Cardiovascular physiology
5.0(1)
Card Sorting
1/133
Earn XP
Description and Tags
Last updated 1:47 PM on 1/12/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
134 Terms
1
New cards
Einstein diffusion vs time
Time is proportional to distance squared, meaning that small changes in distance result in large changes in tiMe. Therefore diffusion over long distances is far too slow.
2
New cards
Neuromuscular gap junction
0\.1 micrometer distance over which neurotransmitters diffuse, taking only 5 millionths of a second.
3
New cards
Cardiac infarct
Condition characterised by the formation of a dense wedge -shaped block of dead tissue in the heart muscle following an interruption to its blood supply
4
New cards
Ischaemia
Muscle that dies due to lack of oxygenated blood supply. The irony being that the adjacent cavity has copious amounts of richly oxygenated blood that cannot diffuse a few millimetres at an adequate rate.
5
New cards
Blood clot blockage/ ‘heart attack’
Thrombus (clot) → Ischaemia → Hypoxia → Necrosis
6
New cards
Ischaemia vs hypoxia
Lack of blood flow vs lack of oxygen
7
New cards
Primary function
Overcome the problem of moving chemicals long distances at a reasonably high speed. Using a pump and bulk flow.
8
New cards
Advantages of circulatory system
1. Organism can get bigger
2. Sustain a higher metabolic rate
3. Direct flow of metabolites between organs
4. Regulation of organ function
9
New cards
Disadvantages of circulatory system
1. Circulatory failure can be fatal
2. High pressure and flow requires control
3. High pressure = stress on vessels
4. Metabolically expensive
10
New cards
Hormones
Chemicals produced and secreted into the bloodstream by an endocrine gland. Carried to distant target organs to interact with receptors.
11
New cards
Adrenal glands
Endocrine organ situated on top of the kidney. Has two distinct zones: inner adrenal medulla and outer cortex.
12
New cards
Adrenal medulla
Makes and secretes adrenaline, a hormone which acts on the heart to increase heart rate and force of contraction.
13
New cards
Thermoregulatory control
A rise in core temp of 0.5°C causes blood vessels close to the skin to dilate, allowing heat loss. E.g. heat loss from rabbit ears.
14
New cards
Adaptation to hot environment
Desert mammals have disproportionately large ears to maximise the heat loss due to dilatation of peripheral circulation.
15
New cards
Immune system
Ciculatory system supports another key system by transporting white blood cells, platelets and red blood cells.
16
New cards
Open circulatory system
The heart pumps fluid through arteries that empty into a haemocoel, which bathes the organs, and return to the heart via veins.
17
New cards
Haemolymph
Fluid which has no distinction between blood and tissue fluid.
18
New cards
Disadvantages of open circulation
Limited control over velocity and distribution of blood flow. (However is usually not needed
19
New cards
Closed circulatory system
Blood does not leave the blood vessels and is sepearate from tissue fluid. Have relatively high blood pressure enabling quick transport to support high metabolic rate.
20
New cards
Squid
Organism with a closed circulatory system containing three hearts, one for each gill and one for the rest of the body.
21
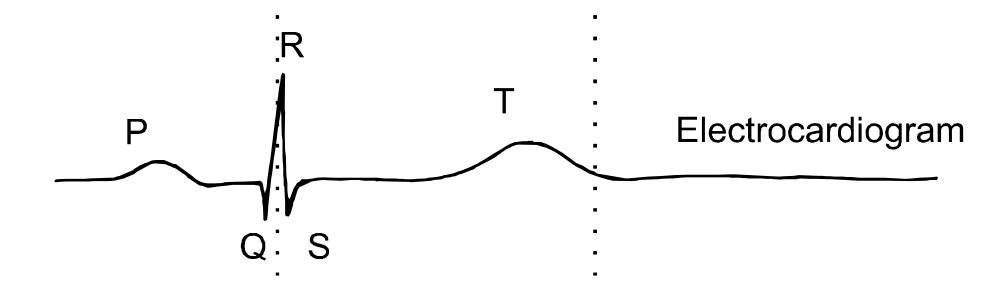
New cards
Single circulation
FISH: Blood flows from the heart to the gills for gas exchange, then to the rest of the body and then back to the heart.≥
22
New cards
Double circulation
Amphibians, reptiles, birds and mammals. Blood flows from heart to lungs, then back to the heart to be repressurised, flow around the body.
