Behavior Disorders Exam 4
1/96
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
97 Terms
Dimensional model
Individuals are rated on the degree to which they exhibit various personality traits
Five factor model of personality (“Big Five”)
Openness to experience
Conscientiousness
Extraversion
Agreeableness
Neuroticism
Prevalence of personality disorders
Affects about 10% of the general population
Origins and course of personality disorders
Thought to begin in childhood
Tend to run a chronic course if untreated
May transition into a different personality disorder
Gender distribution and gender bias in diagnosis
Men more often show traits like aggression and detachment; women more often show deference to others and insecurity in interpersonal relationships
Antisocial Personality Disorder – more often male
Dependent Personality Disorder – more often female
Cluster A
Odd or Eccentric
Paranoid, Schizoid, and Schizotypal personality disorder
Cluster B
Dramatic or Erratic
Antisocial, Borderline, Histrionic, and Narcissistic personality disorder
Cluster C
Anxious or Fearful
Avoidant, Dependent, and Obsessive-compulsive personality disorder
Cluster A (Odd or Eccentric)
Paranoid Personality Disorder
(Overview and clinical features)
Pervasive and unjustified mistrust and suspicion
Few meaningful relationships, sensitive to criticism
Distrust and suspiciousness of others such that their motives are interpreted as malevolen
Cluster A (Odd or Eccentric)
Paranoid Personality Disorder
(Causes)
May involve early learning that people and the world are dangerous or deceptive
Cluster A (Odd or Eccentric)
Paranoid Personality Disorder
(Cultural factors)
More often found in people with experiences that lead to mistrust of others (e.g., prisoners, refugees)
Cluster A (Odd or Eccentric)
Paranoid Personality Disorder
(Treatment)
Focuses on development of trust; cognitive therapy to counter negativistic thinking
Cluster A (Odd or Eccentric)
Schizoid Personality Disorder
(Overview and clinical features)
Detachment from social relationships and a restricted range of expression of emotions in interpersonal settings
Very limited range of emotions in interpersonal situations
Etiology is unclear but may have significant overlap with autism spectrum disorder
Cluster A (Odd or Eccentric)
Schizoid Personality Disorder
(Treatment)
Focus on the value of interpersonal relationships and on building empathy and social skills
Cluster A (Odd or Eccentric)
Schizotypal Personality Disorder
(Overview and clinical features)
Behavior and beliefs are odd and unusual
Socially isolated and highly suspicious
Magical thinking, ideas of reference, and illusions (not delusions)
Many meet criteria for major depression
Some conceptualize this as resembling a milder form of schizophrenia
Cluster A (Odd or Eccentric)
Schizotypal Personality Disorder
(Causes)
Mild expression of “schizophrenia genes”?
May be more likely to develop after childhood maltreatment or trauma, especially in men
More generalized brain deficits may be present
Cluster A (Odd or Eccentric)
Schizotypal Personality Disorder
(Treatment)
Address comorbid depression
Main focus is combination of medication, cognitive behavior therapy, and social skills training
Cluster B (Dramatic or Erratic):
Antisocial Personality Disorder
(Overview and clinical features)
Failure to comply with social norms
Violation of the rights of others
Irresponsible, impulsive, and deceitful
Lack of a conscience, empathy, and remorse
May be very charming, interpersonally manipulative
“Sociopathy” and “psychopathy” typically refer to very similar traits
Psychopathy
Similar to antisocial personality disorder but with less emphasis on overt behavior
Indicators include superficial charm, lack of remorse, and other personality characteristics
