Radiologic Evaluation of Fractures
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
58 Terms
how do you describe a fracture?
anatomic site and extent
type
alignment
direction
special features
associated abnormalities
special types
what is a comminuted fracture?
more than 2 fracture segments
what is an incomplete fracture?
one cortical margin remains intact
relatively stable
seen predominantly in short, flat, or irregularly shaped bones
mostly seen in children or in people with metabolic disorders
how do you describe displacement?
describe position of distal fragment in relation to proximal
position refers to relationship of fragment to normal structure
what is angulation named for?
the direction of angular displacement of the distal fragment in relationship to the proximal fragment
the direction of the apex of the angle formed by the fracture segments
what causes a transverse fracture?
results of a bending force
occurs at right angles to the longitudinal axis
what is a longitudinal fracture?
approximately parallel to the shaft
what causes oblique fracture?
result of combined forces of compression, bending, and torsion
what causes a spiral fracture?
spirals along long axis of bone due to torsion
what is impaction?
results from compression forces related to axial loading
bone is driven into itself
what are the types of impaction fracture?
depression fx
compression fx
what is an avulsion fx?
fragments of bone are pulled away from the main body of bone OR passive resistance of a ligament against a tensile force
occurs at bone prominence
what is a stress fx?
repetitive minor trauma on normal bone
what causes stress fractures?
chronic high-frequency, low level loading does not allow bone sufficient time to heal and remodel
what are the types of stress fracture?
fatigue fx
insufficiency fx
what is a fatigue fx?
excessive stress on healthy bone
normally in young/active people
what is an insufficiency fx?
normal stress on a pathologic bone
typically in old, inactive people
what is an epiphysis?
the end of a bone
what is a physis?
epiphyseal growth plate
what is a metaphysis?
proximal to the physis
what causes difficulties with fx assessment in children?
epiphyseal growth plates
dense growth lines
secondary centers of ossification
large nutrients foramina
what is a greenstick fx?
shaft is fracture on the tension side while the cortex and periostium remain intact on the compression side
what is a torus fracture?
impaction fracture that result in buckling of the cortex
predominantly at the metaphyseal region because of the amount of cancellous bone and newly remodeled trabecular bone present
what is plastic bowing?
compression forces exceed the point in which elastic recoil returns
type of incomplete fracture (microfracture)
describe a type 1 epiphyseal growth plate fracture
fracture line extends through the physis, separating and displacing the epiphysis from the normal position
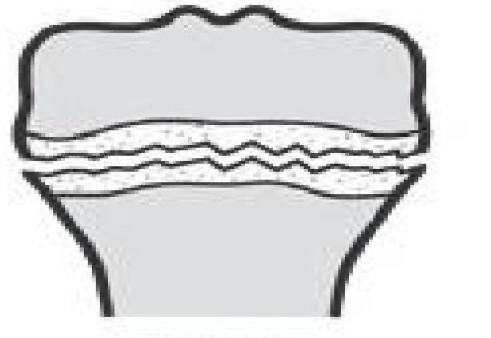
what type of fracture is this?
type 1
what is the prognosis for type 1 fractures?
good for normal growth
describe a type 2 epiphyseal growth plate
fracture line extends through the physis and exits through the metaphysis creating a triangular wedge that displaces with the epiphysis
what is the prognosis for a type 2 fx?
good for normal growth
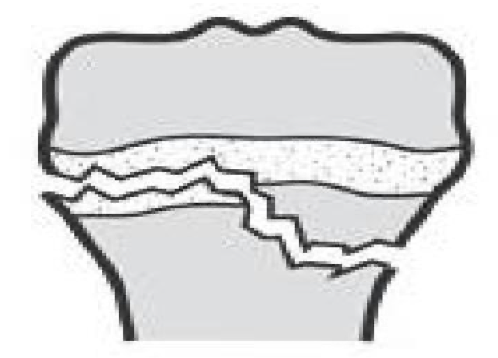
what type of fx is this?
type 2
describe a type 3 fx?
