Arterial Vascular Disease - Clin Med
1/83
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
84 Terms
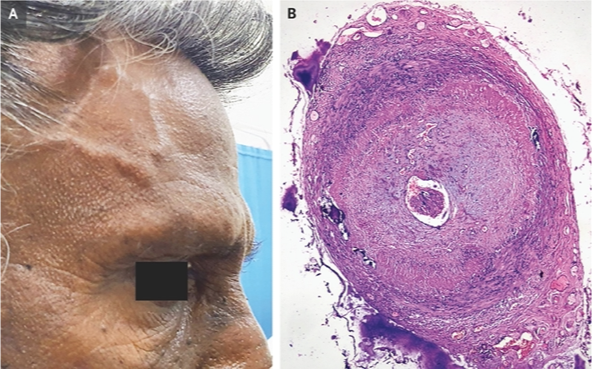
What does this refer to
A 65-year-old woman presents to the emergency department due to a severe headache and visual impairment in the right eye.
Her symptoms are associated with pain with chewing and proximal muscle morning stiffness.
On physical exam, she has decreased visual acuity of the right eye, scalp tenderness on the right, and an absent pulse in the right temporal area.
Laboratory testing is significant for an elevated erythrocyte sedimentation rate.
She is admitted and immediately started on systemic glucocorticoids.
Giant cell arteritis
What does this refer to
Giant cell arteritis
What does this refer to
Chronic vasculitis of large and medium sized vessels
Vascular involvement may be widespread
Most frequently involves cranial branches of arteries that originate from aortic arch
Also known as temporal arteritis
Giant Cell (Temporal) Arteritis

What does this refer to
Age greater than 50 years (peaks at 60-80)
Risk for blindness
More common in whites; rare in Hispanics
More common in Scandinavian descen
Clustering of illness may occur in families
Heavy smoking increases risk in women
F > M
Epidemiology Giant Cell (Temporal) Arteritis
What does this refer to
Unknown/idiopathic —> presumed to be autoimmune
T-cells and monocytes “recruited” to vessel wall = inflammatory response
Association with polymyalgia rheumatica (also autoimmune)
Infectious etiology has also been speculated
Etiology Giant Cell (Temporal) Arteritis
What does this refer to
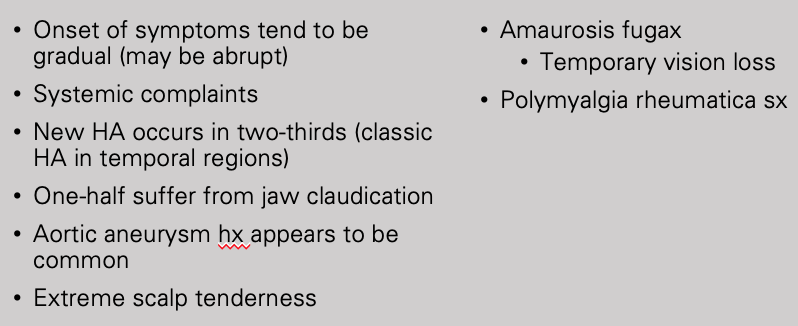
Clinical history Giant Cell (Temporal) Arteritis
What does this refer to
Palpate Pulses
Carotid
Brachial
Radial
Femoral
Pedal
Temporal artery abnormalities
Tender or thickened
Absent temporal pulse
Physical Exam of Giant Cell (Temporal) Arteritis

