PHAR 232-WBC/ID
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
39 Terms
Changes in WBCs can be caused by:
• Disease: Cancer/leukemia
• Drugs: Chemotherapy
• Genetics
normal total WBC count in adult
4.5 to 11 x10^3 cells/μL
What are WBC (leukocytes) and the division?
WBC is the immune system cells.
Divided into:
Granulocytes
lymphocytes
What are granulocytes?
phagocytes-engulf and destroy
What are lymphocytes?
recognizes self/non-self-assist granulocytes
What are the four types of graunolcytes?
neutrophils
eosinophils
basophils
monocytes
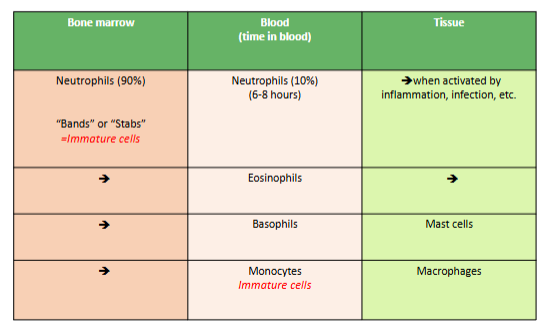
What are neutrophils (aka PMNs, Segs, Polys)?
• Phagocytic cells—attack and digest microbes
• Most are NOT free floating in the blood
• Vast majority are in the bone marrow
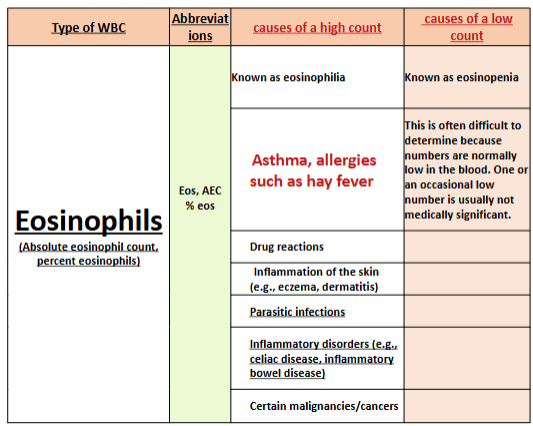
what are eosinophils involved with?
parasites and allergies
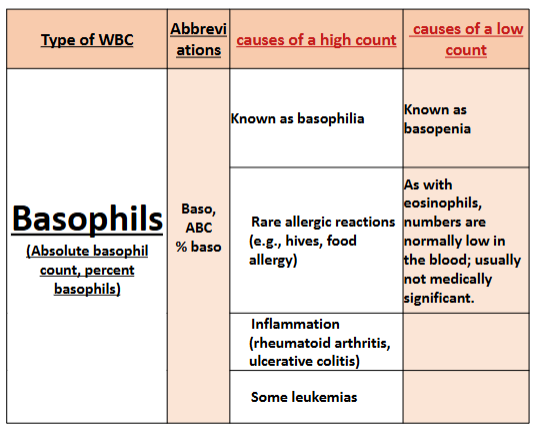
what are basophils involved with?
allergic rxns
release histamine and other mediators when activated
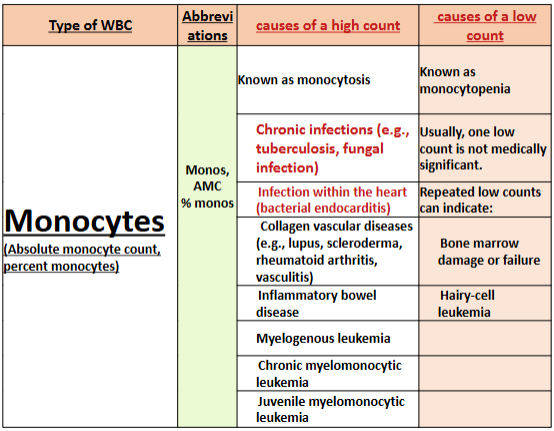
What are monocytes?
