visual fields I
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
40 Terms
what is the visual field - define
The extent of space in which objects are visible to an eye in a given position - not just central but everything you can see (peripheral etc.)
state the size of the visual field (monocular and binocular)
Monocular Field is approx:
o100° temporally
o60° nasally - smaller due to nose
o60° superiorly - smaller due to brows
o75° inferiorly
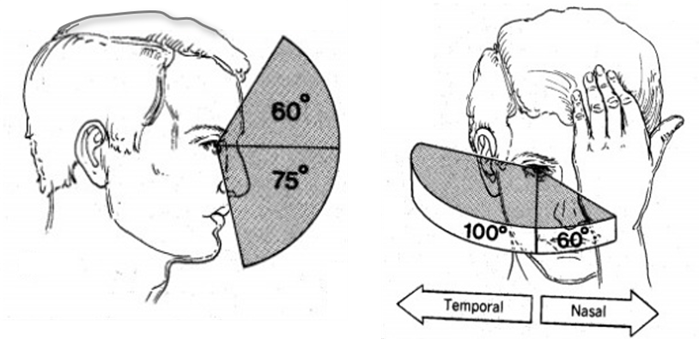
Binocular field:
o120° horizontally
what is the visual field determined by (2)
by our retina
and also the connectivity between the retina and the brain (the visual pathway)
therefore what can the visual field tell us/give us information about (3)
can tell us about abnormalities or damage in the visual system anywhere along this pathway - can be used to detect glaucoma
the characteristic appearance of the visual field defect can help pinpoint exactly where along the pathway the problem lies
diseases anywhere along the visual pathway (including in the brain) can cause problems with a patient’s vision, so it’s not just diseases of the eye that you need to be aware of!
state the 3 main purposes of measuring the visual field
–Detection of abnormalities in visual function
–Locating the site of the abnormality
–Monitoring disease progression
what is static perimetry and explain its general principle (4)
visual field test used to measure a person’s sensitivity to light at different points in their field of vision
measure a patient’s discrimination threshold
this tells us when the patient is just able to detect that the stimulus luminance (a light) is different from the background luminance (a type of contrast perception task)
light stimuli stay in one fixed location, but their intensity (brightness) changes to find the threshold of detection.
define discrimination threshold
•∆L / L (where L is luminance)
Remember, threshold is the minimum amount of change that can be detected - if something cannot be detected - we would say it is BELOW threshold
the smaller the number = the smaller the threshold
what is considered to be within normal threshold values
‘Normal’ threshold values will vary with age and retinal eccentricity (how far away from the fovea a retinal location is)
Most visual field tests are measuring a patient’s threshold at multiple locations and comparing the result with these ‘normal’ values
describe the link between threshold and sensitivity
•The smaller the threshold value, the more sensitive the patient is to small changes in luminance
•So, sensitivity is the reciprocal of the threshold value
how is stimulus intensity/sensitivity graded (3)
Most visual field machines generate light of varying intensities (using neutral density filters)
Stimulus intensity is then graded in decibels (dB) using a logarithmic scale.
The higher the dB value, the dimmer (or less intense) the light
explain how we measure threshold using sensitivity and the dB scale (4)
We tend to measure a patient’s threshold by measuring their sensitivity to light intensities on the dB scale
Greater sensitivity (the ability to discriminate very small changes in luminance between the stimulus and the background) is represented by higher dBs
poor sensitivity (where the difference in luminance must be large in order for the patient to detect it) is represented by lower dB values
So, a threshold of 33dB would be considered good, and a threshold of 6dB would be considered poor - higher dB value = good and vv
Remember, someone with a low threshold for detecting change in light intensity is highly sensitive. !!!