What does this refer to
Giant Cell (Temporal) Arteritis - (Visibly enlarged temporal artery)
What does this refer to
Headache
Scalp tenderness
Thickened temporal arteries
Jaw claudication
Acute visual loss
Weight loss, anorexia, fever, night sweats
Malaise, depression
Presenting symptoms of Giant Cell Arteritis
What does this refer to
Considered in age > 50 years old who has:
New headaches
Abrupt onset of visual disturbances
Symptoms of polymyalgia rheumatica
Jaw claudication
Unexplained fever or anemia
High ESR and/or high serum CRP
Diagnosis Giant cell (temporal) arteritis
What does this refer to
Migraine headache
Takayasu arteritis
Polymyalgia rheumatica (may co-occur with GCA)
Trigeminal neuralgia
Atherosclerotic Disease of Carotid Artery
Differential diagnosis Giant Cell (Temporal) Arteritis
What does this refer to
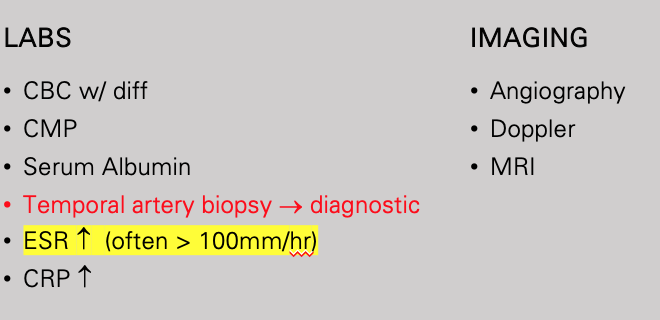
Workup for giant cell arthritis
What is the diagnostic test for giant cell arthritis
temporal artery biopsy
What does this refer to
Age (50 at time of onset)
Localized headache of new onset
Tenderness or decreased pulse of temporal artery
ESR > 50 mm/hour
Biopsy (revealing necrotizing arteritis with mononuclear cells or multinucleated giant cells)
Classification criteria Giant Cell (Temporal) Arteritis
What does this refer to
Rheumatologist
Ophthalmologist
Vascular surgeon
Neurologist
Clinical intervention (Referrals/Consults) Giant Cell (Temporal) Arteritis
What does this refer to
High dose glucocorticoids
Prednisone
Optimal dose for initial treatment uncertain
*Initial daily dose of Prednisone 40-60 mg of prednisone
Acetylsalicylic Acid (ASA)
Clinical management Giant Cell (Temporal) Arteritis
What does this refer to
Symptoms usually controlled promptly and tapering can begin once disease has been controlled adequately
After 2-4 weeks of high dose Prednisone
Is Patient asx and the ESR normal? YES taper
