medical microbio-MODULE 9. GRAM NEGATIVE COCCI (GNC)
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
36 Terms
Classify the genus Neisseria on the basis of:
a. Morphology
b. Staining reaction
c. Cultural requirements: growth optimum temp, CO2 req, suseptible to changes in what
enriched media used (2 antibiotics names and why needed)
a. Morphology: Kidney bean shaped Gram-negative diplococci
b. Staining reaction: gram neg
c. Cultural requirements: Fastidious bacteria but will grow if optimized for temperature at 37° C and if enhanced by 2 to 8% CO2
pathogenic strains will not grow below 25° C or room temp
are quite sensitive to cold temperatures and will die for refrigerated or sample is plated onto media just removed from the refrigerator
Incubator with CO2 filled as a chamber from external Source or candle Extinction jar is often used
highly susceptible to adverse conditions such as drying, chilling, sunlight, pH extremes
Of utmost importance there must be minimal to no delay of culture of samples after collection
Enriched media is required: chocolate agar ( blood agar that has been heated to humalyze rbc, free hemoglobin contains Fe which require is required for growth) or chocolate agar-based media
commonly used media for isolates of pathogenic neisseria is Taylor Martin (TM) agar→ Chocolate-based agar with some antimicrobics added as in VCN agar which is another similar concept that only allows pathogenic bacteria to grow
VCN agar→Chocolate agar modified by addition of antibiotics: Vancomycin to inhibit gram-positive bacteria, colistin to inhibit gram-negative bacteria rods, nystatin to inhibit yeast
Biochemical reactions: Critical criteria of neisseria
media
gram stain
oxidase
CTA
moraella catarrhalis difference from neisseria
growth on media specific for pathogenic strains of neisseria such as ™/ thayer martin agar and VCN agar
gram stain=kidney bean shaped Gram-negative diplococci
Oxidase production= indicates presence of cytochrome oxidase which in the reduced state, the reagent is colorless/ oxidase negative; in the oxidized state, the reagent is dark purple / oxidase positive therefore patient has neisseria
CTA (cystine tryptic agar) sugars to differentiate neisseria species
Yellow color due to acid production of metabolism os sugar = positive, red is negative
If only glucose pos→gonorrhoeae
If glucose and maltose pos→meningitis
Moraella catarrhalis is all neg even though other biochem reactions are all same to neisseria
For laboratory diagnosis of pathogenic Neisseria, outline the three definitive criteria for diagnosis and the final biochemical tests done to complete the identification.
To find if pathogenic neisseria (genus): 1. Grow on VCN or TM agar, 2. Gram neg diplococci, 3. Oxidase positive 4–(species). CTA sugar test
N. meningitis and N. gonorrhoeae are genetically ____ but clinically manifest…
N. meningitis and N. gonorrhoeae are genetically similar but clinically manifest very diff
Gonorrhea is caustve agent of what
most prevalent of the ____ diseases
__% occur in aldolescnets
____to the CDC
Causative agent of gonorrhea,
most prevalent of the classical venereal diseases;
33% of all infections occur in adolescence,
continues to be one of the most commonly diagnosed infections that is reportable to the CDC
Meningitidis
infection of (3) body parts and cause of what disease
effects of this worldwide
beyond perinatal period, commonly transmitted how
major causes of bac meingitis (2 important) and in kids (1 important)
what does this overall mean in lab/clinic
is an infection of the membrane, the meninges, and CSF surrounding the brain and spinal cord;
is a major cause of death and disability worldwide.
