Biomed Cardiovascular system ( PART 1)
1/57
Earn XP
Description and Tags
First set of flashcards
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
58 Terms
What is the cardiovascular system?
What is the function of the cardiovascular system?
The cardiovascular system is a closed system of the heart and blood vessels.
heart to vessels - vessels circulate blood to all the body/cells
Functions: transport O2, Delivers Hormones & nutrients, Removes co2 - cells in body
Anatomy of the Heart
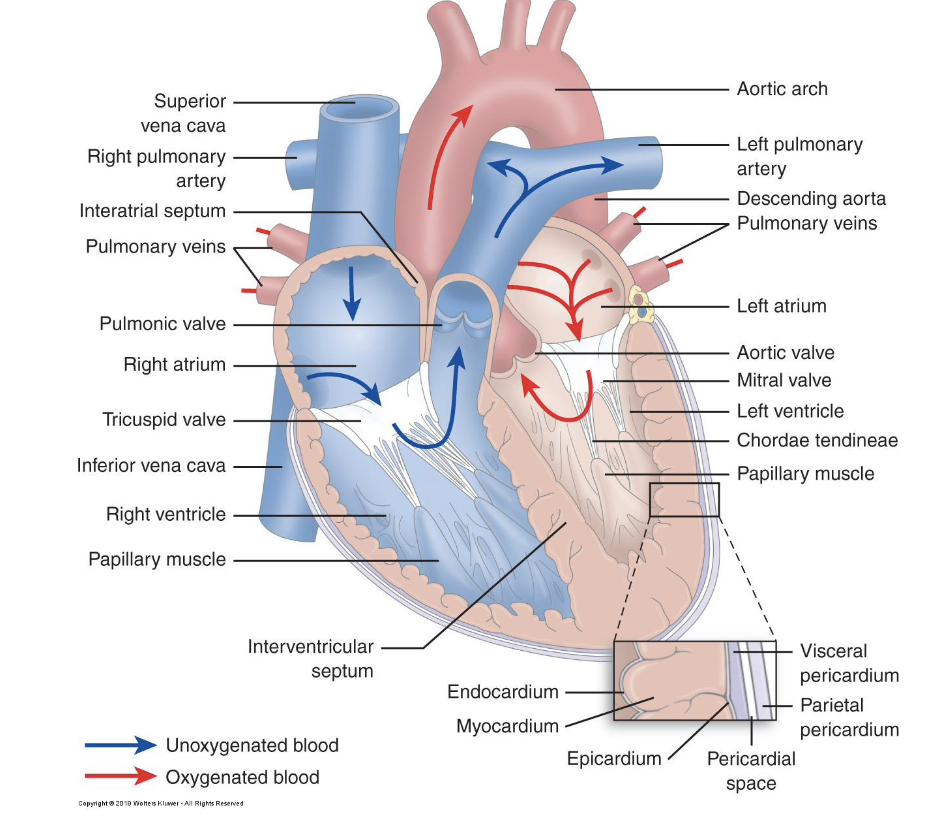
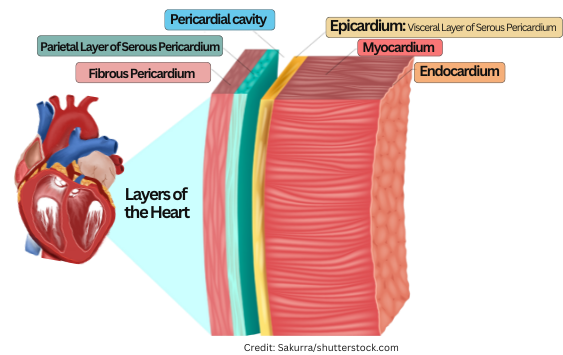
The location and layers of the Heart
Pericardium
Epicardium
Myocardium
Endocardium
Location b/t the lungs and behind the sternum
Pericardium - outer membraneous sac w/lubricating fluid (Pericardial Effusion=Cardiac tamponade)
Epicardium - outside layer of connective tissue on the surface of the heart
Myocardium - the heart muscle with tight interconnective cells of cardiac muscle tissue (muscle don’t want hypertrophy)
Endocardium - the inner epithelial and connective tissue lining of the heart and valves
Layers of the heart
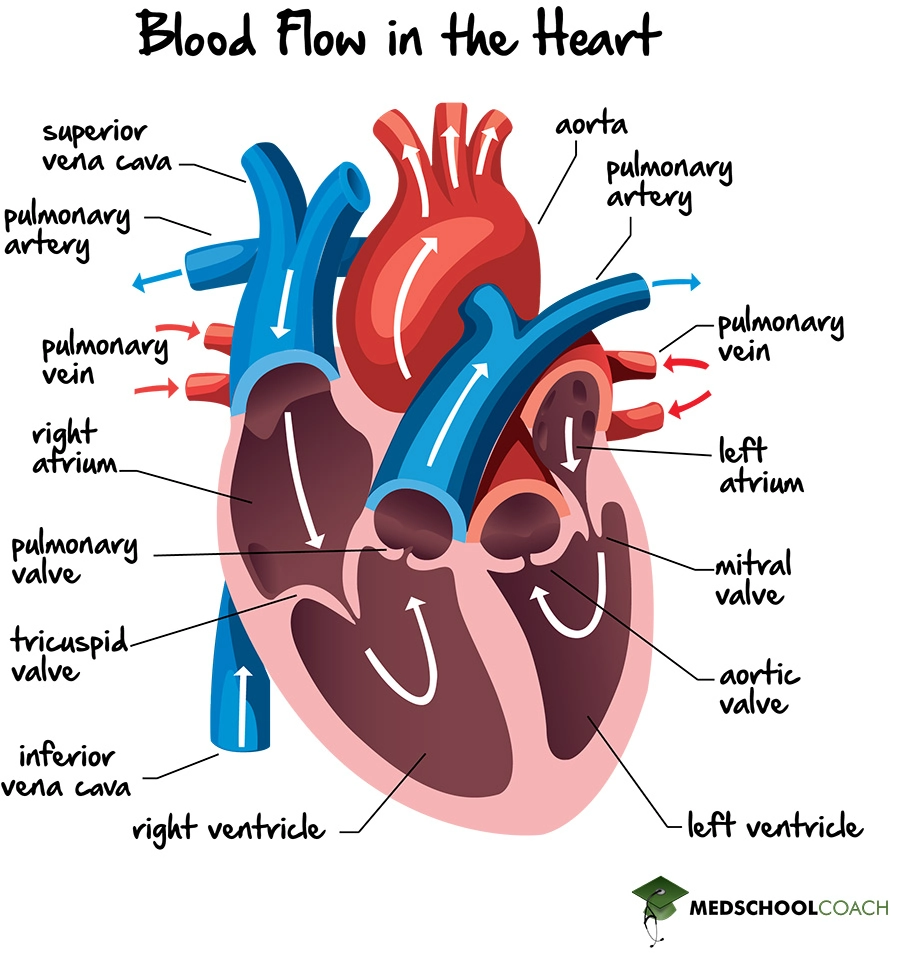
Pathway of the blood in the heart
Superior + Inferior Vena Cava → RA→ tricuspid→ RV→ left + right pulmonary artery→lungs→pulmonary vein→LA→bicuspid→LV→aortic valve→aorta→body
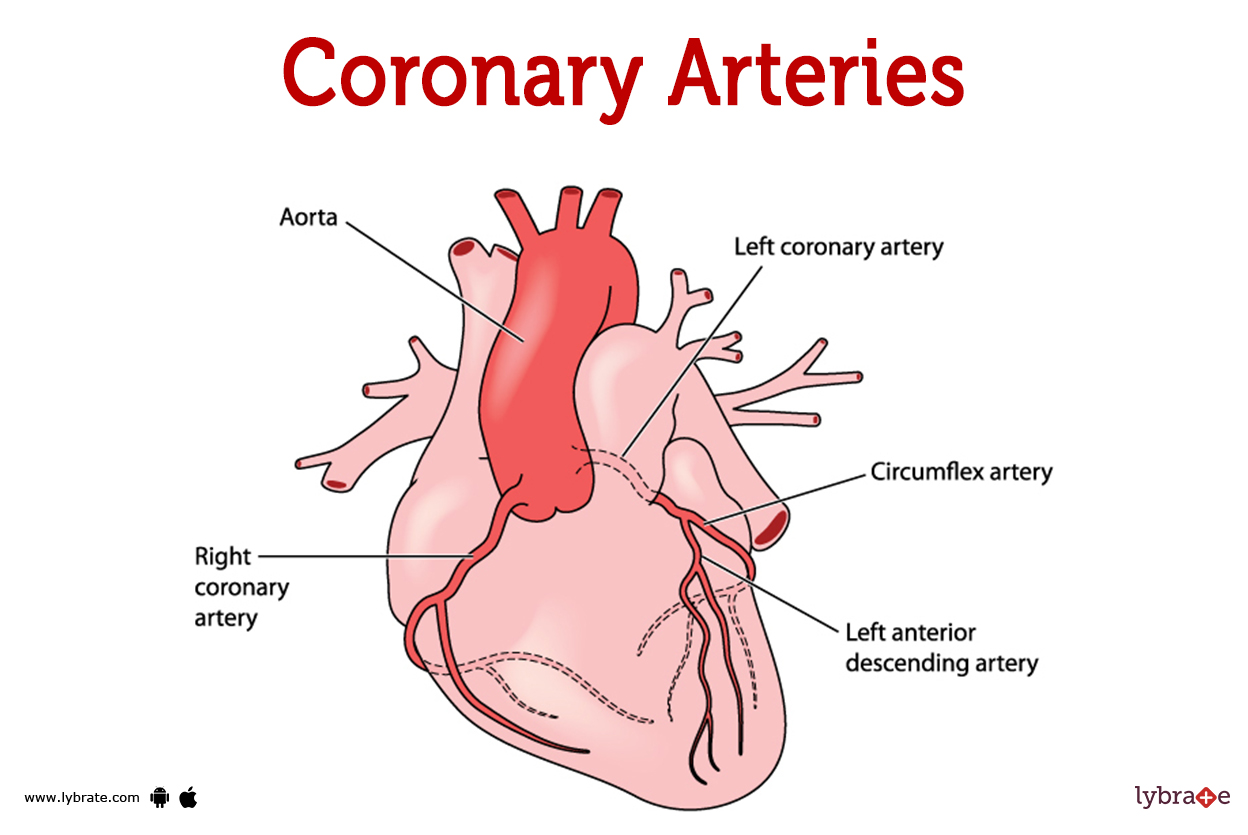
Aorta:
The first set of arteries off the aorta are the coronary arteries→ These arteries supply the heart itself
The heart make up:
4 chambers = 2 upper thin atria/ 2 lower thick ventricles
septum divides the right and left sides
Atrioventricular valves - b/t the atria and ventricles
