Final Weekly Recap
1/11
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
12 Terms
Week 11 – Practice Question 1.1
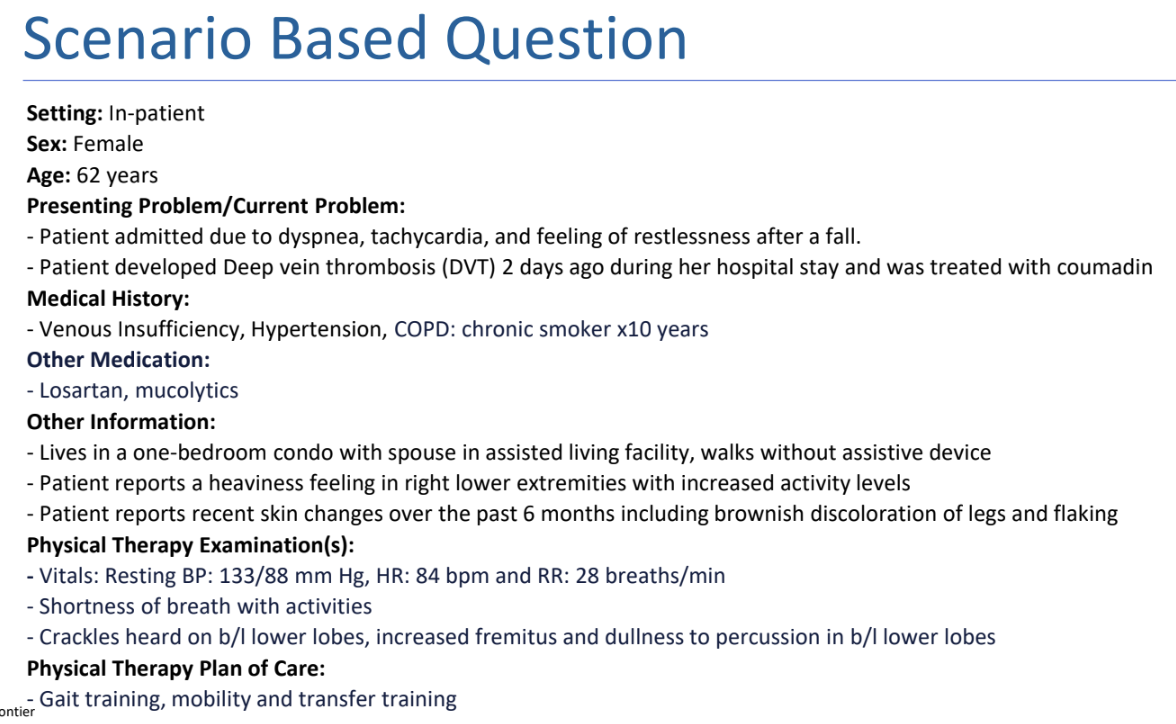
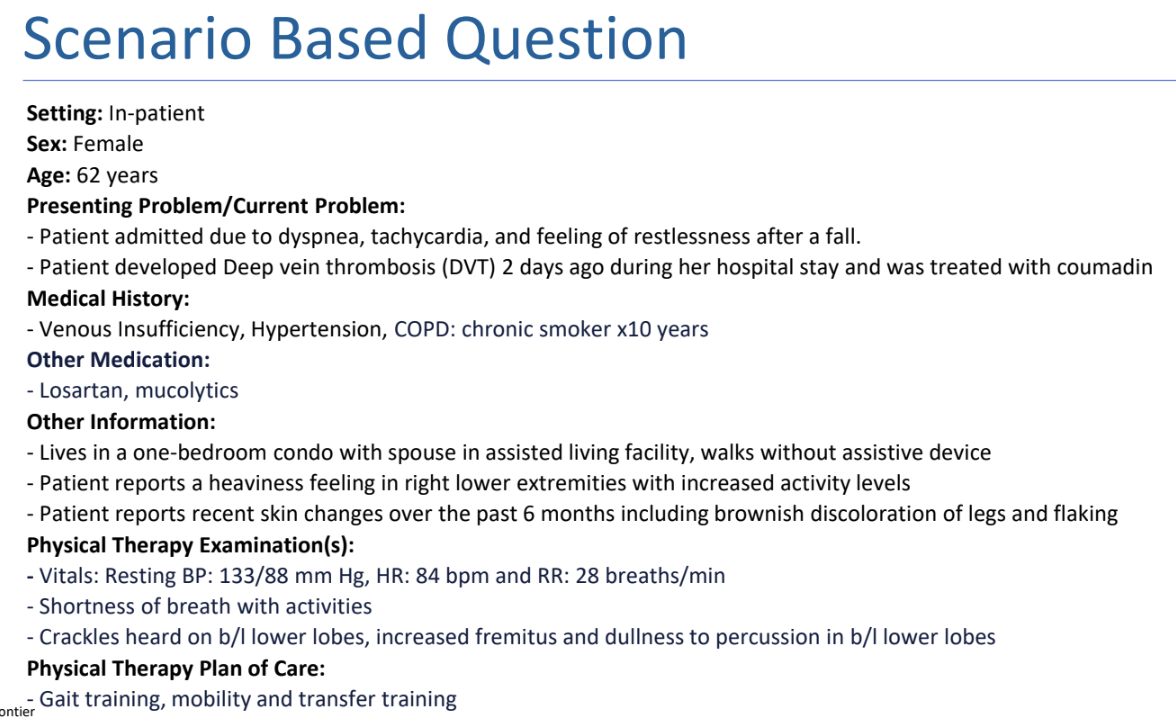