what average sensitivity would we expect in a healthy/young px
33dB
however different normal levels based on px age
limitation of using dB scale to establish sensitivity
sensitivity (dB) cannot be compared across different types of machine
because the calculation is based on the background luminance of the machine and the maximum intensity of the bulbs in the machine - which varies between manufacturers
state the methods we can use to determine threshold (3)
method of limits
stair case
psychometric function
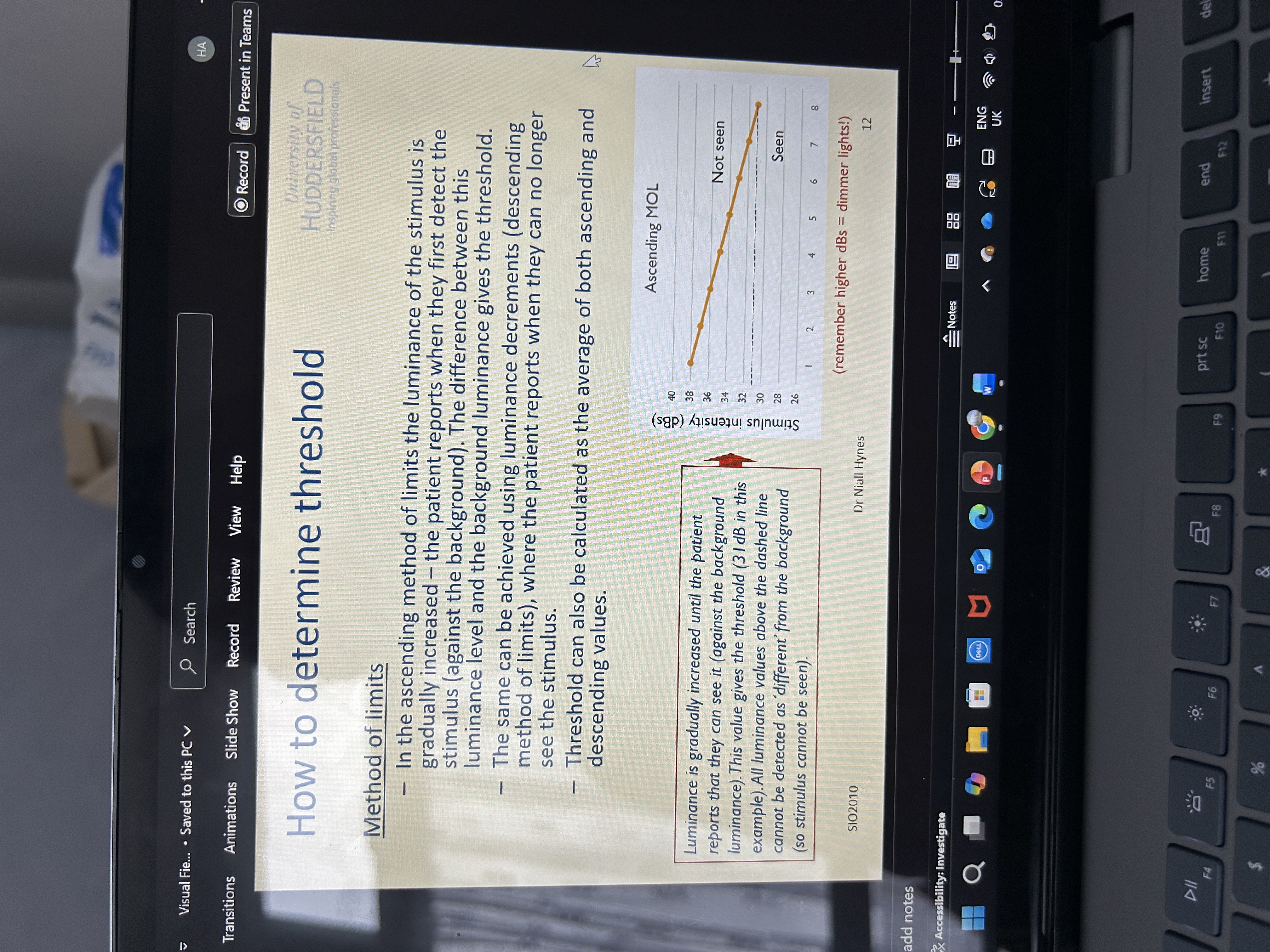
explain the method of limits in determining threshold (5)
the luminance of the stimulus is gradually increased
the patient reports when they first detect the stimulus (against the background)
The difference between this luminance level and the background luminance gives the threshold
the same can be achieved using luminance decrements (descending method of limits), where the patient reports when they can no longer see the stimulus - start bright and gradually dim until they cannot see it
Threshold can also be calculated as the average of both ascending and descending values - best way to do it
