Ch 5: Pancreas
1/99
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
100 Terms
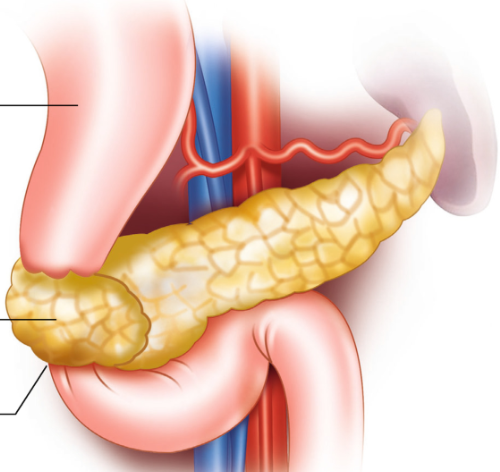
How does the pancreas develop embryologically, and what is its adult location and peritoneal status?
It develops from two embryologic buds that fuse, forming a comma-shaped organ. It is located in the epigastrium between the C-loop of the duodenum and the splenic hilum and is a retroperitoneal organ (though part of the head may be peritoneal-covered).
What are the main anatomic parts of the pancreas, including the uncinate process?
The pancreas consists of the head, neck, body, and tail. The uncinate process is a posteromedial extension of the pancreatic head present in some individuals.
Why is the pancreas considered both an exocrine and endocrine gland?
It is exocrine because it secretes digestive enzymes via ducts into the duodenum, and endocrine because it releases hormones directly into the bloodstream via the islets of Langerhans.
What digestive enzymes and substances are produced by the exocrine pancreas, and what are their functions?
Amylase: digests carbohydrates (starch → sugar)
Lipase: digests fats (→ fatty acids & glycerol)
Trypsin, chymotrypsin, carboxypolypeptidase: digest proteins
Sodium bicarbonate: neutralizes gastric acid
Which pancreatic cells perform the exocrine function?
Acinar cells, which produce digestive enzymes and sodium bicarbonate.
Describe the pancreatic ductal anatomy and key named structures.
Digestive enzymes drain into the main pancreatic duct (duct of Wirsung), which runs the length of the pancreas before draining into the duodenum at the major duodenal papilla.
An accessory duct (duct of Santorini) may branch from it and drain separately into the duodenum via the minor duodenal papilla.
Where do pancreatic enzymes mix with bile, and how do they enter the duodenum?
They mix at the ampulla of Vater (hepatopancreatic ampulla) and enter the duodenum through the sphincter of Oddi, which sits on the major duodenal papilla.
What hormone triggers gallbladder contraction and sphincter of Oddi relaxation, and why is this important?
Cholecystokinin (CCK), released by the duodenum in response to chyme, causes gallbladder contraction and relaxation of the sphincter of Oddi, allowing bile and pancreatic enzymes to enter the duodenum simultaneously.
What structures perform the endocrine function of the pancreas?
The islets of Langerhans, which are clusters of endocrine cells scattered throughout the pancreas.
Match islet cell types with their hormones and functions.
Alpha cells → Glucagon (raises blood glucose by promoting hepatic glucose release)
Beta cells → Insulin (lowers blood glucose by promoting glucose utilization)
Delta cells → Somatostatin (inhibits insulin and glucagon secretion)
What is the arterial blood supply to the pancreas by region?
Head: gastroduodenal artery
Body & tail: splenic artery and superior mesenteric artery
How is venous drainage of the pancreas accomplished?
Via the splenic vein, superior mesenteric vein, inferior mesenteric vein, and portal vein.
What are the main technical challenges of pancreatic sonography, and how can visualization be improved?
Challenges include bowel gas and body habitus. Visualization may be improved by:
Having the patient drink water to fill the stomach and duodenal C-loop (improves head visualization)
Left lateral decubitus for the pancreatic head
Right lateral decubitus scanning through the left kidney and spleen for the tail
Upright scanning
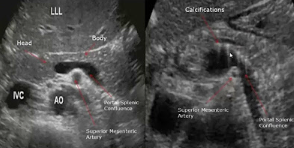
How is the pancreas identified sonographically using surrounding vasculature?