23
New cards
Branchial cicuit
Vessels that serve the gills (respiratory organs)
24
New cards
Pulmonary circuit
Vessels that serve the lungs (respiratory organ)
25
New cards
Systemic circuit
Vessels that serve the rest of the body.
26
New cards
Trout dissection
Remove the **isthmus** (triangle of skin between the gills and pectoral fins), allows access to **pericardial cavity** (a sac). The triangular ventricle can be seen leadin to the **bulbous arteriosus** which represents the beginning of the **ventral aorta**, into which the ventricle ejects blood. Blood flows through the gills, becoming oxygenated and is taken to tissues via the **dorsal aorta**.
27
New cards
Amphibians
2 atria, 1 ventricle. Compensate for inefficiency by having rich vascular beds just beneath the surface of their moist skins, so blood returns to the heart already partially oxidised.
28
New cards
Birds and mammals
Septum separates atria and ventricles into two seperate chambers.
29
New cards
Aorta
Artery that takes blood from heart to systemic circulation
30
New cards
Arterioles
Small vessels connecting arteries and capillaries.
31
New cards
Capillaries
Tiny, 1-cell-thick walled vessels, that act as a bridge between arteries and veins. Thins walls allows oxygen and nutrients to pass from blood to tissues, and waste products vice versa.
32
New cards
Venules
Small vessels that connect veins to capillaries
33
New cards
Superior and inferior vena cava
Veins through which blood returns to the right side of the heart.
34
New cards
Pulmonary artery
Vessel that carries blood from the right ventricle to the lungs for oxygenation.
35
New cards
Pulmonary veins
Vessels that return oxygenated pulmonary blood to the left atrium.
36
New cards
Pericardial sac
Location of the heart, lower surface connected to the diaphragm.
37
New cards
Annulus fibrosus
Connective rings that surround the valves of the heart- the atria-ventricular (AV) valves and the semi-lunar/arterial valves.
38
New cards
Chordae tendinae
Collagenous tendons connected to the thin flaps of tissue of the AV valves. Tethered to papillary muscle, providing stability .
39
New cards
AV closing mechanism
Ventricle contracts, blood pushes against the underside of the valve forcing it into its closed position.
40
New cards
Tricuspid valve
AV valve that separates the right atrium from the right ventricle (R-S-T)
41
New cards
Mitral valve
AV valve that separates left atrium from left ventricle.
42
New cards
Semi-lunar valves
Separate the ventricles from the main arteries. Do not need connective tissues.
43
New cards
Aortic valve
Valve between left ventricle and AORTA
44
New cards
Pulmonary valve
Valve between right ventricle and PULMONARY artery
45
New cards
Tunica intima
Endothelium and its elastic connective tissue
46
New cards
10 micrometers
Nearly all cells in the body are within at least … of a capillary
47
New cards
Tunica media
Dense population of smooth muscle cells organised cocentrically with bands of elastic tissue. Varied thickness between vessels, e.g. thick layer in large elastic arteries to smooth pressure changed.
48
New cards
Tunica adventitia
Collagenous extracellular matrix containing fibroblasts, blood vessels and nerves. Functions to add rigidity and form.
49
New cards
Veins
Vessels that have relatively thin walls and large cross-sectional areas. Hold about 2/3 of the body’s blood.
50
New cards
Delayed compliance
Within tenths of a second, the pressure in a vessel returns to normal following a sudden increase or decrease. Result from smooth muscle cells changing length allowing the volume of the circulatory to inc or dec. (occurs in veins)
51
New cards
Darcy’s law
Q= ∆P/R i.e. liquids flow down pressure gradients from high pressure to low pressure against resistance
52
New cards
Perfusion pressure
Pressure difference between the arteries that supply a region and the veins that drain it.
