MRAD 2410: Module 2 (Tubes & Lines)
1/113
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
114 Terms
list the 2 types of specialty catheters
central lines/central venous catheters (CVCs), pulmonary artery flow directed catheters (PACs)
structurally, what is a central line
a long flexible catheter
where are CVCs inserted into (3)
through the skin and into the SVC, the cavo-atrial junction, or within the RA
role of CVCs
allow for long term infusions of meds
what type of patients require CVCs
those in critical condition + requiring continuous support with multiple IV meds
T or F: CVCs allow for large volumes of fluid boluses
true
why are CVCs a useful method for delivering medicine
many meds are irritating to peripheral blood vessels
list the 3 categories of CVCs
non-tunneled catheters, tunneled catheters, peripherally inserted central catheter
purpose of non-tunneled catheters
allow for fast and reliable venous access for meds and blood draws
describe now NTCs are inserted at bedside
inserted, then secured with a dressing until placement is confirmed
once NTC placement is confirmed, how are they secured
via sutures
which vessels are NTCs inserted into
subclavian or jugular veins
NTCs are inserted into either subclavian or jugular veins. which side of the body is preferred + why
right side; most direct path to the SVC
what are tunneled catheters used for
for patients that are well and physically able, but require ongoing venous access for outpatient therapies
list 3 common types of tunneled catheters
hickman lines, broviac lines, permacath catheters
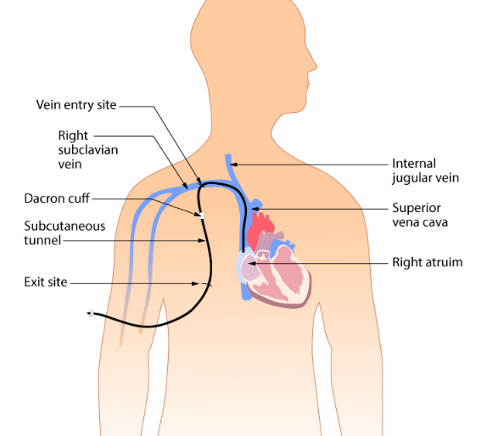
structurally/functionally, how is a tunneled catheter different from a non tunneled catheter
tunneled also go to the jugular or subclavian veins, but first it is tunneled through subcutaneous tissue beneath the chest skin
role of the tunnel of tunneled catheters
reduces the risk of infection, provides protection against accidental dislodgement
describe how the tunnel for tunneled catheters is created
inject local anesthetic by making two small incisions; one at the vein entry site and one 2-3 inches below the clavicle. skin is separated from underlying tissue = the tunnel. catheter is positioned in the vein and some is threaded through while the rest remains outside the skin
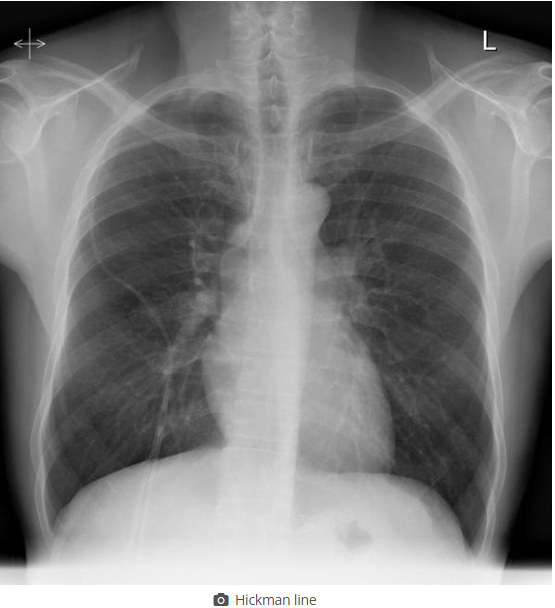
what is this
tunneled catheter (CVC)
a port-a-cath line is a type of tunneled catheter. describe how it’s structure is unique
contains an implantable port rather than an external port. it is sutured in place beside the ribcage, and the pt will not have any part of the catheter dangling
peripherally inserted central catheters (PICCs) are a type of CVC. describe the insertion site
upper arm and into the basilic vein
role of PICCs
for long or short term use for pts who are mostly well but require vascular access for treatment
benefits of PICCs
reduced infection rates compared to other CVCs, have reduced risks during insertion, and are easy for the pt to take care of
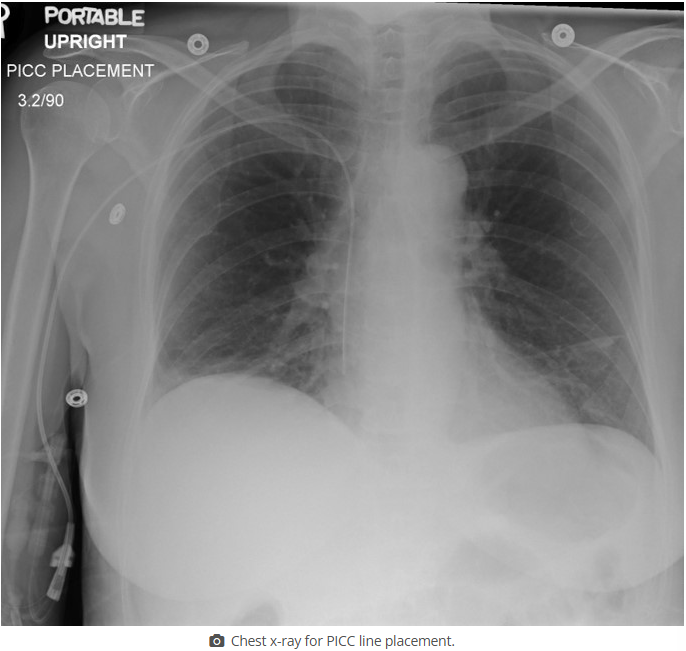
what is this
PICC
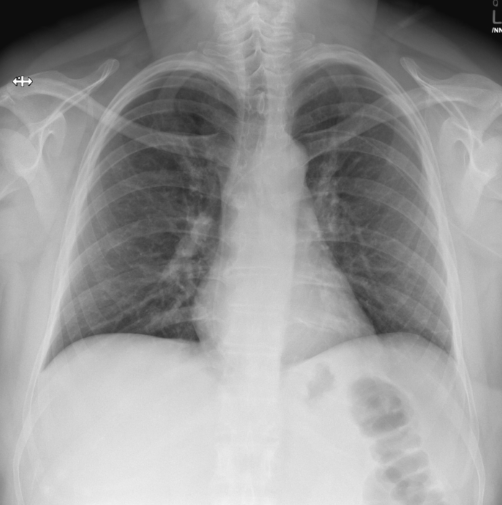
which catheter type does this image show (be specific)
non tunneled CVC
what is the entry point shown in this image for a non-tunneled CVC
subclavian vein
what type of catheter is shown in this image (be specific)
non-tunneled CVC
what is the insertion point shown for this non-tunneled CVC
jugular vein
what catheter type is shown in this image (be specific)
tunneled CVC
what catheter type is shown in this image (be specific)
PICC (type of CVC)
how do we see CVCs on xrays
they all have a radiopaque strip
what must a tech pay attention to when doing a CXR to confirm CVC line placement
don’t dislodge the line (it’s not secure yet), have good technique for visualization, position correctly so placement confirmation is accurate
