Module 3: Oral Manifestations of Collagen Vascular Disease
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
25 Terms
collagen vascular disease
-group of acquired disease that have common diffuse inflammation of small blood vessels and connective tissue, but various etiologies
Sjorgen syndrome pathophysiology
*Chronic, systemic autoimmune disease
*Unknown cause
*Lymphocytic infiltration of exocrine glands that produce tears (lacrimal glands) and saliva (salivary gland) → chronic impairment
1. Plasmacytoid dendritic cells release interferon (protein released in response to pathogens)
2. IFN stimulates salivary acinar and duct cells to produce autoantigens: Ro (SSA) & La (SSB)
3. Post-transcriptional modification of Ro/La increases autoantigenicity
4. Acinar and ductal epithelial cells present Ro/La to Th-cells
5. Th Cells activate cytotoxic T Cells and B/Plasma Cells
6. Autoreactive T Cells and autoantibody producing B Cells → necrosis of salivary gland epithelium
7. Upon necrosis, more Ro/La released which is taken up by APC
8. APC releases more interferon (cycle beings again)
Sjorgen syndrome epidemiology
*0.5% population
*Middle-aged adults
*Female 9:1
Sjorgen syndrome clinical features
*Enlargement of Major Salivary Gland
- 30-50%
- diffuse, firm enlargement of major salivary glands
- usually bilateral, nonpainful or slightly tender, intermittent or persistent
- risk of retrograde bacterial sialadenitis
- acini destroyed in chronic inflammation & dilation of salivary ducts
- punctate sialectasia (fruit-laden branchless tree) on sialogram
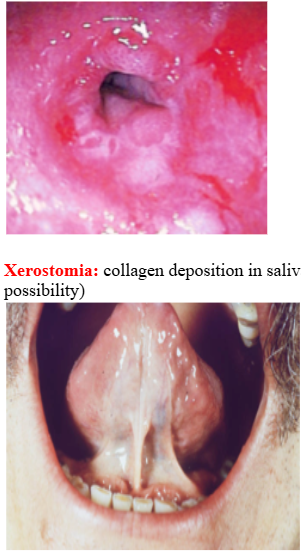
*Xerostomia (dry mouth)
- fissured tongue and atrophy of papillae
- saliva may appear frothy
- difficulty swallowing, altered taste, or difficulty in wearing dentures
- secondary candidiasis
- dental decay, especially cervical caries
*Xerophthalmia (dry eyes) – Keratoconjunctivitis sicca
- reduced tear production by the lacrimal glands → decreased watery layer of tear film but normal mucin production → mucoid discharge, resulting in scratchy, gritty sensation, perceived presence of foreign body
- defects of the ocular surface epithelium – blurred vision +/- aching pain
- ocular dryness worsens as day progresses
→Xerostomia + Xerophthalmia = Sicca Syndrome (extremely red conjunctiva)
Primary Sjogren Syndrome = Sicca Syndrome for > 3mo
Secondary Sjogren Syndrome = Sicca Syndrome + Another CT Disorder
- RA (15%), SLE (30%), Scleroderma, PBC
- may develop years after onset of above disease
*40x increased risk for lymphomas (MALT lymphomas)

Sjorgen syndrome diagnosis- Keratoconjunctivitis sicca
- Schirmer Test: confirms decreased tear production - filter paper placed over margin of lower eyelid; diagnostic if length of wetting <5mm after 5 min
- Rose Bengal Dye: stains damaged conjunctival and corneal cells
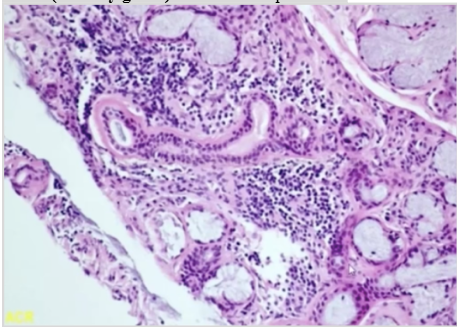
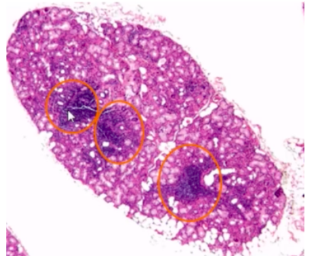
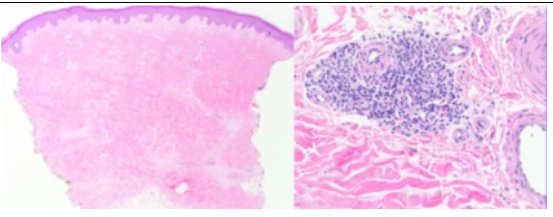
Sjorgen syndrome diagnosis- histopathology
- harvest minor salivary glands from incision on lower labial mucosa
- 1+ foci of chronic inflammatory cells (50+ lymphocytes & plasma cells) adjacent to normal=appearing acini per 4mm2
Sjorgen syndrome diagnosis- autoantibodies
- Specific for SS: presence of SSA and/or SSB antigens
- Non-specific: Rheumatoid Factor (60% of cases +, auto-Ab against Fc portion of IgG); ANA (75-85% of cases +, auto-Ab against various proteins in nucleus)
*High rbc sedimentation rate (non-specific measure of inflammation)