immature macrophages-actually are an agranulocyte
Granulocytes locations
Neutrophils table
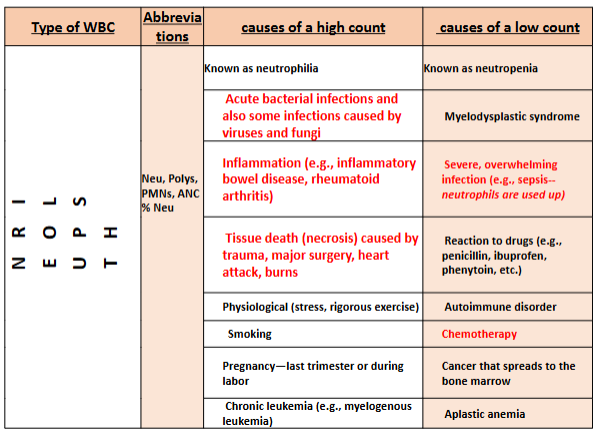
What is ANC?
absolute neutrophil count
WBC count * [(pmn%/100) + (bands%/100)] = ANC
-categorizes neutropenia
How is neutropenia categorized?
Neutropenia can be categorized as mild, moderate, or severe
• Mild neutropenia – ANC >1000 and <1500 cells/microL
• Moderate neutropenia – ANC >500 and <1000 cells/microL
• Severe neutropenia – ANC <500 cells/microL
What are some medications that must monitor the ANC to prevent severe life threatening neutropenia?
-clozapine
-certain chemotherapy agents
What else can ANC be used for?
ANC can be used to monitor immunosuppression and can signal the start of anti-microbial therapy
Eosinophils Table
Basophils Table
What are macrophages?
mature form of monocytes
where are macrophages found?
Mostly found in tissue
• Lymph nodes, lungs, spleen, liver, bone marrow
What are the functions of macrophages?
Phagocytic cell
• Eats bacteria and foreign cells
• Destroys old RBCs and helps recycle iron
• Takes surface antigens of pathogens and then displays on cell surface with a MHC protein to present to a lymphocyte.
-APC= Antigen presenting cell
Monocytes Table
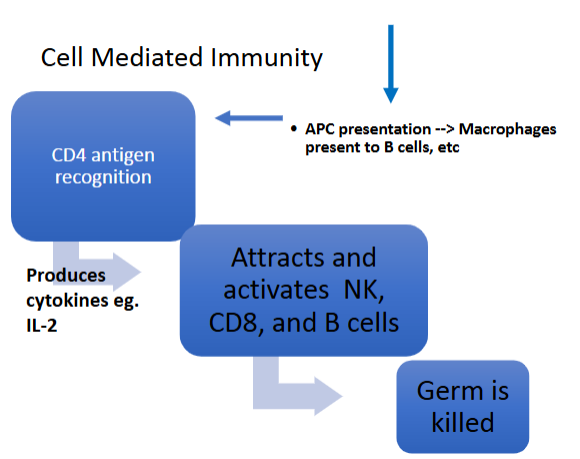
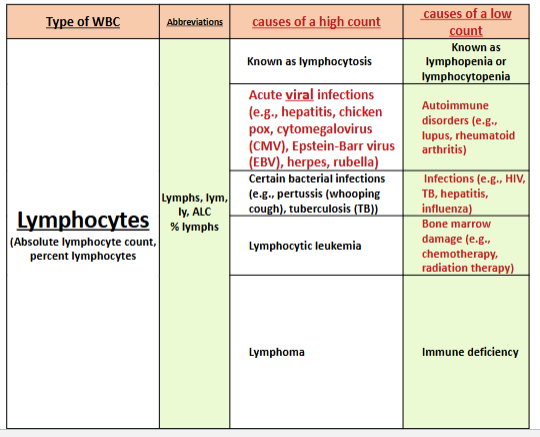
What are the different kinds of lymphocytes?
•Cell mediated immunity
•B cells
•NK cells
•T-cells:
-Are differentiated by CD markers
-CD4 ---Helper cell
-CD8--Cytotoxic cell
Cell Mediated Immunity Table
What are B-cells?
