The lens and the retina
1/105
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
106 Terms
What is the point of antior chamber acquired immune deviation?
it prevents the classic T helper response, as it would make scar tissue in the eye and reduce vision
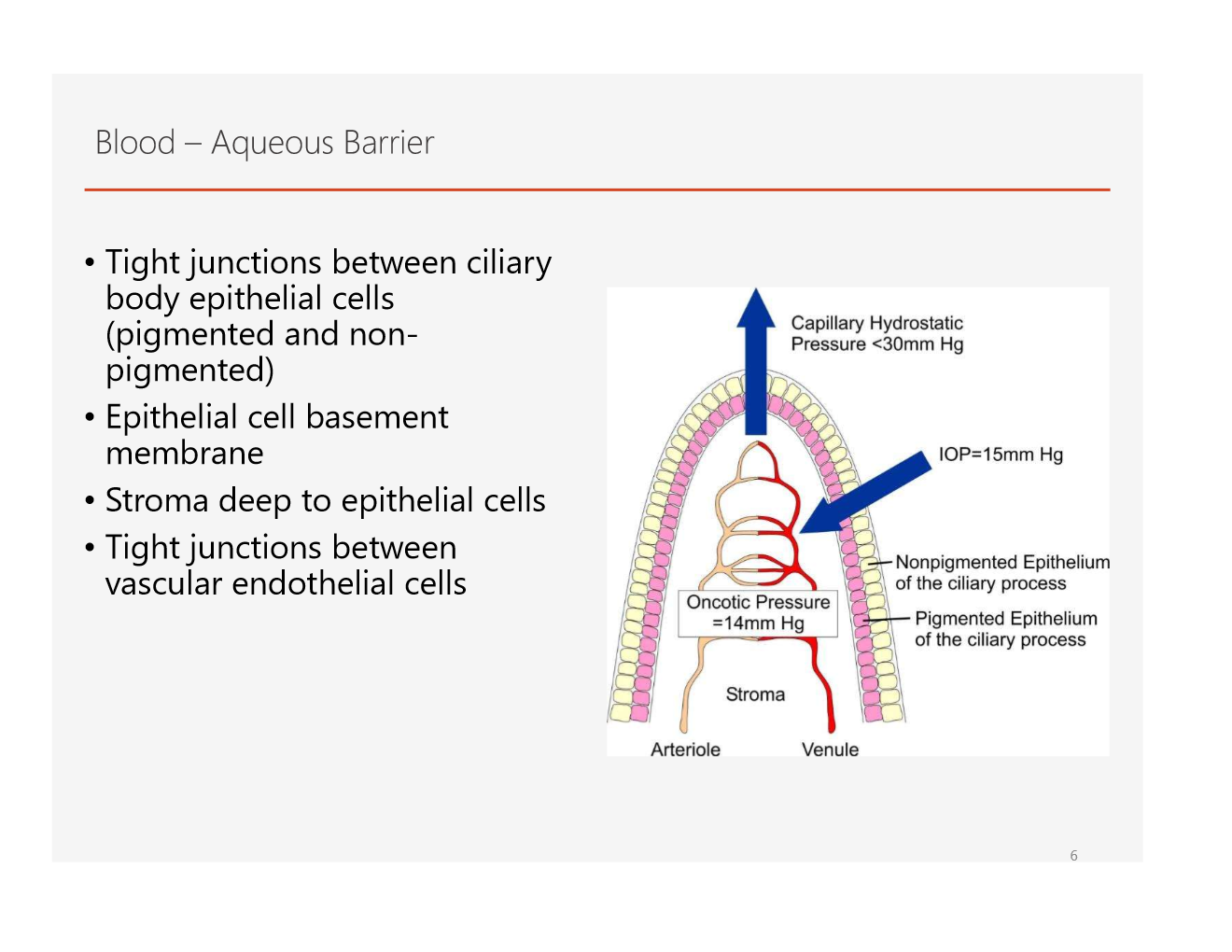
what are the layers of the aqueous barrier?
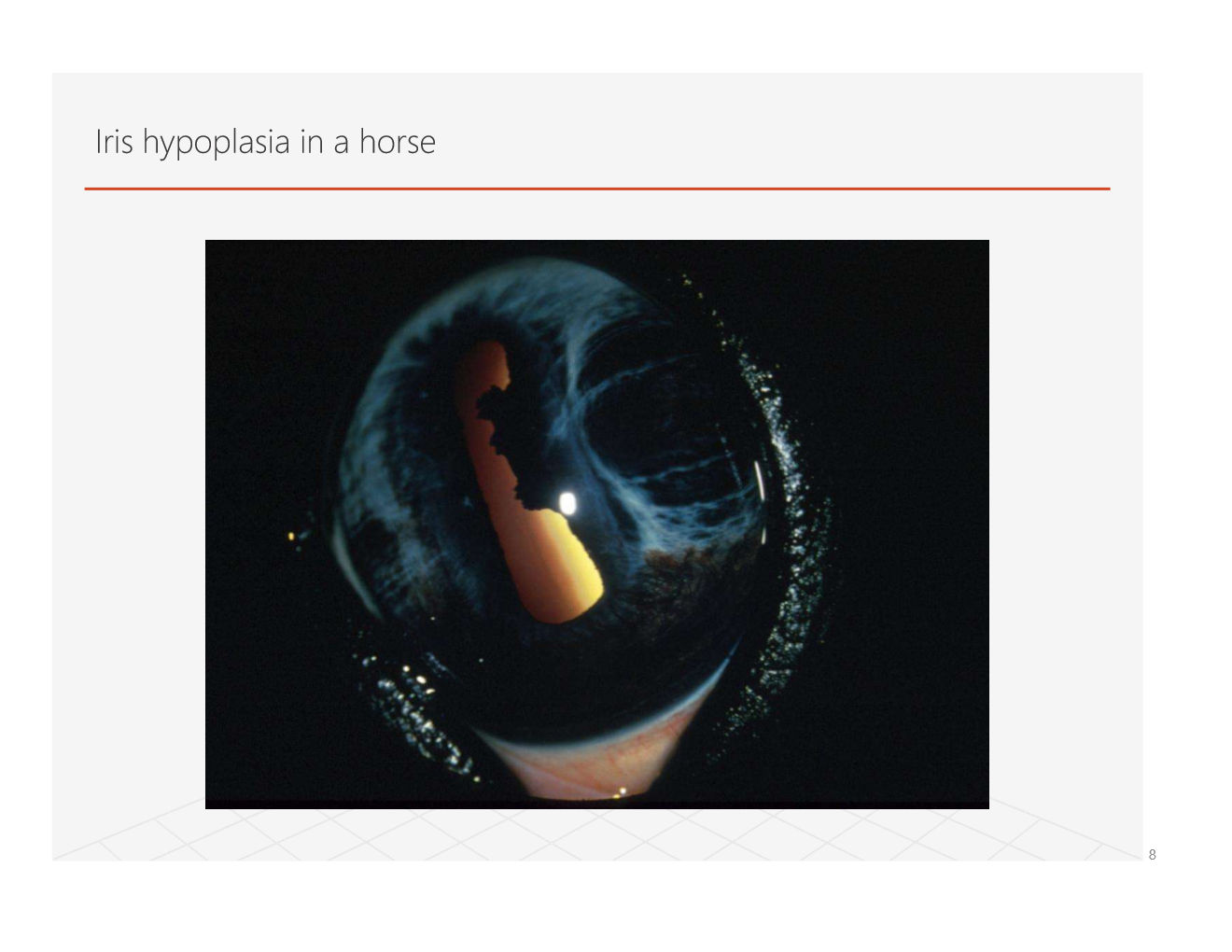
what are some congenital diseases of the eye?
