BIOLOGY TOPIC 6
1/38
Earn XP
Description and Tags
Infection, immunity and forensics
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
39 Terms
Forensic science key questions
What is the identity of the individual?
When did they die?
How did they die?
IDENTIFICATION OF BODY
Personal belongings (passport, driving license e.t.c)
Unique features (tattoos/surgery scars)
Fingerprinting
Dental records
DNA profiling
EXON
The sequence of DNA bases that codes for a sequence of amino acids
INTRON
The sequence of DNA bases that DOESN’T code for a sequence of amino acids.
Which contain short-tandem repeats
Process of pre-mRNA to mRNA
The introns are spliced out to leave the exons that code for amino acids to make proteins

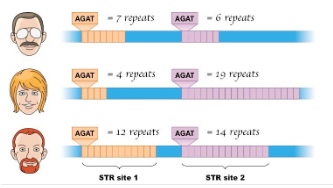
Theory of DNA profiling
Relies on individuals with unique DNA base sequences
There is a large amount of DNA that doesn’t code for proteins
Inside introns are STR’s (short tandem repeats) that are repeating base sequences.
PROCESS OF DNA PROFILING
Obtain DNA sample
Create DNA fragments: using resttriction enzymes to cut DNA by targeting base sequences, breaking phosphodiester and Hydrogen bonds= sticky ends
Amplify DNA fragments (PCR)
Separate DNA fragments (gel elctrophoresis)
Visualise the fragments
PCR (similar to DNA replication)
Polymerase chain reaction to amplify the dna fragments.
DNA fragments, primers, DNA (Taq) polymerase and free nucleotides are added to a thermocycler- 95 degrees temp casues DNA strands to separate
Primers join to their complementary bases at 55 degrees
synthesis of DNA- temp increases to 70 degrees (optimum temp for DNA polymerase), DNA polymerase attaches nucleotides to along each of their separated DNA strands.
The more cycles= exponential increase of quantity of DNA
(repeated 20-50 times)
GEL ELECTROPHORESIS
Separates the DNA fragments from PCR.
DNA placed onto agarose gel in an electrophoresis tank submerged into a buffer solution and connected to positive+negative electrodes
DNA is negatively charged so they move through the gel towards the anode.
Smaller fragments move fastes and furthest
A DNA marker is added to a gel which contains fragments of known length
These are then incubated with a DNA probe
Sample is shone under UV light and positions of DNA bands are seen and compared
TIME OF DEATH (Forensic entomology)
Body Temperature- When a person dies, the body starts to cool as heating processes (respiration) stops (algor mortis)
Muscle stiffness - After death, respiration stops, oxygen is not diffused in. This causes anaerobic respiration and produces lactic acid which reduces the pH, denaturing the active site of enzymes. This means the substrate cannot bind and ATP is not generated. Muscle fibres do not have any enerfy for contraction and so become fixed in place (rigor mortis)
DECOMPOSITION
Microorganisms in and out of the body release extracellular enzymes that breaks down the body’s polymers into monomers.
Few hours-days: skin turns green as cells+ tissues are broken down
Few days-few weeks: methane released and body becomes bloated skin starts to fall off
After several weeks- tissues liquifey and leak outside of body
Few months-few years- body tissues completely broken down and only bones remain
After several decades- bones disintegrate and nothing remains of body.
STAGES OF SUCCESSION
Few hours- Flies appear on body and lay eggs (larvae)- takes 24 hours to hatch
Beetles- eat decomposed body fat
Other insects e.g moths feed on liquified parts of the corpse + any clothes on the body
Other insects appear once the bodys proteins have been digested- they feed on food in the digestive system that were not fully digested
Burying beetle- eats dead flesh
When the body is fully decomposed, all the remaining insects leave.