Tricuspid valve ( Right AV) & Bicuspid/mitral Valve (Left AV)
valves are attached via chordae tendinae attached to muscular projections within ventricles
Semilunar valves are the aortic and pulmonic valves
View of the heart
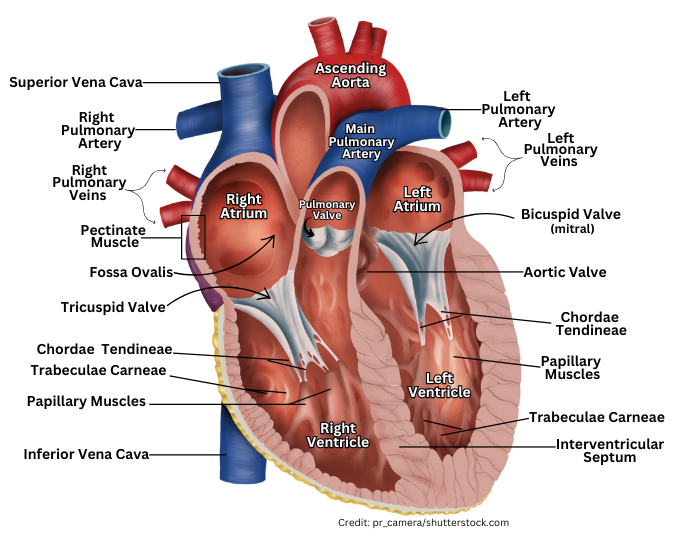
Chambers of the heart
Atria: receiving blood chambers (LA & RA)
Ventricles: Discharging chambers (RV& LV)
LV hypertrophy seen in people with chronic high BP - increasing work the heart to pump the blood out
LV - is also the workhorse of the heart
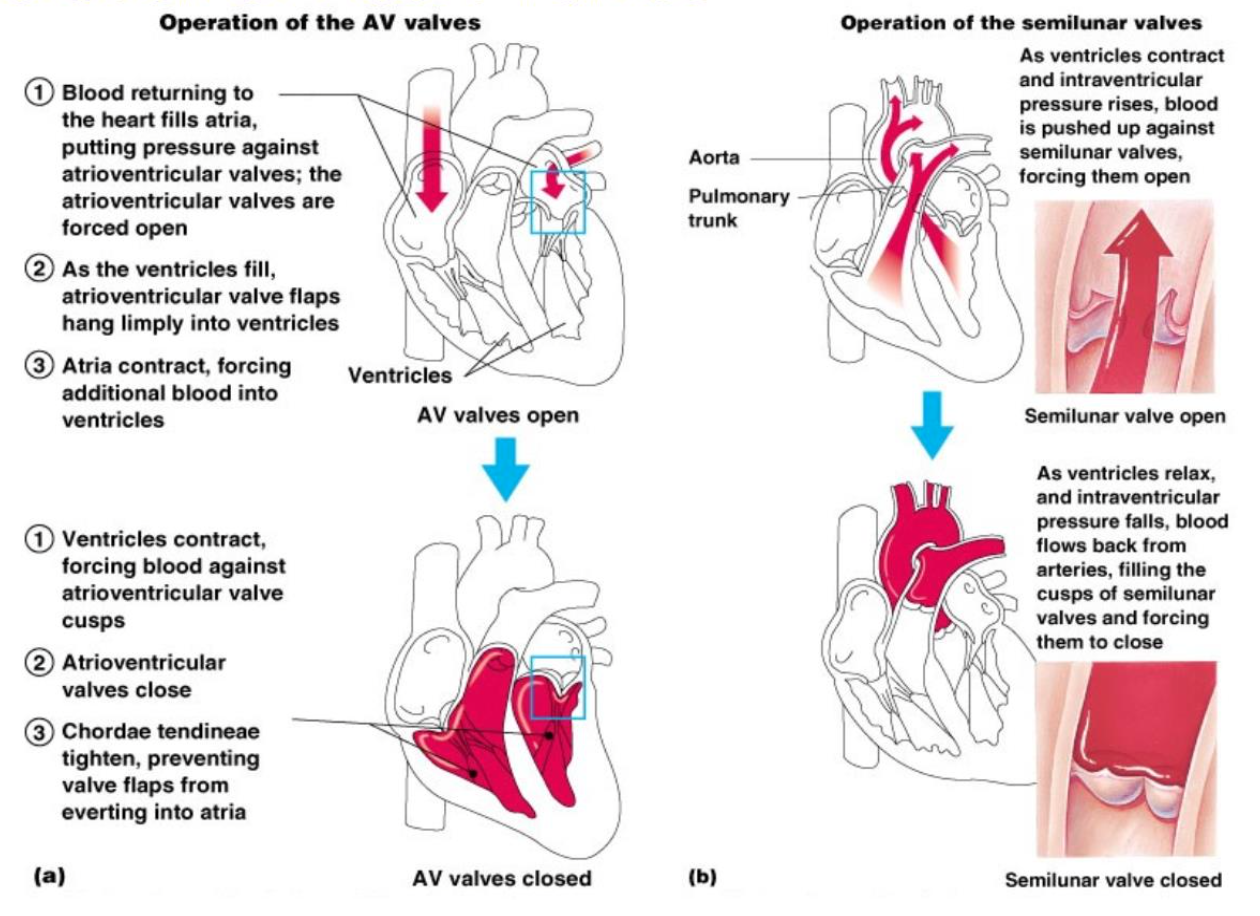
Heart valves
allow blood in one direction - valves open as blood is pumped through
valves close to prevent backflow
4 valves
Atrioventricular: b/w the atria and ventricles
bicuspid valve (mitral) - LAV
Tricuspid valve - RAV
Semilunar valves: Pulmonary & Aortic
Chordea tendinae = anchor + maintain valve stable and shut
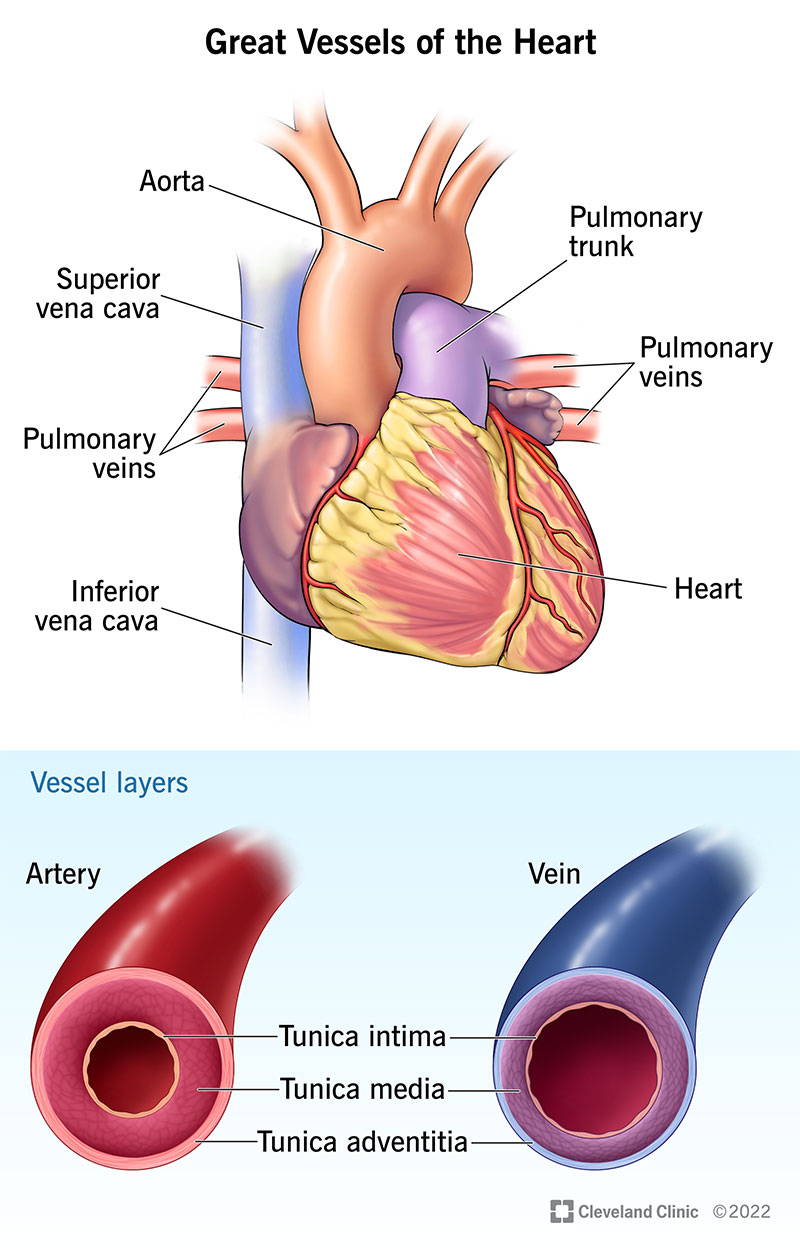
Great vessels of the heart
Aorta - leaves the LV (largest)
Pulmonary arteries - leave the RV (carry deoxygentated blood to the lungs)
Pulmonary veins (4) - oxygenated from lungs
Vena Cava - Superior and Inferior -
SVC syndrome (tumor compression) - impedes lymphatic drainage (edema superior) - veins better at handling edema then arteries
IVC syndrome lower extremity edema
The blood vessels 3 types
Arteries (arterioles) - carry oxygenated blood away from the heart except the pulmonary and some fetal (have higher pressures inside *aorta*)
Capillaries - where nutrients and gas exchange happens
Veins (venules) - carry deoxygenated blood toward heart except pulmonary veins carry oxygen rich blood from lungs to heart
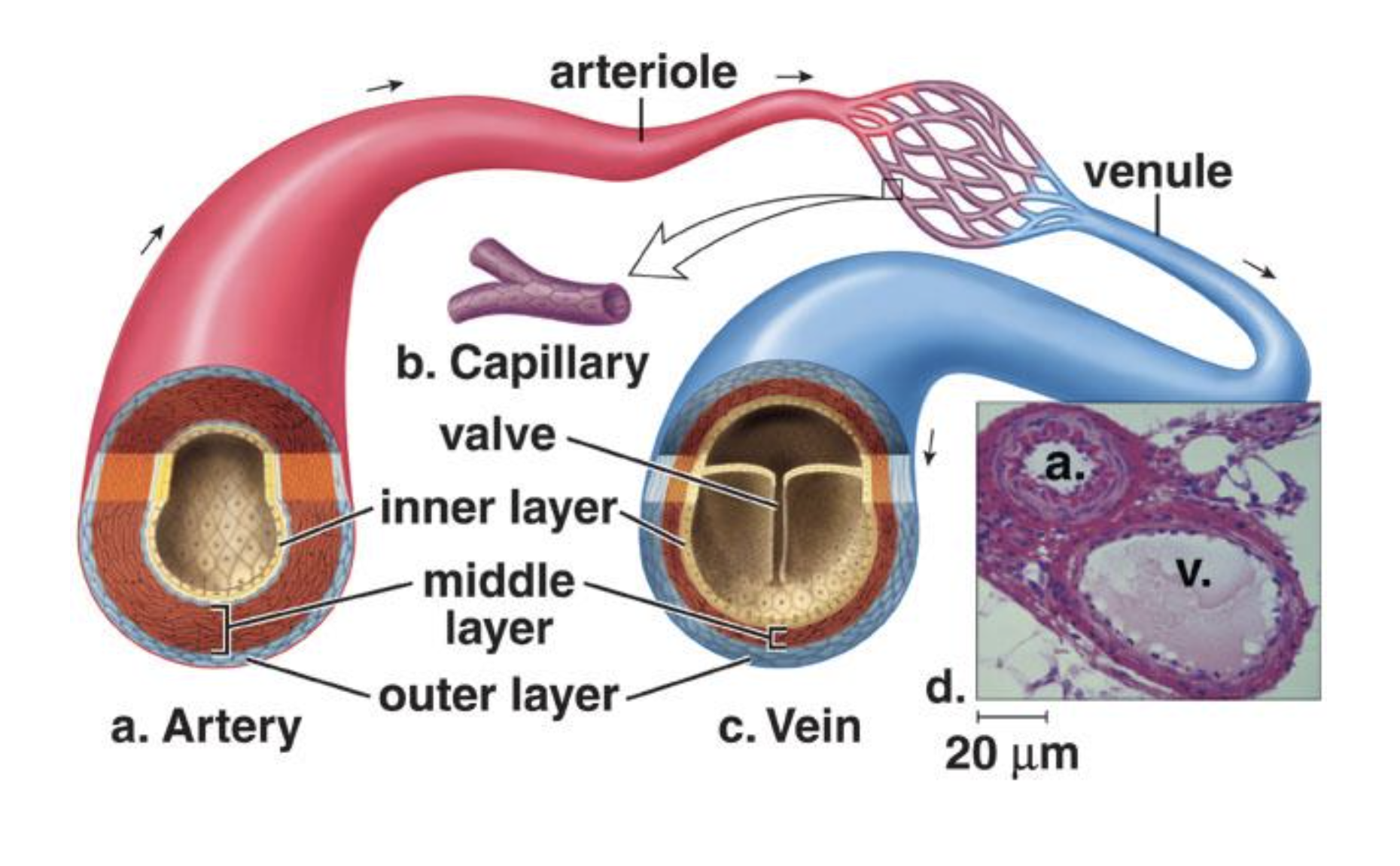
Arteries