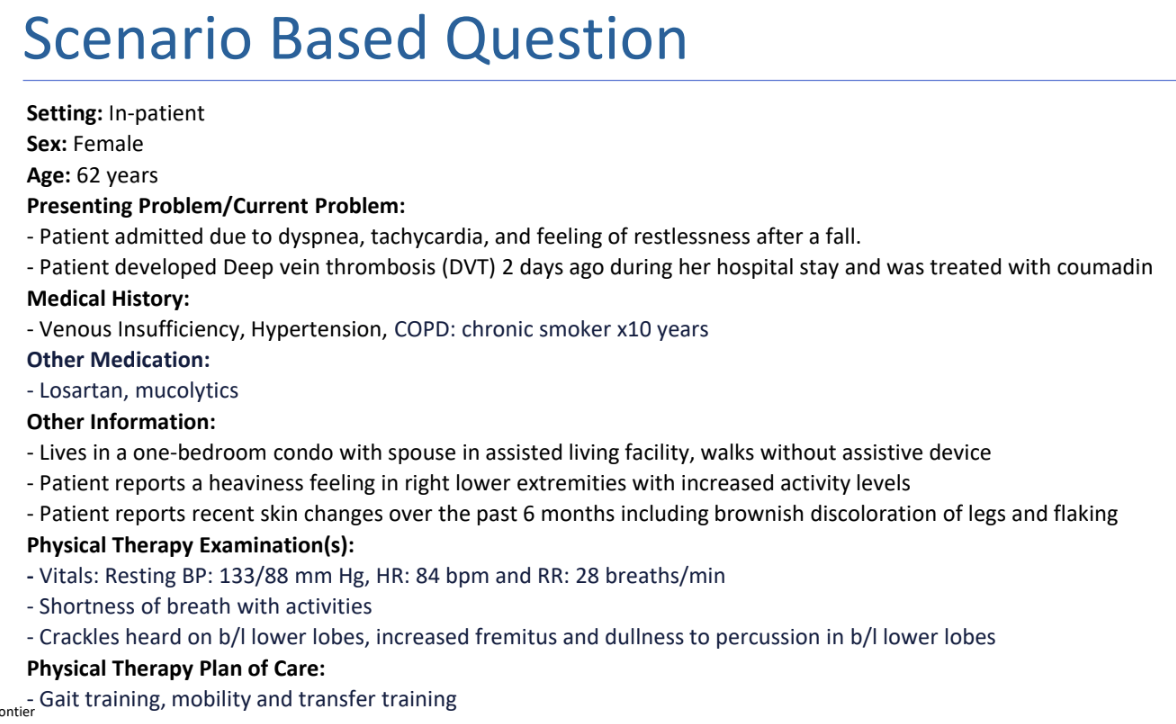
On reading the medical reports, the physical therapist sees that the International Normalized Ratio (INR) level is 2.5. What is the MOST APPROPRIATE step to be taken by the physical therapist?