How the body PREVENTS INFECTIONS:
Mucus membrane- contains lysozyme which kills bacteria damaging their cell wall and bursting them open (chemical barrier)
Skin- physical barrier, blood clots minimises entry of pathogens
Trachea- contains goblet cells which secrete mucus and trap pathogens (chemical barrier)
Stomach- highly acid which can denature proteins and kill pathogens (chemical barrier)
INFLAMMATION
Histamines trigger dilation of blood vessels and permeability of capillary walls
Phagocytes and killer cells attracted to site of infection- chemotaxis
NON-SPECIFIC IMMUNE RESPONSE:
Fast- acting and has the same response for all pathogens
Interferons (proteins) released by cells in presence of pathogens
Antigens on pathogen bind to receptor on phagocyte (macrophage)
Phagocyte engulfs pathogen via endocytosis
pathogen becomes enclosed in a vesicle
lysosome fuses with vesicle and lysozymes released to break down pathogen and released from phagocyte via exocytosis.
Phagocyte takes the pathogens antigens and presents it on its surface (antigen presenting cell)
LYMPHOCYTES
T- cells: produced in bone marrow and mature in thymus gland
types: T helper, T memory, T killer
B- cells: produced and matured in bone marrow
have antibody receptors and divide by mitosis to produce plasma cells+ B memory cells
SPECIFIC IMMUNE RESPONSE
T helper cells bind to APC via complementary CD4 receptors
T helper cells release cytokines to activate next steps e.g activating B cells and producing T killer cells
T killer cells kill the pathogens—- T memory cells produced
B cells differentiate into plasma cells which secrete antibodies—— B memory cells
ANTIBODIES
After infection, the body makes memory cells which help the body launch a quicker immune response for a future infection of the same pathogen
ACTIONS OF ANTIBODIES
Agglutination- 2 binding sites mean antibodies can clump several pathogens together= more efficient phagocytosis
Antibodies can bind to toxins released by pathogens which is engulfed by ohagocytes
Neutralisation- They can block the antigens of pathogens preventing them from entering body cells
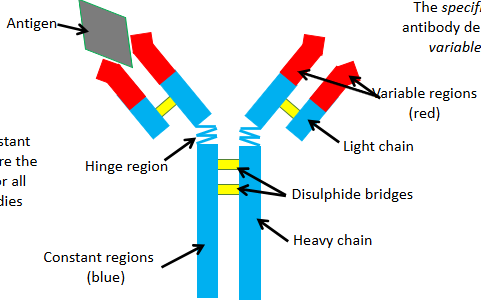
SHAPE OF AN ANTIBODY