Begin tapering 2.5-5mg/day every 2 weeks to a dose of 20mg/day
Then decrease dose by 10% every 2 weeks to a dose of 10mg/day
Then decrease dose by 1mg/day every 4 weeks
Flares are the rule if tapered too quickly
Glucocorticoid tapering Giant Cell (Temporal) Arteritis
What does this refer to
SE of high dose/long term steroid use is decreased bone density
Prevent this decreased bone density with prophylactic tx
Prophylactic measures
Obtain a baseline bone density (when patient starts steroids)
Administer (1500 mg of calcium/800 IU of vitamin D-3 per day)
Consider bisphosphonates or hormonal therapy for osteopenia/osteoporosis
Prophylaxis of decreased bone density Giant Cell (Temporal) Arteritis
What does this refer to
Many patients tend to run a self-limited course over several months to several years
Dose can eventually be reduced and discontinued in the majority of patients
A few may need low dose prednisone for years
Complications
Blindness
20-50% have recurrence
Some patients have GCA and PMR at the same time
Prognosis/patient education Giant Cell (Temporal) Arteritis
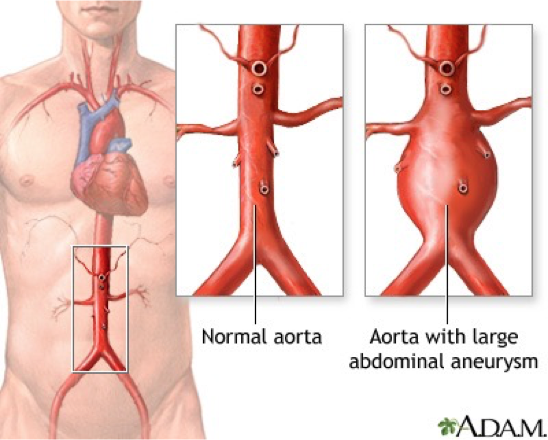
What does this refer to
A 67-year-old man presents to his primary care physician due to vague epigastric discomfort.
He denies it being associated with meals and reports that this pain occurred insidiously.
Medical history is significant for hypertension.
He has been smoking 1-pack of cigarettes per day for the past 30 years.
On physical exam, he has a pulsatile abdominal mass that is tender to palpation.
An abdominal ultrasound is performed, which demonstrates a 6 cm abdominal aortic aneurysm.
He is scheduled for an elective abdominal repair surgery for the following day.
Aortic aneurysm and dissection
What does this refer to
Aneurysm: arterial dilation
Diameter of that region is increased > 50% relative to normal aortic diameter
Normal diameter of the aorta at the level of the renal arteries is approximately 2.0 cm (range 1.4 to 3.0 cm) in most individuals