heterchromia iridis
iris coloboma
aniridia and hypoplasia
persistent pupilary membrane
what causes persistant pupillary membrane(ppm)?
the mesenchymal tissue which is the vascular supply to develop the eye is abnomally formed. it doesnt regress completely because of this and remains at birth.
sometimes hereditary

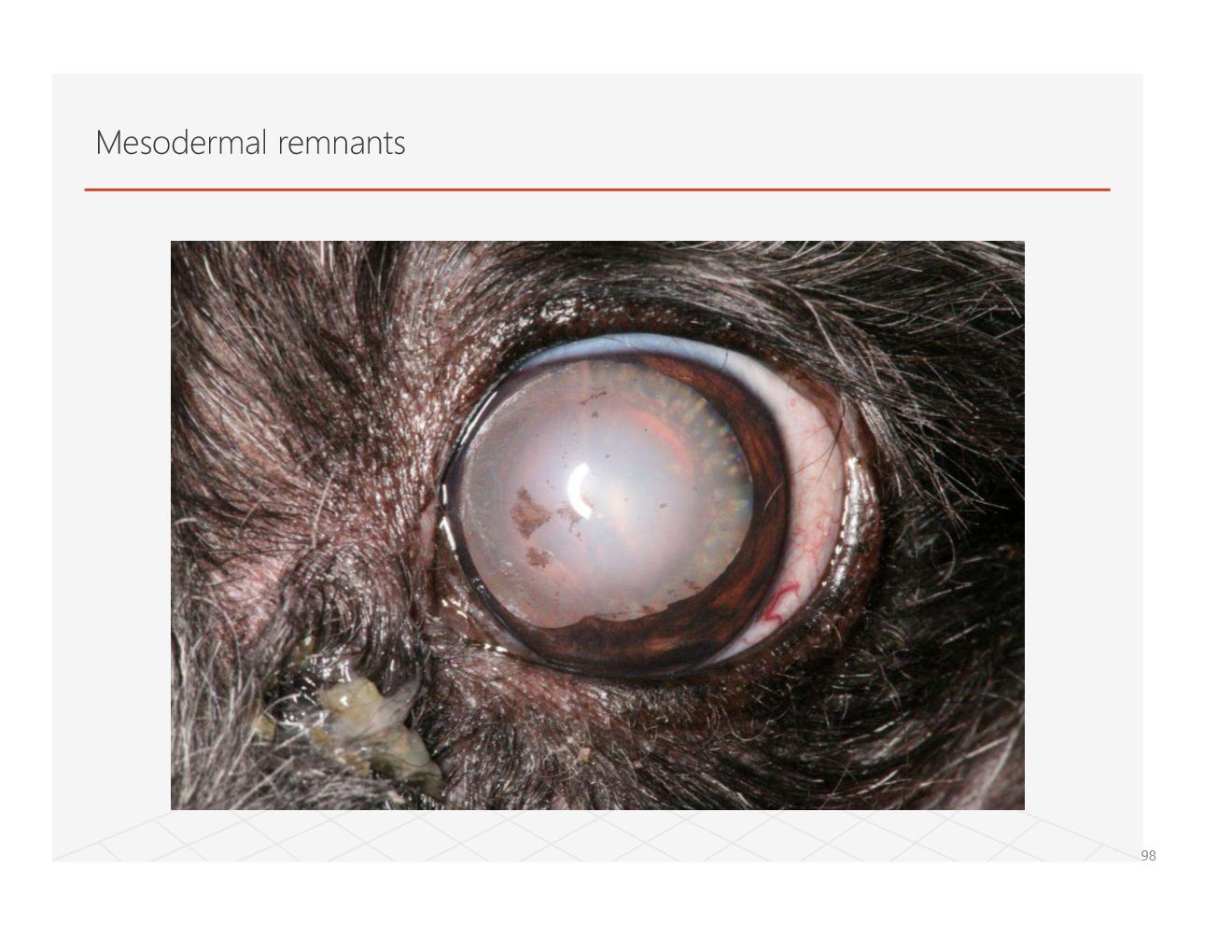
what is this?
PPM! visible focal cataract with origin from iris collarete. affects:
iris, lens, cornea
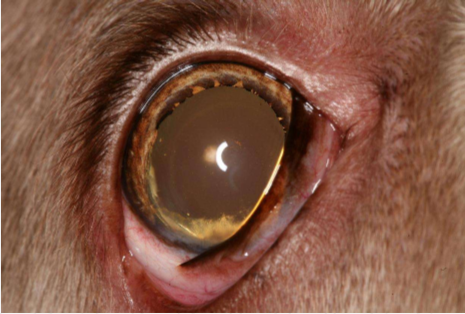
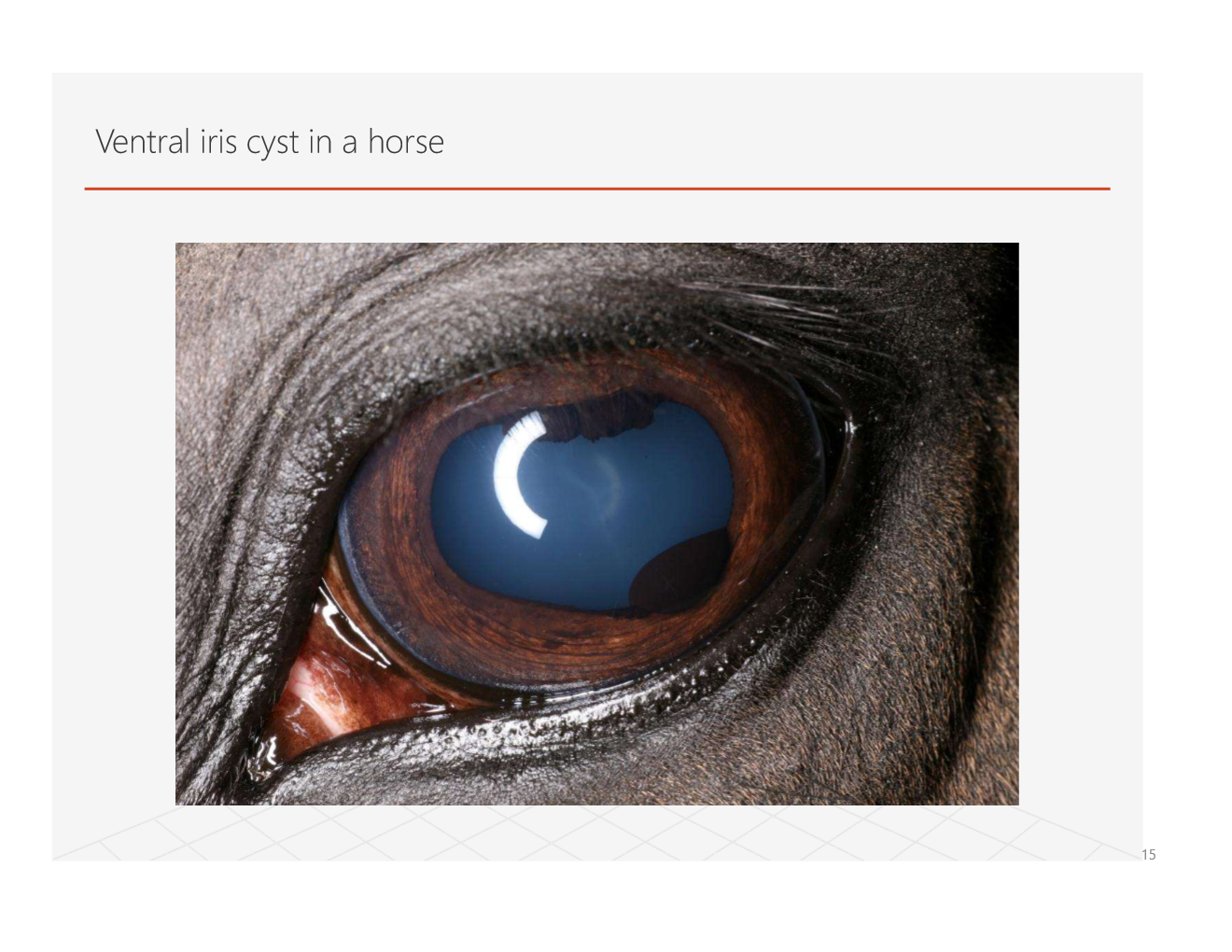
what are examples of degenerative eye changes?