The specifity of the antibody depends on its variable regions
The constant regions are the same for all antibodies
Each antibody has a different shaped variable region~ due to different amino acid sequences
The variable region is complementary to a specific antigen forming an antibody- antigen complex.- from the B cell
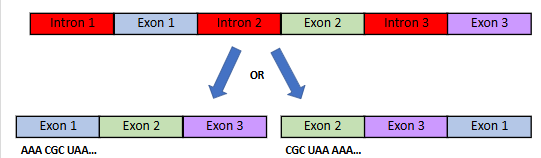
SPLICING~ one gene many proteins
After transcription, prior to leaving the nuclear pore:
The mRNA is spliced (pre-mRNA)- introns are cut out using restriction enzymes
The remaining exons piece together to form mature mRNA which leaves the nucleus via the nuclear pore for translation
example question: (how can one gene can give rise to more than one protein)
ALTERNATIVE SPLICING
Certain exons can be recombined into different orders to make different codons, which will code for a different sequence of amino acids which determing how the protein folds= new protein
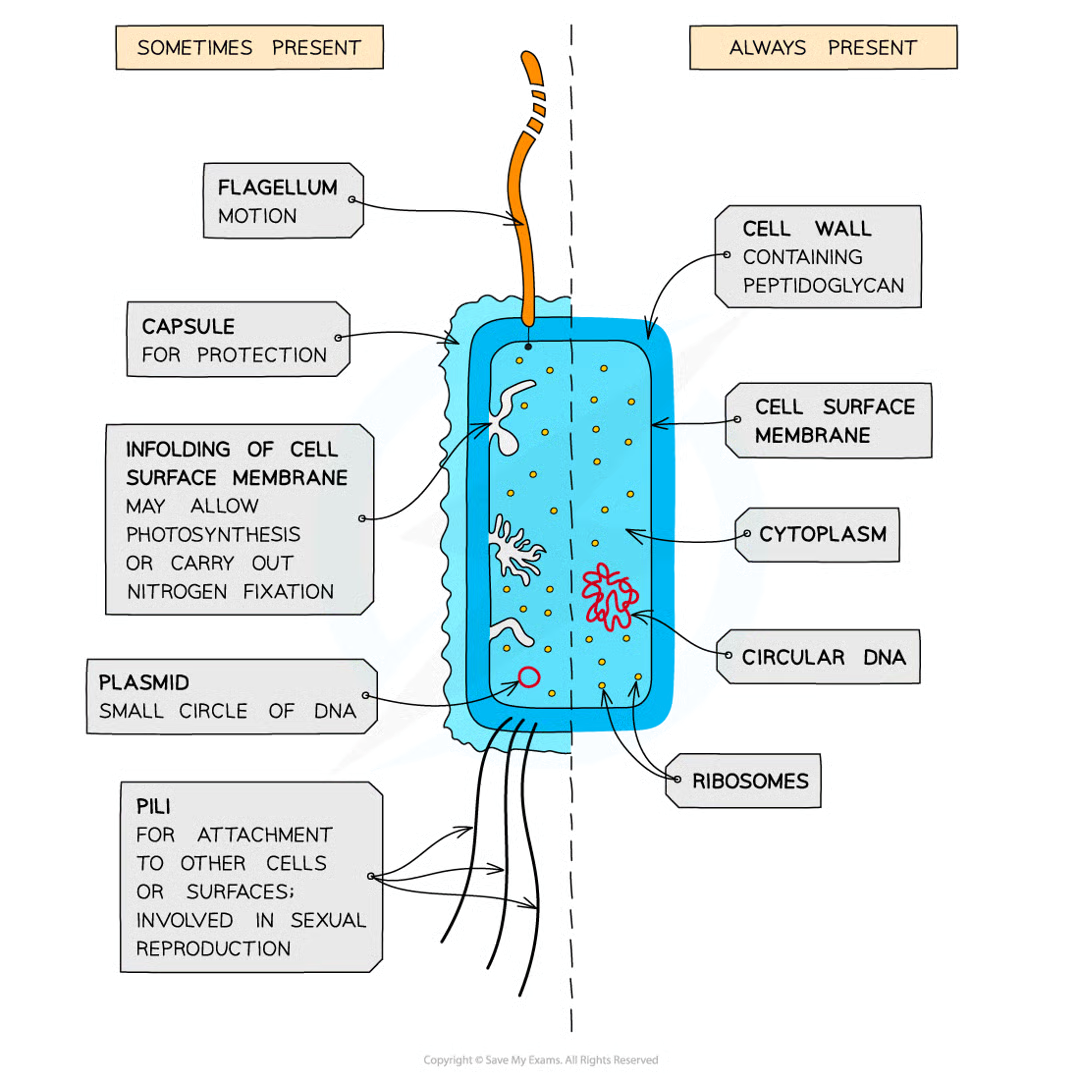
BACTERIA STRUCTURE
small single celled prokaryotes
lacks membrane-bound organelles
70S ribosomes
No nucleus- only have dna loop/ plasmid
cell wall with peptidoglycan
cell memrbane with mesosome cell membrane folding
capsule- prevents cell dehydration
flagella- movement
pili- allows bacteria to attach to other cells/ surfaces and transfer substances
VIRUS STRUCTURE
non-cellular
nucleic acid core- either DNA or RNA
can be single or double stranded
No membrane/cytoplasm/ribosomes
some have an outer envelope layer from the membrane phospholipids
contains proteins in caspid
attachment proteins- sticks out of capsid/ envelope to allow the virus to attach itself to a host cell

ACTIVE IMMUNITY
When an antigen enters the body triggering a specific immune response (long term immunity)
Natural active: from exposure to pathogens
Artificial active: from vaccination
PASSIVE IMMUNITY
Acquired without an immune response- antibodies gained from another source
Natural passive: e.g babies receiving antibodies from placenta of mother
Artificial passive: Given by an injection
This doesn’t activate the immune system so no memory cells are enabled= short term immunity
But antibodies appear in blood immediately than in active.
