Pulmonary Special Tests Study Worksheet – PCM III
1/12
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
13 Terms
1. Describe how to perform percussion of the thorax. What are you listening for?
1. Percussion involves tapping the chest wall with fingers to assess resonance. Dullness suggests consolidation or effusion; hyperresonance suggests pneumothorax or hyperinflation.
1. What is tactile fremitus and how is it assessed? What does increased vs decreased fremitus suggest?
1. Tactile fremitus is the vibration felt on the chest when the patient speaks (often saying something like '99'). Vibration is always felt in normal patients. It is the difference in comparison side-to-side that we are looking for. Increased fremitus is caused by things that make the lungs more dense, like consolidation. Decreased fremitus is caused by things that make the lungs less dense, like pneumothorax or chronic obstructive pulmonary diseases. (Interestingly, pleural effusions also cause decrease fremitus in the lower part of the effusion, which is counterintuitive, but near the top of the effusion will have an increase in fremitus.)
1. How is egophony tested, and what does a positive result mean?
1. Egophony: Have patient say 'E' while auscultating. If it sounds like 'A', this suggests lung consolidation.
1. What is bronchophony, and how do you perform and interpret the test?
1. Bronchophony: Have patient say '99'. If it sounds loud and clear, it's positive, indicating consolidation.
1. How is whispered pectoriloquy tested, and what would a positive finding suggest?
1. Whispered pectoriloquy: Patient whispers '1-2-3'. If whispered words are distinctly heard, it's positive and suggests consolidation.
1. How do you assess diaphragmatic excursion? What conditions might reduce excursion?
1. Excursion: Ask patient to exhale fully, percuss to find dullness, then repeat during full inspiration. Mark the distance. Decreased in COPD, effusion, or neuromuscular weakness.
1. What exam findings might suggest a pneumothorax?
1. Pneumothorax may present with hyperresonance to percussion, decreased fremitus, absent breath sounds, and tracheal deviation (if tension).
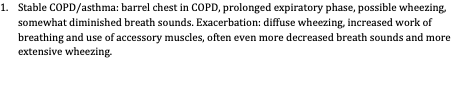
1. What findings might you expect in stable COPD or asthma? How does this change compared to those found during an exacerbation?
1. Stable COPD/asthma: barrel chest in COPD, prolonged expiratory phase, possible wheezing, somewhat diminished breath sounds. Exacerbation: diffuse wheezing, increased work of breathing and use of accessory muscles, often even more decreased breath sounds and more extensive wheezing.
1. Which of the following findings is most consistent with lung consolidation?
A. Hyperresonance to percussion, decreased fremitus, and absent breath sounds
B. Dullness to percussion, increased fremitus, and egophony
C. Tympany to percussion, decreased fremitus, and crackles
D. Dullness to percussion, decreased fremitus, and normal breath sounds
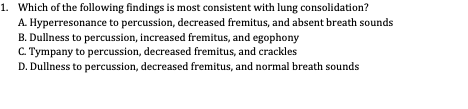
1. Answer: B – Consolidation causes dullness, increased fremitus, and egophony.
1. Which of the following suggests a pleural effusion?
A. Increased tactile fremitus and bronchophony
B. Hyperresonance to percussion and increased breath sounds
C. Dullness to percussion and decreased breath sounds
D. Tympany to percussion and wheezing
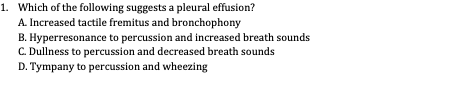
1. Answer: C – Pleural effusion causes dullness, decreased breath sounds, and decreased fremitus.
Egophony is considered positive when 'E' sounds like 'A' over an area of consolidation. (T/F)
1. True – The 'E to A' change (egophony) is a classic sign of consolidation.
1. Whispered pectoriloquy is decreased in the setting of lung consolidation. (T/F)
1. False – Whispered pectoriloquy is increased (not decreased) in consolidation.
1. Matching
a. Tactile fremitus
b. Egophony
c. Percussion
d. Whispered pectoriloquy
1. Detects changes in vocal transmission through lung tissue
2. Dullness or hyperresonance suggests pathology
3. Whispered numbers are heard clearly over consolidation
4. 'E' to 'A' change in sound over affected lung field
1. Match:
a → 1
b → 4
c → 2
d → 3