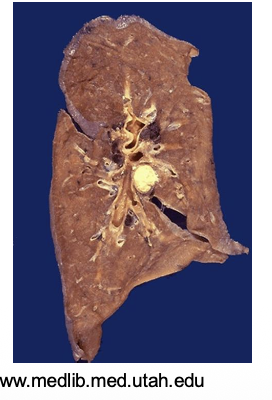
Caseous necrosis (Form of Necrosis)
Cheese-like mixture of proteins and lipids
Caused by: tuberculosis, syphilis, certain fungi
Caseous necrosis causes (Form of Necrosis)
Tuberculosis, syphilis, certain fungal infections
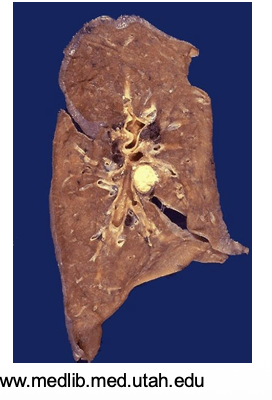
Gangrene necrosis (Form of Necrosis)
Tissue death due to loss of blood supply (two types: wet and dry)
Wet gangrene (Form of Necrosis)
Gangrene with bacterial infection

Dry gangrene (Form of Necrosis)
Gangrene with little or no infection
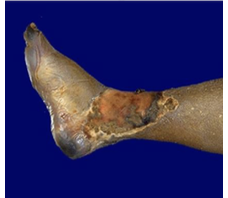
Liquefactive necrosis (Form of Necrosis)
Rapid dissolution of dead cells into liquid
– Cells dissolve, leaving a fluid filled cavity
– Caused by: bacterial, sometimes fungal infections; in the brain, cerebral artery occlusion can cause it
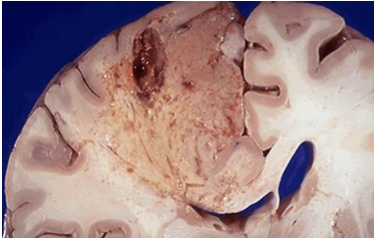
Liquefactive necrosis causes (Form of Necrosis)
Bacterial infections or cerebral artery occlusion in the brain
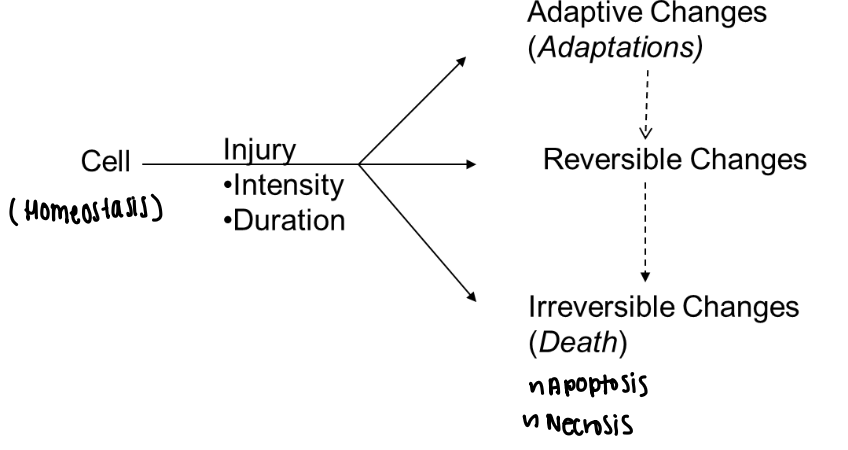
Apoptosis
Programmed and regulated cell death
It is a highly ordered process that minimizes potentially damaging responses of the host
– With apoptosis, inflammation is not initiated
• Induced by:
– Normal physiology, for example, maintenance of organs
– DNA damage, misfolded proteins, among other factors
Apoptosis inflammation
Does not trigger inflammation
Apoptosis triggers
DNA damage, misfolded proteins, normal tissue maintenance
During this Apoptosis process:
• Caspases are activated; they are a special group of enzymes that carry out the cell’s death
• Changes in cell morphology:
– Shrinkage of the cytoplasm
– Condensation and cleavage of nucleus (these nuclear changes are similar to necrosis)
• Formation of apoptotic bodies
– Membrane-bound bodies that contain organelles (organelles may still be functional)
– Phagocytized
• One or a few cells undergo apoptosis, not large groups of cells
Necrosis vs apoptosis
Necrosis is uncontrolled and inflammatory; apoptosis is controlled and noninflammatory
Etiology
The cause or origin of a disease
Categories:
Acquired
Idiopathic
Congenital
Genetic (chromosomal or monogenic/mendalin)