A. Continue with the planned exercise routine
B. Stop exercises until the INR levels are corrected
C. Increase the exercise routine
D. Advice the patient
A. Continue with the planned exercise routine
RATIONALE: INR for 2-3 is normal for patients on warfarin and exercise can be continued
INR = International normalized ratio
INR: Normal: 0.9-1.1
For individuals on anticoagulants
>2.5 Guard against falls
>3.0 Risk for hemarthrosis (no closed chain activities)
>4.0 increase in exercise routine may be contraindicated or modified; discuss with physician
> 6.0 Bed rest till corrected
Week 10 - PRACTICE QUESTION 1.2
Which of the following physical therapy interventions is MOST appropriate to address the patient’s venous insufficiency (brownish discoloration of legs and flaking, heaviness in LE that increases with activity) ?
A. Perform ankle pumps in a seated position multiple times per day to facilitate venous return.
B. Prescribe a daily progressive walking program combined with elevation of the lower extremities during rest.
C. Implement cycle ergometry using a recumbent bike for 20 minutes to improve lower extremity circulation.
D. Initiate resisted lower extremity exercises in dependent positions to promote venous return.
B. Prescribe a daily progressive walking program combined with elevation of the lower extremities during rest.
RATIONALE: A walking program promotes calf muscle pump function, and elevation at rest helps reduce venous pressure. This is the most appropriate management for chronic venous insufficiency, especially post-DVT.
A) Ankle pumps can help with circulation, but they are not good as a stand-alone intervention especially in the sitting position (dependent position will not assist venous return)
B) While recumbent biking supports aerobic function, it may not assist the calf muscle pump as effectively as walking. Also, this mode may be too demanding for a patient with COPD and dyspnea.
D. Resisted exercises in dependent positions can worsen venous pooling and not facilitate venous return.
Week 10 – Practice Question 1.3
In addition to mobility and gait training, what else should the physical therapist’s PRIMARY focus with this patient be?
A. Getting the patient to quit smoking
B. Breathing reeducation to increase efficiency of ventilation
C. Airway clearance and secretion removal
D. Graded inspiratory muscle training
C. Airway clearance and secretion removal
RATIONALE: address the secretions removal;
B - Good but not needed at this time. Focus on symptoms.
C- Is right to address the current problems;
D- helpful in long run to strengthening respi muscles;
CLEAR Secretions first rest all is late and long term goal/treatment.
Week 9 – Practice Question 2
A patient presents to an outpatient clinic 8 weeks post right total knee arthroplasty. Which of the following interventions is BEST to implement at this stage of recovery?
A. Ankle pumps
B. Long arc quadriceps seated on plinth
C. Single-leg balance tasks
D. Gait training in parallel bars
C. Single-leg balance tasks
RATIONALE: At 6 weeks post-operative, the patient is typically in phase II of total knee arthroplasty rehabilitation. During this stage, the focus shifts toward closed chain strengthening, proprioceptive training, and aerobic conditioning. Single-leg balance tasks are appropriate to improve neuromuscular control and prepare the patient for dynamic functional activities.
Option A is appropriate for phase I to assist with circulation and reduce the risk of deep vein thrombosis.
Option B is an open chain strengthening exercise, generally emphasized earlier in rehabilitation.
Option D is used in the early post-operative period to promote ambulation with maximal support and is typically discontinued as the patient progresses to independent gait.