what do techs do for follow up imaging after a CVC placement
we compare with previous images to see if the line has moved/withdrawn
T or F: techs are qualified to access central lines
FALSE
techs are not qualified to access central lines, but what can we use them for
injecting contrast media, however the radiology nurse or pts ward nurse must access all connections and disconnections
tip location for CVCs vary, but roughly where should they terminate
between SVC and RA
ideally, the tip of the CVC should be in the same vertical plane as which structure
SVC
what is the result if the catheter terminates before the SVC (ie in the subclavian or brachiocephalic veins)
higher risk of infection, thrombosis
role of catheters that terminate in the SVC
fluid injections
for SVC placements of catheters, what will this look like on a radiograph
tip ends 2cm above the level of the carina
for CVC placements in the SVC, what risks are there if the tip extends below the level of the carina
cardiac tamponade
role of the catheters that terminate at the cavo-atrial junction
long term use, infusion of meds that might be irritating (ie chemo)
for catheters that terminate at the cavo-atrial junction, what will the tip look like on a radiograph
ends approx 2 vertebral bodies below the level of the carina
T or F: typically we don’t want catheters to terminate in the atrium
true
why would catheters migrate to the RA over time
due to patient position over time
list 3 risks associated with atrial CVC placement
cardiac tamponade, tissue erosion, perforation
after CVC placement, which factor (other than time) could contribute to the migration of the catheter tip into the RA
lines are placed when the pt is supine or trendelenburg, so it might move once the pt is placed upright
in which scenario would we want the catheter to end in the RA
for hemodialysis
undiagnosed CVC malpositioning leads to ___ and ___
morbidity and mortality
give some examples of what issues result from undiagnosed CVC malpositioning (6)
vessel erosion, perforation, venous thrombis formation, subsequent migration, catheter dysfunction, cranial infusion rather than central circulation
most frequently malpositioned CVCs are within which vessel
jugular vein
most frequently malpositioned CVCs are within the jugular vein. describe this
tip points up the vein rather than down towards the heart
where does the PICC line terminate in this image
RA
pulmonary artery flow directed catheters (PACs) are the second type of specialty catheter in this course. what is their role
measure cardiac output and BP within the heart
what type of patients need PACs
ones that require intensive monitoring (ie following open heart surgery, and pulmonary hypertension)
what does the info we get from PACs help us with
diagnosing heart failure, elevated stress on heart function, and monitoring oxygen saturation between both sides of the heart
T or F: PACs aid in continuous temp monitoring
true
T or F: PACs can deliver fluids + meds
true
brand name of PACs
Swan-Ganz catheter
which vessels are PACs inserted into (3)
subclavian, jugular, or femoral veins
where does the tip of the PAC end
RA
what do we do with the PAC once it’s in the RA
using a balloon tip, we direct it to the left or right pulmonary artery
what does a PAC look like radiographically
seen making a large U turn within the heart shadow, tip rests in the pulmonary trunk below the carina or is to the right/left of the carina in one of the pulmonary arteries
when are NG/OG tubes used
when the pt is unable to swallow safely
NG/OG tubes are used when a pt cannot swallow safely. when might this be (5)
declining consciousness, stroke, aphasia, cognitive decline resulting in poor nutrition, oral/esophageal tumor resulting in obstruction
how do we use NG tubes during an overdose