Multifactorial
Genetic etiology
Disease caused by mutations in DNA
Mutations or variations in DNA
• Chromosomal: abnormalities in chromosomes (e.g., structural or numeric)
• Monogenic/Mendelian
– Autosomal dominant
– Autosomal recessive
– X-linked
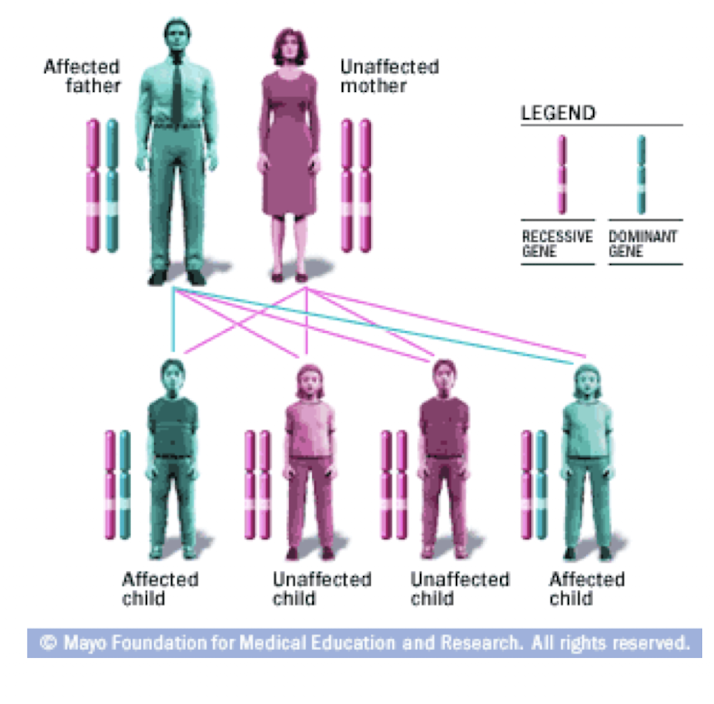
Single Gene, Autosomal Dominant Disorder
General characteristics:
• Single gene variation (mutation) in an autosome
– Males and females are equally affected
• An individual who inherits one copy of the gene variation will have the disease
• Usually successive generations are affected, the disease does not occur in the offspring of unaffected individuals
Example: Huntington’s Disease
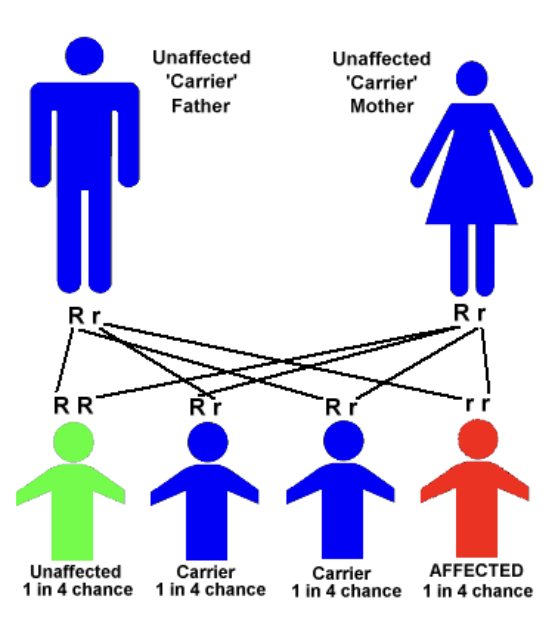
Single Gene, Autosomal Recessive Disorder
General characteristics
• Single gene variation (mutation) in an autosome
– Males and females are equally affected
• An individual who inherits two copies of the gene variation will have the disease
• Carriers have one copy of the gene variation and can pass the gene variation to offspring
– Carriers are usually clinically healthy
• Seems to skip generations
Example: Sickle Cell Anemia
Single Gene, X-linked Disorder
General characteristics
• Single gene variation (mutation) in an X chromosome
– A male who inherits the gene variation will have the disease
– Males are affected more than females
– No father-to-son transmission of the gene variation
• Daughters of an affected male are carriers of the gene variation and can pass it to offspring
– Daughter could be an asymptomatic carrier, or daughter could have variable symptoms of the disease
• Seems to skip generations
Example: Hemophilia
Multifactorial etiology (Disease)
Genetic background, environmental factors, lifestyle contribute to the
pathogenesis of the disease
Pharmacology
The study of drugs and their interactions with living systems through chemical processes
Pharmacotherapy
– Drugs to treat disease or injury
• In general, drugs may replace, mimic or block the action of an endogenous substance or process
Therapeutic intervention
Any method used to treat or manage disease (ex: Surgery, Radiation, Genetic, Immunological)