Week 8 – Practice Question 3
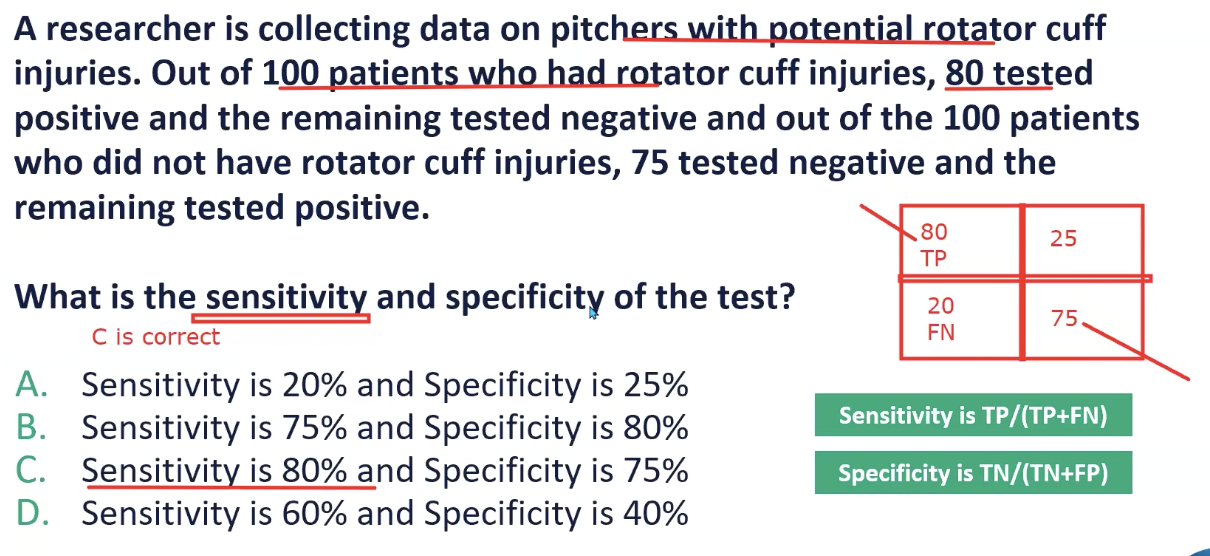
A researcher is collecting data on pitchers with potential rotator cuff injuries. Out of 100 patients who had rotator cuff injuries, 80 tested positive and the remaining tested negative and out of the 100 patients who did not have rotator cuff injuries, 75 tested negative and the remaining tested positive. What is the sensitivity and specificity of the test?
A. Sensitivity is 20% and Specificity is 25%
B. Sensitivity is 75% and Specificity is 80%
C. Sensitivity is 80% and Specificity is 75%
D. Sensitivity is 60% and Specificity is 40%
C. Sensitivity is 80% and Specificity is 75%
RATIONALE: Sn = TP/ TP+FN, Sp= TN/ TN+FP. TP = 80, FN=20, TN= 75, FP = 25
Sn is 80% and Sp = 75%
Week 7 – Practice Question 4
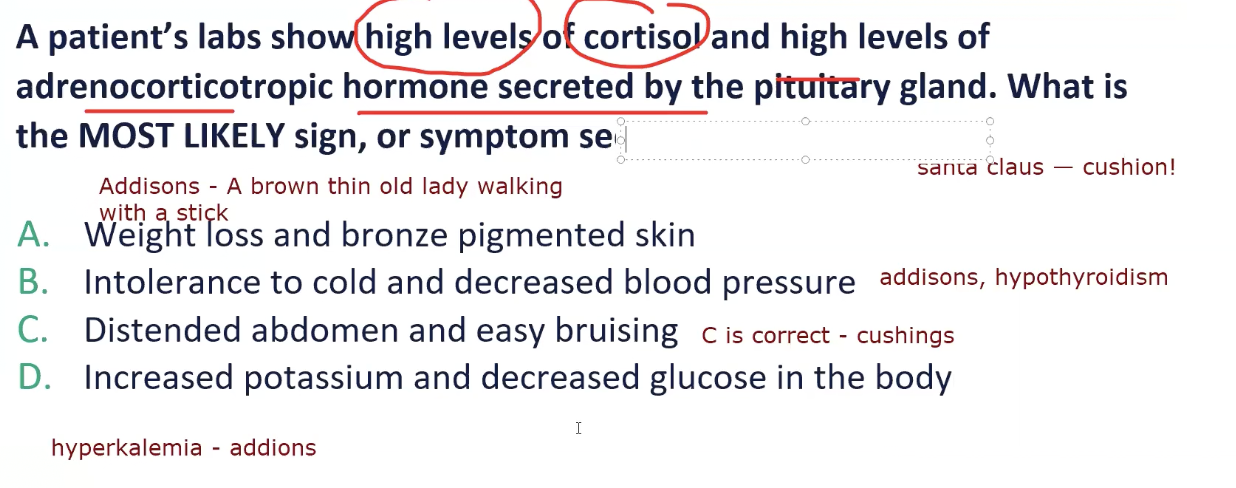
A patient’s labs show high levels of cortisol and high levels of adrenocorticotropic hormone secreted by the pituitary gland. What is the MOST LIKELY sign, or symptom seen in this case?
A. Weight loss and bronze pigmented skin
B. Intolerance to cold and decreased blood pressure
C. Distended abdomen and easy bruising
D. Increased potassium and decreased glucose in the body
C. Distended abdomen and easy bruising
RATIONALE: This presentation is consistent with Cushing’s disease, which is caused by excess secretion of adrenocorticotropic hormone (ACTH) from the pituitary gland, resulting in elevated cortisol levels. Classic signs of Cushing’s disease include truncal obesity, hyperglycemia, a rounded “moon” face, abdominal striae, easy bruising, proximal muscle weakness, and osteoporosis.