senile iris atrophy, uveal cysts
Which of the two is this? how does it occur?
canine iris atrophy
the iris loses strength so the pupil can no longer constrict (iris thinning)
what is uveitis?
inflammation of the uveal tract
iris
ciliary body
choroid
etiopathogenesis of uveitis?
primary disease
secondary to lens, scleral, or corneal damage
primary ocular disease (endogenous)
secondary to systemic neoplasia, infection, or immune mediated disease (exogenous)
What role does occular tissue have in inflammation?
blood-aqueous barrier
antioxidants in aqueous humor
Anterior Chamber-Associated Immune Deviation (ACAID)
lack of intrinsic lymphatic system
what are the phases of inflammation?
active
redness, heat, exudate, pain, loss of function
sub-acute
chronic
what are clinical signs of uveitis?
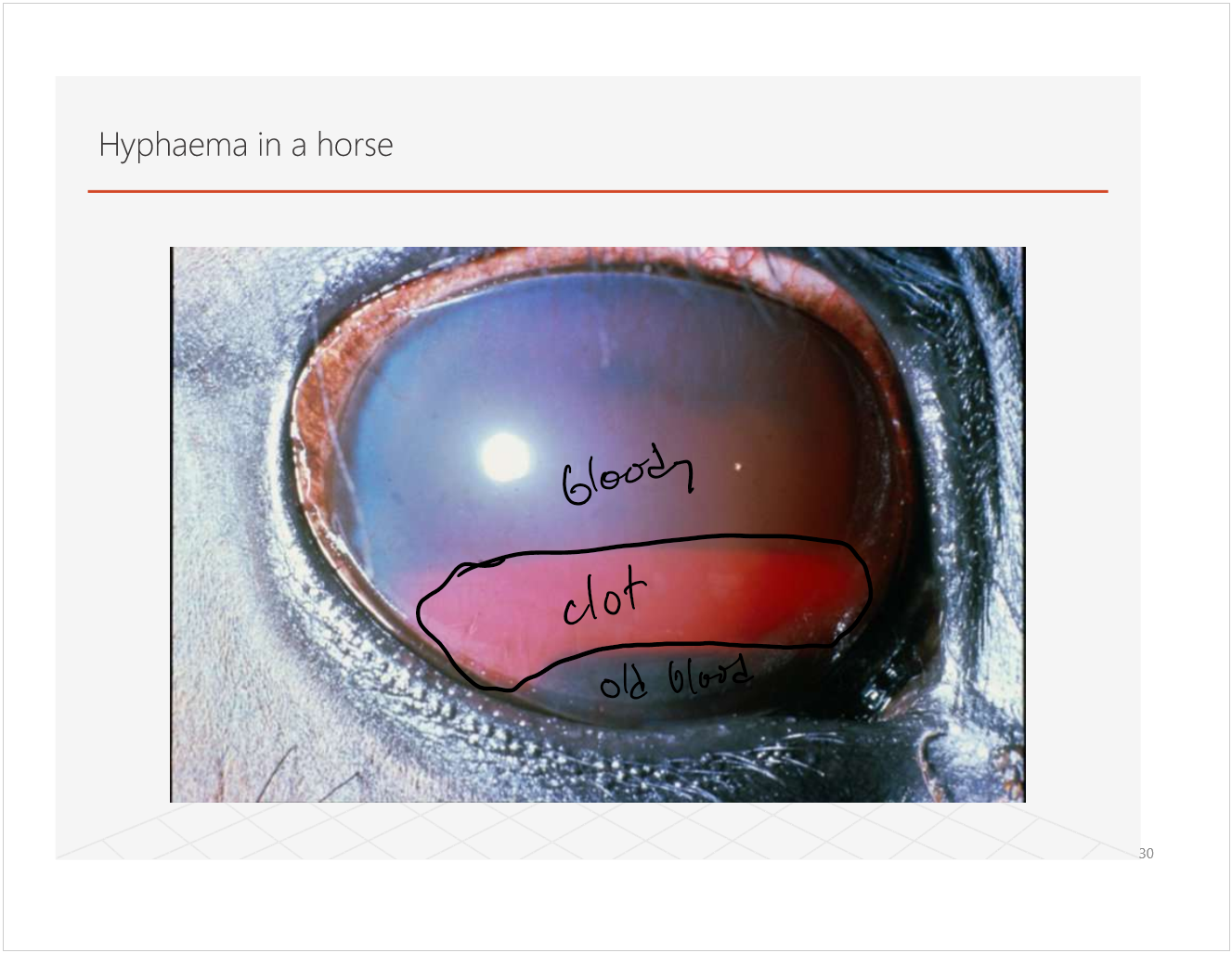
aqueous flare, fibrin, hyphema, hypopyon
miosis
reduced intraocular pressure
limbal neovascularization and corneal edema
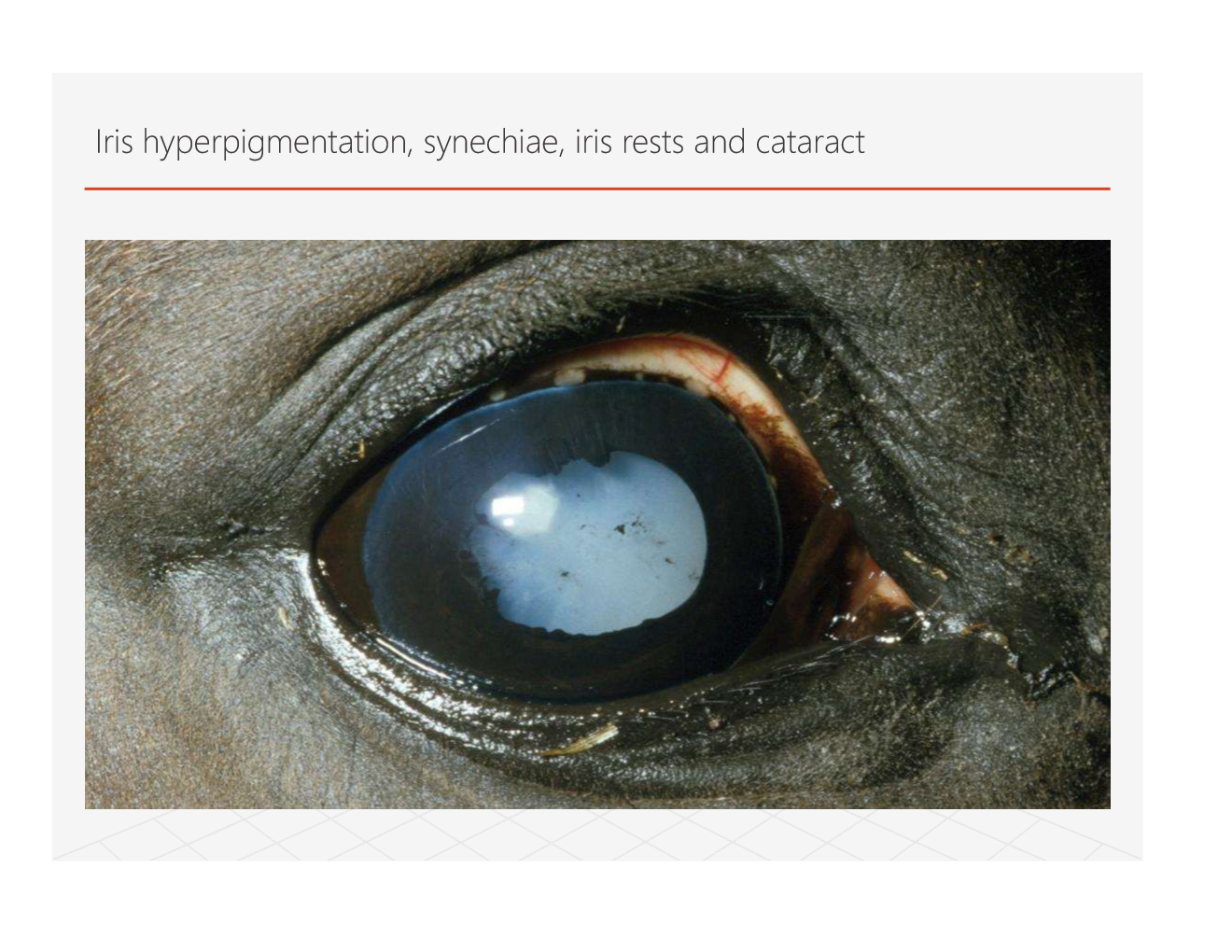
iris hyperpigmentation
keratic precipitates
iris swelling
synechiae
reduced vision
what are the types of exudates?