NG tube is inserted to suction gastric contents, or provide a neutralizing agent (activated charcoal)
T or F: prior to initial NG tube use, a CXR is done to confirm placement
true
how do we see NG and OG tubes on a radiograph
they have a radiopaque strip
during xrays, if a pt has an NG/OG tube that is being used for a feeding pump, what must we not do + why
don’t place them supine; increases risk of aspiration
describe NG/OG tube insertion and handling
the approx length is externally marked prior to insertion, then tube is lightly secured, then CXR is done to confirm placements. once confirmed, the tube is firmly secured with tape or neck ties
ideal NG tube position
tip should be at least 10cm past the gastro-esophageal junction
on an xray, where will the end of the NG tube be
10cm below the diaphragm, aka over the gastric bubble
complications of NG tubes (6)
tissue trauma, esophageal/mediastinal perforation, pneumothorax, aspiration, hemorrhage, rarely death
list 2 common mispositions for NG tube placement
tip entering the right bronchus, or looping back towards the larynx
describe the optimal appearance of an NG tube on an xray (not just where it ends)
should be // to the spine and slightly left of the SPs, enters the stomach at the diaphragm level, curves with the shape of the stomach and passes the gastric bubble, the weighted tip should point downwards and be slightly angled L/R

describe the incorrect NG tube placement
ends in the right bronchial tree

describe the incorrect NG tube placement
loops back within the esophagus

describe the incorrect NG tube placement
insufficient insertion; needs to be longer
where do chest tubes go
into the pleural space
role of chest tubes
remove fluid or air
what types of pts need chest tubes
those from ICU, CCU, or trauma, or non-acute pt with chronic lung pathologies where fluid builds up in the chest
where are chest tubes inserted
5th intercostal space + slightly anterior to the midaxillary line
what are chest tubes connected to outside of the body
drainage receptables or mechanical suction units
list the two types of chest tubes
large bore, small bore
what are large bore chest tubes used for
pneumothorax (air removal)
what are small bore chest tubes used for
fluid drainage
how are we able to see chest tubes on radiographs
they have a radiopaque strip
where in the body will large bore chest tubes terminate + why
superior/anterior portions of the pleural cavity; air rises
where in the body will small bore chest tubes terminate + why
inferiorly/posteriorly; fluid sinks
before positioning a pt with a chest tube, how are chest tubes secured and how do we move with them
they’re secured to the mattress via kelly clamps, so we remove the clamps before positioning
complications of chest tube insertion (4)
pneumothorax, surgical emphysema, tension pneumothorax, hemorrhage
role of pacemakers
maintain adequate heart rate; used when the natural pacemaker isn’t fast enough or if there is a block in the electrical conduction system
how do we program modern pacemakers
externally programmable, the cardiologist can set optimum pace mode for each pt
what are temporary PMs used for + give examples
treat short term heart problems; slow heartbeat from a heart attack, surgery, or overdose
what are permanent PMs used for
long term heart rhythm problems
how does the pacemaker work
provides low levels of electrical stimulation to the heart muscle; it can sense the pts heart rate and provide stimulation when needed
describe internal pacemakers
surgically implanted inside the pt chest
how big is the generator component of an internal pacemaker
size of a matchbox, weighs 20g
describe external pacemakers
bulk remains in a pocket created under the skin, the leads are placed transvenously
rules for 24h post insertion for pacemakers
pt cannot abduct or lift their left arm