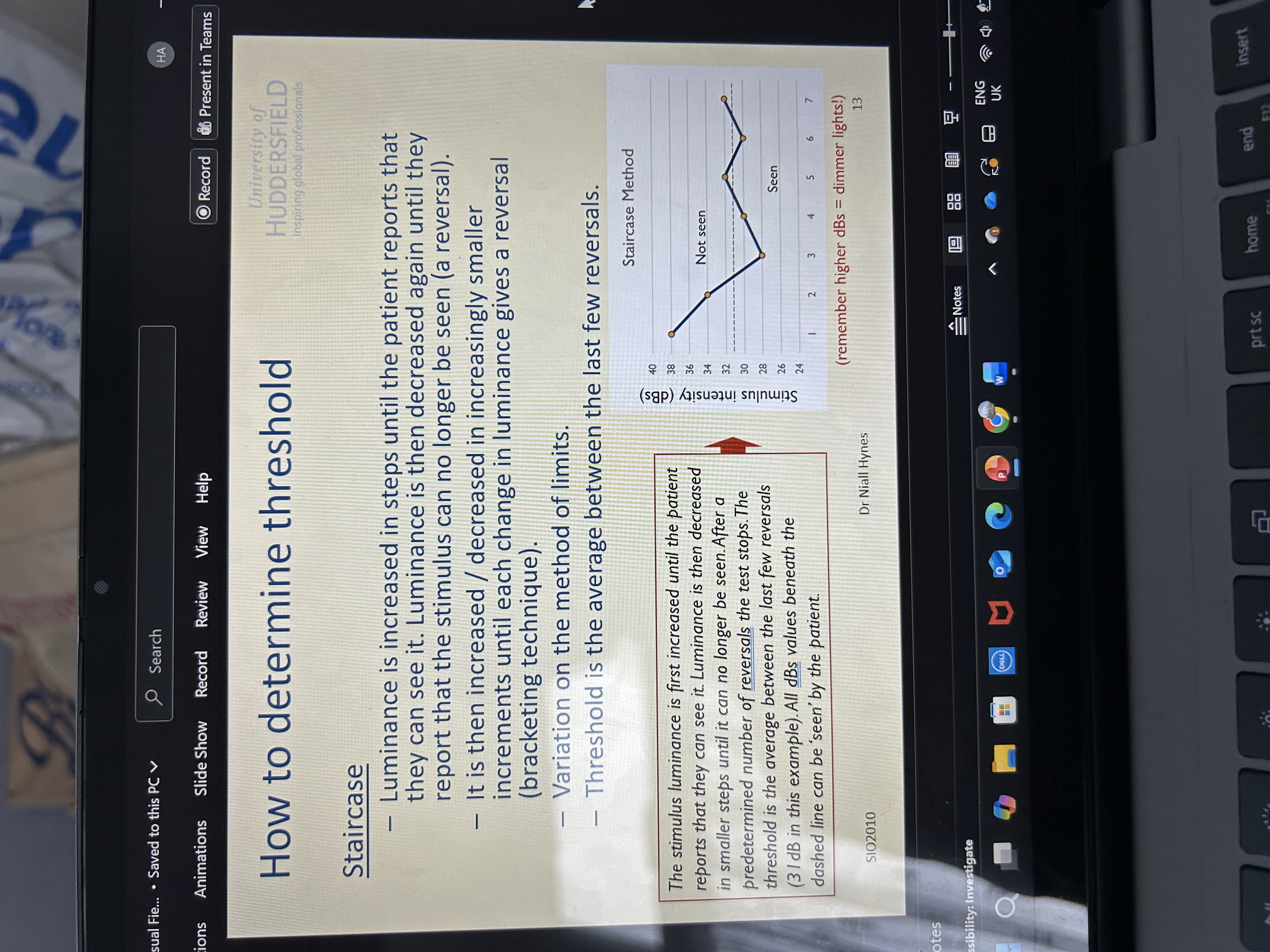
explain the staircase method in determining luminance (5)
Luminance is increased in steps until the patient reports that they can see it
Luminance is then decreased again until they report that the stimulus can no longer be seen (a reversal)
It is then increased / decreased in increasingly smaller increments until each change in luminance gives a reversal (bracketing technique)
Variation on the method of limits
Threshold is the average between the last few reversals
explain the psychometric function method in determining threshold (8)
Stimuli are presented at different intensities (luminance values), and the patient reports when they can see the stimulus
A curve can be plotted showing the different stimulus intensities in dB (x axis) against the percentage of times the patient responded that they saw the stimulus (y axis)
When they could see the stimulus 50% of the time, the corresponding value is taken as the threshold (24dB in this example)
As the light gets brighter, the % of “yes” responses increases
So, the curve starts low and rises like an S-shape (sigmoid).