53
New cards
Blood flow
= perfusion pressure / vascular resistance
54
New cards
Cardiac output
= blood pressure / vascular resistance
(because perfusion and blood pressure are almost equal as pressure in the venous system is only a few mmHg)
(because perfusion and blood pressure are almost equal as pressure in the venous system is only a few mmHg)
55
New cards
Stroke volume
Amount of blood pumped out of each ventricle per beat.
56
New cards
Heart rate
Speed of beating of ventricles
57
New cards
Determinants of blood pressure
Vascular resistance *x* cardiac output, where cardiac output = stroke volume x heart rate.
58
New cards
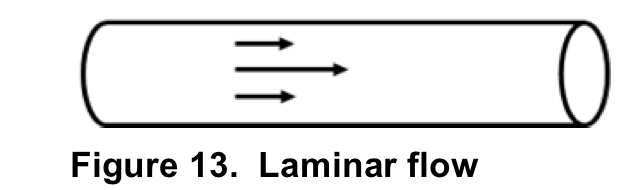
Laminar flow
A description of blood flow through a vessel where streams in the centre of the vessel travel the fastest, whilst those at the outside experience more pressure and are therefore slower. Forms a parabola shape.
59
New cards
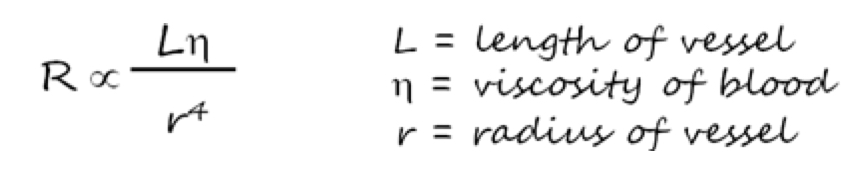
Poiseuille’s Law
Shows how resistance is influenced by the length of the vessel, radius of the vessel and the viscocity of blood.
60
New cards
Haematocrit
Ratio of blood cells to plasma, indicative of blood viscocity.
61
New cards
Vasomotion
Change in vessel diameter, caused by nerves, hormones and local factors.
Vasodilatation- Increase
Vasoconstriction- decrease
Vasodilatation- Increase
Vasoconstriction- decrease
62
New cards
Noradrenaline
Hormone that acts on receptors on blood vessels to increase vasoconstriction. Tonically active to maintain total peripheral resistance and arterial blood pressure.
63
New cards
Sympathetic tone
Vasoconstrictor which topically impose a squeezing tone on vessels to maintain total peripheral resistance. Withdrawing tone is the simplest way to dilate a blood vessel.
64
New cards
Dilation
Normally, adrenaline causes constriction, in skeletal muscle adrenaline can cause dilatation so that distribution of blood is to the areas.
65
New cards
Endothelium-derived relaxation factor (EDRF)
Term by which nitric oxide (NO) was first known by when it was released by vessel endothelium.
66
New cards
Nitric oxide (NO)
Chemical for which its formation is stimulated by substances that activate endothelial cells such as ACh. Produced via cleavage form the amino acid arginine by NO synthase.
67
New cards
Arginine
Amino acid from which NO is cleaved from
68
New cards
NO synthase
Enzyme that catalyses formation of NO, regulated by Ca²⁺ -calmodulin complex.
69
New cards
Ca²⁺-calmodulin complex
Intracellular complex that regulates NO synthase. Means that agents that promote extracellular calcium entry (ACh) increase the rate of NO synthase.
70
New cards
Sphygmomanometer
Used to estimate arterial blood pressure. Inflatable cuff encircles the upper arm and is inflated until pressure exerted is higher than the pressure driving arterial blood, causing blood flow to stop. Pressure is released until the Korotkoff sound is heard, representing highest artery pressure (shown on pressure gauge).
71
New cards
Korotkoff sound
Thumping sound with each wave of pressure.
72
New cards
Systolic pressure
Highest pressure at which the Korotkoff sound is first heard.
73
New cards
Diastolic pressure
Point at which the Korotkoff sound disappears, lowest arterial pressure.