Head: right lateral to SMV, anterior to IVC, inferior to portal vein
Uncinate process: posterior to SMV (may surround it) and anterior to the aorta
Neck: anterior to the portal confluence
Body: anterior to the SMV, splenic vein, and SMA
Tail: splenic vein marks the posterior border
What are the key sonographic landmarks in the pancreatic head on transverse imaging?
Two round anechoic structures may be seen:
Anterior: gastroduodenal artery
Posterior: common bile duct
Describe the normal echogenicity of the pancreas across age groups.
Adults: echogenicity of the pancreas is greater than the liver and equal to or greater than the spleen
Pediatrics: pancreas appears more hypoechoic due to less surrounding fat
Diffuse peculiarly hyperechoic pancreas in adults may indicate pancreatic steatosis
What is the normal appearance and size of the main pancreatic duct?
If visualized, it appears as two parallel echogenic lines with an anechoic lumen.
Normal AP diameter ≤ 2 mm.
What are the normal sonographic size measurements of the pancreas?
Measured in the AP dimension:
Head & body: 2–3 cm
Tail: 1–2 cm
What are the two most common congenital anomalies of the pancreas?
Pancreatic divisum and annular pancreas
What embryologic abnormality causes pancreatic divisum, and how does it alter ductal drainage? Why does this anomaly increase the risk of pancreatitis?
Pancreatic divisum results from failure of fusion of the pancreatic ducts, leading to a shortened main pancreatic duct that drains only the pancreatic head, forcing the duct of Santorini to drain the majority of the pancreas through the much smaller accessory papilla.
Increased pancreatitis risk is because the accessory duct (Santorini) is smaller and must drain a larger-than-normal volume of pancreatic enzymes, creating a functional obstruction that predisposes patients to acute and chronic pancreatitis, even though many are asymptomatic.
What is an annular pancreas, and what is its primary clinical consequence?
An annular pancreas results from abnormal development of the ventral pancreatic bud, causing pancreatic tissue to encircle the duodenum, which may lead to duodenal obstruction.
Describe the defining features of the following main distinctive subtypes of pancreatitis:
Gallstone pancreatitis
Hemmorrhagic pancreatitis
Autoimmune pancreatitis
Groove pancreatitis
Necrotizing pancreatitis
Interstitial edematous pancreatitis
Gallstone pancreatitis: pancreatitis caused by gallstones with obstruction of the pancreatic duct
Hemorrhagic pancreatitis: bleeding within or around the pancreas; high morbidity and mortality
Autoimmune pancreatitis: chronic pancreatitis due to immune-mediated pancreatic injury
Groove pancreatitis: chronic pancreatitis localized to the pancreatic head with inflammation of the CBD and second portion of the duodenum
Necrotizing pancreatitis: acute pancreatitis with pancreatic parenchymal and peripancreatic tissue necrosis; high morbidity and mortality
Interstitial edematous pancreatitis: most common form of acute pancreatitis; inflammatory edema without necrosis
What is acute pancreatitis and what are its two major subtypes?
Acute pancreatitis is inflammation caused by leakage of pancreatic enzymes from acinar cells into the pancreatic parenchyma and surrounding tissues.
Subtypes:
Interstitial edematous pancreatitis (more common, better prognosis)
Necrotizing pancreatitis (less common, higher mortality)
What are the two most common causes of acute pancreatitis?
Alcohol abuse and biliary tract disease (especially choledocholithiasis)
Which laboratory findings are most characteristic of acute pancreatitis?
Elevated amylase (within 24 hours)
Elevated lipase (within 72 hours; more specific)
Leukocytosis
Hyperglycemia
Elevated ALT and other LFTs when gallstone pancreatitis is present
Severe disease may show decreased hematocrit due to hemorrhage
What clinical features are typical of acute pancreatitis?