However, if you wanted to be certain that the patient could detect the stimulus you could choose a different y-axis value to indicate the threshold (75% for instance) - “At this intensity, the patient detects the light 3 out of 4 times — we’re more certain it’s visible.” - in comparison to the 50%
The steeper the curve, the less variable the patient’s responses were - the patient goes from not seeing → seeing the stimulus very quickly as brightness increases → Their responses are consistent and reliable.
very time consuming however !!!

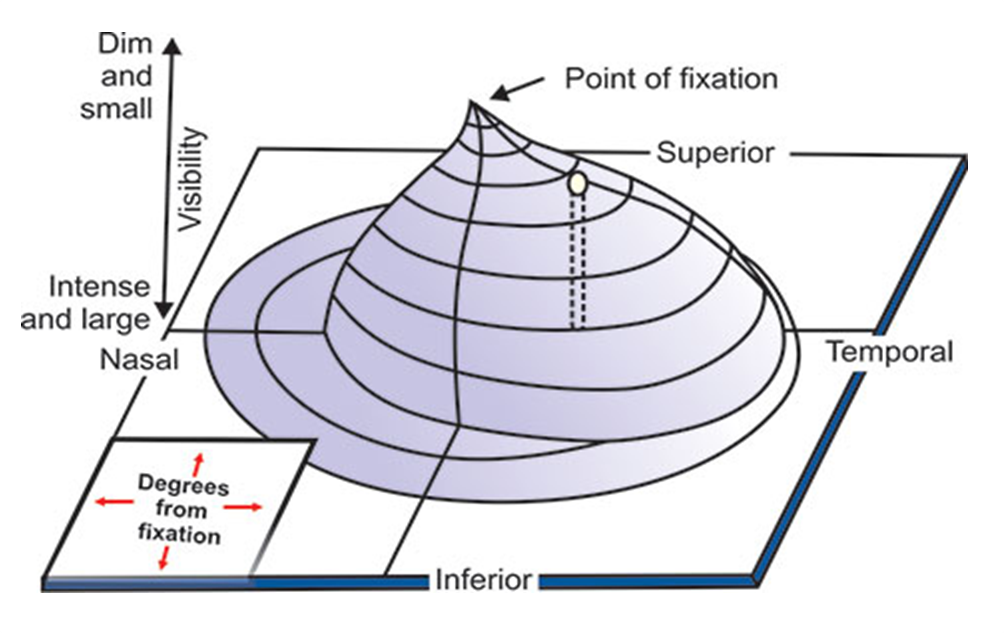
describe what is meant by the ‘hill of vision’/island of vision (4)
3D representation of the sensitivity of the retina (or visual field) to light - shows how sensitive different parts of your retina are to light stimuli.
Sensitivity is highest at the fovea (centre) and gradually decreases toward the periphery
therefore sensitivity decreases with increasing eccentricity
note the optic disk - physiological blind spot - see the dip in the diagram - 15 degrees to the side

why do we still see a complete image even though we have a blind spot
due to BV - information from both eyes together
brain fills the rest of the information in
define perimetry
The determination of the extent of the visual field, usually for the purpose of detecting anomalies in the visual pathway
essentially - visual field testing
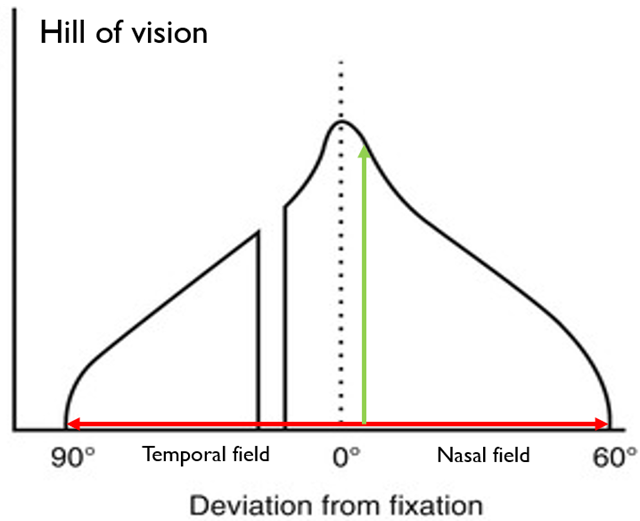
may want to measure the extent (red arrow – width of the plot) of the visual field, and/or the sensitivity (green arrow – height of plot) of vision at various locations within the field
explain how certain pathologies can affect the sensitivity of a px’s vision and their visual fields (4)
Certain ocular pathologies such as cataract or glaucoma can affect the sensitivity of our patient’s vision
This would mean that lights need to be brighter in order for them to be detected (compared with a normal eye)
This may also impair the patient’s day-to-day visual function
Other conditions such as retinitis pigmentosa (progressive degeneration of photoreceptors - mainly rods, then cones = gradual vision loss) can constrict the visual field (‘tunnel vision’ - can be compared to like looking through a straw) in which case we might want to measure the extent of the patient’s visual field - can affect driving (day to day tasks)
describe what kinetic perimetry is (3)