Arteries (arterioles) - carry oxygenated blood away from the heart except the pulmonary and some fetal (have higher pressures inside *aorta*)
Smooth muscle → constricts/dilates→based on BP (response to fluid volume/BP)
middle layer of the artery wall is smooth muscle
constricts to regulate blood flow and blood pressure
Arterioles can constrict or dilate, changing blood pressure
Capillaries
-walls are only one cell thick to allow exchange of gases and nutrients with tissue and fluid
-present in all body but capillary beds aren’t open at the same time
-Contraction of a sphincter muscle closes off the bed and blood flows through arteriovenous shunt that bypass the capillary bed
What happens at the capillaries?
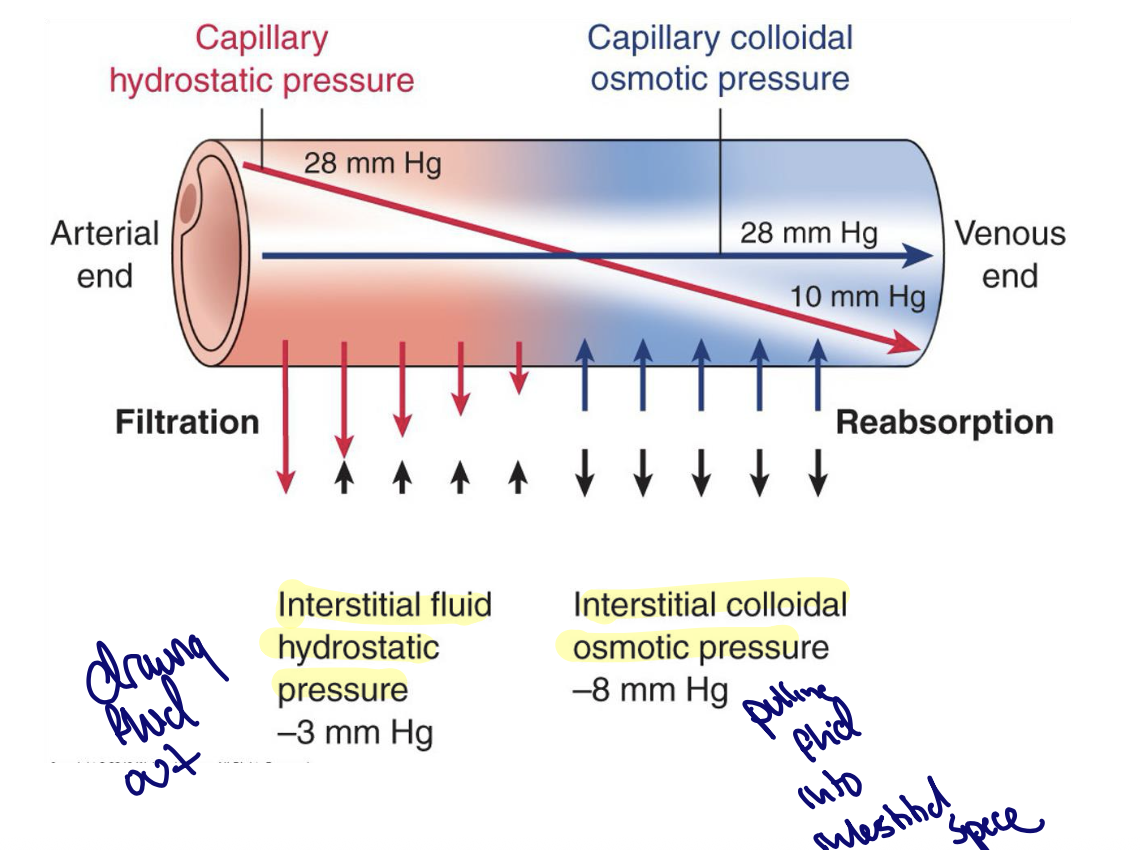
Starling forces govern fluid across a capillary membrane
fluid between the capillaries and interstitial space is balanced by:
Capillary hydrostatic pressure - pushes fluid out (filtration)
Capillary Colloid Osmotic Pressure(CCOP) - pull fluid in w/proteins (reabsorbs)
Also influenced by interstitial pressures: hydrostatic and colloid osmotic
Net effect = the effect of the hydrostatic and the osmotic
@ venous reabsorption because Oncotic>Hydrostatic - why oxygen and nutrients are delivered to tissues from the blood
@arteria ends filtration because Hydrostatic>Oncotic -how waste products and CO2 return to blood stream
Blood flow in the capillaries
Time?
1 cell thick allows for nutrients exchange
Bypassed via AV shunt
Blood moves slowly cuz more capillaries than arterioles
slow movement allows time for substances to be exchanged
Capillary exchange
Renal and Hepatic Circulation are different
What are Veins?
What are there blood flow?