74
New cards
120/80 mmHg
Average human arterial pressure, systolic/diastolic
75
New cards
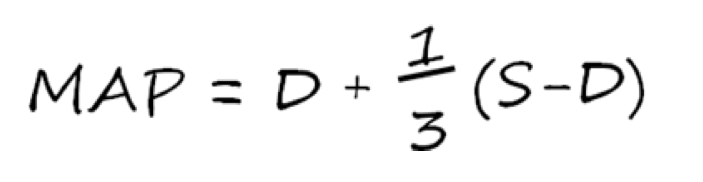
Mean arterial blood pressure (MAP)
Diastolic plus a third of the difference between diastolic and systolic.
76
New cards
Arterial stiffness
Measure of the rigidity of blood vessels. Increases with age and cardiovascular disease. Vessels deposit calcium and collagen.
77
New cards
Increase in pulsality
Increase in systolic pressure relative to the diastolic pulse or an increase in the pulsality index (S-D/mean). Signify increased vascular resistance.
78
New cards
Exercise
NOT full body motion. But rather can be a single muscle/group of muscles. Doesn’t necessarily lead to changes in cardiac output, ventilation or adrenaline levels.
79
New cards
30-fold
Factor by which blood flow per unit of time in a rhythmically contracting muscle increases.
80
New cards
Local vasodilatation
Process caused primarily by local metabolites acting directly on the muscle arterioles. Explains the lag in return to normal blood flow once exercise has ended.
81
New cards
Metabolic autoregulation
More local metabolites, due to increased utilisation of oxygen. Therefore oxygen used=oxygen supplied, positive feedback loop.
82
New cards
Local metabolites
By-products of metabolism. E.g lactic acid and adenosine.
83
New cards
Dormant capillaries
Capillaries that have no blood flow at rest due to closed sphincters.
84
New cards
Recruitment of capillaries
Increased perfusion pressure during exercise opens dormant capillaries, shortening diffusion distance and contributing a 2-3 fold increase in surface area.
85
New cards
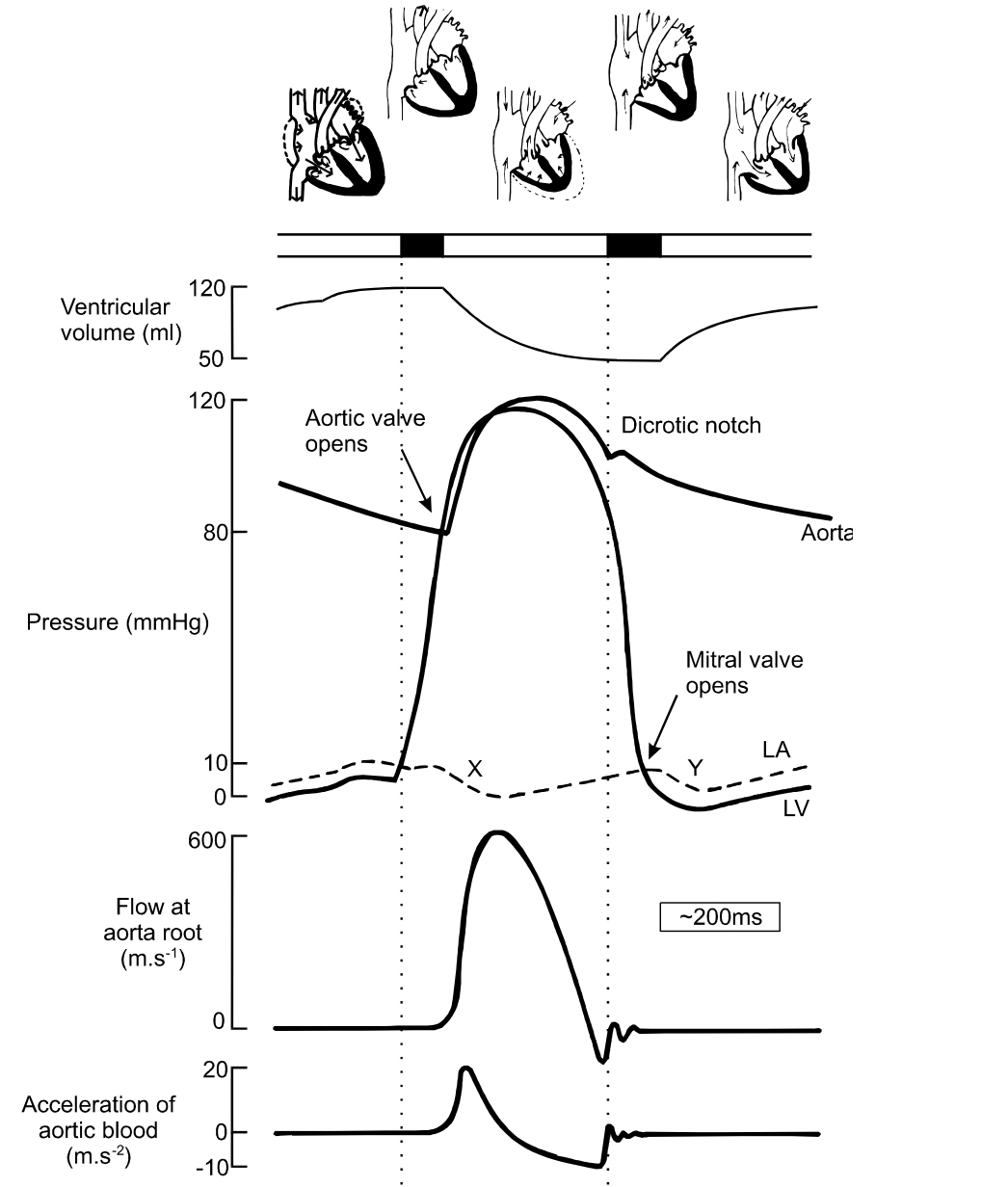
The cardiac cycle
Events associated with blood flow through the heart during one complete heartbeat. Systole, diastole, atria.
86
New cards
1. Atrial systole
Atria contract synchronously to provide the ventricles with last 20% of blood through the AV valves.
87
New cards
Atrial kick/boost
Additional blood forced into ventricles by atria