type of visual field test where the stimulus/targets are moving
a moving light stimulus (of fixed brightness and size) is brought from an area the patient cannot see (the periphery) toward the centre of vision until it becomes visible
plots the FULL extent of the px visual field - how far in degrees they can see
kinetic vs static perimetry (5)
Feature | Kinetic | Static |
|---|---|---|
Stimulus | Moving | Stationary |
Brightness | Fixed | Varies |
Measures | Field extent (boundaries) | Light sensitivity (threshold) |
Typical tool | Goldmann perimeter | Humphrey perimeter |
Best for | Mapping field shape | Detecting early/central defects |
describe the limitations of kinetic perimetry (2)
perhaps not the best method for plotting localised scotomas (small, specific blind spots) - as focuses on boundaries not sensitivity, moving stimulus can skip over small scotomas, examiner dependent (subjective), better for gross field defects
or determining the patient’s threshold - not good at determining a px’s sensitivity (e.g. in early glaucoma - causes subtle decreases in sensitivity, not total vision loss - kinetic perimetry can’t pick that up)
what can we use to measure kinetic perimetry (2)
goldmann perimeter - most popular - introduced in 1945
octopus 900 machine
explain the procedure of using the Goldmann perimeter to measure kinetic perimetry (5)
maps the entire visual field with different targets (lights which varied in size and brightness)
patient stares at the centre of the machine - and the target lights are gradually moved from the outside of the bowl (from where they cannot be seen) in towards the centre
smaller targets wouldn’t be able to appreciate in the periphery but more likely to appreciate in the centre as sensitivity is higher here
The patient reports when they first see the light, and also if it disappears at all
This can be very time consuming!

explain Goldmann field plots (4)
chart showing how sensitive a px’s visual field is - test uses moving light stimuli (kinetic perimetry), and the patient tells the examiner when they first see each one. The results are then plotted manually on a circular chart
Different targets are plotted in different colours - makes it easy to compare how different stimuli create different isopters (lines of equal sensitivity)
Typically larger, brighter targets are more easily detected than small dim ones - big, bright lights stimulate more photoreceptors → easier to see → create larger isopters (extend further into periphery) and vv