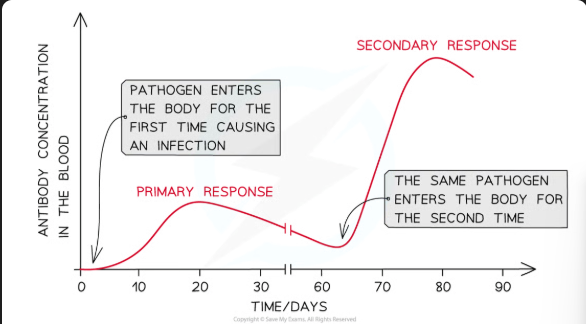
VACCINATION
Contains antigens that are put into the body to induce artificial active immunity
either dead/weakened pathogens/ antigens
produces long term immunity as they cause memory cells to produced and a stronger secondary response
ANTIGENIC VARIATION
Vaccinations need to be constantly modified to keep up with changes of a pathogen’s antigens
The change is due mutations that change the shape/ structure of the antigens
THE EVOLUTIONARY RACE
both hosts and pathogens evolving at the same time
HIV evasion mechanism: kills T helper cells, reducing no. cells to detect the virus due to high mutation rate= new strains of the virus which are not detected by memory cells and prevents cells from presenting antigens to surface
TB evasion mechanism: produces substances that prevents a lysosome from fusing with the phagocytic vacuole= they multiply + disrupt antigen presentation
TB (Mycobacterium tuberculosis)
Transmission- when infected people with the active form of TB cough/ sneeze and transmit liquid lipid droplets of TB bacteria in the air
uninfected people inhale these droplets (more likely in overcrowded areas)
Inside the lungs: the bacteria is engulfed by phagocytes. The bacteria may survive and reporiduce in phagocytes
Over time, the infected phagocytes become encased in tubercles in the lungs- bacteria remain dormant
The bacteria CAN become activated and attack the immune system at a later stage e.g if HIV arises
the length of time between infection and developing TB can vary from a few weeks to a few years
SYMPTOMS OF TB
First symptoms- fever, fatigue, coughing
secondary: lung inflammation and respiratory failure and spread to other parts of the body- organ failure
HIV- Human immunodeficiency virus
Transmitted through: bodily fluids (mucus/saliva) in blood transfusions, sexual intercourse or sharing needles.
It contains RNA (enveloped virus) with reverse transcriptase and integrase enzymes
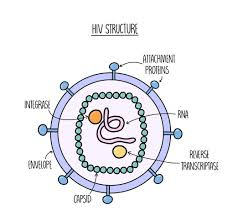
REPLICATION OF HIV
The virus infects T helper cells in the blood.
attachment proteins on virus binds to CD4 receptors of t helper cells
Capsid is released into T cell and releases RNA via endocytosis
Reverse transcriptase uses viral RNA as a template to make complementary viral DNA
this DNA is inserted into host DNA (human) via integrase enzyme
It uses the host enzymes to produce viral proteins