Cluster B (Dramatic or Erratic):
Antisocial Personality Disorder
(Causes)
Often show early histories of behavioral problems, including conduct disorder
“Callous-unemotional” type of conduct disorder more likely to evolve into antisocial PD
Families with inconsistent parental discipline and support
Families often have histories of criminal and violent behavior
Recent research suggests that psychopathy is a less reliable predictor of criminality (and there are “successful psychopaths”)
Neurobiological Contributions to Antisocial Personality
Prevailing neurobiological theories
Underarousal hypothesis – cortical arousal is too low
Cortical immaturity hypothesis – cerebral cortex is not fully developed
Fearlessness hypothesis – fail to respond to danger cues
Gray’s model: Inhibition signals are outweighed by reward signals
Underarousal hypothesis
Cortical arousal is too low
Cortical immaturity hypothesis
Cerebral cortex is not fully developed
Fearlessness hypothesis
fail to respond to danger cues
Gray’s model
Inhibition signals are outweighed by reward signals
Development of Antisocial Personality
(Genetic influences)
More likely to develop antisocial behavior if parents have a history of antisocial behavior or criminality
Development of Antisocial Personality
(Developmental influences )
High-conflict childhood increases likelihood of APD in at-risk children
Development of Antisocial Personality
(Impaired fear conditioning)
Children who develop APD may not adequately learn to fear aversive consequences of negative actions (e.g., punishment for setting fires)
Development of Antisocial Personality
(Arousal theory)
People with APD are chronically under-aroused and seek stimulation from the types of activities that would be too fearful or aversive for most
Development of Antisocial Personality
(Psychological and social influences)
In research studies, psychopaths are less likely to give up when goal becomes unattainable
May explain why they persist with behavior (e.g., crime) that is punished
Development of Antisocial Personality (APD)
(Causes)
APD is the result of multiple interacting factors
Mutual biological-environmental influence
Early antisocial behavior alienates peers who would otherwise serve as corrective role models
Antisocial behavior and family stress mutually increase one another
Treatment of Antisocial Personality
Few seek treatment on their own
Antisocial behavior is predictive of poor prognosis
Emphasis is placed on prevention and rehabilitation
Often incarceration is the only viable alternative
May need to focus on practical (or selfish) consequences (e.g., if you assault someone you’ll go to prison)
Cluster B (Dramatic or Erratic):
Borderline Personality Disorder (BPD)
Unstable moods and relationships
Impulsivity, fear of abandonment, very poor self-image
Suicidal and nonsuicidal self-injurious thoughts and behaviors
Comorbidity rates are high with other mental disorders, particularly mood disorders, substance use disorders, and eating disorders
Risk for Borderline Personality Disorder
Strong genetic component
High emotional reactivity may be inherited
May have impaired functioning of limbic system
Early trauma/abuse increases risk
Risk for Borderline Personality Disorder
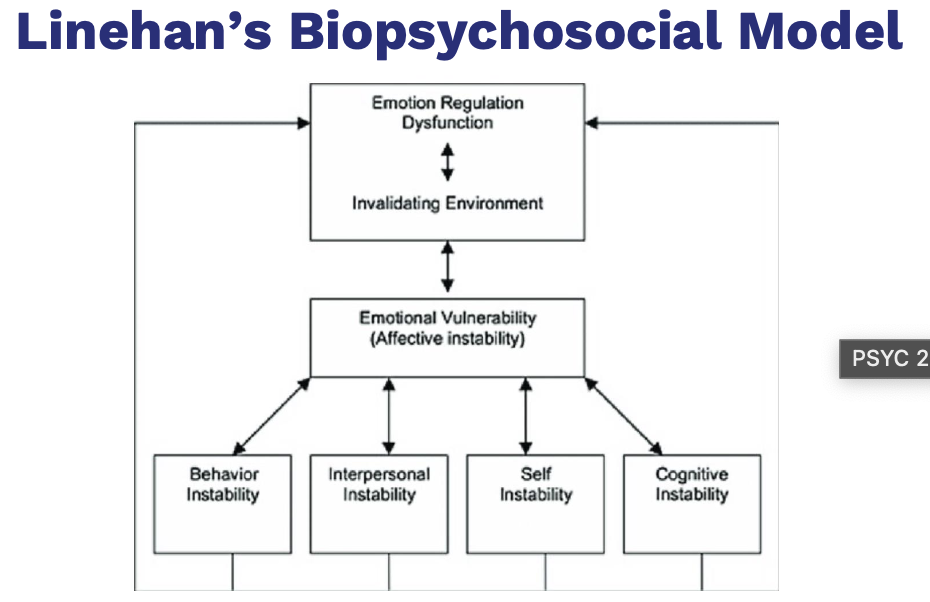
(“Triple vulnerability” model)
Generalized biological vulnerability
Generalized psychological vulnerability
Specific psychological vulnerability Linehan’s Biopsychosocial Model of Risk
Borderline Personality Disorder Treatment
Antidepressant medications provide some short-term relief
Dialectical behavior therapy* is most promising treatment
Focus on dual reality of acceptance of difficulties and need for change
Focus on interpersonal effectiveness