fx line that extends from the joint surface through the epiphysis across the physis
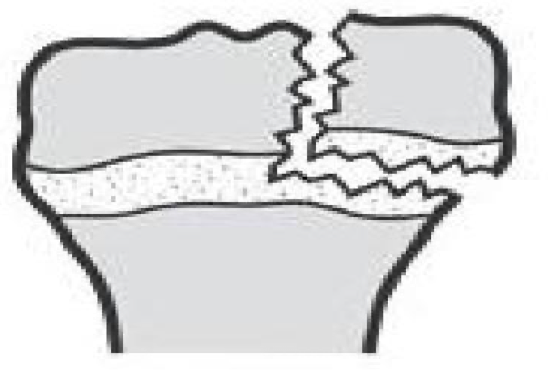
what type of fx is this?
type 3
describe a type 4 fx
fracture line extends from the joint surface through the epiphysis, physis, and metaphysis
what is the prognosis for a type 4 fx?
partial growth arrest is possible and surgical fixation may be necessary
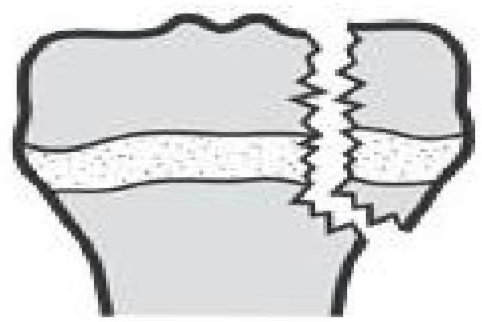
what type of fx is this?
type 4
describe a type 5 fx
fracture is a crush type injury that damages the physis by compression
what is the prognosis of a type 5 fx?
eventual growth arrest may be the only indication of this injury

what type of fx is this?
type 5
what is the name of the classification for growth plate fractures?
Salter-Harris
what does SALTER stand for?
Straight across
Above
Lower
Through Everything
cRush
what happens in callus formation?
hematoma forms
metabolic reaction occurs
organization/ossification
new bone proceeds towards and bridges the gap
callus is formed
what are the phases of fracture healing?
hematoma
inflammation
soft callus
hard callus
remodeling
what happens during the hematoma phase?
bleeding
fibrin clot will form
what happens during the phase of inflammation?
cells involved
cells
macrophages
mesenchymal cells
stem cell migrate to the fracture and form the granulation tissue and will release growth factors
granulation tissue tolerates the greatest strain before failure
what two types of meds make fx healing harder and why ?
COX-2 inhibitors and NSAIDs
depress Runx2 which is important for differentiation of osteoblasts
what is secondary bone healing?
healing through cartilage formation
lack of stability helps the formation of cartilage which later on can change to endochondral ossification
what happens when a hard callus is formed?
type 2 collagen changes to type 1
what is type 1 collagen?
bone
what is type 2 collagen?
cartilage
blood flow is need to give the fracture site nutrients to heal. when does blood flow increase and when does it return to normal?
2 weeks
3 months
what happens during the remodeling phase?
the woven bone will be replaced by stronger, laminar bone
fracture healing will be complete with the continuation of the medullary cavity
when does the remodeling stage begin and end?
2 weeks
continues for many years
how does the endochrondral bone formation occur?
chondrocyte proliferation then hypertrophy
matrix mineralization
chondrocytes die
vascular invasion, ossification, and remodeling to lamellar bone
what are the growth factors involved in fracture healing and what do they do?
bone morphogenetic protein
transforming growth factor beta (TGF-B1)
insulin-like growth factor 2 (IGF2)
platelet-derived growth factor (PDGF)
what does bone morphogenetic protein do?
osteoinductive causing the undifferentiated mesenchymal cells to differentiate into osteoblasts
what does transforming growth factor beta (TGF-B1) do?
will make the mesenchymal cells produce type 2 collagen and proteoglycans trying to produce endochondral ossification
what does insulin-like growth factor 2 (IGF-2) do?
stimulate type 1 collagen
what does platelet-derived growth factor (PDGF) do?
attracts inflammatory cells to the fracture site (chemotactic)
released from platelets