The blind spot is drawn in black - where the optic nerve exists - no photoreceptors
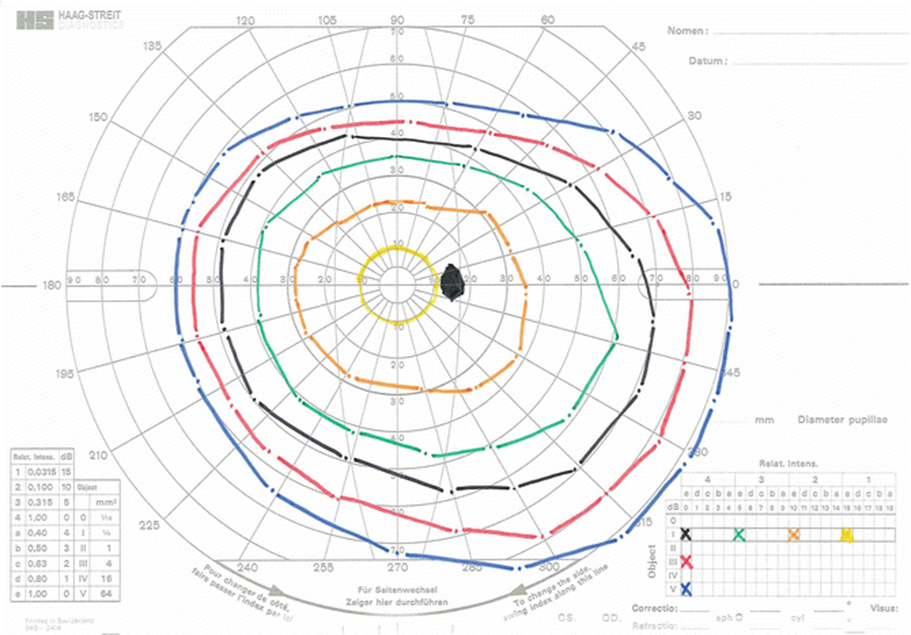
explain how we can interpret results/notations/values from the Goldmann field plots (4)
Target size varied from 0 (0.0625mm2) to V (64mm2) - small to big - each Roman numeral step roughly quadruples the area
Target intensity (brightness) varied from 1a (19dB = dimmest) to 4e (0dB = brightest)
Number (1–4) = major brightness step - Letter (a–e) = minor step within that number - So, 1a is dimmest, and 4e is brightest
If you see a notation like III4e, that means:
III → medium-sized stimulus
4e → very bright
→ So this target is large and bright → easily seen → produces a large outer isopter.
Conversely, I1a means:
Smallest and dimmest stimulus → difficult to see → forms a tiny central isopter.
explain the use of automated static perimetry (5)
the targets / stimuli do not move - they are simply presented (flashed on/off) at a number of different locations within the patient’s visual field
this is done on a computerized/automated machine (unlike the Goldmann which requires manual operation) - less time consuming
Useful for measuring the patient’s threshold or detecting localised scotomas
Tests can be categorised as ‘threshold’ (measuring sensitivity for each point) or ‘suprathreshold’ (measuring for a few points - easier target to measure so quicker)
Various machines available, most popular in the UK include the Humphrey Visual Field Analyser (Zeiss), Henson (Elektron Eye Technology) and Octopus (Haag Streit)
what are the standard automated visual field test programs used in perimetry
30-2
24-2
tell the machine where to show light spots to see which parts of your vision are working well and which might have defects.
The difference between them is mainly how wide the field is tested (30° vs 24°) and how many points are checked (76 vs 54).
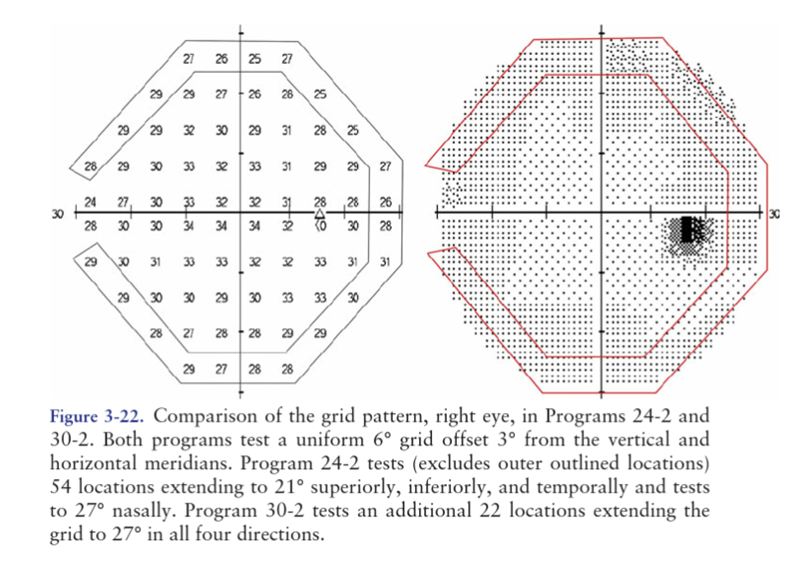
explain the 30-2 test program (5)
presents stimuli to 76 different locations/point within a uniform grid
The test extends out to 30° from fixation - central 30 degrees (field tested)
stimuli are spaced 6° apart - vertically and horizontally
The “-2” in the name refers to the fact that stimuli are offset from the vertical and horizontal midline by 3°
mainly used for wider central and near periphery