These assemble to form copies of viral particles that bud from the host cell and infect other T helper cells
SYMPTOMS OF HIV
Flu-like symptoms
over a long period of time, the virus reducces the number of T helper cells meaning they cannot activate B cells, so less/no antibodies are produced
This leads to AIDS (acquired immune deficiency syndrome):
immune system is so weak it can no longer fight off normal infections (oppurtinistic)
can lead to TB infections and spread to other organs= death
FACTORS AFFECTING SPREAD OF HIV
Age, existing infections, strain of HIV and access to healthcare
TYPES OF ANTIBIOTICS
Antibiotics damage bacteria cells only
BACTERICIDAL- kill bacterial cells
BACTERIOSTATIC- inhibit bacterial growth
How do bacteriostatic work
Interfering with the growth of bacteria:
breaks down peptidoglycan cell wall
binding to ribosomes to prevent protein synthesis
viruses+ eukaryotic cells are not damaged by antibiotics because they dont have cell walls and have different ribosomes+ enzymes
CPAC 15: Investigating effects of different antibiotics
transfer bacterial culture (e.coli) onto agar plate using sterile pipette and spread using innoculating loop (lawning technique)
stelirise by passing equipment through bunsen burner before and after use
soak paper discs into different antibiotics: Tetracycline, Chloramphenicol and amoxycillin and in control (water)
Place each disc in a quarter of the agar plate
Lightly tape the lid onto petri dish and invert and incubate at 25 degrees for 24 hours
Measure zone of inhibitions for all anitbiotics, larger zones means they are the most effective- use stats test
HOSPITAL ACQUIRED INFECTIONS
Measures to reduce risk of infections:
staff and visitors must wash hands regularly
when infected with a HAI they must be isolated to prevent spread
surfaces and equipment disinfected before and after use
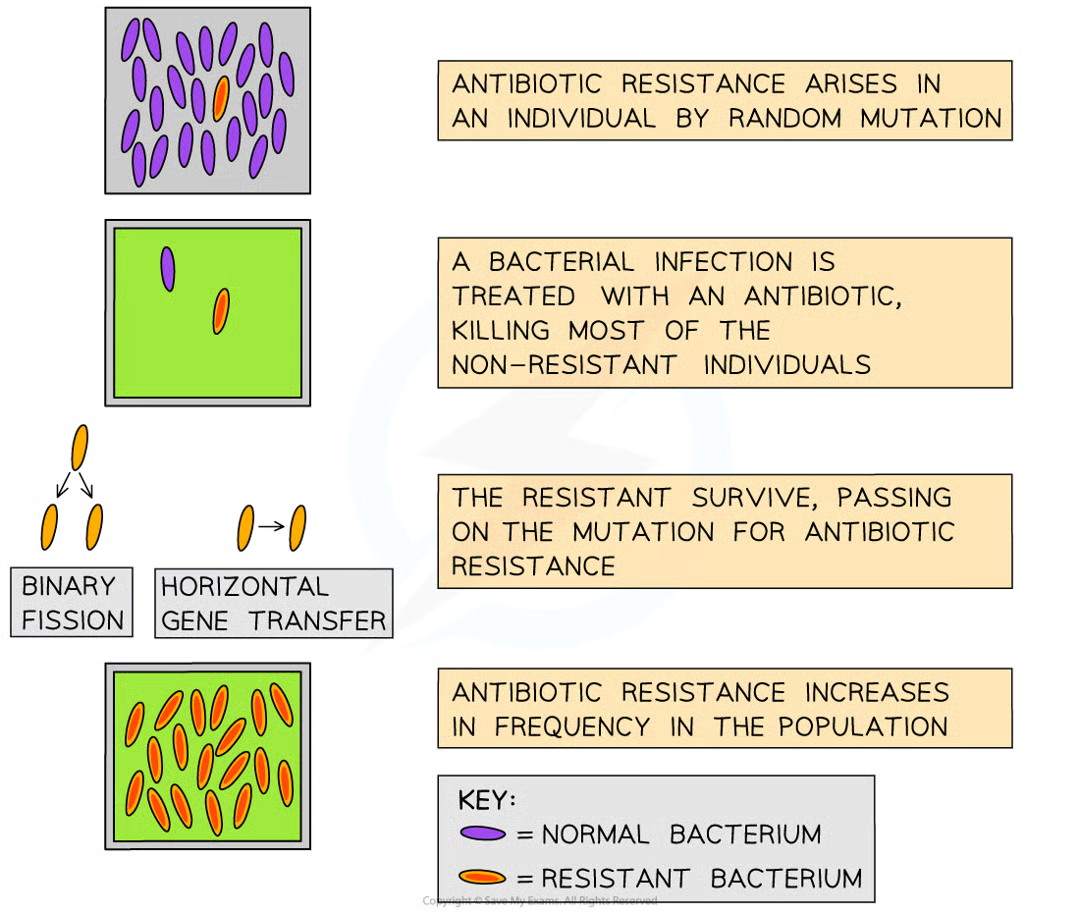
ANTIBIOTIC RESISTANCE:
HAI’s are caused by antibiotic resistant bacteria e.g MRSA resistnace to methicillin
Hospitals provides a selection pressure for natural selection:
random mutations
the bacterial infection is treated with antibiotics which only kill most of the bacteria
the resistant with advantageous alleles survuve and pass these genes (binary fission and transfer of genes through pili)
the resistance increases in population= antibiotic can no longer work.