Diameter greater than 3.0 cm is generally considered aneurysmal
Aortic Aneurysm
What does this refer to
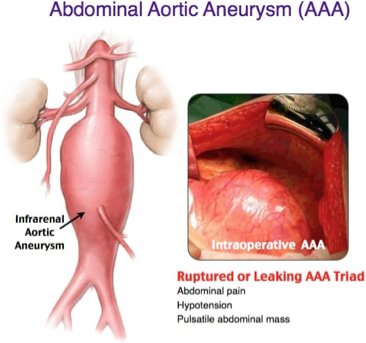
Abdominal (aortic aneurysm) (AAA)
Thoracic
Ascending (aorta)
Aortic arch
Descending (aorta)
Most Common types of Aortic Aneurysms
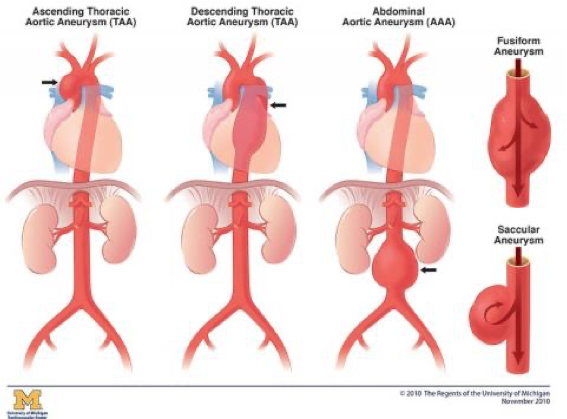
What does this refer to
Re
What aneurysm shape is the following
bulging on one side
Saccular

What aneurysm shape is the following
Bulging on all sides
Fusiform

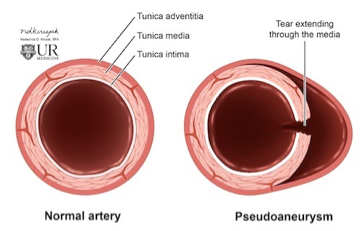
What aneurysm shape is the following
hematoma that forms as the result of a leaking hole in an artery
Pseudoaneurysm
What does this refer to
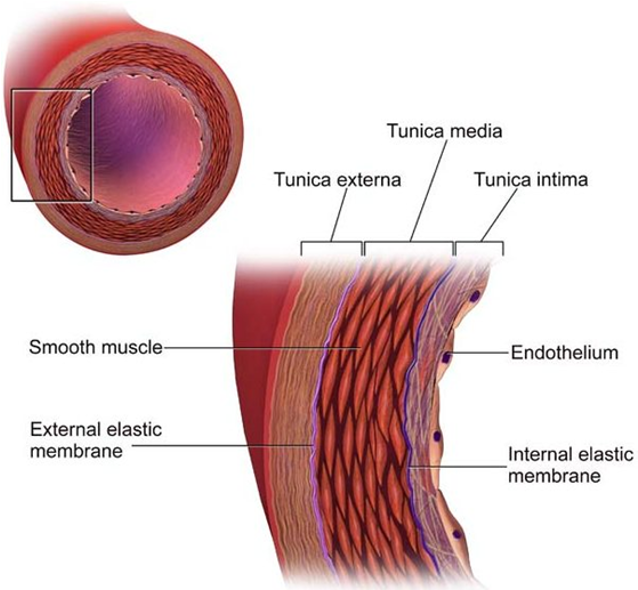
Weakening of the aortic wall
breakdown of the extracellular matrix proteins elastin and collagen (help vessels hold their structure/shape)
Congenital- anatomic defect
Atherosclerosis
HTN
DM
Smoking
Etiology/Pathogenesis/Risk Factors Aortic Aneurysm
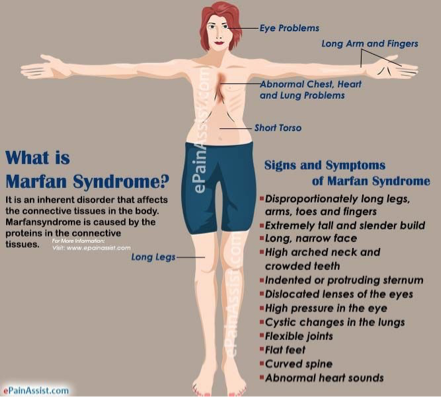
What does this refer to
Marfan’s syndrome
Risk factor of aortic aneurysm
What does this refer to
Occasionally may cause discomfort
More concern is risk of rupture
severe pain
massive internal hemorrhage
without prompt treatment, death occurs rapidly
Clinical history Aortic Aneurysm
What does this refer to
Communication through a “stalk” from the artery to the “sack”
Hematoma often develops within the sack
Pseudoaneurysm
What does this refer to
Often asx until dissection begins
Abdominal/chest pain and back pain
“Gnawing, ripping or tearing” abdominal pain
Compression of nerve roots
Associated sx:
Anxiety
N/V
Clammy skin
Tachycardia
Clinical history of aortic aneurysm
What does this refer to
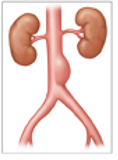
May be incidental on rad scans
Palpable, pulsatile abdominal mass
Groin pain
Skeletal hip pain
Other symptoms/findings of aortic aneurysm