Venules drain blood from capillaries & join to veins and take blood to heart
valves that prevent backward flow
carry 70% of bodies blood and act as reservoir during hemorrhages
Blood flow depends on: skeletal muscle contraction, valves, respiratory movements
compression of veins causes blood to move forward past a valve then prevents backflow
Thoracic and abdominal pressure occur with changes in breathing assist return of blood
inc. pressure = inc. venous function
Issues with Veins
Varicose veins- develop when the valves of veins become weak causing blood to settle out - espicially lower
Hemorrhoids because of varicose veins in the rectum
Phlebitis inflammation of a vein and can lead to blood clots (phlebitis by itslef is okay but inflammation is what leads to clotting) - death if cloth is carried to a pulmonary vessel
remove IV compress suction
Blood under pressure is sent out to the arteries
BP is greatest at the aorta - LV of the heart is thicker than the right because the left pumps blood to the entire body
BP decreases @ the cross-sectional area of the arteries and then arterioles increase
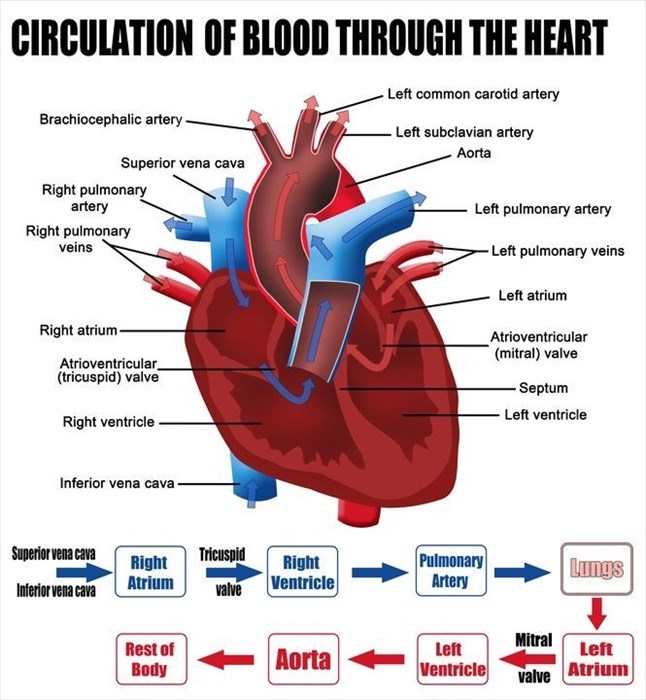
Passage of the blood through the heart *important for exam*
deoxygenated blood is returned from the body into the S&I Vena Cava →RA→tricuspid→RV→pulmonary semilunar valve→pulmonary trunk and arteries to lungs→(oxygenated) pulmonary veins leaving lungs→LA→bicuspid(mitral)→LV→aortic semilunar valve→aorta→body
tricuspid (RA-RV), pulmonary, mitral(LA-RV), aortic
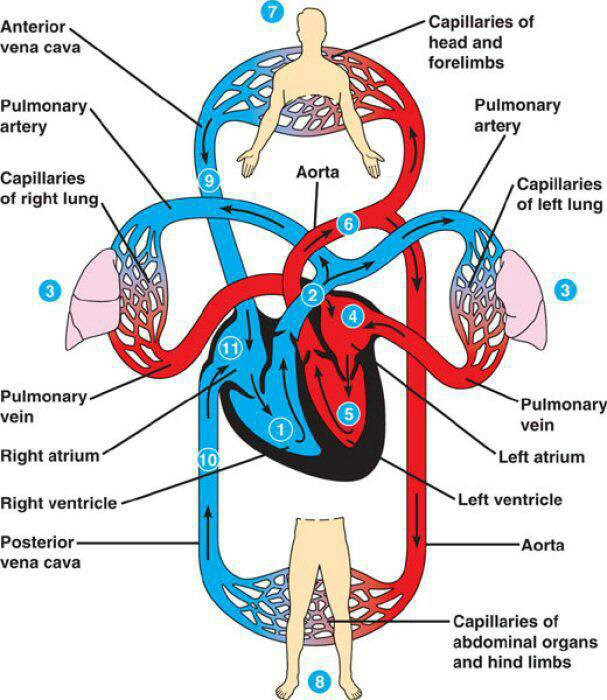
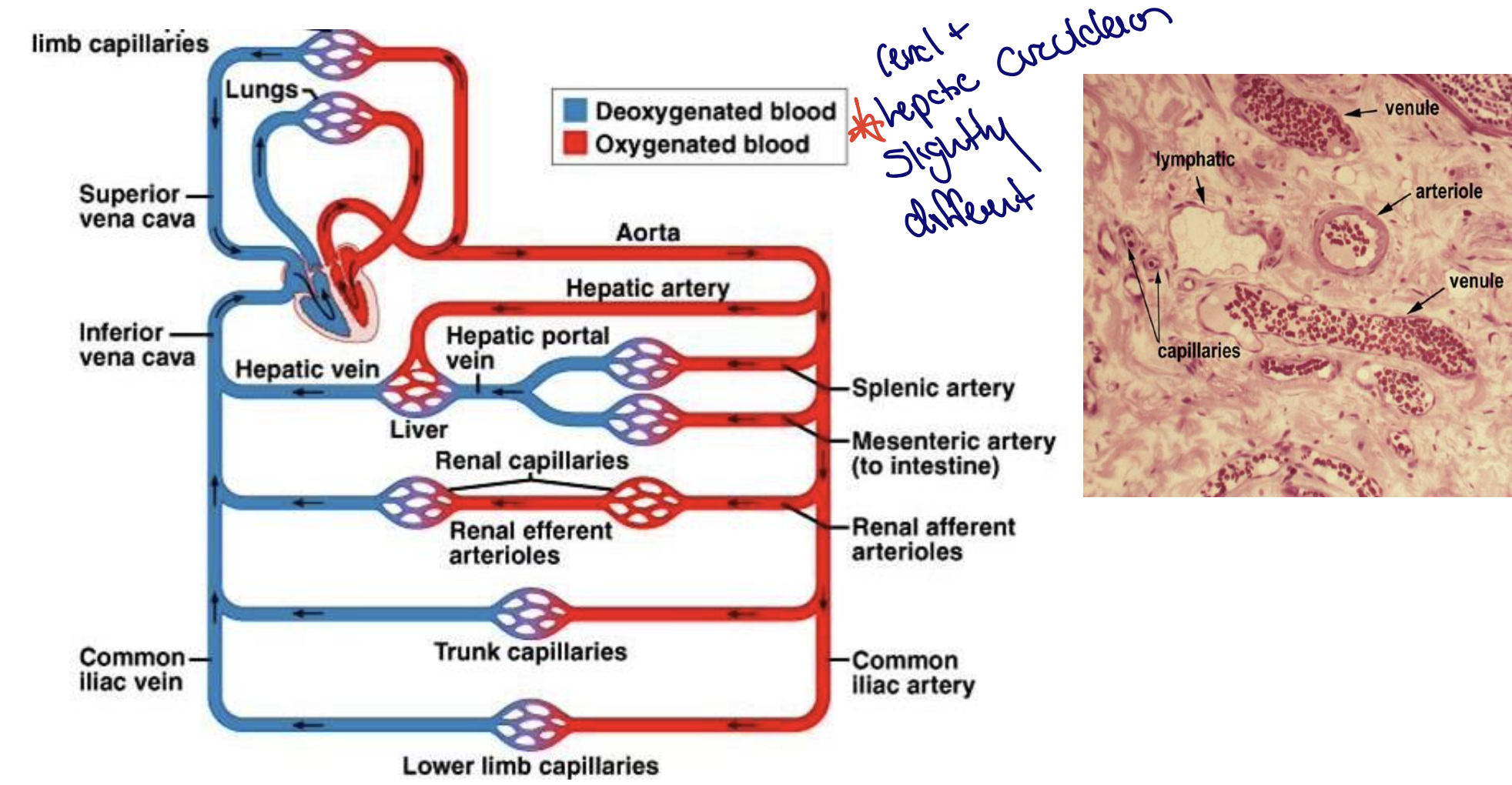
The vascular pathway has 2 circuits maintain homeostasis
pulmonary circuit
systemic circuit
Pulmonary: circulates blood through the lungs
begins with the pulmonary trunk from RV branches into 2 pulmonary arteries (take oxygen-poor blood to the lungs)
lungs oxygen diffuses into the blood and carbon dioxide diffuses out of blood to be expelled through the lungs
4 pulmonary veins return oxygen-rich blood to LA
Adults
arteries carry blood that is high in co2 and low in o2
veins carry blood that is high in o2 and low in co2
why DVT ends up in pulmonary circuit
Systemic: circulates blood through the rest of the body
systemic circuit starts with the aorta carrying O2-rich blood from the LV
aorta branches w/and artery going to each specific organ
artery divides into arterioles and cappilarries which then lead to venule
adults
artreies carry blood that is high in O2 and low in CO2
veins carry bklood that is low in O2 and high in CO@
Arterial embolisms will not end up in pulmonary but rather end up back into the Right heart
Coronary arteries
serve the heart itself - first branch off the aorta
can easily get clogged, leading to heart disease
CAD - plaque build up (atherosclerotic) - plaques can rupshure and occlude vessels and this leads to a heart attack
Hepatic portal system