serous- aquous flare
fibrinous- fibrin clot
sanguinous- hyphema
purulent- hypopyon
quiz pending
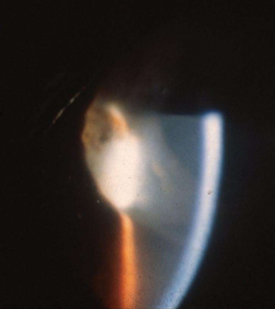
you look thru a slit microscope at the eye and see this, what is it?
aqueous flare, looks like smoke in sunlight


this?
hypopyon
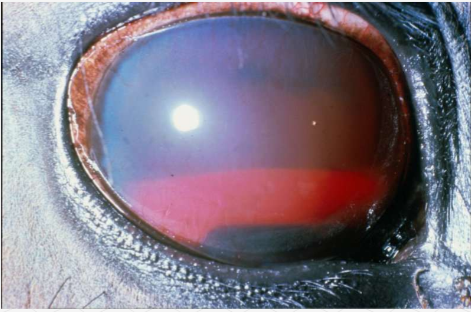
aaand this?
now a challenging one
pupil miosis, iris rubeosis, corneal neovascularization!
what happens in the subacute phase of inflammation?
immunological reactions establish
localized
PMN and mononuclear phacocytes
injury
Uncontrolled
leukocytes
blood vessel proliferative
fibroblast
may resolve or become chronic
what are causes of chronic uveitis?
initiating factor not elimated
immune mediated disease established
epitope spreading
molecular mimicry
e.g. equine recurrent uveitis
leptospira
again, what are the clinical signs of uveitis?
aqueous flare, fibrin, hyphema, hypopyon
miosis
reduced intraocular pressure
limbal neovascularization and corneal edema
iris hyperpigmentation
keratic precipitates
iris swelling
synechiae
reduced vision

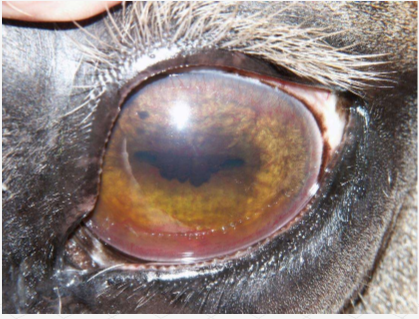
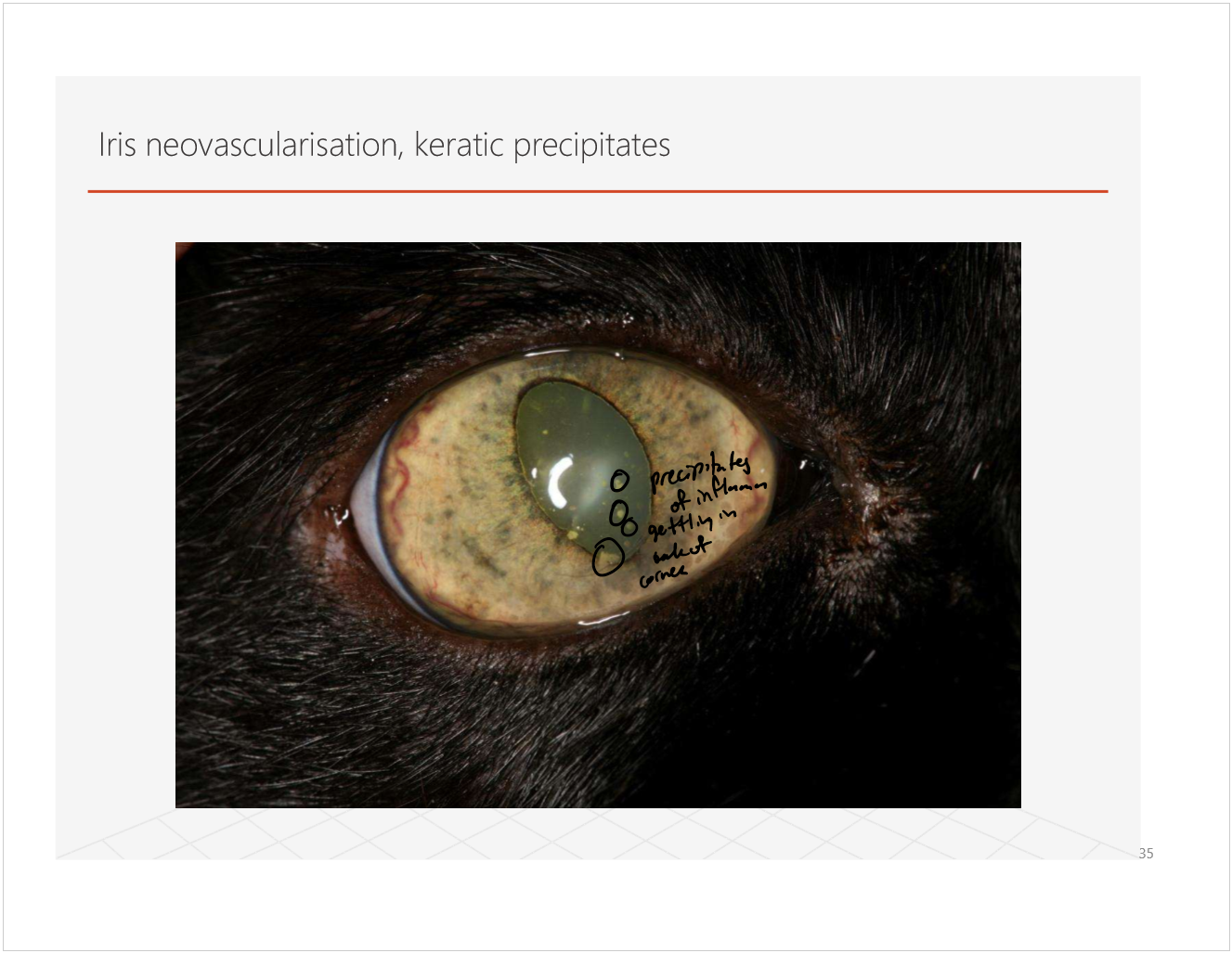
what is this?