*Elevated serum IgG levels (indicative of immune status)
Sjorgen syndrome diagnosis- exclusion criteria
- Past head and neck radiation treatment
- Hepatitis C Infection
- AIDS
- Preexisting Lymphoma
- Sarcoidosis
- Graft-Versus-Host Disease (GVHD)
- Use of Anticholinergic Drugs
Sjorgen syndrome treatment
*Supportive Care:
- dry eyes → artificial tears
- dry mouth → artificial saliva, sugarless gum or candy, sialagogue modifications (pilocarpine, cevimeline)
- dental caries → daily fluoride application
- secondary candidiasis → antifungal therapy
systemic lupus erythematosus (SLE) pathophysiology
*Chronic disease of variable severity with waxing and waning course
*Significant morbidity, can be fatal
*Preclinical Phase: autoantibodies common to other autoimmune diseases
*More Disease: organ specific clinically overt autoimmune phase
*Late Damage: infection, atherosclerosis, malignancies – related to complications of longstanding disease and immunosuppressive therapy
*Apoptosis related release of endogenous nucleic acid antigens stimulate IFN production which in turn activate B and T cells
SLE epidemiology
*Average age at diagnosis = 31 years
*Women 8-10x
SLE clinical features
*Fever, weight loss, arthritis, fatigue, general malaise
SYSTEMIC:
*Malar Rash
- 40-50%
- butterfly pattern over malar area and nose
- sunlight makes lesions worse
*Cardiac Involvement:
- 30-50% - pericarditis with chest pain
- 50% - Libman-Sacks Endocarditis
(warty vegetations → mitral valve regurgitation)
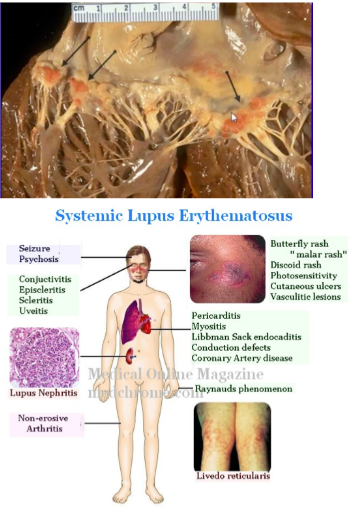
SLE oral manifestations
*Oral lesions in 5-25%
- palate, buccal mucosa, gingiva
- variable appearance – lichenoid areas, nonspecific ulcer, granulomatous lesion
*Lupus Cheilitis: vermillion of lower lip with varying degrees of ulceration, pain, erythema, hyperkeratosis

SLE diagnosis
*Direct immunofluorescence:
- Normal tissue (+ 26-60%) → Positive Lupus Band Test
- Lesional tissue (+95%)
- Deposition of immunoreactants (IgM, IgG, C3) in a shaggy or granular band at the basement membrane zone
- RA, Sjogren Syndrome, Systemic Sclerosis may have similar findings
*Serum Antibody Detection:
- ANA (antinuclear antibodies): 95%, non-specific (also in SS)
- Antibodies vs dsDNA: 70-80% (specific for SLE)
- Anti-SM (very specific for SLE)
SLE treatment
*Avoid excessive exposure to sunlight (UV may precipitate disease activity)
*Mild active disease: NSAIDS + antimalarials
*Severe acute episodes that involve arthritis, pericarditis, thrombocytopenia, nephritis: systemic corticosteroids +/- other immunosuppressive agents
SLE prognosis
*82-90% 5 year survival rate
*63-75% 20 year survival rate
*Depends on which organs are affected and how frequently disease reactivated
*Renal failure is most common cause of death
*Long-term immunosuppression medication → increased mortality due to infection and malignancy
*Worse prognosis for men than women
systemic sclerosis (Scleroderma) pathophysiology
*Relatively rare
*Immune-mediated condition
*Deposition of dense collagen in tissues and organs in extraordinary amounts → obliteration of blood vessels
*Most dramatic effects seen in skin
*Major organ-based complications involving lungs, heart, kidneys, GI determine morbidity and mortality
*Unknown etiology
systemic sclerosis epidemiology
*Relatively rare
*19/1,000,000 each year
*Female 5x
*Adults
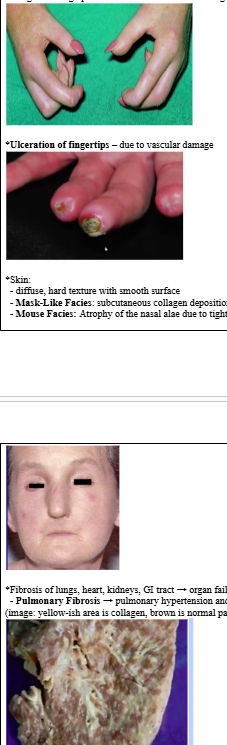
systemic sclerosis clinical features
*Raynaud Phenomenon:
- often 1st sign
- vasoconstriction in fingers, toes, ears, nose triggered by emotional distress or exposure to cold