Carries blood rich in nutrients from (digestion) the small intestine to the liver organ, monitors the composition of blood
Dual Blood supply
receives O2-rich blood from hepatic artery
receives nutrient-rich (no O2) from portal vein from GI Low O2 but high nutrients
Sinusoidal Capillaries (livers)
highly permeable allow for nutrients (proteins, cells) to exchange and more between blood and hepatocytes
Key role in fluid imbalance
liver makes albumin, which maintains oncotic pressure
liver dysfunction= low albuinum = low oncotic pressure =edema
Venous Drainage into systemic circulation:
blood exits hepatic veins to inferior vena cava and return to the heart
liver failure can cause an increase in portal system pressure → Varicose veins in esophagus - inc. build up of blood
heart failure can cause hematensia
heart creates blood pressure to propel blood into the arteries and arterioles
Arterioles lead the capillary to where the exchange with tissues takes place
Blood Flow in the arerioles
Arteries: BP due to the pumping of the heart accounts foe the flow of the blood in the arteries
Systalic pressure is high when the heart expels blood ( ventricular contrcation)
Dystolic pressure is when the heart ventricles relax (vetricular relaxatoion
BP decreases as it gets farther from the LV - becasue blood enters more and more arteries
smaller diameters more smooth muscle - constrict and dilaetes
Blood flow in capillaries
Slow flow = increase gas/nutrient exchange
-a slower movement because more capillaries →allows time for substances to be exchanged between the blood and tissue
Capillaries: DEC BP, DEC velocity, INC Surface Areas
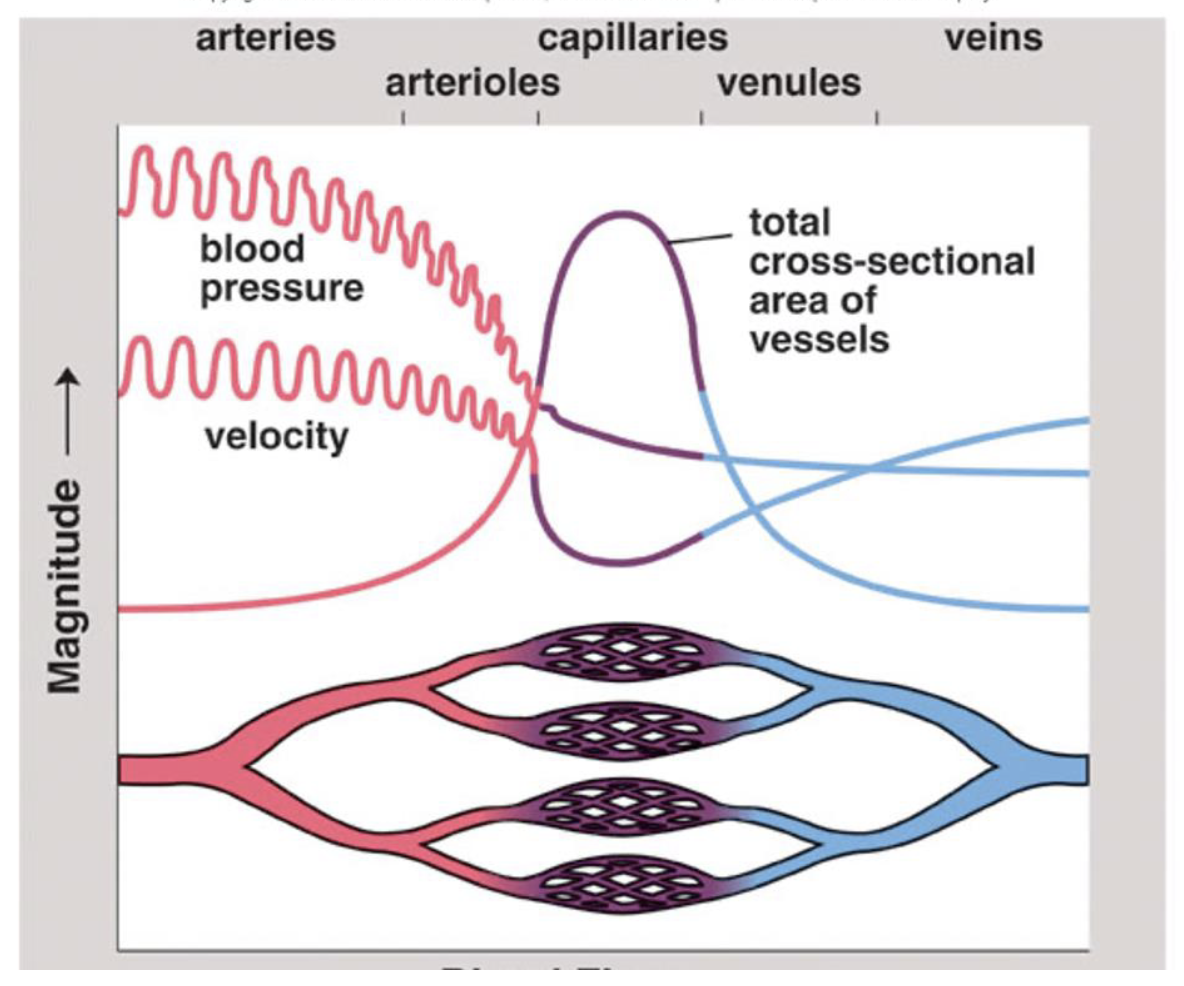
Blood flow in Veins
Lower flow state - there is still pressure form the heart but it is much lower than the arteries
Veins have larger diameters, valves, little smooth muscle
Venous blood flow is more dependent on
skeletal muscle contraction
presence of valves in veins and respiratory movement
Compression of veins causes the blood to move forward papss the valves, and the valves prevent the blood form moving backward - normally
changes in the thoracic and abdominal pressure that occur with breathing also assist in the return of blood
Coronary artery circulation
serve the heart itself - they are the first branch off the aorta
they are susceptible to build up - because of small diameters which can lead to heart diseases
The heart beat - cardiac cycle
S1 and S2
2 atria contract simutanesouly and then 2 ventricles contract and then the heart relaxes
Systole is the contraction
Diastole is their relaxation
S1= AV close
S2= semilunar close
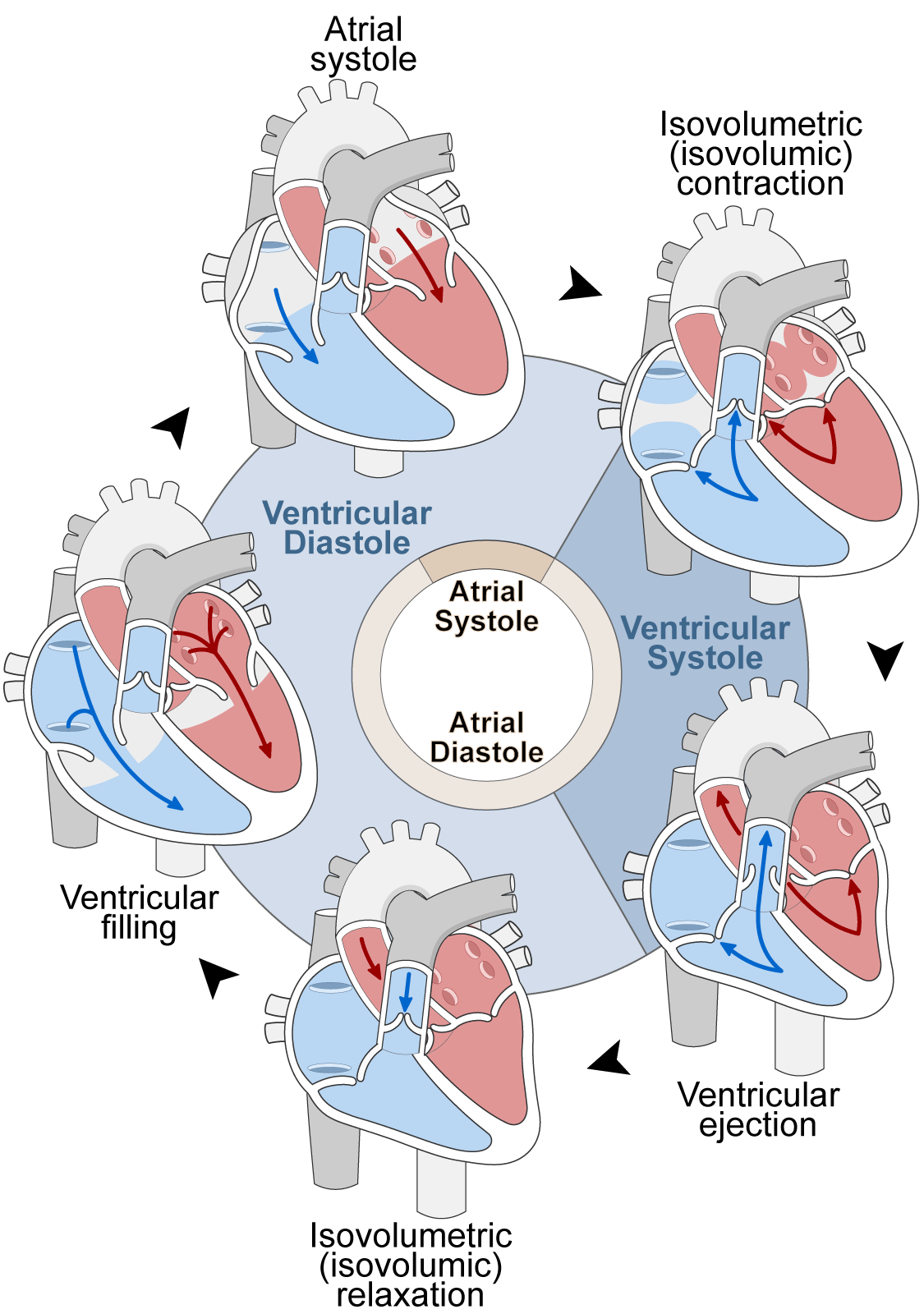
How heart Valves function
pressure builds up in Atria→AV open→blood flow to ventricle, AV close→ ventricles contract→ flow through semilunar valves → semilunar valves close
What is Preload?
What is AfterLoad?