iris neovascularization, keratic precipitates
precipitates of inflamm getting in back of cornea
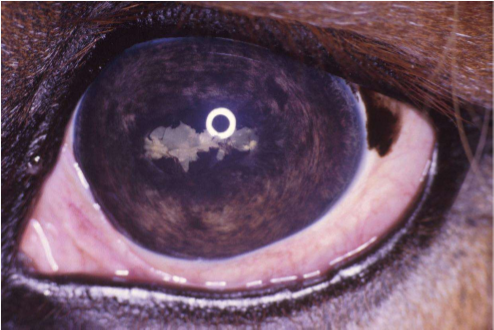
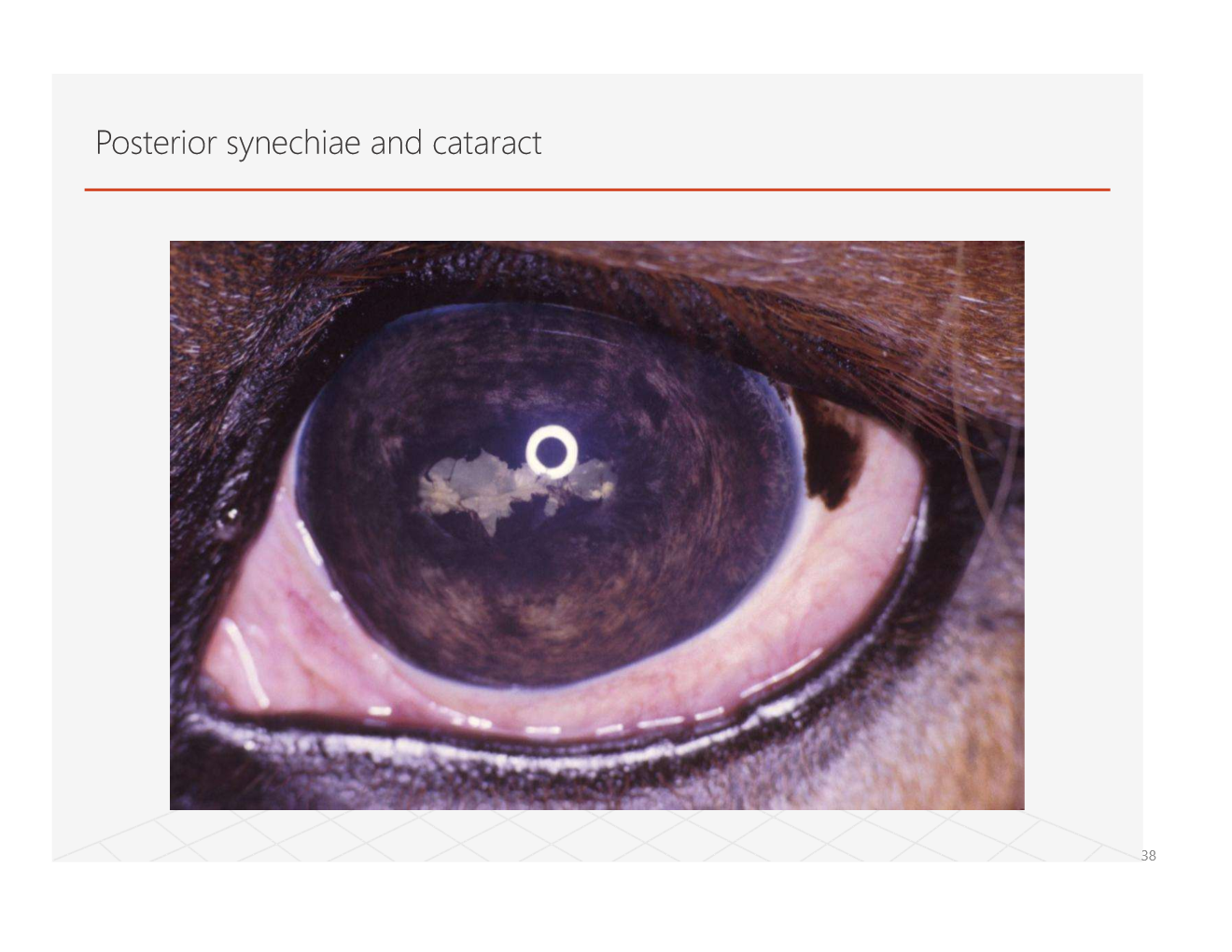
what is this?
developed from uveitis

what is this?
wjat are some specific causes of uveitis?
lens induced uveitis
hyperlipidemia
trauma
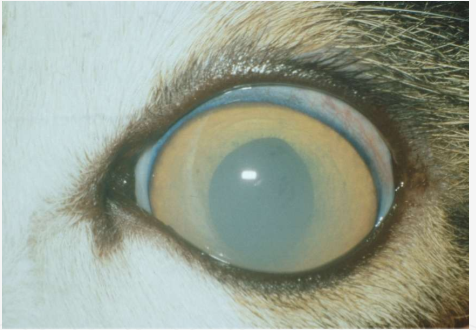
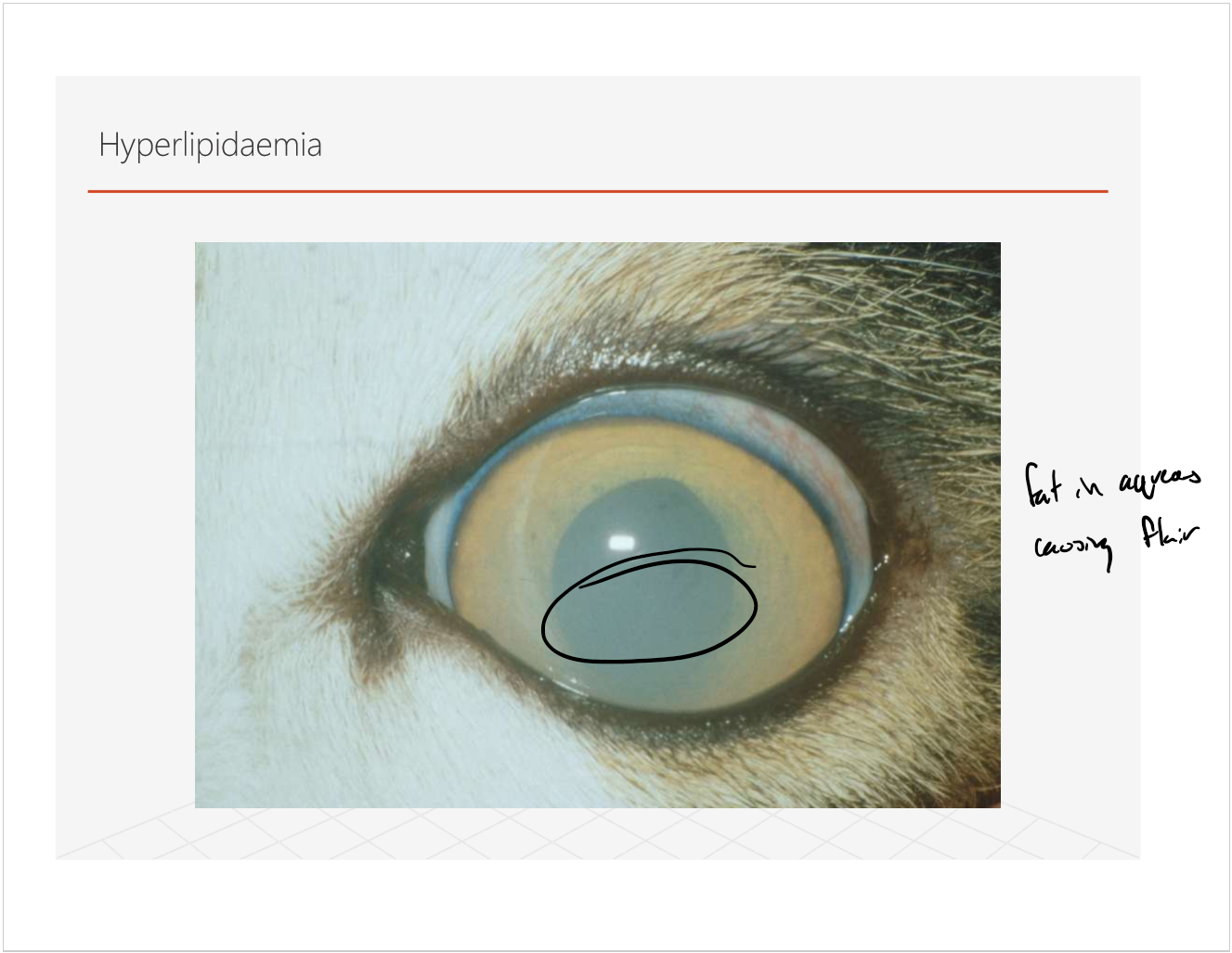
what is it?