Focus on distress tolerance to decrease reckless/self-harming behavior
Dialectical behavior therapy (DPT)
Most promising treatment for Borderline Personality Disorder (BPD)
Involves exposing the client to stressors in a controlled situation
Helping the client regulate emotions and cope with stressors
Cluster B (Dramatic or Erratic):
Histrionic Personality Disorder
(Overview and clinical features)
Overly dramatic and sensational
May be sexually provocative
Often impulsive and need to be the center of attention
Thinking and emotions are perceived as shallow
More commonly diagnosed in females
Histrionic Personality Disorder
(Causes)
Etiology unknown due to lack of research
Histrionic Personality Disorder
(Treatment options)
Focus on attention seeking and long-term negative consequences
Targets may also include problematic interpersonal behaviors
Little evidence that treatment is effective
Cluster B (Dramatic or Erratic):
Narcissistic Personality Disorder
(Overview and clinical features)
Exaggerated and unreasonable sense of self-importance
Preoccupation with receiving attention
Lack sensitivity and compassion for other people
Highly sensitive to criticism; envious and arrogant
Narcissistic Personality Disorder
(Causes)
Largely unknown
Failure to learn empathy as a child
Sociological view - Product of the “me” generation (Baby Boomers)
Narcissistic Personality Disorder
(Treatment)
Focus on grandiosity, lack of empathy, unrealistic thinking
Emphasize realistic goals and coping skills for dealing with criticism
Little evidence that treatment is effective
Cluster C (Anxious or Fearful):
Avoidant Personality Disorder
(Overview and clinical features)
Extreme sensitivity to the opinions of others
Highly avoidant of most interpersonal relationships
Interpersonally anxious and fearful of rejection
Low self-esteem
Avoidant Personality Disorder
(Causes)
May be linked to schizophrenia; occurs more often in relatives of people with schizophrenia
Experiences of early rejection
Childhood experiences of neglect, isolation, rejection, and conflict with others
Avoidant Personality Disorder
(Treatment)
Similar to treatment for social phobia
Focus on social skills, entering anxiety-provoking situations
Good relationship with therapist is important
Cluster C (Anxious or Fearful):
Dependent Personality Disorder
(Overview and clinical features)
Reliance on others to make major and minor life decisions
Unreasonable fear of abandonment
Clingy and submissive in interpersonal relationships
Dependent Personality Disorder
(Causes)
Not well understood but may be linked to failure to learn independence
Dependent Personality Disorder
(Treatment options)
Therapy typically progresses gradually due to lack of independence
Cluster C (Anxious or Fearful):
Obsessive-Compulsive Personality Disorder (OCPD)
(Overview and clinical features)
Excessive and rigid fixation on doing things the right way
Highly perfectionistic, orderly, and emotionally shallow
Unwilling to delegate tasks because others will do them wrong
Difficulty with spontaneity
Often have interpersonal problems
Obsessions and compulsions are rare
Obsessive-Compulsive Personality Disorder (OCPD)
(Causes)
Are not well known
Moderate genetic contribution
Obsessive-Compulsive Personality Disorder (OCPD)
(Treatment )
Treatment targets include cognitive reappraisal techniques to reframe compulsive thoughts
Target rumination, procrastination, and feelings of inadequacy
Attention deficit hyperactivity disorder (ADHD)
Maladaptive levels of inattention, excessive activity, and impulsiveness
Specific learning disorder
Academic performance that is substantially below what would be expected given the person’s age, intelligence quotient (IQ) score, and education.