Abdominal pain (worse supine, relieved by sitting or leaning forward)
Back pain
Fever
Nausea and vomiting
Severe cases may progress to shock, ileus, hemorrhage
Why can sonography be limited in diagnosing acute pancreatitis?
Because mild acute pancreatitis may show a normal-appearing pancreas, although ultrasound is valuable for evaluating gland size, echogenicity, biliary obstruction, and complications.
What are the key sonographic appearances of acute pancreatitis?
Normal pancreas (mild disease)
Diffuse enlargement with hypoechoic echotexture (diffuse pancreatitis)
Focal hypoechoic enlargement, often in the head (may mimic neoplasm)
Ill-defined pancreatic margins
Unencapsulated peripancreatic fluid collections (phlegmon)
What is a pancreatic pseudocyst and when does it form?
A pseudocyst is an encapsulated fluid collection formed as the body attempts to contain leaked pancreatic enzymes in moderate to severe pancreatitis.
Common location: lesser sac between the pancreas and stomach
Appearance: anechoic mass with posterior enhancement, may contain internal echoes
Identify two vascular complications can result from acute pancreatitis.
Splenic vein thrombosis
Splenic artery pseudoaneurysm
How do focal and diffuse acute pancreatitis differ sonographically?
Focal pancreatitis: localized hypoechoic enlargement (often pancreatic head), may mimic tumor
Diffuse pancreatitis: global pancreatic enlargement with diffuse hypoechogenicity and surrounding fluid
What is chronic pancreatitis and how does it develop?
Chronic pancreatitis results from repeated or prolonged pancreatic inflammation, leading to irreversible destruction of pancreatic tissue with atrophy, fibrosis, and calcification. Not all patients with acute pancreatitis progress to chronic disease.
What are the most common causes of chronic pancreatitis?
Chronic alcohol abuse (most common)
Hyperparathyroidism
Congenital anomalies (e.g., pancreatic divisum)
Genetic disorders
Pancreatic duct obstruction
Trauma
What structural changes occur in chronic pancreatitis?
Pancreatic atrophy
Fibrosis
Parenchymal and/or ductal calcifications
Pancreatic duct dilation
Possible biliary obstruction
What are the typical clinical findings of chronic pancreatitis?
Patients may be asymptomatic or present with:
Persistent epigastric pain and back pain
Jaundice
Weight loss and anorexia
Nausea, vomiting, constipation
Possible elevation in ALP, amylase, and lipase (note that these enzymes may also be normal)
How do laboratory findings in chronic pancreatitis differ from acute pancreatitis?
In chronic pancreatitis, amylase and lipase may be normal or only mildly elevated, unlike acute pancreatitis where they are typically significantly elevated.
What are the key sonographic findings of chronic pancreatitis?
Small, atrophic pancreas
Heterogeneous or hyperechoic echotexture
Poorly defined margins
Calcifications within the parenchyma and/or ducts
Dilated pancreatic duct
Pancreatic duct stones
Possible biliary dilation
Possible pseudocyst
Possible portosplenic vein thrombosis
Name 4 complications that are commonly associated with chronic pancreatitis.
Pancreatic pseudocyst formation (up to 40%)
Pancreatic duct obstruction
Biliary obstruction
Portosplenic vein thrombosis
How can chronic pancreatitis be differentiated sonographically from acute pancreatitis?
Chronic: small, hyperechoic, calcified, poorly marginated pancreas
Acute: enlarged, hypoechoic pancreas with peripancreatic fluid
What is the most common primary pancreatic malignancy and in whom is it most often found?
Pancreatic adenocarcinoma (pancreatic ductal carcinoma); most commonly found in men.
What are the major risk factors for pancreatic adenocarcinoma?
Cigarette smoking, diabetes mellitus, chronic pancreatitis, high-fat diet, and genetic predisposition.
Where is pancreatic adenocarcinoma most commonly located?
The head of the pancreas.
Why do pancreatic head masses commonly cause jaundice?
They obstruct the common bile duct, leading to biliary obstruction and jaundice.