Option A: These findings are associated with Addison’s disease (adrenal insufficiency), which is characterized by decreased cortisol levels and often includes bronze skin pigmentation and weight loss.
Option B: Cold intolerance and hypotension are associated with Addison’s disease (adrenal insufficiency), not Cushing’s; could also be hypothyroidism, (Priyam’s husband)
Option D: Increased potassium and decreased glucose are also signs of Addison’s disease, not Cushing’s.
Week 6 – Practice Question 5
A physical therapist is working with a patient who had a stroke that has left their left upper extremity paralyzed. The patient tries to use their left arm to feed themselves. They continue to get frustrated and believe nothing is wrong with their left arm. Based on the patient’s response, which of the following perceptual disorders do they MOST LIKELY have?
A. Unilateral neglect
B. Anosognosia
C. Right-left discrimination
D. Figure-ground discrimination
B. Anosognosia
RATIONALE: Unilateral neglect: is the inability to register stimuli from one side of the body or environment.
Anosognosia: lack of awareness or denial of paretic limb
Right left discrimination: inability to identify right and left sides of the body
Figure ground discrimination: inability to visually distinguish a figure from background
Week 5 – Practice Question 6
A patient with a transfemoral (above-knee) amputation is being evaluated during gait training. The physical therapist observes that the prosthetic knee collapses into excessive flexion during early stance phase. Which of the following prosthetic alignment modifications is the MOST APPROPRIATE to reduce this deviation?
A. Plantar flex the prosthetic foot
B. Move the prosthetic foot laterally
C. Increase the socket flexion angle
D. Dorsiflex the prosthetic foot
A. Plantar flex the prosthetic foot
RATIONALE: Plantar flexing the prosthetic foot shifts the ground reaction force (GRF) anterior to the prosthetic knee, promoting a more stable extension moment during early stance. This adjustment reduces excessive knee flexion and helps prevent knee buckling, which is a common issue in transfemoral amputees when the foot is too dorsiflexed or misaligned posteriorly.
Option B (Move the prosthetic foot laterally) affects mediolateral balance but does not influence sagittal knee stability.
Option C (Increase the socket flexion angle) may increase the flexion moment, further exacerbating the knee collapse.
Option D (Dorsiflex the foot) increases the knee flexion moment, worsening the deviation.
Week 4 – Practice Question 7
A patient presents with swelling in the lower legs that has progressively worsened over the past few years. The swelling is symmetrical and spares the feet. There is no history of trauma or surgery, and elevation has not improved the symptoms. On examination, the feet are unaffected, the skin appears smooth, the edema is non-pitting, and joint range of motion is normal. Which of the following is the MOST LIKELY diagnosis for this patient?
A. Lymphedema
B. Deep vein thrombosis
C. Lipedema
D. Chronic venous insufficiency
C. Lipedema
RATIONALE: Lipedema is characterized by symmetrical, non-pitting edema that typically affects the lower extremities while sparing the feet. It presents without skin discoloration or fibrosis and is often associated with a sensation of heaviness. The chronic progression and lack of response to elevation are also consistent with lipedema.
Option A: Lymphedema commonly starts distally, including the feet, and is usually asymmetrical. It often presents with pitting edema in early stages and may progress to fibrosis and skin changes.
Option B: DVT generally presents with acute, unilateral swelling, pain, and warmth, typically following trauma, surgery, or periods of immobility all of which are absent here.
Option D: Chronic venous insufficiency can present bilaterally, but the edema is typically pitting and associated with skin changes such as hyperpigmentation or ulceration. It also tends to improve with elevation, which this patient does not report.