Preload- how full is the heart before it contracts
the stretching of the ventricle as it fills with blood during diastole
degree to which the cardiac muscles are stretching during contraction- the volume in the blood in the ventricles at the end of diastole
the filling phase before its let out
Afterload - pressure the ventricle must overcome to eject blood into the circulatory system during systole ( pumping phase)
inc BP = inc afterload
the wall stress during the contraction and ejection
how hard the heart has to work
resistance the heart must overcome to pump blood out of ventricle
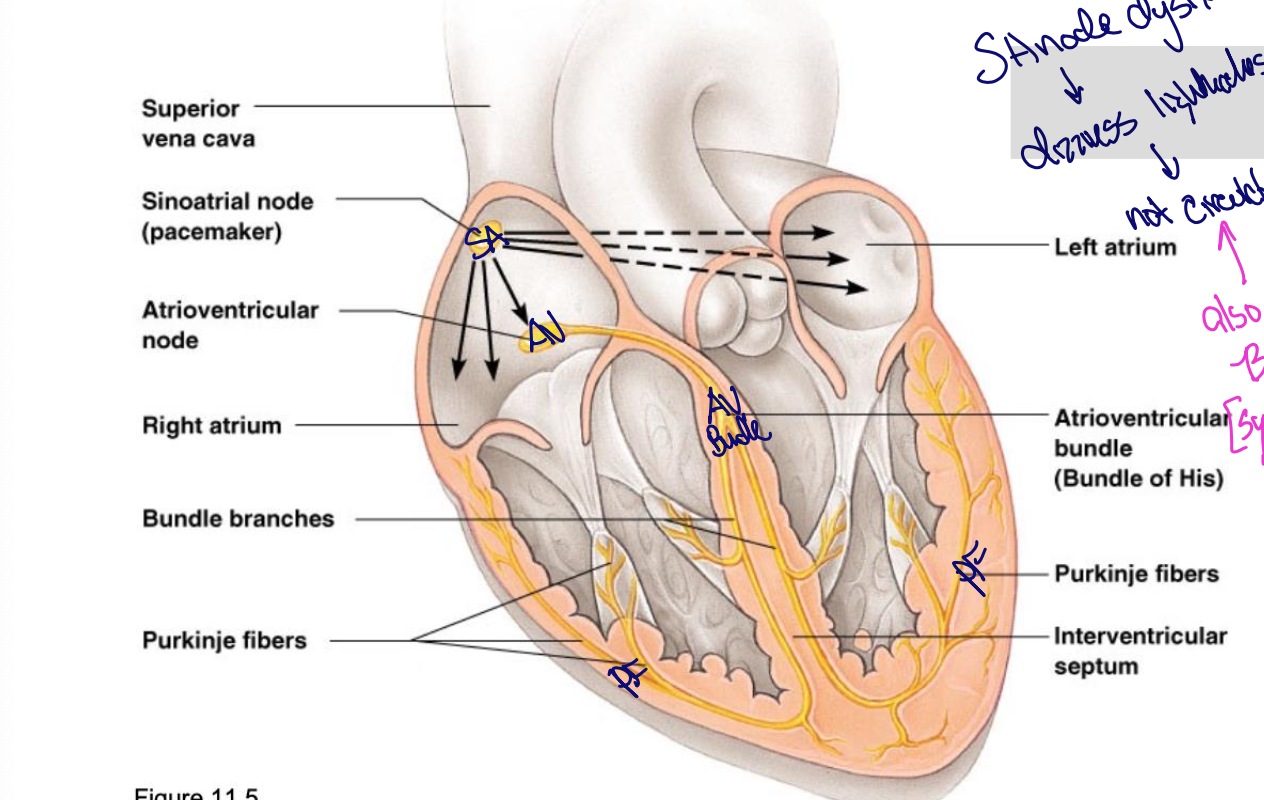
Control of the heartbeat
The SA node (pacemaker) initiates the heartbeat and causes the ATRIA to contract
AV node conveys the stimulus and initiates the contraction of the ventricles
Signal for the ventricles to contract, tables from the AV node through the atrioventricular bundle to the smaller Purkinje fibers
If the SA node fails the AV node will take over, but the contractions will be much slower
SA node →AV node→AV Bundle of His →purkinjee fibers
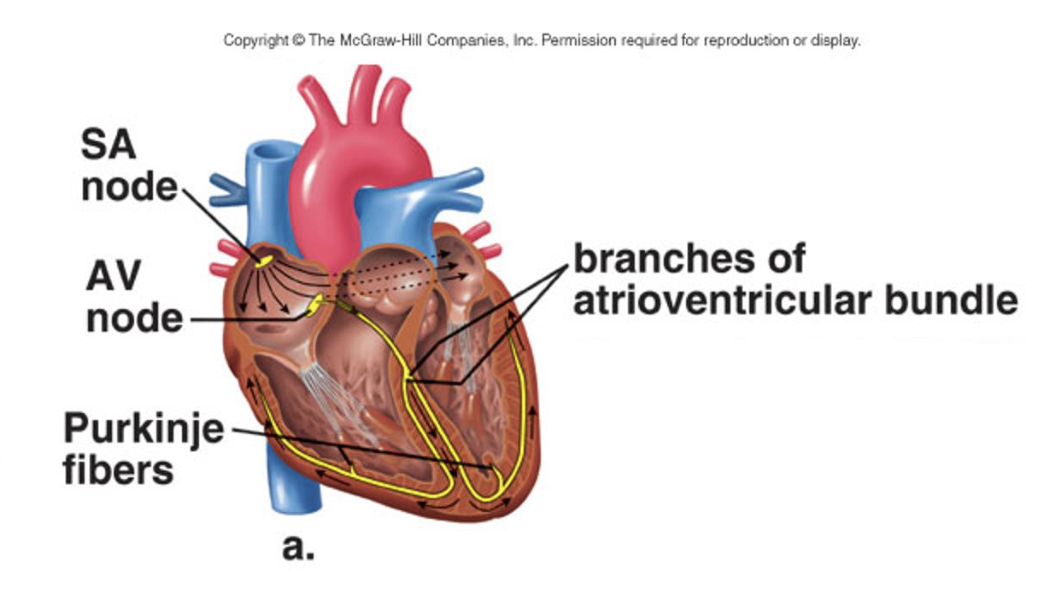
If there is and SA node dysfunction
Dizziness, fatigue, fainting, SOB, no longer circulates volume effectively - also a symptom of B-blockers (symptomatic Bradycardia)
Extrinsic control of the heart
Outside of the heart
a cardiac control center in the medulla oblongata speeds or slows down the heart rate via the Autonomic nervous system: PNS (slows HR) and the SNS (increases the heart rate)
Hormones such as epinephrine and norepinephrine from the adrenal medulla also stimulate faster heart rate
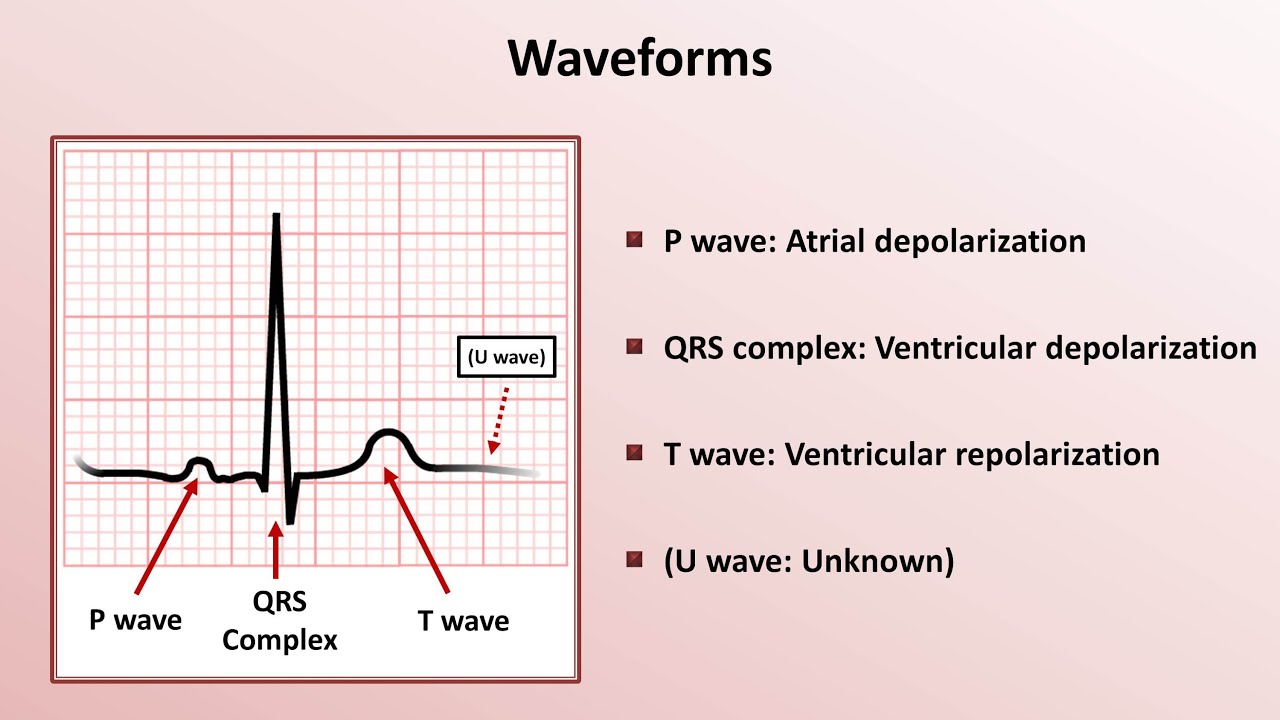
What is and ECG?