What does this refer to
May be palpable as a pulsatile mass (AAA)
Bruit may be heard from turbulent blood flow (AAA)
“Gushing noise”
BP May be elevated followed by a sudden Hypotensive episode
Persons w/ Marfan syndrome are often males that are tall and “skinny”
Long extremities, fingers
Pertinent physical exam findings of Aortic Aneurysm
What does this refer to
Abdominal pain
Hypotension
Pulsatile abdominal mass
Ruptured or leaking AAA “triad” Aortic Aneurysm

What does this refer to
Pulsatile mass Aortic Aneurysm
What does this refer to
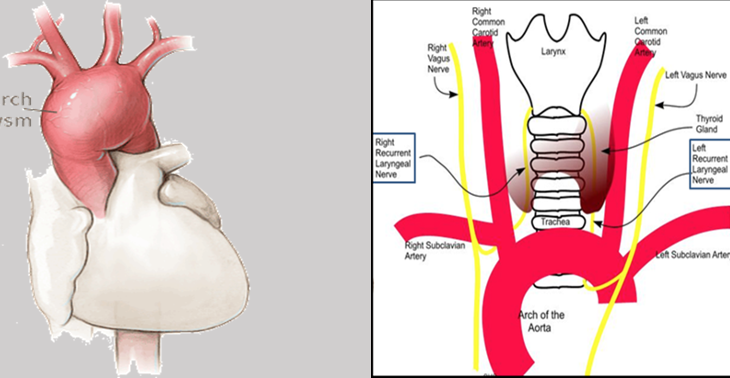
Pertinent historical findings/clinical sx (Thoracic) aortic aneurysm
What does this refer to
Angina Pectoris
Myocardial infarction
Pulmonary embolism
Pancreatitis
Gastroenteritis
Mechanical back pain
Differential Diagnosis Aortic Aneurysm
What test is gold standard and confirmatory of aortic aneurysm
Angiography
What does this refer to
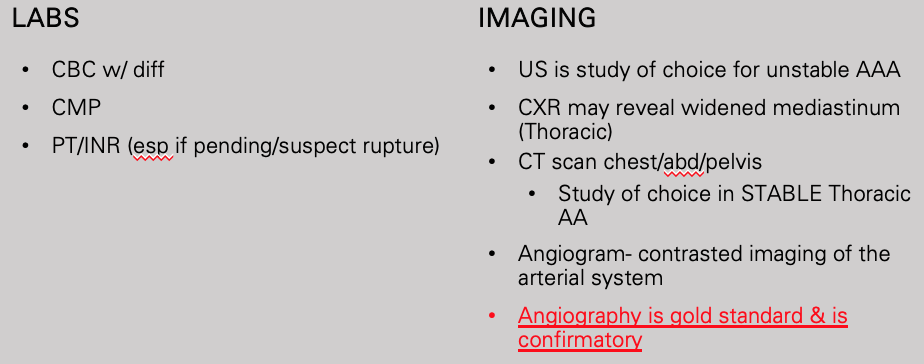
Workup aortic aneursym
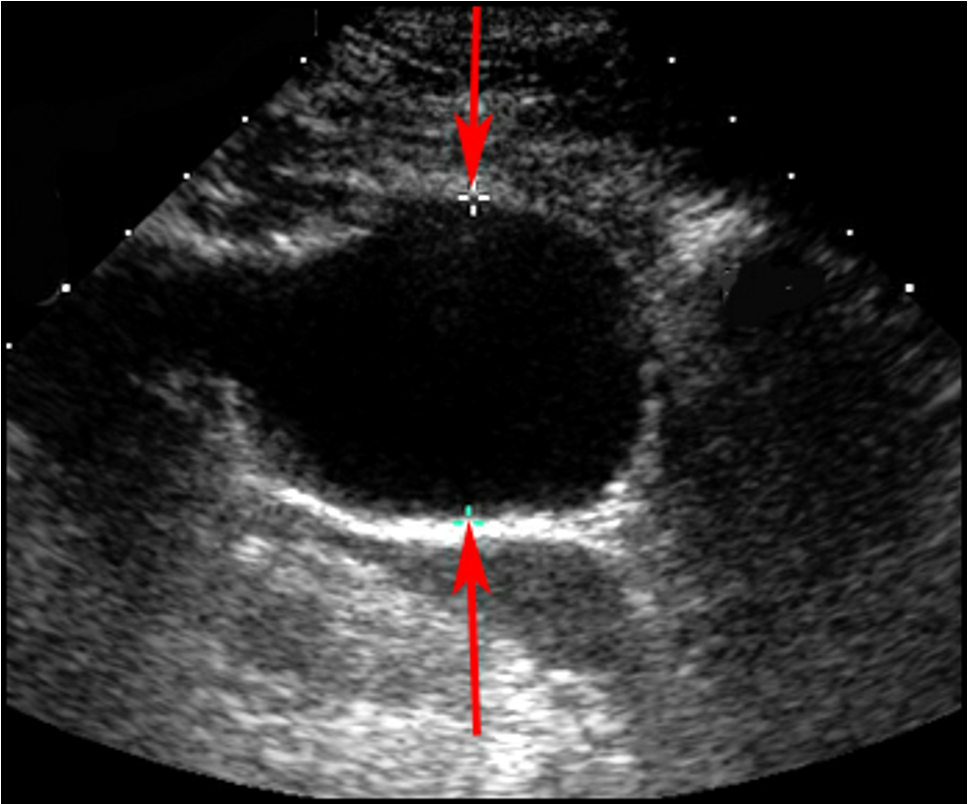
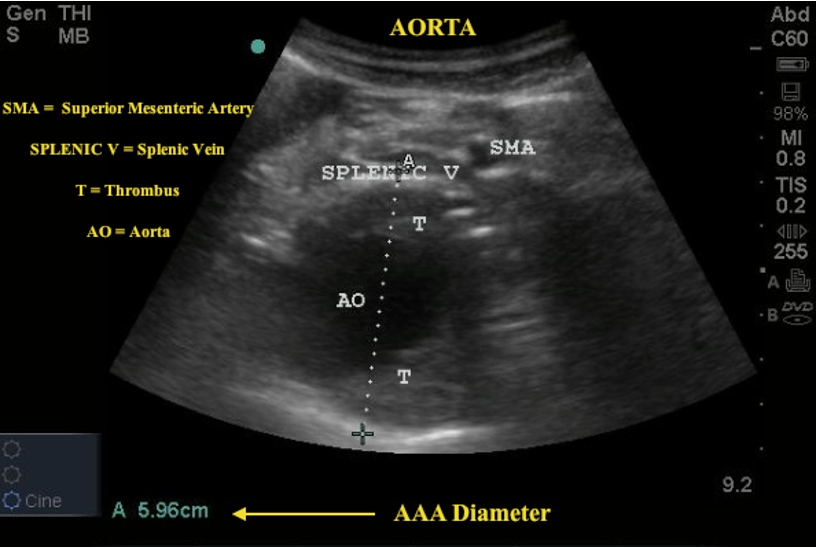
What does this ultrasound refer to
aortic aneurysm
What does this chest x-ray refer to
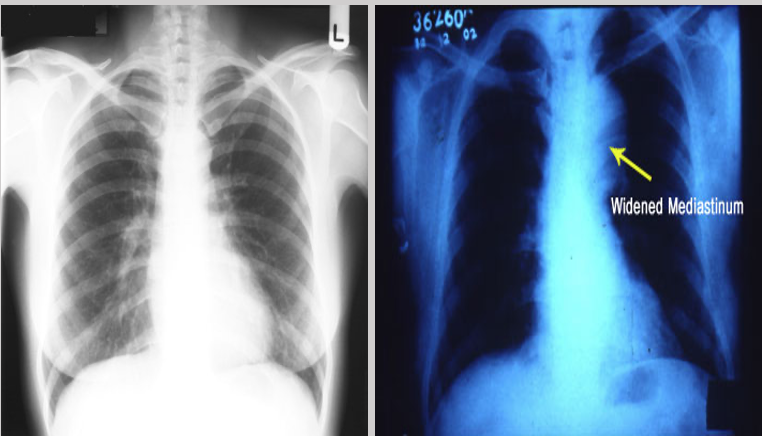
Thoracic Aneurysm
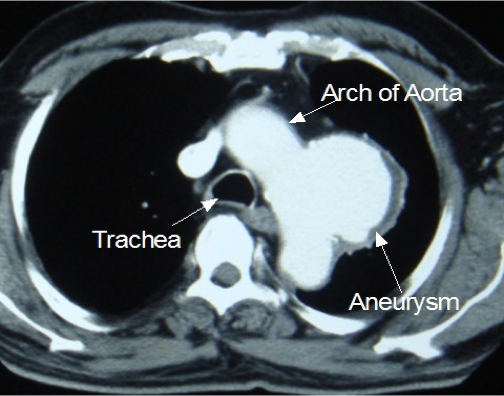
What does this CT refer to
Thoracic Aneurysm
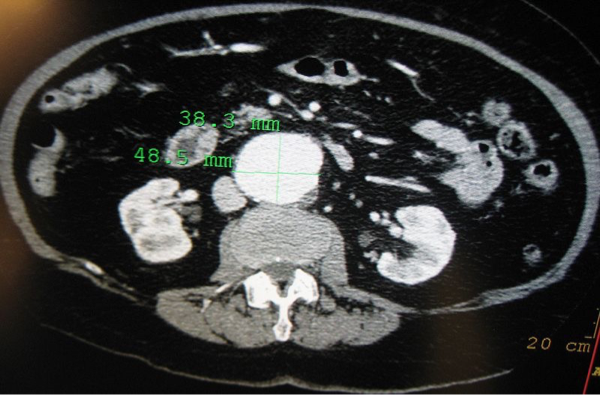
What does this CT refer to
Abdominal Aortic Aneurysm
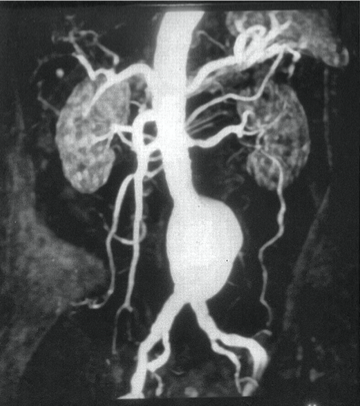
What does this angiogram refer to
Aortic Aneurysm
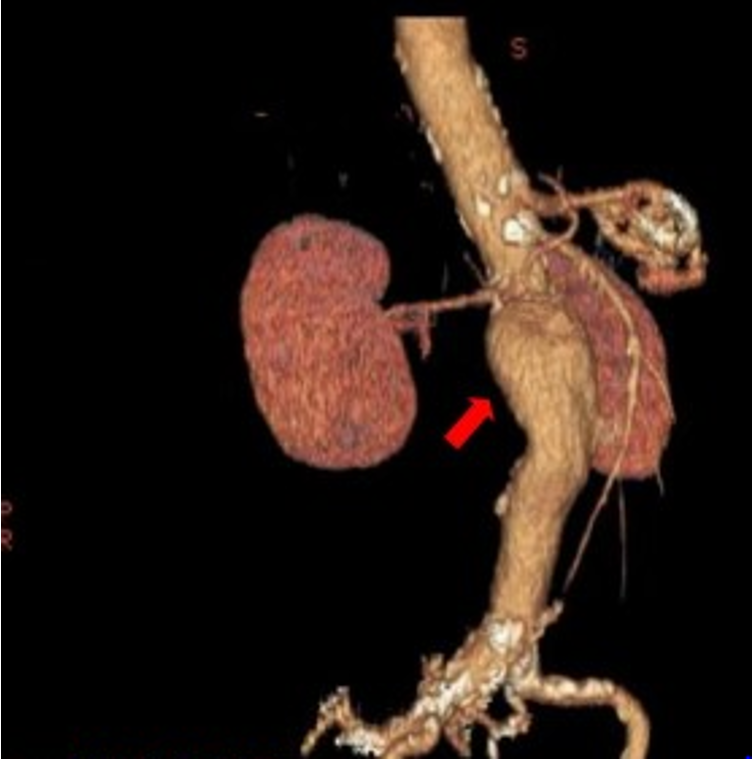
What does this CT angiography refer to
Aortic aneurysm
What does this refer to
Strict BP control
Smoking cessation
Refer to a vascular surgeon
Decide if surgical candidate
Recommendations about how to follow the patient clinically
Example might be ordering CT q 6 mo to monitor growth
Medical management of aortic aneurysm
What does this refer to
Prevent RUPTURE!