hyperlipidemia
fat in the aqueous causing flare
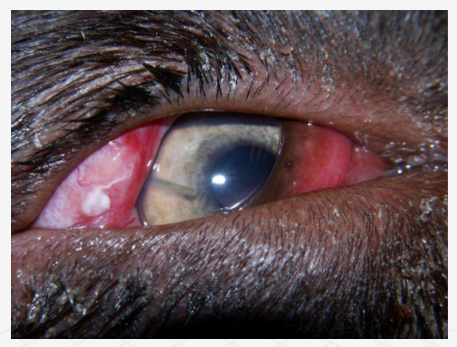
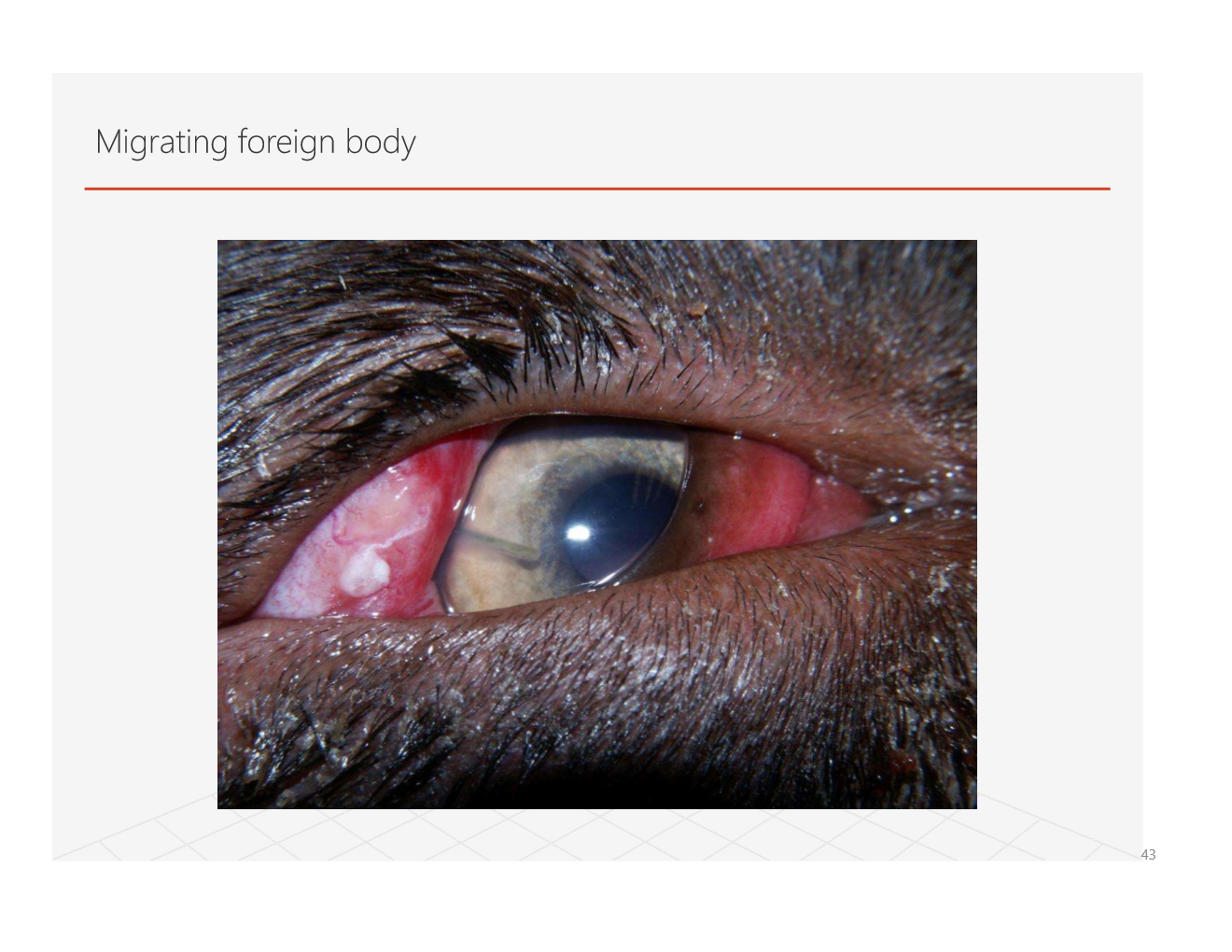
what is this?
an eyelash foreign body
what are some canine uveitis causes?
infectious canine hepatitis
canine brucellosis
canine ehrlichiosis
uveodermatological syndrome
protozoal disease
leishmaniasis
toxoplasmosis
pigmentary and cystic glaucoma
not an inflamm disease but looks like uveitis clinically
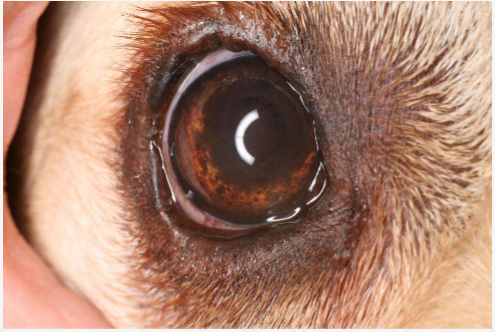
which of those is in this picture?