a recording of the electrical change that occurs in the myocardium during a cardiac cycle
Atrial depolarization creates the P-wave the ventricular depolarization creates QRS wave, and repolarization of the Ventricles produces the T-wave
graphical recording of hearts electrical activity - deteced via skin electrodes - shows depolarization and repolarization - used for detecting arrhythmias, ishcemias, infractions, electrolyte isues
What does an ECG show
ECG shows electrical activity
atrial depolarization = atrial systole
ventricular depolarization = ventricular systople
EKG/ECG what do each mean
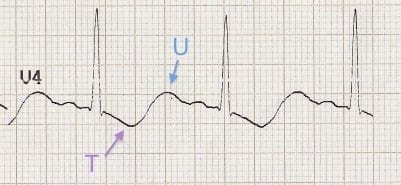
P wave: impulse across atria, atrial depolarization
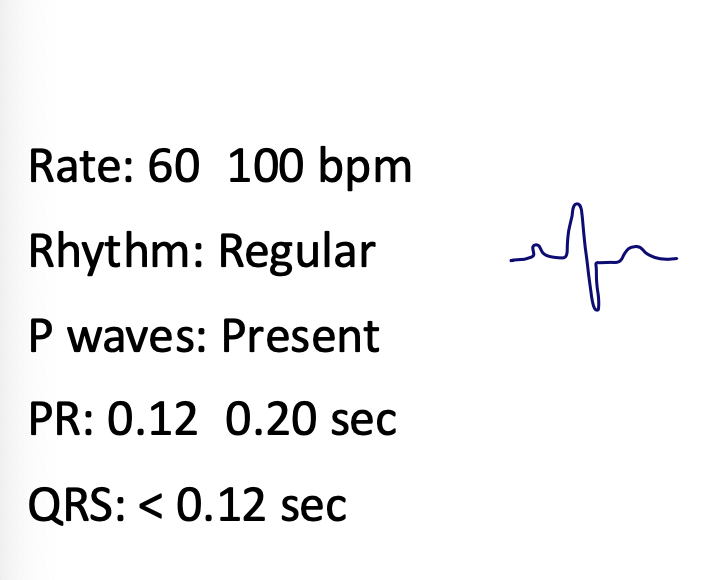
PR: atria to ventricle movement : 0.12- 0.20 sec
QRS complex: spread of impulse down the septum around ventricles in Purkinje; ventricular depolarization <0.12 sec
QT: <0.44 sec (varies with HR)
T: ventricular repolarization
U-wave : late repolarization
Interpret ECG
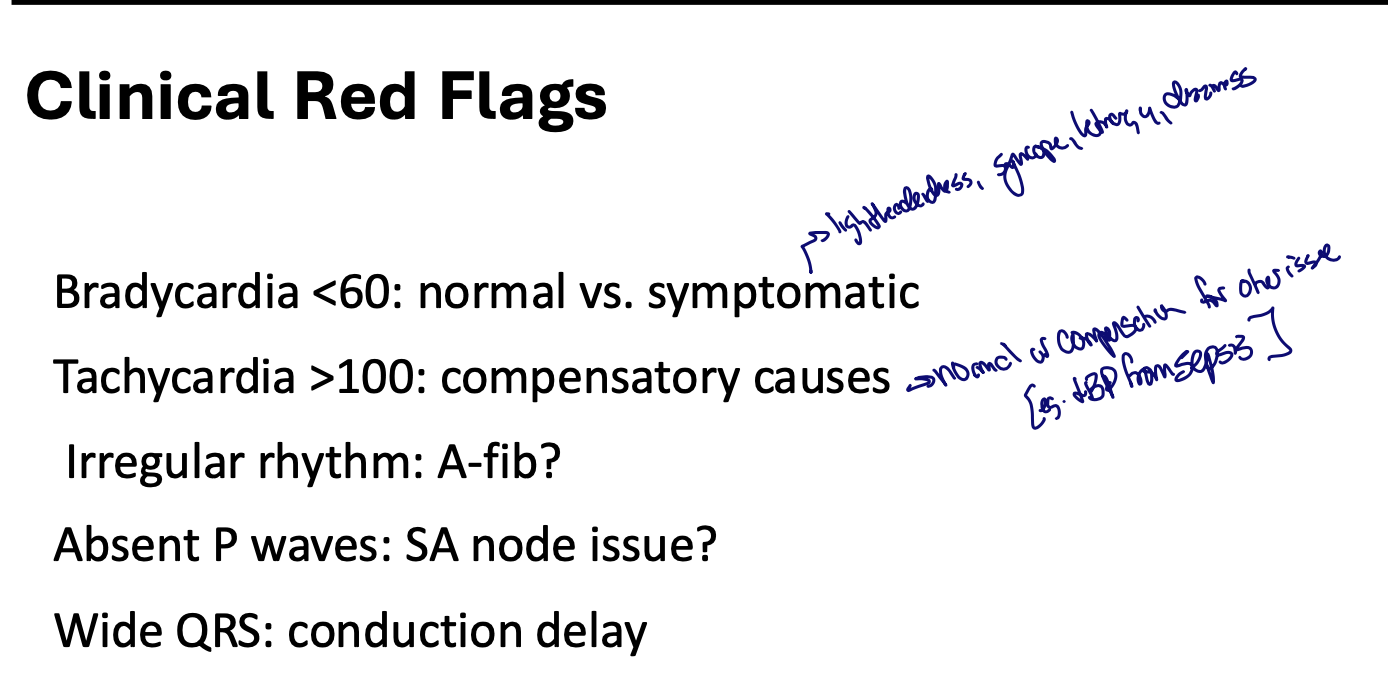
Clinical red flags in EKG
Symptoms for brady: lightheadedness, dizziness, lethargy, SOB,
Symptoms for tachy: normal or compensation for sometheling - with a decrease in blood pressure most likley sepsis - sweating
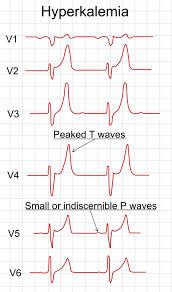
Hyperkalemia
Peaked T-waves and wide QRS (renal dysfunction)
tall peaked T waves - multiple leads
severe hyperkalemia
Hypokalemia
Flat T wave and U wave
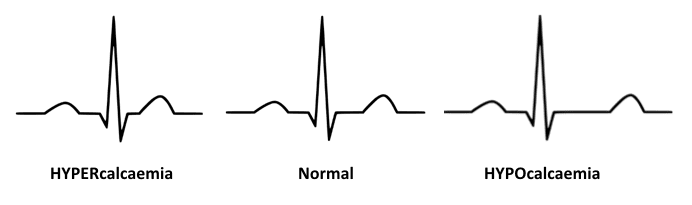
Hypercalcemia and Hypocalcemia
hyper: SHORT QT
hypo: LONG QT wave
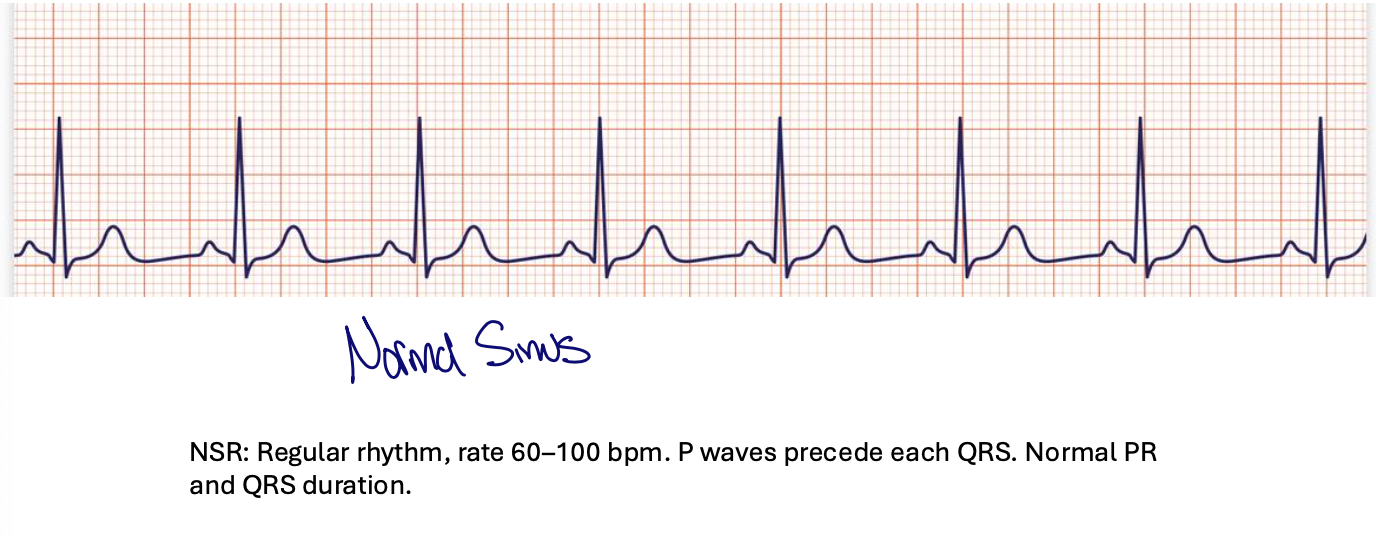
Normal sinus in a ECG
reugular rythym
rate: 60-100 bpm
p waves procede eachh QRS
normal PR and QRS
SINUS brady
Rate: <60 bpm
everything else is normal - common in well conditioned poeple
Can be nromal or systemic

atrial fibrillation
Decreases Cardiac Output
Irregular rhythm no visbile P waves narrow QRS risk for thromboembolism
Usually wide but doenst have to be
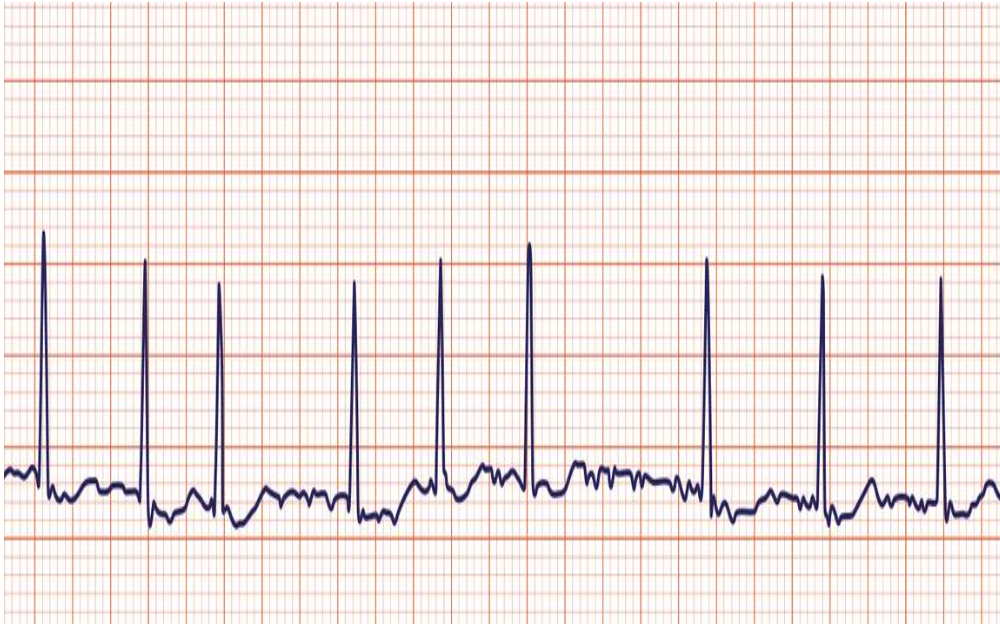
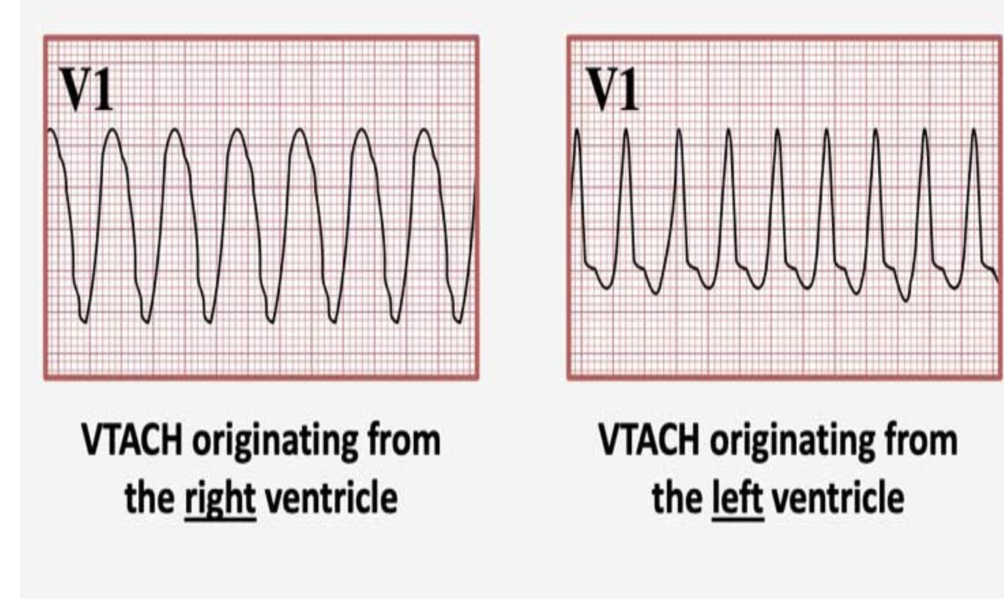
Ventricular tachycardia (Vtach)
Wide QRS
regular rapid rhythm
life thretannig
originates from the right or left ventricle
needs cpr immediatly
Cardiac Output and Stroke Volume
The amount of blood pumped by each side of the heart in one minute
CO= (heart rate) x (stroke volume)
Normal CO= 5-6 L/min
Stroke volume: volume of blood pumped by each ventricle in one contraction - normal stroke volume is 60-100 mL of blood per beat
Examples of Low CO
The heart is not pumping enough blood
CHF, MI, cardiomyopathy (pump)
severe blood loss(hemorrhage) (volume)
Septic shock (pump and volume and vasodilation)
Examples of high Cardiac output
body needs increase blood flow or there is increased vascular resistance
intense exercise and pregnancy as well as conditions such as spesis( initial), severe anemia, hyperthyroidism
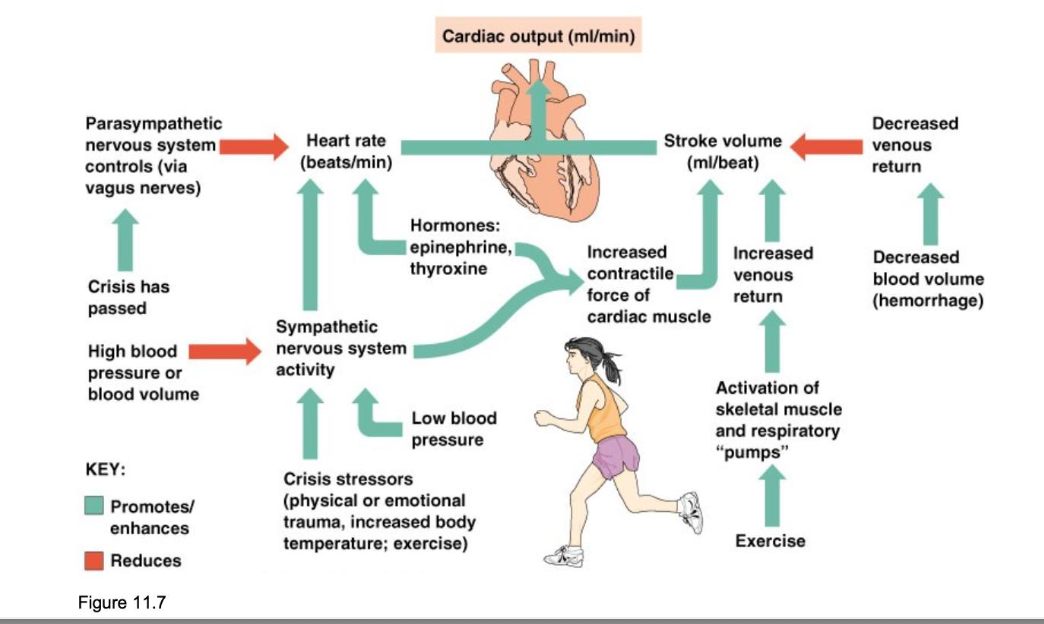
Heart Rate Regulation
How its regulated
Why HR would change
Increased HR
Decreased GR
SV usually remains constant
Starling’s law of the heart: blood fill = stretch = contraction force