What is Courvoisier gallbladder and what does it suggest?
A palpable, enlarged gallbladder caused by obstruction from a (potentially malignant) pancreatic head mass.
What is the “double duct sign” and what does it indicate?
Simultaneous dilation of the common bile duct and pancreatic duct, commonly seen with pancreatic adenocarcinoma.
What are the classic clinical findings of pancreatic adenocarcinoma?
Jaundice
Weight loss
Loss of appetite
Epigastric or back pain
Elevated amylase/lipase
Elevated ALP and liver enzymes
Courvoisier gallbladder
History of smoking, diabetes, or chronic pancreatitis
What is the most common sonographic appearance of pancreatic adenocarcinoma?
A hypoechoic mass in the head of the pancreas with ductal dilation.
Why must the liver be carefully evaluated when pancreatic adenocarcinoma is detected?
Because stage 3 disease includes distant metastasis, commonly to the liver.
What surgical procedure is performed for pancreatic adenocarcinoma and what is removed?
The Whipple procedure (pancreaticoduodenectomy):
Head of the pancreas
Gallbladder
Portions of the bile ducts
Proximal duodenum
What are the two types of pancreatic cystadenomas and how do they differ?
Serous (microcystic): small, always benign
Mucinous (macrocystic): larger, malignant potential
When a mucinous cystadenoma becomes malignant, what is it called?
Mucinous cystadenocarcinoma.
Where are mucinous cystic tumors most commonly located?
The body and tail of the pancreas.
How does pancreatic adenocarcinoma location differ from cystadenocarcinoma?
Adenocarcinoma: head of pancreas
Cystadenocarcinoma: body or tail
What is the typical sonographic appearance of a serous cystadenoma?
A small cystic mass that may appear solid and echogenic due to the cyst’s very small size.
What sonographic features suggest a mucinous cystadenoma or cystadenocarcinoma over a serous cystadenoma?
Multilocular cystic mass
Mural nodules
Calcifications
Possible pancreatic duct dilation
Where do islet cell tumors arise and what are they also called?
From the islets of Langerhans; also called pancreatic neuroendocrine tumors.
What are the two most common islet cell tumors?
Insulinoma (most common, usually solitary)
Gastrinoma (often multiple)
What clinical syndrome is caused by a functional gastrinoma?
Zollinger–Ellison syndrome — excessive gastric acid secretion causing peptic ulcers.
What is the Whipple triad and which tumor is it associated with?
Associated with insulinoma:
Hypoglycemia
Low fasting glucose
Relief with IV glucose
What are common symptoms of insulinoma?
Hypoglycemia, palpitations, sweating, tremors, headaches, and possible diabetic coma.
What is the most common sonographic appearance of an islet cell tumor?
A small hypoechoic mass, sometimes with calcifications.
How do functioning islet cell tumors appear on color Doppler?
They are often hypervascular.
What conditions are associated with true pancreatic cysts?
Von Hippel–Lindau disease, cystic fibrosis, and autosomal-dominant polycystic kidney disease (ADPKD).
What key entity must be ruled out when a pancreatic cyst is seen?
A pancreatic pseudocyst, especially if there is a history of acute or chronic pancreatitis.
What are the clinical clues suggesting a true pancreatic cyst (over pseudocyst)?
History of von Hippel–Lindau disease, cystic fibrosis, or ADPKD.
What is the most common indication for pancreatic transplantation?
Treatment of severe type 1 diabetes mellitus.
How often is pancreatic transplantation performed with concurrent renal transplantation?
Approximately 80% of the time.
Where are the pancreas and kidney placed when both are transplanted?
Pancreas on the right side, kidney on the left side of the abdomen.
What are the two main types of pancreatic transplant drainage techniques?
Exocrine bladder drainage
Exocrine enteric drainage (more common)
How does exocrine bladder drainage work and what are its drawbacks?
Donor duodenum is anastomosed to the urinary bladder; associated with dehydration and bladder irritation.
How does exocrine enteric drainage work? Explain the Y-graft in this transplant type.