Feline causes of uveitis
feline infectious peritonitis (FIP)
bartonella henselae
toxoplasma gondii
FIV
feline herpes virus-1
FeLV
equine causes of uveitis
leptospira spp.
equine herpesvirus
equine viral arteritis
farm animal causes of uveitis
bovine malignant catarrhal fever
infectious bovine rhinotracheitis
classical swine fever
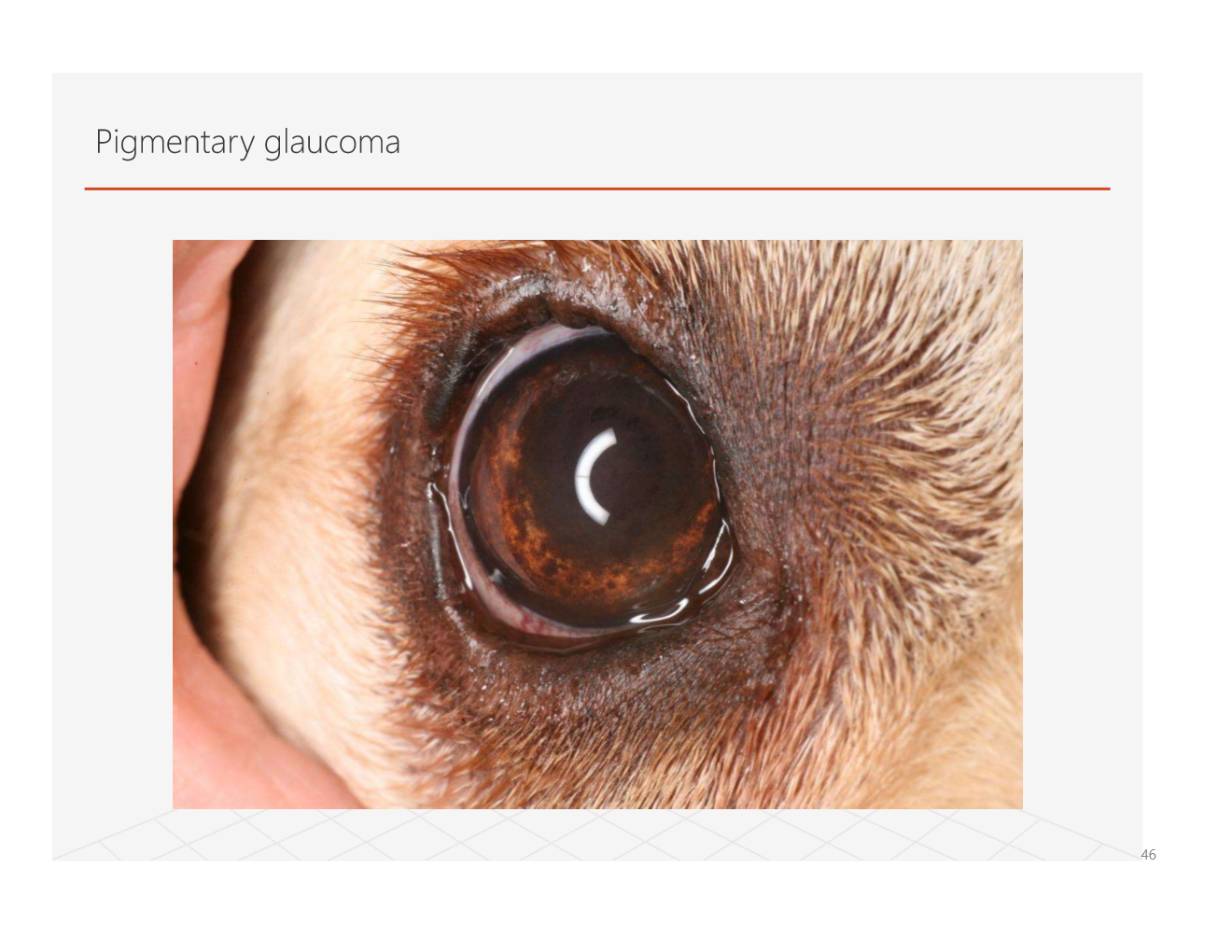
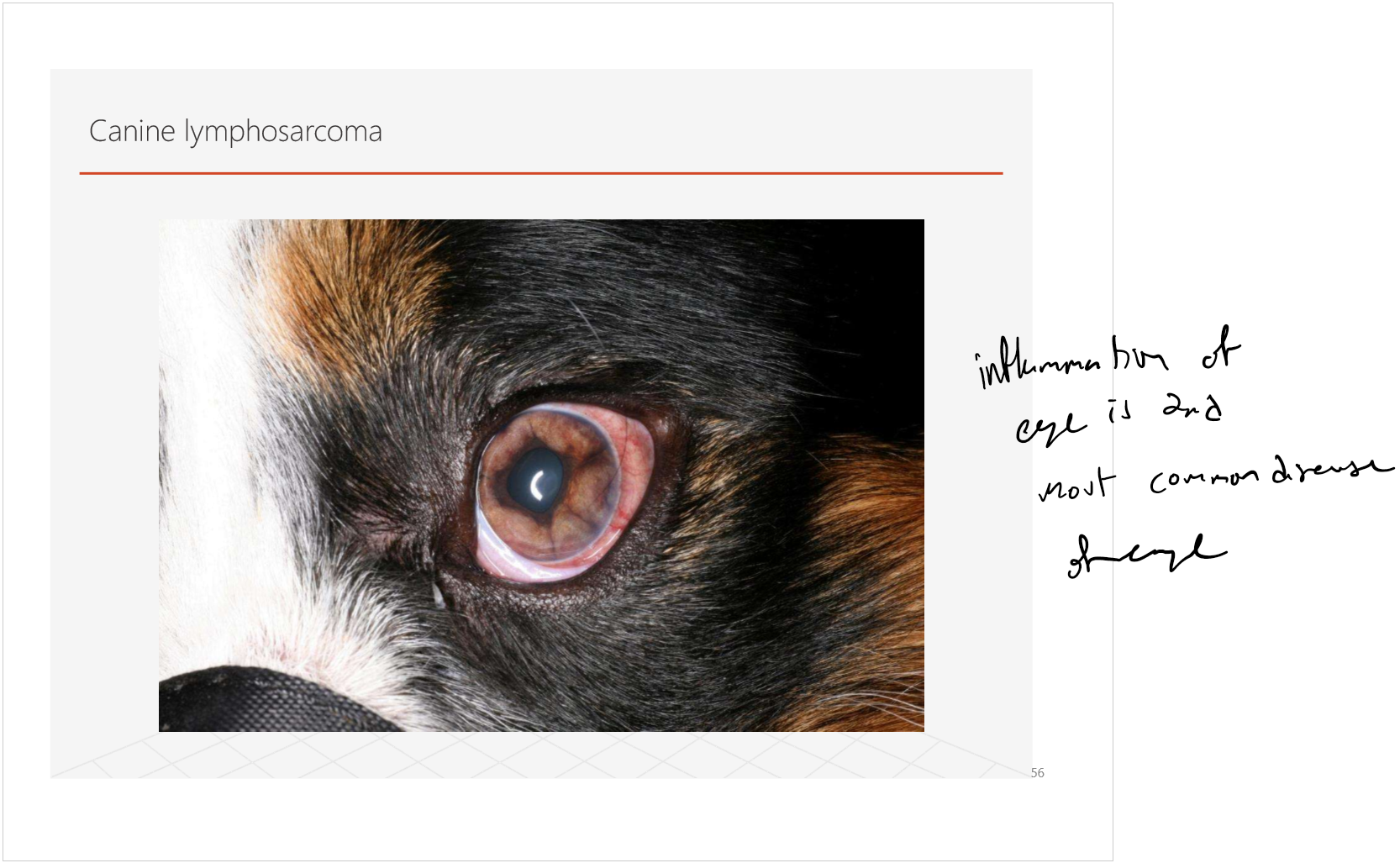
what are some common types of neoplasia of the eye?