B-cells
• Normally express IgM
•Upon activation by T-cells they turn into
plasma cells
• Produce
• IgA
• IgD
• IgE
• IgG
• IgM
Lymphocytes Table
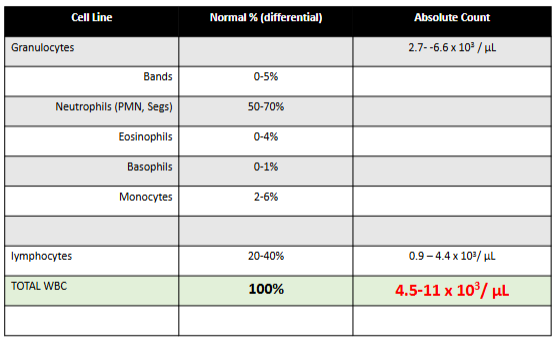
Differential % and Count
What are markers of imflammation?
acute phase reactants (APR)
ESR
C-RP
What is ESR?
Erythrocyte sedimentation rate.
• Increase in APRs cause aggregation RBCs causing them to settle faster.
• Measures the distance RBCs fall in heparinized blood in one hour.
• Units are mm/hr
• Inflammation causes them to clump and fall faster
What are C-RP?
C-Reactive Protein
• Complexed CRP activates the classical complement pathway.
• CRP elevations are nonspecific and may be useful for the detection of systemic inflammatory processes
• Elevated values are consistent with an acute inflammatory process.
Infection test ordering and interpretation steps
WHAT NEEDS TO BE CONSIDERED/ASSESSED.
1. Does the patient have an infection?
2. If they do, what is causing it?
3. Where is the infection?
4. What antibiotics will work on this patient?
a) How do I monitor it?
b) Are they allergic?
c) Can the antibiotic get to the site of infection?
d) Is the infection resistant to this antibiotic?
what are the following steps when asking “do they have an infection”?
•What are the three main causes of infection?
•Presenting factors ??
•Other tests---radiology, etc.
•Indicators:
- Increase in WBC – Leukocytosis
- Increase in “bands” or “stabs”
- Increase in ESR
What are some test to find “What kind of infection/What’s causing it?”?
• Gram stain- fairly fast
• Microscope- fairly fast
• RDT (rapid diagnostic technologies)- fairly fast but
only for limited organisms
• Immunologic- Antibody/antigen detection tests-
some fast/slow
• Cultures- can take days
• Sensitivity- can take days
• DNA probes –can take days
What does GRAM STAIN/microscope show us?
• Provides 3 important pieces of information pretty fast.
• Has limitations
How does gram stain tell us what kind of infection occurred?
•Gram stain can get you pretty close pretty fast.
•Use gram stain/morphology charts
•Use usual causative pathogens charts for type/location of infection.
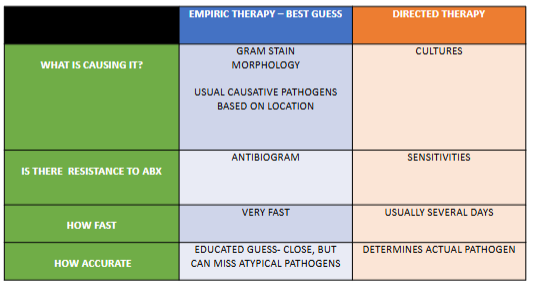
Why is empiric therapy?
• Is a reasonable guess when you need to start therapy NOW.
• Most of the time will need to confirm the empiric assessment.
• Based on:
-Typical causative pathogens for location of infection
-Gram stain results with morphology
-Available antibiotics and their spectrum of activity
• BUT---- You don’t have any information about bacterial resistance
-This comes from cultures and sensitivity info but it takes days for results
• SO----You guess based on the historical patterns of resistance for your
area
How to make an antibiotic choice?
• While waiting for cultures and sensitivity..........
• ANTIBIOGRAM
-Think of this as a generic predictor of sensitivity.
-Based off of culture and sensitivity results for a particular institution or region.
-Historical results for each particular species and level of resistance encountered at a particular institution or laboratory
When is directed therapy used?
• Can only be done with Cultures and Sensitivity information
• Culture can confirm or deny empiric pathogen assessment.
• Sensitivity can confirm or deny effectiveness of your antibiotic choice.
-What else can confirm or deny your empiric antibiotic choice?????
• Culture information identifies the species of pathogen
• Sensitivities information determines what level of antibiotic resistance is present in this isolate.
EMPIRIC VS. DIRECTED THERAPY TABLE