Beyond the perinatal period, bacteria commonly transmitted from person to person through exchange of respiratory secretions are responsible for most cases of bacterial meningitis
Causative agent of meningococcal meningitis, which has the potential to occur as epidemics
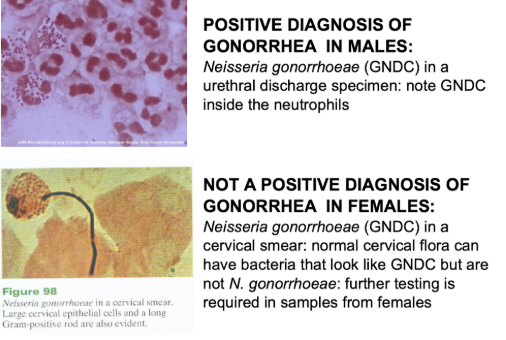
Major causes of bacterial meningitis in adults are streptococcus pneumoniae which is a gram positive diplococcus, neisseria meningitis which is a gram-negative diplococcus, hemophilus influenza which is a small gram negative rod;
Major causes of bacterial meningitis in newborns and children are streptococcus agalactidae which is Group B strep that is a gram positive coccus, listeria monocytogenes which is a gram-positive rod=>All to say that gram stain results determine what a disease could be within minutes so that way the first antibiotic can be administered
procedure if CSF is suspected of contam of meningitis
additional causes of meningitis
why important to know causative agent
When CSF comes in and suspected of contamination of meningitis, made stat
Spinal fluid tap collection to get CSF From between the subarachnoid space and Pia matter
Additional causes of meningitis are viruses, fungi and yeasts, and parasites as well so pretty much any microbe
knowing the cause is important because severity of disease can be different, and treatment of illness can be different as determined by the patient's age, patience immune status, bacterial route of transmission
other species of Neisseria relative pathogenicity and location (2)
There are other species of Neisseria In humans, most are considered non-pathogenic and are part of the normal flora of the upper respiratory tract and other mucosal surfaces
Ex) path to ID N.gonorhoeae—4 steps
Gram neg diplococci on gram stain
Growth on media specific for neisseria (chocolate or TM/VCN media)
Oxidase positive (purple)
CTA sugars shows only glucose positive
only known natural reservoir of pathogenic neisseria is
humans
Clinical infection occurrence and transmission of N. meningitis
Peak occurrence of disease in children
only known reservoir—> and carrier
spread how
pop at risk
Is worldwide and varies between sporadic cases and epidemic cases
Peak occurrence of disease in children from 6 to 24 months of age
human nasopharynx is the only known reservoir
adult nasopharyngeal carrier
meningococci spread from person to person by Airborne droplets of infected nasopharyngeal secretions
others at risk are the military or those in boarding institutions / individuals living in close proximity to each other
Clinical infection and occurrence of N. gonorrhoeae
pathological determinant
natural host
most common disease of what and how many cases reported/ age group
The presence of pili on virulent forms seems to be the only pathologic determinant
Humans are the only natural host (as with whole genus)
Is world wide and most common classic vernal disease with 1 mil cases reported annually
Disease is most common in indiv 20-24 yr
Transmission N. gonorrhoeae: (adults and newborns)
most common transmission is by sexual contact
Newborn infants can become infected during passage through the birth canal
N. meningitis portal of entry
where do infections usually stop —>what does this mean for patient
what if infection proceeds (incubation time and mech of spread)—>symptoms
body locations (3)
Invasion: Meningococci enter the body via the upper respiratory tract and establish themselves in the membrane
most infection stop in the nasopharynx and the outcome of the host becomes an asymptomatic carrier
if the infection precedes, and incubation period is a few days, mangococci are spread via the bloodstream / septicemia, which results in metastatic lesions in various areas like the skin, meninges, and eyes
N. gonorrhoeae Invasion: primary infection begins where
other possible portals (4)
Primary infection usually begins at the epithelium of the urethra
Cervix, conjunctiva, rectal and pharyngeal mucosa may also serve as portals of entry
Morbidity and mortality N. meningitis:
death rate (developed and developing countries)
% left with disability
3 types of disabilities
On an annual basis, 1 million cases of bacterial meningitis occurs globally and 200,000 of these die