Childhood-onset fluency disorder
Stuttering
Language Disorder
Limited speech in all situations
Tourette’s disorder
Motor and vocal tics
High comorbidity with ADHD and OCD
Three subtypes of ADHD
Inattentive presentation
Hyperactivity -fidgeting
Impulsivity - blurting out things
ADHA Genetic contributions
Seems to fun in families
DAT1 – dopamine transporter gene has been implicated, as have norepinephrine, GABA, and serotonin
Neurobiological correlates of ADHD
Smaller brain volume
Inactivity of the frontal cortex and basal ganglia
Abnormal frontal lobe development and functioning
ADHD represents a Delay not a ….
not a Deviation in brain development
Biological Treatment of ADHD
Goal of biological treatments: reduce impulsivity and hyperactivity, improve attention
(T/F) ADHD is diagnosed more often in boys than girls
True
Causes of Specific Learning Disorder
Learning disorders run in families, but specific difficulties are not inherited
Two main areas of impairment in Autism Spectrum disorder
Two main areas of impairment: Communication and social interaction
10% to 33% don’t acquire effective speech
Restricted, repetitive patterns of behavior, interests, or activities
Rett disorder (genetic disorder associated with MeCP2 gene)
Constant hand-wringing, intellectual disability, and impaired motor skills.
Defects in Joint attention
The ability to communicate interest in an external stimulus and another person at the same time
Naturalistic teaching strategies
Arranging the environment so that the child initiates an interest (such as placing a favorite toy just out of reach)
Lesch-Nyhan syndrome
Intellectual disability, symptoms of cerebral palsy, self-injurious behavior
Phenylketonuria (PKU)
Cannot break down phenylalanine, which is found in some foods
Results in intellectual disability when the individual eats phenylalanine
Down syndrome
Most common chromosomal cause of intellectual disability
Extra 21st chromosome (Trisomy 21)
Distinctive physical symptoms
Fragile X syndrome
Symptoms include learning disabilities, hyperactivity, short attention span, gaze avoidance, perseverative speech
Primarily affects males
Cultural-familial intellectual disability
Refers to intellectual disability influenced by social environmental factors, such as:
Abuse
Neglect
Social deprivation
(T/F) If someone has PKU, dietary manipulations can prevent them from developing intellectual disability?
True
Delirium
Temporary confusion and disorientation
Major or mild neurocognitive disorder
Broad cognitive deterioration affecting multiple domains
Alzheimer’s disease causes dementia
Due to prion disease
proteins in the brain that reproduce and cause damage
Frontotemporal
Due to Parkinson’s Disease
Dopamine pathway damage
Motor problems- Tremors, posture, walking, speech
Vascular
Due to Huntington’s disease
genetic autosomal dominant disorder
Caused by a gene on chromosome 4
involuntary limb movements
Aphasia
difficulty with language
Apraxia
impaired motor functioning
Agnosia
failure to recognize objects
Vascular Neurocognitive Disorder
Caused by blockage or damage to blood vessels
Second leading cause of neurocognitive disorder after Alzheimer’s disease
Onset is often sudden (e.g., stroke)
Pick’s disease
Produces a cortical dementia like Alzheimer’s
Occurs relatively early in life (around 40s or 50s)
Neurocognitive Disorder Due to Lewy Body Disease
Lewy bodies are microscopic protein deposits that damage the brain over time
Symptoms onset gradually
Symptoms include impaired attention and alertness, visual hallucinations, motor impairment
Creutzfeldt-Jakob disease
Type of Prion Disease
May result from a number of sources, including the consumption of beef from cattle with “mad cow disease.”
Deterministic genes
Rare genes that inevitably lead to Alzheimer’s
Beta-amyloid precursor gene
Presenilin-1 and Presenilin-2 genes
Susceptibility genes
Make it more likely but not certain to develop Alzheimer’s
ApoE4 gene is located on chromosome 19 and associated with late onset Alzheimer’s
Civil commitment laws
When a person can be legally declared to have a mental illness and be placed in a hospital for treatment
Deinstitutionalization
Movement of people with mental illness out of institutions
Problem: Led large numbers of ill people to become homeless
Transinstitutionalization
In practice, people with mental illness have been moved out of large mental hospitals to other institutions, including prisons and nursing homes
Criminal commitment
Accused of committing a crime and are also Detained in mental health facility
Diminished capacity
Reduced ability to understand their behavior
Requirements for competence
Understanding of legal charges
Ability to assist in one’s own defense
Essential for trial or legal processes
Burden of proof is on the defense
Tarasoff v. Regents of the University of California
Must warn individual in danger
Clinical efficacy axis
Involves thorough consideration of scientific evidence to determine whether intervention is effective compared to alternative treatment
Clinical utility axis
Concerned with the effectiveness of the intervention in the practice setting (i.e., are results generalizable to real world)