- skin becomes white → blue and numb → red and throbbing
- can occur in healthy people
*Acro-osteolysis:
- resorption of terminal phalanges and flexion contractures (shortening of muscle tissue) → shorted fingers
- due to microvascular occlusion
*Sclerodactyly:
- due to abnormal collagen deposition → fingers become stiff, skin becomes tense/shiny
- fingers undergo permanent flexure → claw-like fingers
*Ulceration of fingertips – due to vascular damage
*Skin:
- diffuse, hard texture with smooth surface
- Mask-Like Facies: subcutaneous collagen deposition in facial skin → smooth, taut face
- Mouse Facies: Atrophy of the nasal alae due to tightening of the skin → pinched nose
*Fibrosis of lungs, heart, kidneys, GI tract → organ failure
- Pulmonary Fibrosis → pulmonary hypertension and heart failure, primary cause of death (image: yellow-ish area is collagen, brown is normal parenchyma)
systemic sclerosis oral manifestations
*Microstomia: limitation of mouth opening due to collagen deposition in perioral skin (70%)
*Purse String-Like Mouth: furrows radiating from mouth
*Loss of attached gingival mucosa and multiple gingival recession
- decreased vascularity and tissue ischemia resulting in increased periodontal disease and tooth mobility
*Dysphagia: collagen deposition in lingual and esophageal mucosa produces firm, hypomobile tongue and inelastic esophagus → hinders swallowing
*Xerostomia: collagen deposition in salivary gland tissues (secondary Sjogren Syndrome a possibility)
*Diffuse widening of the periodontal ligament space
(increased collagen synthesis in PDL)1
*Resorption of posterior ramus of the mandible, coronoid process, chin, condyle (+individual tooth resorption): due to increases pressure from collagen production
systemic sclerosis diagnosis
*Clinical signs: stiffened skin texture + Raynaud Phenomenon
*Skin biopsy: abundant collagen deposition
*Anti-topoisomerase I (anti-Scl70): systemic sclerosis – autoantibodies vs enzymes that regulate over/underwinding of DNA
systemic sclerosis treatment
*No medication for complete treatment
*Directed at controlling symptoms
- esophageal dilation for dysphagia
- Ca Channel blockers to increase blood flow
- ACEI for controlling HTN related to renal dysfunction
*Dental Management:
- Collapsible dental appliances with special hinges to facilitate insertion and removal of dentures for patients with microstomia
- Surgical correction of open bite associated with condylar resorption
systemic sclerosis prognosis
*Poor
*Especially poor if heart affected (most die of pulmonary involvement)
*Better in patients with limited cutaneous involvement: 80-90% 10 year survival
*Worse in patients with diffuse systemic sclerosis: 60-75% 10 year survival
1 scleroderma
*Mild variant of systemic sclerosis
*Affects only a solitary patch of skin
*”En Coup de Sabre” – Strike of the Sword: resembles scars
*Only a cosmetic concern, rarely life threatening

CREST syndrome (limited scleroderma)
*Mild variant of systemic sclerosis
*Adults: 50-70 years
*Female
*Signs may not appear synchronously but develop sequentially over months to years
Calcinosis cutis – calcium deposits in skin
Raynaud Phenomenon – spasm of vlood vessels to cold or stress
Esophageal Dysfunction – acid reflux and decrease in motility of esophagus
Sclerodactyly – thickening and tightening of skin on fingers and hands
Telangiectasia – dilations of capillaries causing red marks on skin surface
*Diagnosis: Anti-centromere antibodies (part of chromosome that links sister chromatids)