case fatality rates vary with age of patient and time of illness and strain of bacterium causing infection
case fatality rates are 3 to 19% and developed countries and higher in developing countries with fatality rates of 37 to 60%
up to 54% of survivors are left with a disability due to The Infection Colon deafness, intellectual disabilities, neurological sequelae
Determinants of N. meningitidis pathogenicity: (2)
Capsule: Contribute to the invasive properties of the meningococci, inhibits phagocytosis
endotoxin from the gram-negative cell wall which has LPS
Is released when cell dies, especially Gram-negative
is responsible for the extensive vascular damage that is a component of the disease process
while many gram negative bacteria produce endotoxin, the levels produced by meningococcal bacteria are 100 to 1,000 times greater than normal
endotoxin targets the heart, affecting its ability to pump; and no toxin also causes blood vessel leakage throughout the body, as every vessel starts to hemorrhage, major organs like the lungs kidneys and adrenals are damaged and eventually destroyed
Symptoms of N. meningitis:
slight, moderate, severe (emboli meaning)
6 infections accompanying severe symps
waterhouse-friderichsen syndrome
Vary from slight to moderate to severe
slight = mild febrile disease that can be accompanied by pharyngitis
Moderate = systemic disease characterized by fever, exhaustion
severe= Abrupt onset, headache, stiff neck, fever, petechial eruptions or pinpoint hemorrhages developing into larger Hemorrhage areas causing emboli of mangococci
emboli= a mass, such as a clump of bacteria or detached blood clot, foreign material like air bolus, that travels through the bloodstream and lodges and blood vessels, blocking it
Severe may be accompanied by:
Meningitis– inflammation of the meninges / membranes that envelop the brain and spinal cord
Septecemia– bacterial infection of the blood
Arthritis– inflammation of the joints
pericarditis– inflammation of membranes surrounding the heart
Involvement of any organ system is possible
may cause disseminated intravascular coagulation (DIC) followed by death as rapidly as one hour from onset of symptoms
Or waterhouse-friderichsen syndrome (adrenal gland involvement)
Complications N. meningitidis—mortality rate of treated vs untreated
after effects (5)
Mortality is 85% if left untreated, 10% if treated early
Time is of the essence
Some patients may survive meningococcal meningitis with no after affects
Others may have lifelong pathologies such as deafness, CNS damage, necrosis of large areas of tissue requiring grafts, amputation, blindness
Pathogenesis of N. gonorrhoeae
Invasion: primary infection portals of entery and —>human response (what becomes obstructed and why)
Primary infection begins at portal of entry (epithelium of the urethra, cervix, conjunctiva, rectal and pharyngeal mucosa)
Result of infection is inflammatory response with dense infiltration of neutrophils
In some individuals, ducts and glands become obstructed by the cellular exudate forming cysts or abscesses
N. gonorrhoeae effects on males (% aquire, incubation, % asymp, complications-4- and symp), females (% asymp, 4 symp, complication and 2 mech of this), children (3 infections)
Males:
During unprotected intercourse–25% chance of acquiring gonorrhea from infected indiv (dec w/ condom use)
Incubates for 2-7 days
10% remain asymptomatic, others present with burning on urination and yellow pus discharge
Complications include urethral stricture (narrowing of urethral tube), prostatitis, sterility, occlusion of vas deferens with scar tissue
Females:
20-80% may be asymptomatic
Symptoms include burning or freq urination, vaginal discharge, fever, abdominal pain
Complications include PID (pelvic inflammatory disease) resulting from ascending infection w/ fallopian tubes and ovaries
This type of infection is a major cause of sterility by 2 mech:
Scar tissue causes partial obstruction of fallopian tubes such that fertilized ovum becomes trapped causing ectopic preg (doesn’t go to full term)
Scar tissue completely closes off lumen of fallopian tubes
Children 3 infects:
gonococcal ophthalmia neonatorum
Neonatal gonococcal arthritis
Gonorrheal vulvovaginitis
N. meningitis immunity
antibodies aquired how and rel amt of defense of adults vs children (what age is most at risk)
how do kids and adults aquire antibodies
Antibodies present in the blood of very young infants is presumably acquired through the placenta
the lowest antibody titer present in infants is those between the age of 6 and 24 months due to loss of antibody provided passively by mother and inability / immature ability to make their own antibodies
Adults have moderate immunity and antibody titers develop during the carrier state
treatment N. meningitidis and gonorroheae
N. meningitidis:
For many years penicillin. Now dual therapy of azithromycin and ceftriaxone
N. gonorrhoeae
Usually penicillin, however new resistance emerging with beta-lactamase positive
prevention N. meningitidis: (2)
what is used during epidemics to eradicate carrier state—why
what is used for close contacts
how are vaccines made (2) in relation to seriotypes
what group meningococci are only modestly effective
Antimicrobial prophylaxis
Rifampin is used during epidemics to eradicate the carrier state (adult nasopharyngeal colonization)
Rifampin remains the drug of choice for prevention due to low cost, ease of admin, and well established record among infants/children
Rec is for chemoprophylaxis of household members and other close contacts of persons w/ invasive meningococcal disease
Immunization
Immunity following meningococcal infection is serogroup specific
Internationally marketed meningococcal vaccines are based on combos of group specific capsular polysaccharides (A and C serotypes for eg) or conjugates between group C specific polysaccharide and a protein carrier
Polysaccharide vaccines are safe and highly immunogenic
Vaccines currently on market against group B meningococci have shown only modest efficacy in children and adults
Commonly used media for isolates of pathogenic neisseria (2)
what is a transport system specific for neisseria like in free clinics
male vs female lab diag (where sample taken and outcome)
Commonly used media for isolates of pathogenic neisseria is Taylor Martin (TM) agar→ Chocolate-based agar with some antimicrobics added as in VCN agar which is another similar concept that only allows pathogenic bacteria to grow
VCN agar→Chocolate agar modified by addition of antibiotics: Vancomycin to inhibit gram-positive bacteria, colistin to inhibit gram-negative bacteria rods, nystatin to inhibit yeast
Transport system specific for a neisseria such as the jembec plate system complete with CO2 generating tablets and TM plates and bag for more affordable incubation
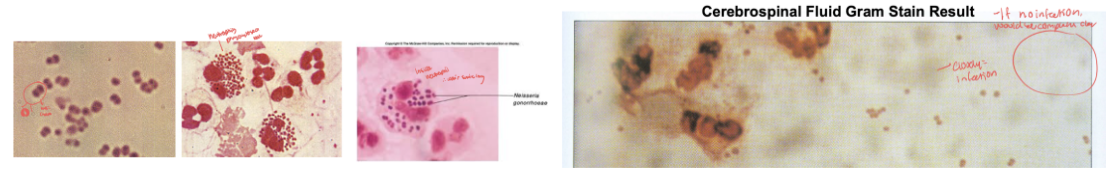
Lab diag in N. gonorrheae
male=>urethral discharge can see gram neg diplococci and leukocytes
female=> cervical smear with many epithelial cells, other bac similar to nisseria thus need more testing
Name the component of N. meningitidis responsible for the characteristic skin and tissue hemorrhaging in meningococcal meningitis. Discuss the importance of this virulence factor to the pathogenesis of Neisseria meningitidis.—>severe symptoms of n. meningitidis
Severe symptoms of N. meningitis=
petechial eruptions or pinpoint hemorrhages developing into larger Hemorrhage areas causing emboli of mangococci
emboli= a mass, such as a clump of bacteria or detached blood clot, foreign material like air bolus, that travels through the bloodstream and lodges and blood vessels, blocking it
Severe may be accompanied by:
Meningitis– inflammation of the meninges / membranes that envelop the brain and spinal cord
Septecemia– bacterial infection of the blood
Arthritis– inflammation of the joints
pericarditis– inflammation of membranes surrounding the heart
Involvement of any organ system is possible
may cause disseminated intravascular coagulation (DIC) followed by death as rapidly as one hour from onset of symptoms
Or waterhouse-friderichsen syndrome (adrenal gland involvement→turns red bc blood build up and no longer properly functional)
Name the most prevalent of the classical venereal diseases and identify what population has the highest incidence of infection.