Aneurysms >5.5 cm (5 cm in good operative candidates) often surgically repaired
Symptomatic PTs with any size aneurysm often candidates for surgery
U/S every 6 months for aneurysm 4-4.5cm
U/S annually for aneurysms 3-4 cm
Thoracic aneurysm surgery more complex with greater risks
Surgery may be delayed until absolutely necessary
Surgical Management Aortic Aneurysm
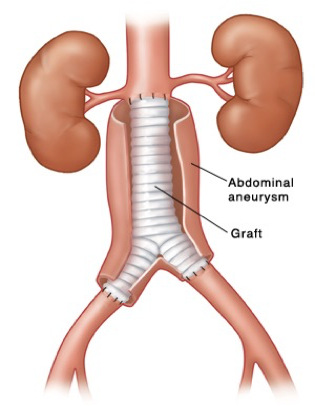
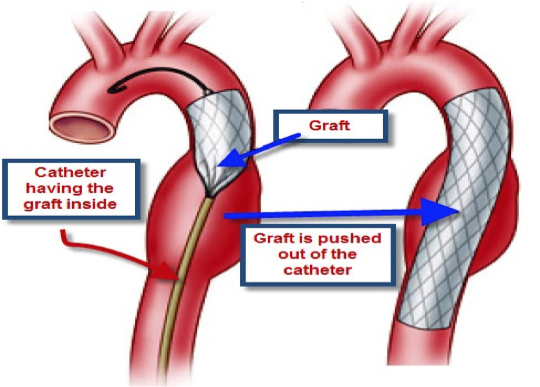
What does this refer to
Open surgical repair vs. endovascular
Open repair
Low or average risk of operative complications
Direct visualization
Endovascular repair
High risk of complications from open operations
Minimally invasive
Access usually through femoral arteries
Surgical candidates aortic aneurysm
What does this refer to
Open Repair Aortic Aneurysm
What does this refer to
Endovascular repair aortic aneursym
What does this refer to
1-time screening with ultrasonography
Men aged 65 to 75 yo
Men aged 65 to 75 years who have ever smoked
Screening/Health Maintenance Aortic Aneurysm
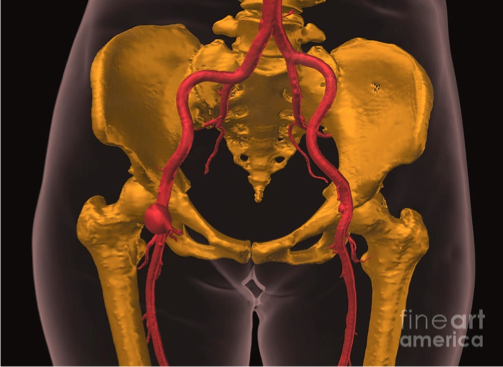
What does this refer to
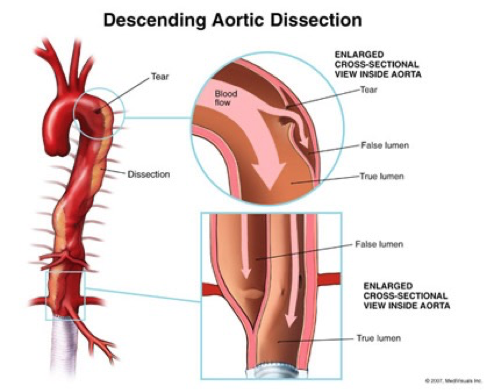
Aortic dissection
What does this refer to
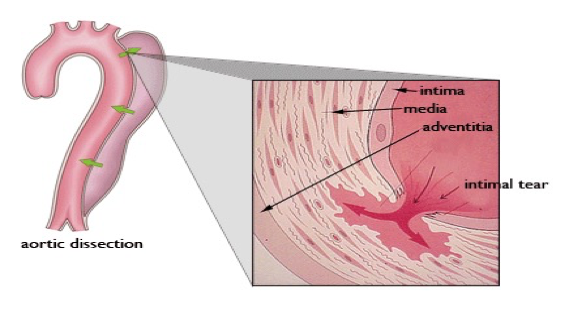
Tear in the inner wall of the aorta (intima) causes blood to flow into the middle layer (media) and force the layers apart
Aortic dissection
What does this refer to
Etiology/Pathogenesis/Risk Factors Aortic Dissection
What does this refer to (in terms of aortic dissection)
Most simplified classification system EVER!
Stanford system divided into:
Stanford Type A (proximal)
_______________
Involves the Ascending aorta
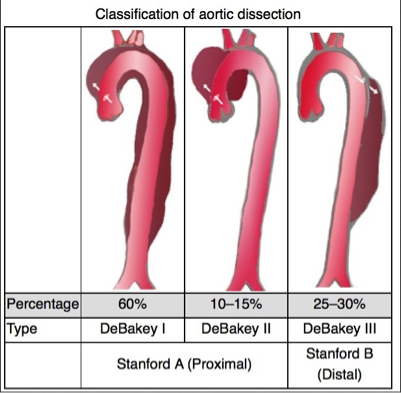
What does this refer to (in terms of aortic dissection)
Most simplified classification system EVER!
Stanford system divided into:
Stanford Type B (distal)
__________
Does NOT involve the ascending aorta
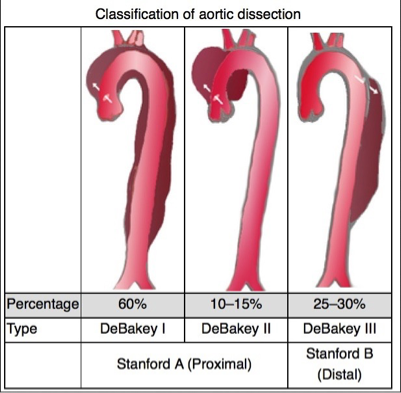
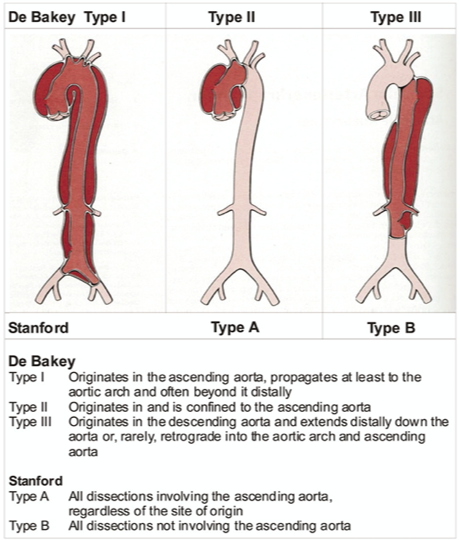
What does this refer to
Stanford Typing System Aortic Dissection
What does this refer to
Most commonly in the aortic arch or L subclavian
Always include in differential of chest pain
Typically c/o severe sharp, “tearing” (ripping) sensation in the chest or back
Be suspicious of dissection in high risk patients c/o pain radiating to the back
Pain may migrate as the dissection extends
Stanford Type A-chest pain anteriorly—may hear new murmur in aortic area
Stanford Type B-may see pain between scapular areas/back pain.