explain the 24-2 test program (5)
extends out to 21° in all directions except nasally, where it goes out to 27° (as early glaucomatous field loss can occur in the nasal region)
It therefore tests 54 locations
spacing between locations - 6 degrees horizontally and vertically
midline offset - yes (-2-3 degrees)
mainly used for central vision and routine glaucoma checking
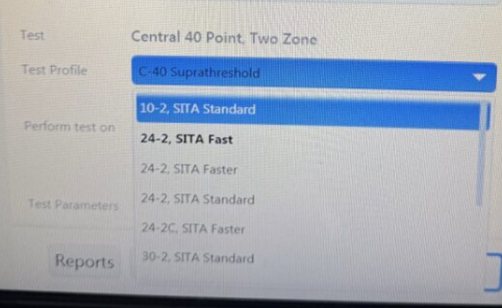
explain the use of threshold tests (3)
These plot the patient’s exact threshold at various locations
Useful for detecting or monitoring subtle changes such as in early disease
However, this can be time consuming! On the Humphrey VFA the ‘full threshold’ method employs a ‘staircase’ at each location
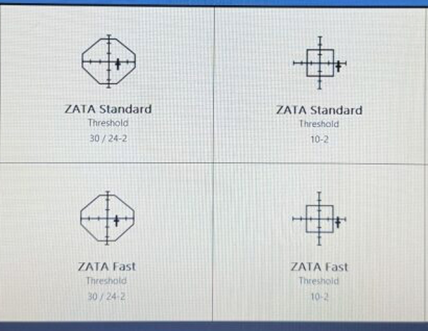
explain the efficiency of modern automated perimetry in threshold testing (4)
Often modern machines employ a special algorithm to help predict the patient’s thresholds based on knowledge of a ‘normal’ visual field, and threshold values that have already been determined in nearby locations – this speeds up the test considerably - don’t have to go through each point
Humphrey VFA this is called SITA - Octopus is called TOP - Henson, it is called ZATA.
They all work in slightly different ways!!
Typically, it takes ~3-5 minutes per eye, to do a full threshold test - varies depending if there is an issue or not - and also depends on the px
explain the use and benefit of suprathreshold tests that have a single stimulus (4)
tend to use age-matched normal values as a starting point, and then present stimuli which are several decibels brighter
assumption is that all stimuli will be above the patient’s threshold (easily seen), and someone with a normal field will get a full score
It is quicker, and not as difficult for the patient (as most lights can be easily detected)
can therefore be used a screening tool
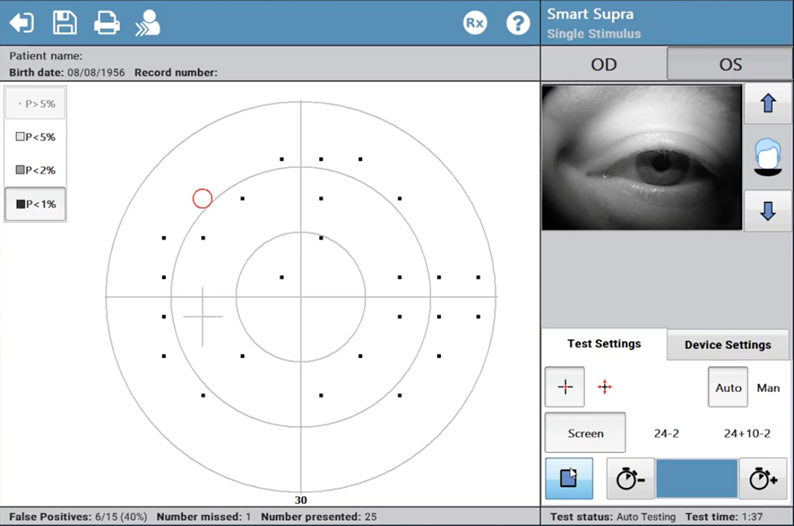
what is the limitation of single stimulus suprathreshold tests (2)
they may miss subtle defects…
If the field is abnormal it can be very time consuming, as the machine goes on to plot the exact threshold of each ‘missed’ point (not using the speedy algorithm).
explain the use of suprathreshold tests that have multiple stimulus (5)
Initially determines a rough ‘threshold’ for the patient, then presents subsequent stimuli several dB above threshold
Presents between 1-4 stimuli simultaneously at different locations.