Neisseria gonorrhoeae is causative agent of gonorrhea, most prevalent venereal disease; adolescents (⅓ of cases) occur in this group
Is world wide and most common classic vernal disease with 1 mil cases reported annually
Disease is most common in indiv 20-24 yr
Briefly explain the Waterhouse-Friderichsen Syndrome; include symptoms, cause, treatment, diagnosis.
body part involved
from what infection og
leads to what organ failure
how characterized
what if not treated immediately
progression of disease (~7)
Adrenal gland involvement
severe meningococcal infection (N. meningitidis)
Fulminant disease state that occurs suddenly and of great intensity
adrenal gland failure due to bleeding into adrenal gland
characterized by acute adrenal gland insufficiency, profound shock
fatal if not treated immediately
events of acute fatal meningococcal infection include: sudden onset with severe headache, rapid progression of disease, fever, coma, collapse, cyanosis or bluish pallor due to decreased oxygen intake, hemorrhaging of skin and mucous membranes
“gonococcal ophthalmia neonatorum”
due to what
most common manifestation
severe conjunvtivitis symp
treatment (3 antibi and type of admin and percents of soln)
% of school of blind due to no treatment before
“Neonatal gonococcal arthritis”
highly destructive form of what
onset and acute or subacute
“gonorrheal vulvovaginitis”
age group
may cause what
gonococcal ophthalmia neonatorum is infant gonorrhea and is due to infection acquired during passage through birth canal
Infection of the eye is most common manifestation (28% develops this if born to mom w/ infection)
Conjunctivitis is usually severe: N. gonorrhoeae can penetrate intact corneal epithelium and cause microbial keratitis, ulceration, perforation
Installation of 1% silver nitrate solution or antibiotic ointment (.5% erythromycin or 1% tetracycline) into conjunctival sac of newborn soon after birth is done to prevent blindness
Prior to routine use of Ag nitrate, 50% of children in schools for blind were bc of gonococcal ophthalmia neonatorum
Neonatal gonococcal arthritis
Highly destructive form of arthritis
Acute w/ onset at 1-4 weeks of life (later mani)
Gonorrheal vulvovaginitis
Usually occurs in older children (girls 2-8 yrs) in cases suspected of sexual abuse
May cause sterility
Describe disseminated intravascular coagulation (DIC) in terms of its progression, organs involved and patient prognosis,
A severe symptom of meningitis
can result in death as rapidly as 1 hour from onset of symptoms
Is always a secondary problem
is pathogenic activation of coagulation or blood clotting mechanisms
in other words, it is abnormal clotting (coagulopathy) within blood vessels (intravascular) that is widespread throughout the body (disseminated)
the causes are widespread formation of clots in the blood where abnormal bleeding occurs, clots disrupt blood flow within organs which leads to kidney failure, multiple organ failure, hypovolemia (not enough volume of blood to circulate), shock, and death
State a benefit the capsule provides to Neisseria meningitidis and to us as clinitians
sero group that accounts for >90% mengio disease
# of sero groups and on basis of what
Serological groups→capsule used for ID:
12 groups of N. meningitis have been ID on basis of immunological activity of capsular polysaccharides
Serogroups A, B, C account for >90% of meningococcal disease
Virulence factor: harder to phagocytize by neutrophils or macrophages
State the only known pathogenic determinant of Neisseria gonorrhoeae.
The presence of pili on virulent forms seems to be the only pathologic determinant
Discuss the most significant infections caused by Moraxella catarrhalis and what population of people is most affected by this bacteria.
cell morphology, gram stain, aerobic/anaerobic, oxidase
2 previous names
pathogenic?
most sig infections occur where and cause what 2 infections
__most common cause of those 2 infections
infections in what pop are more common
Gram neg diplococcus w/ kidney bean appearance, aerobic, oxidase pos, (all just like genus neisseria)
Why previously known as neisseria catarrhalis and then changed to branhamella catarrhalis
Previously considered to have no sig pathogenic conseq→recently associated w/ infection but not common
Most sig infections are in upper respiratory tract infections, specifically:
Otitis media (ear) and sinusitis in children
Lower respiratory tract infections in adults
3rd most common cause of otitis media and sinusitis in children following strep pneumoniae ad hemophilus influenzae
Infections in adults are more common if underlying conditions are present, esp in elderly
why does neisseria need chocolate blood agar plates as opposed to BAP
need free Fe in hemoglobin to grow
what is responsible for the extensive vascular damage that is a component of N. meningitidis
endotoxin release 100-1000x greater than norm
most meningitis infections enter__ and stop—
but if proceeds incubates ands spreads via bloodstream where
the upper resp tract
stop in memb of the nasopharynx
skin, meninges, eyes