Neck or jaw pain may occur with involvement of aortic arch
Pertinent Historical findings/clinical Sx Aortic Dissection
What does this refer to
Peripheral extremity pulses may be decreased
Elevated BP in most cases (may see decreased BP)
Difference in pulse amplitude (strength)
Unequal BP in upper extremities (UE)
Aortic valve or ascending is affected new aortic regurgitation murmur
Pertinent Physical Exam Findings Aortic Dissection
What does this refer to
Aortic embolism
Acute MI
Angina Pectoris
Pulmonary embolism
Pancreatitis
Gastroenteritis
Mechanical back pain
Differential Diagnosis Aortic Dissection
What does this refer to
Widened mediastinum on CXR
Transesophageal echocardiography (TEE) esp if AKI or contrast allergy
CT scan Chest, Abd, Pelvis with IV Contrast when TEE cannot be quickly performed
Sonography SPEED protocol
Aortic angiography (MRI) is gold standard
Not universally available
Expensive
Workup aortic dissection
What does this refer to
SPEED
Sonographic Protocol for the Emergent Evaluation of (Aortic) Dissections
Combines TTE and abdominal aorta US
Abdominal aorta 6”
Xiphoid to bifurcation (iliacs)
Designed for patients too unstable to leave the ER for imaging
Workup – Speed Protocol Aortic Dissection
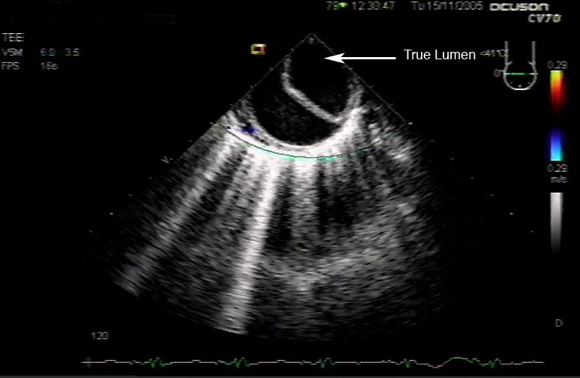
What does this refer to
Transesophageal echo Aortic Dissection

What does this CT scan with IV contrast refer to
Aortic Dissection

What does this CT chest refer to
Aortic Dissection
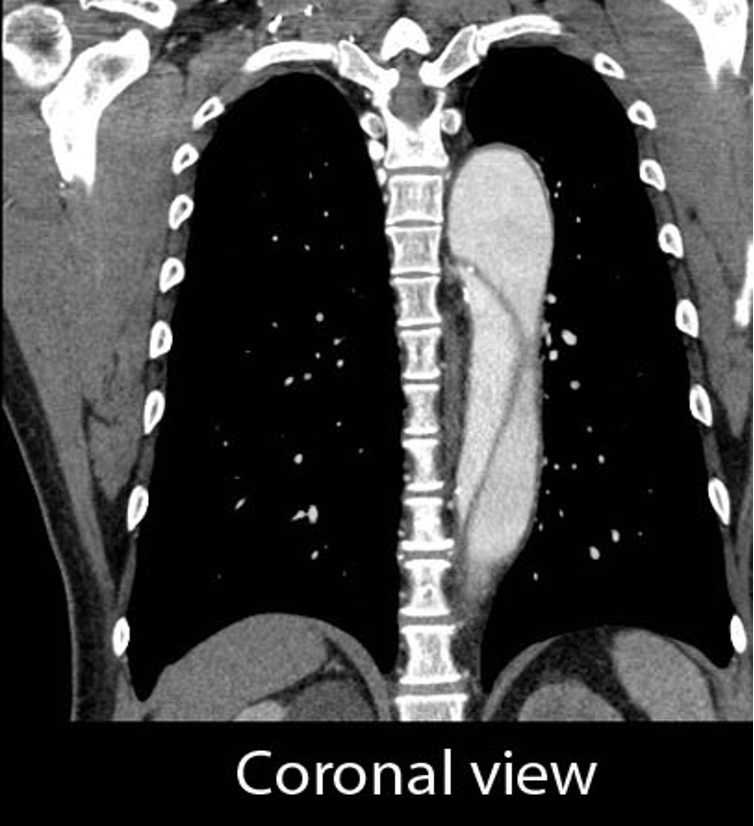
What does this coronal CT view refer to
Aortic Dissection

What does this angiography refer to
Aortic Dissection
What does this refer to
Acute dissection suspected
Labetalol and sodium nitroprusside IV typically used to aggressively lower BP
Lowest level that adequately supports cerebral, cardiac and renal perfusion
Goal is systolic BP 100-120mmHg within 20 mins
Hypotensive
IVF and vasopressors
Dopamine/Dobutamine
Epinephrine/Norepinephrine
Patients with a dissection that does not threaten organs may be observed with strict BP control
MUST be completely asymptomatic
At discretion of CT specialist
Cardiologist specializing in vascular repair
Beta blocker often used as first line
Medical Management Aortic Dissection
What does this refer to
Tx choice often depends on location
Stanford type A (ascending aortic) dissection
Immediate Open surgical mgmt superior to medical mgmt