88
New cards
Jugular vein pulse
Seen due to the retrograde movement of blood into the venae cavae when the atria contract. (In the neck)
89
New cards
2. Isovolumetric contraction
Ventricular contraction without a change in ventricular volume. Forces the AV valves closed, pressure builds up.
90
New cards
3. Ventricular ejection
Pressure is generated by the ventricles, opening the semi-lunar valves (aortic valve on the left). High pressure blood is forced into the arteries, displacing low-pressure blood into the vasculature. Arterial pressure increases (blood enters faster than it can leave).
91
New cards
4. Isovolumetric relaxation
Ventricles begin to relax, rapid fall in ventricular pressure. Small amount of blood flows backwards closing the aortic valve, causes the dicrotic notch. Final third of ventricular blood flows away due to momentum.
92
New cards
Dicrotic notch
Brief rise in arterial pressure caused by closing of the aortic valve.
93
New cards
Stroke volume
Overall change in ventricular volume between ventricular ejection and Isovolumetric relaxation.
94
New cards
5. Late diastole
Both sets of chambers are relaxed and ventricles fill passively. End of cycle.
95
New cards
Phonocardiogram
Heard via auscultation through a stethoscope. First ‘lub’ is closure of AV valves. Second ‘dub’ is closure of semi-lunar valves.
96
New cards
Electrodes
Detect small changes in potential detected between different locations on the skin
97
New cards
Electromyogram
Recording of the burst of electrical activity taking place when the muscle is contracted.
98
New cards
Electroencephalogram
Electrodes are placed on the skull to record neuronal activity
99
New cards
Electrocardiogram
Process where small potentials (\~1mv) are recorded between different locations on the skin that reflect the underlying activity of the heart. The electrical events coupled to the mechanical events of the cardiac cycle.
100
New cards
Waves
Deflections above and below the baseline of an ECG.