This helps the heart match its output to the blood returning to it, a crucial mechanism to maintain adequate blood flow
Changing the heart rate is the best way to change the cardiac output - NOT SV
Increased heart rate
SNS (crisis or low BP)
hormones (epinephrine or Thryoxine T3 or T4)
Exercise
Decreased blood volume
Hypotension or hypovolemia
Decreased heart rate
parasymathetic nervous syten
high BP (hypertension) high blood volume (hypervolemia)
decreased venous return - associated with hypovolemia
medication
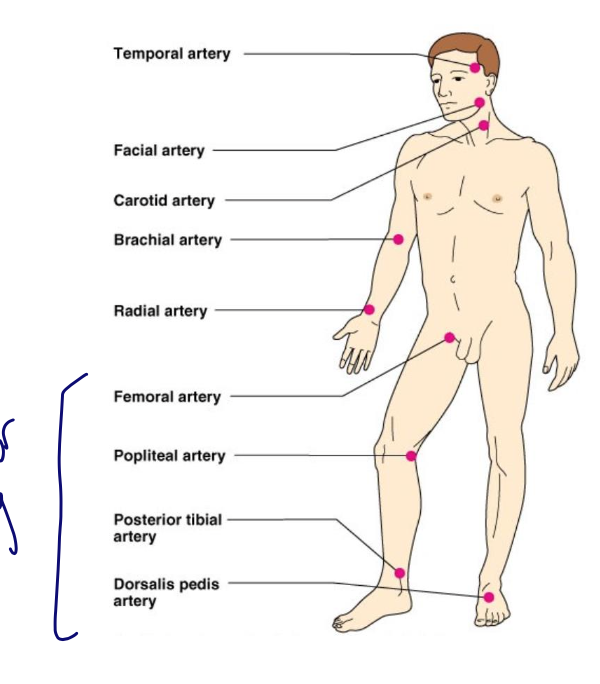
Vital signs to messure
Pulse (arterial) - pulse pressure wave of blood
monitored at pressure points where pulse can be palpated
certain arteries are used for assessing PAD - femoral, polietal, tibial, dorsialias
Blood pressure: the pressure of larger arteries
Resipitory rate
Body temperature
all indicative of the efficiney of a system
Blood pressure: on pressure of larger arteries
systolic pressure at the peak of ventricular contraction
diastolic pressure when the ventricles relax
pressure in blood vessels decreases as the distance away from the heart increases
L. Brachial artery relaxed best levels of the heart
Foremarm and ankle
Factors affect BP
Neural
ANS (sympathtic)
SNS inc SA node, Vasocuntsictioun = increase in contraction force
PNS= DEC HR + BP
renal
regulate by altering blood volume
renin - hormonal control
temperature
heat has a vasodilatation effect = decrease in BP
Cold has a vasoconstriction effect increases BP
checmical and med
Diets - High NA
Variations of BP
Normal: sys(110-140) and dys(60-80)
Hypotension: low systolic less than 110 and its usual illness- important to know patient’s baseline
Hypertension, high systolic 140 above can be dangerous if chronic
hypertensive emegeyc above 180 and dys above 100
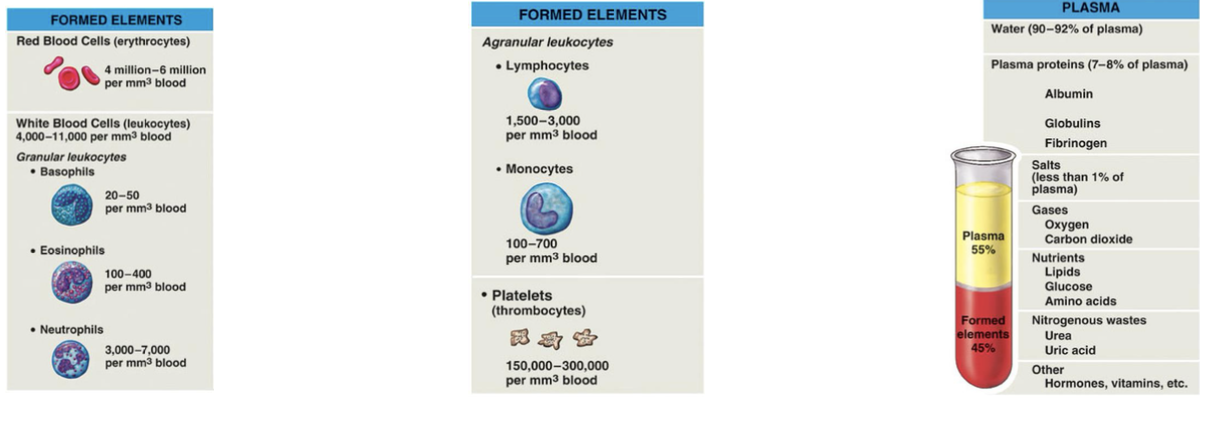
Blood basics what is blood?
Specialized CONNECTIVE TISSUE
Functions: transport regulation, protection
usually 5 liters in average adult
Sustain life cardiovasculr system
Plasma
Makes up about 55% Blood volume
key proteins: albumin (oncotic pressure) + fibronogen (clotting) + globulins (immune functions)
Cellular compensate of blood
Cardiovascular blood health
RBC: contain hemoglobin and carry oxygen and most abundant in the blood
WBC: immune defense,
Platelets (thrombocytes: fragmented cells that initiate blood clotting
CBC with differentiation helps identify the kinds of WBC and
Perfusion requires adequate BV + plasm proteins and platets and clotting factors
disruptions impact CO and tissue oxygenation
Cardiac Labs
Troponin: releases in response to herat damadge or high stress
normal less .04
if tested 12 -24 hours later after a heart attack, you will see heart damage and an increased level
MI if elevated
BNP: <100
CHF if elevated - disguising fluid bc of atrial stretch
CK-MB; creatain kinase myocardial bond = increases heart damage and injury loss
<5
cardiac damage marker if higher
Potassium: 3,5-5.5
dysrhythmias if potassium is elevated
Magnesium 1.5-2.5
torsades if low
creates dysrhythmias
Tropinist & CKMB are intracellular- if they are found in blood it means that the heart has been damdged