Week 3 – Practice Question 8
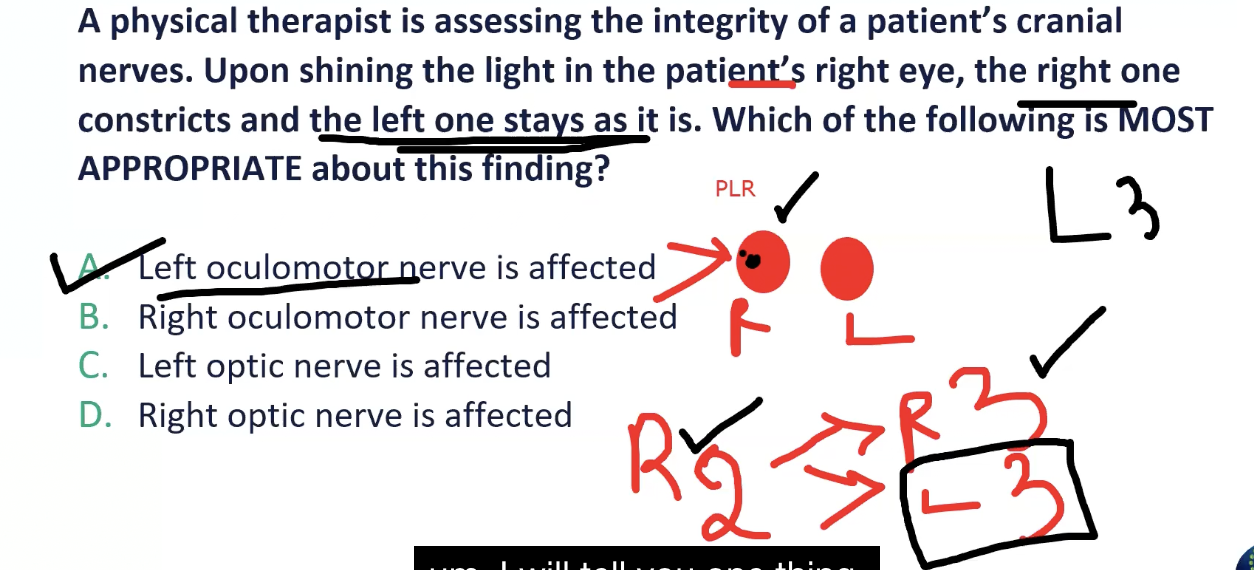
A physical therapist is assessing the integrity of a patient’s cranial nerves. Upon shining the light in the patient’s right eye, the right one constricts and the left one stays as it is. Which of the following is MOST APPROPRIATE about this finding?
A. Left oculomotor nerve is affected
B. Right oculomotor nerve is affected
C. Left optic nerve is affected
D. Right optic nerve is affected
A. Left oculomotor nerve is affected
RATIONALE: When optic nerve is affected, shining light in ipsilateral will lead cause an abnormal response in both eyes. When oculomotor nerve is affected, it will cause an abnormal response on the ipsilateral side only.
Week 2 – Practice Question 9
An athlete is seven weeks status post-ACL reconstruction and has had an uncomplicated recovery process and is in the moderate protection phase of rehabilitation. Which intervention is the MOST APPROPRIATE currently?
A. Proprioceptive training including single leg stance on a BOSU ball
B. Plyometric training including single leg box jumps
C. Advanced agility drills including the figure-eight pattern
D. Sprint training on a treadmill with 10% incline
A. Proprioceptive training including single leg stance on a BOSU ball
RATIONALE: During an uncomplicated ACL recovery, the time frame is approximately 0-4 weeks in the maximum protection phase, 4-10 weeks in the moderate protection phase, and 11-24 weeks in the minimum protection phase. Plyometric training and advanced agility drills are initiated in the minimum protection phase while proprioceptive training is initiated in the moderate protection phase.
Week 1 – Practice Question 10
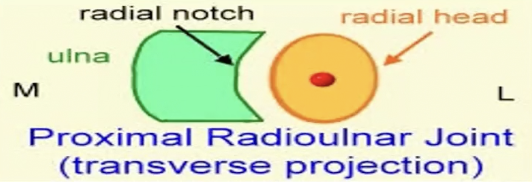
A patient presents with limited forearm pronation. Which mobilization technique should be performed at the proximal radioulnar joint to improve this motion?
A. Posterior glide of the radial head
B. Anterior glide of the radial head
C. Posterior glide of the ulna
D. Anterior glide of the ulna
A. Posterior glide of the radial head
RATIONALE: An Anterior glide of the radial head is used to improve forearm Supination at the proximal radioulnar joint.
A posterior glide of the radial head is used to improve forearm pronation at the proximal radioulnar joint.
The glide is given to the moving bone, which is the radius. The mnemonic to recall this is Proximal Radioulnar Joint: “PPP” → Proximal, Pronation and Posterior glide