Donor duodenum is anastomosed to a loop of jejunum. a Y-graft is used to connect the donor’s superior mesenteric artery and splenic artery. These arteries are joined via a segment of donor iliac artery, forming a Y configuration. The base of the Y-graft (iliac portion) is then anastomosed to the recipient’s common iliac artery. This approach allows both arterial supplies of the pancreas to be connected via a single arterial anastomosis (minimizing the number of anastomoses in the recipient= reduced operative time and risk).
What are the key components of a pancreatic transplant ultrasound exam?
Evaluation of vascularity, pancreatic parenchyma, and fluid collections.
List types of fluid collections that may be seen after pancreatic transplantation.
Abscess, ascites, hematoma, urinoma, pseudocyst.
What is the expected appearance of the pancreatic parenchyma immediately after transplant?
Homogeneous and may appear hypoechoic.
Why is a hypoechoic pancreatic transplant concerning?
It may indicate pancreatitis or acute rejection, requiring clinical correlation.
What are the sonographic findings of acute pancreatic transplant rejection?
Hypoechoic or heterogeneous gland with elevated resistive indices.
What resistive index finding suggests acute rejection?
Elevated RI, often abnormal compared to baseline.
What are the sonographic findings of chronic pancreatic transplant rejection?
Hypoechoic echotexture, atrophy, and calcifications.
What vascular complications can occur after pancreatic transplantation?
Arterial stenosis, arterial thrombosis, graft thrombosis, pseudoaneurysm, splenic vein thrombosis, and strictures.
What findings suggest splenic vein thrombosis?
Elevated arterial inflow RI (often >1.0) and absent splenic vein flow.
What must be suspected if no flow is detected within the transplanted pancreas?
Graft thrombosis.
When may an ultrasound-guided pancreatic transplant biopsy be performed?
To differentiate rejection from other complications.

A: left lobe liver
B: CBD
C: portal-splenic confluence
D: splenic vein
E: GDA
F: SMA
G: Aorta
H: LRV
I: IVC
J: Stomach
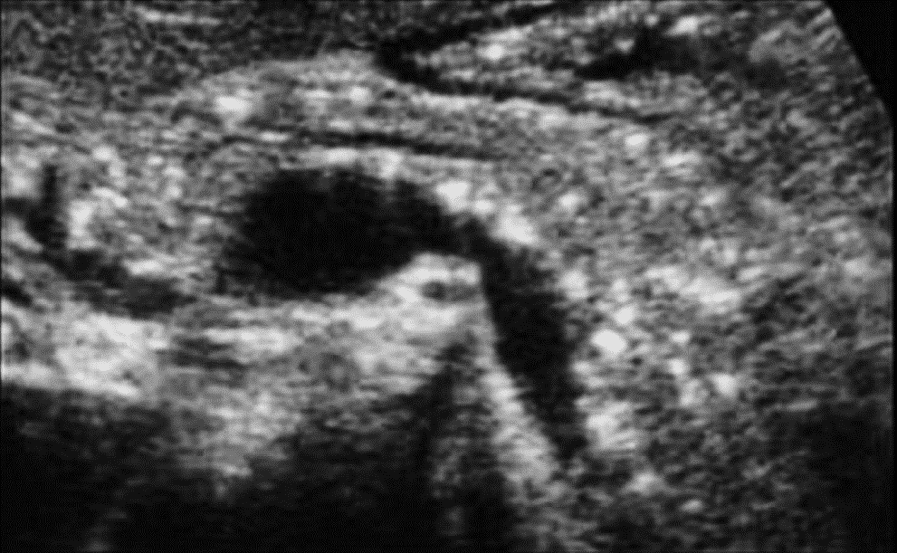
Which congenital anomaly of the pancreas is demonstrated in this image?
Pancreas divisum
Which congenital anomaly of the pancreas is demonstrated in this image?