Uncomplicated Stanford type B (distal aortic)
Medical mgmt preferred over surgical intervention
Repair if evidence of rupture or vessel occlusion
Medical management of aortic dissection
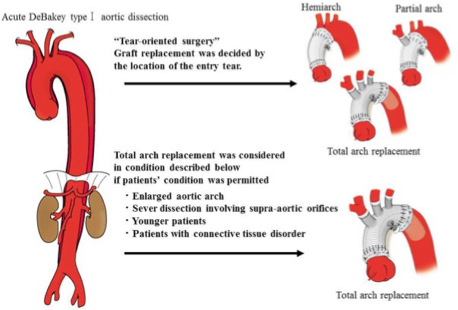
What does this refer to
Objective is often to resect (remove) the most severely damaged segments of the aorta, and prevent entry of blood into the false lumen
Graft inserted post resection
Surgical Management Aortic Dissection
What does this refer to
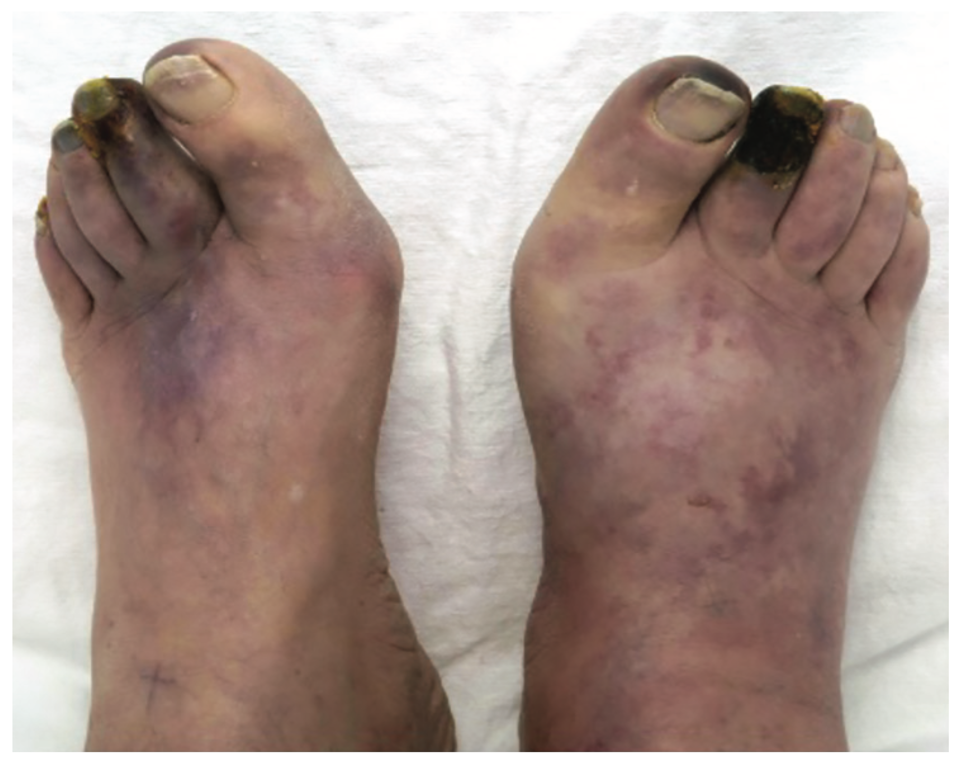
peripheral arterial disease
What does this refer to
A 50-year-old man presents to his primary care physician for pain in his lower legs with long walks.
He reports walking 10 blocks before feeling the pain and that it resolves with rest.
His medical history includes hyperlipidemia, hypertension, and diabetes.
His blood pressure is 145/80 mmHg, pulse is 90/min, and respirations are 18/min.
On physical exam, his distal pulses are faint.
His bilateral calves are dry and hairless with no peripheral ulcers.
His skin is cool to the touch, especially in his feet.
An ankle-brachial index is performed.
Peripheral vascular disease
What does this refer to
Atherosclerotic disease leading to peripheral artery obstruction
PAD regarded as a coronary heart disease risk equivalent
Peripheral Artery Disease (PAD)
What does this refer to
Age ≥70 years
Age 50-69 years with a history of smoking or diabetes
Age 40-49 with diabetes and at least one other risk factor for atherosclerosis
Known atherosclerosis at other sites (coronary, carotid, or renal artery disease)
Positive Family history
Smoking
HTN
HLD
M > F
AA > Caucasian
Epidemiology Peripheral Artery Disease (PAD)
What does this refer to
Risk factors
Similar to those for development of coronary atherosclerosis
Most often affects the popliteal artery
Atherosclerotic disease —> obstruction of peripheral arteries
Associated Conditions
Leriche syndrome —> aortoiliac occlusion
BLE claudication
PLUS impotence
PLUS lower extremity muscular atrophy
CAD
Etiology of peripheral artery disease (PAD)
What does this refer to
Progressive severity
asymptomatic
intermittent claudication
pain at rest
nonhealing wounds
ulceration
gangrene and threatened limb
Clinical history of Peripheral Artery Disease (PAD)
What does this refer to
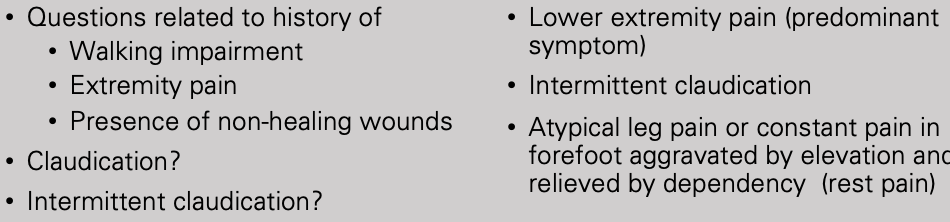
Physical exam peripheral artery disease (PAD)
slide 82