Patient must state how many lights are ‘seen’ on each presentation
Any missed points (i.e. the patient indicates that fewer lights are seen than were actually presented), must be determined using a clock face analogy (“where were the lights in relation to the numbers on a clock?”). The examiner can then indicate missed stimuli on the printout.
A very quick screening tool - may need to do further tests (single stimulus) or more sensitive tests if there is an issue
what are some specialist tests we can use to measure threshold (2)
10-2 test
Estermann test
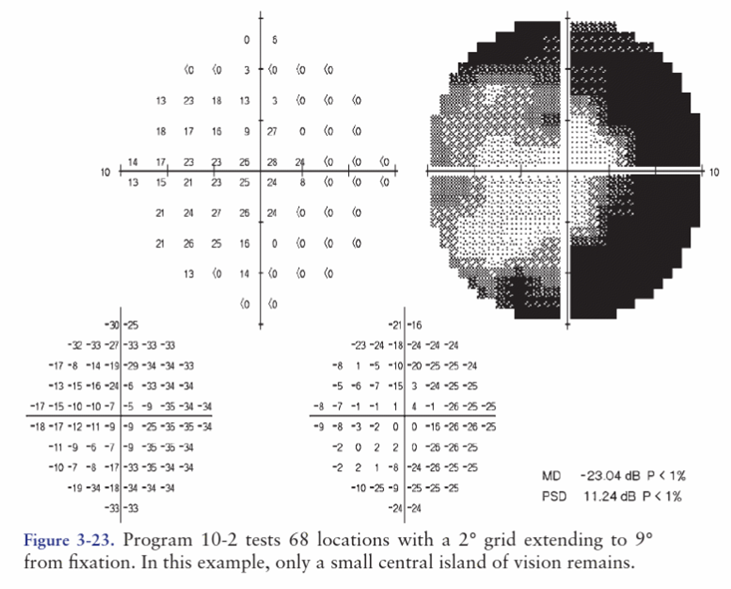
explain the 10-2 test and when it would be helpful (4)
concentrates on the macular region
testing out to central 10°, with stimulus spacing of 2°
tests 68 locations within the 10 degrees in total - very sensitive
can be helpful in mapping out central defects, or in end-stage disease where only a small island of vision is remaining (as 24-2 would take a very long time to complete).
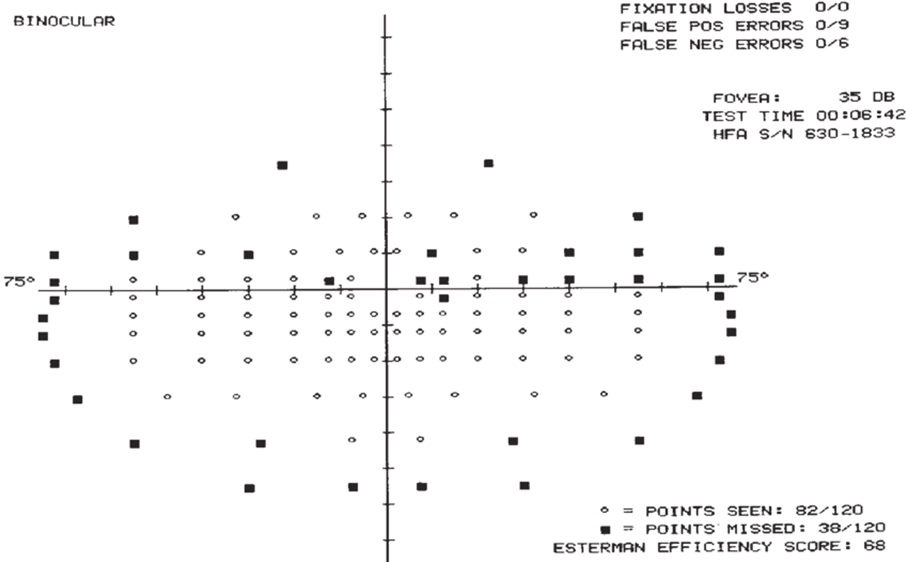
explain the Estermann test (3)
a binocular (in comparison to all the other tests we have looked at which are MV), suprathreshold test
often used to determine a patient’s legality to drive (may be requested by the DVLA)
It tests 120 points at 10dB (fairly bright stimuli), and spans ~150° horizontally and 90° vertically.