Annular pancreas
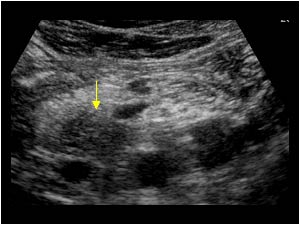
This patient presents with elevated lipase and amylase and leukocytosis. Which form pathology is most likely represented by the arrow in this image?
Focal acute pancreatitis of the pancreatic head
favored over mass due to leukocytosis!!!
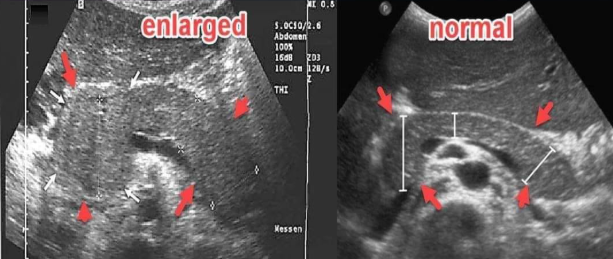
The pathology demonstrated on the left image is most likely:
Diffuse acute pancreatitis
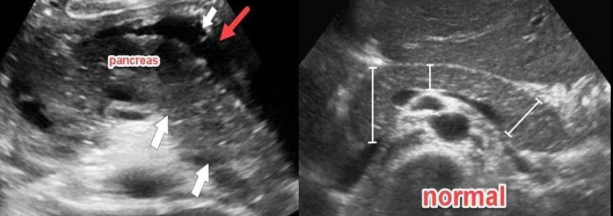
What is the red arrow pointing to? Which pancreatic pathology is this sonographic finding associated with?
Peri-pancreatic fluid, pancreatitis
What pathology is suggested by the findings in the image on the right? (left is normal)
Chronic pancreatitis (calcifications + heterogenous appearance)
A 50-year-old female presented to the hospital with a history of chronic abdominal pain for 6 months.
She is a known alcoholic and had been diagnosed with acute pancreatitis in the past.
Which pancreatic pathology is most likely?
Chronic pancreatitis (The pancreas appears hyperechoic. The pancreatic duct is slightly dilated. Multiple hyperechoic calcifications are seen within the pancreatic tissue.)

Finding commonly associated with pancreatitis
Pancreatic pseudocyst

Male patient presents with extreme weight loss, enlarged palpable gallbladder, and jaundice. What is the most likely pathology indicated by the arrow?
Pancreatic adenocarcinoma (located in the pancreatic head, most common primary pancreatic cancer, more common in men)

This patient presents with hypoglycemia causing palpitations and tremors, and relief of symptoms with IV glucose administration. What is the most likely diagnosis?
Functioning insulinoma

Patient presented with repeated attacks of hypoglycemia. A small well-defined hypoechoic pancreatic nodule with internal vascularity on color doppler was noted. What is the most likely diagnosis?
Functioning insulinoma

45 year old woman with von-Hippel Lindau disease. What is the most likely diagnosis?
True pancreatic cyst
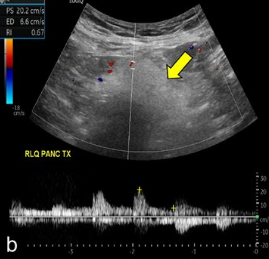
Evaluate the arterial flow of this transplant pancreas.
Arterial Doppler shows a sharp systolic upstroke with continuous diastolic flow and normal RI of 0.7. Findings suggest no complications.
What are the cells of the pancreas that produce amylase and lipase?
Acinar
Beta
Delta
Alpha
Acinar
Which of the following would be most likely to increase an individual's likelihood of developing chronic pancreatitis?
Hashimoto thyroiditis
Splenic varices
Hepatitis
Hyperparathyroidism
Hyperparathyroidism
Cystic fibrosis is associated with an increased risk of:
Pancreatic cysts
Pancreatic calcifications
Pancreatic duct stones
Pancreatic cystadenocarcinoma
Pancreatic cysts
Amylase converts:
Sugar to starch
Starch to sugar
Sugar to fat
Fat to starch
Starch to sugar