melanoma/melanocytoma
adenoma/adenocarcinoma
lymphoma
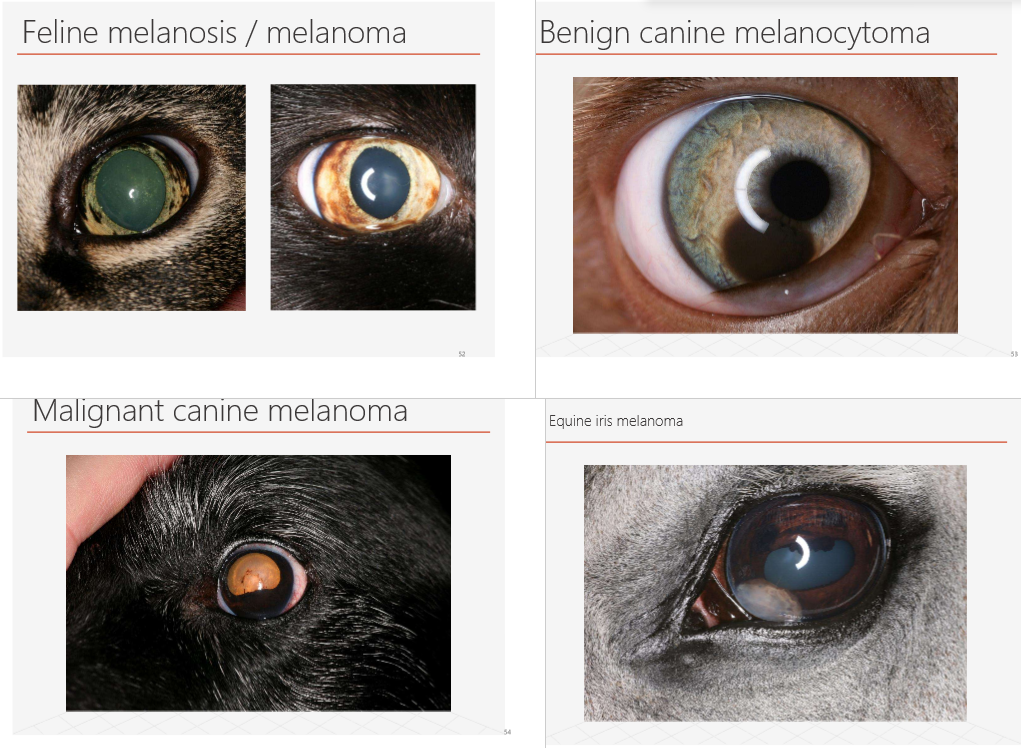
if ur dying to know what they look like i guess (flip for one more)
what is glaucoma?
diseases that cause death of the neural cell layers within the retina and optic nerve head.
most of these diseases related to and produce clinical signs of a raised intraocular pressure
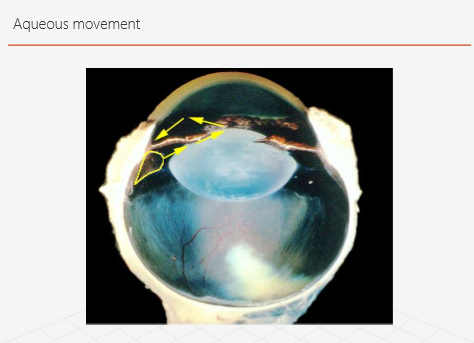
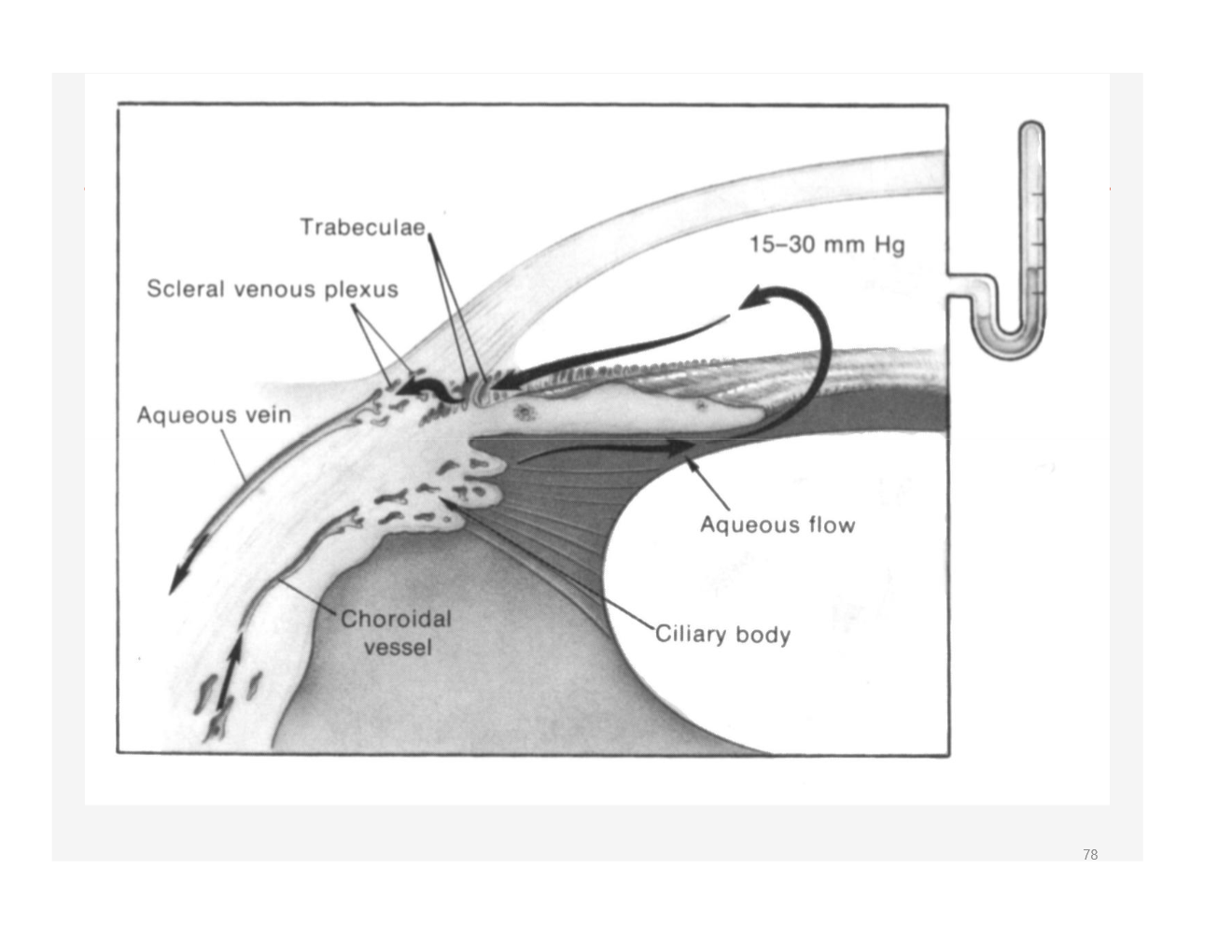
How does the aqueous usually regulate pressure?
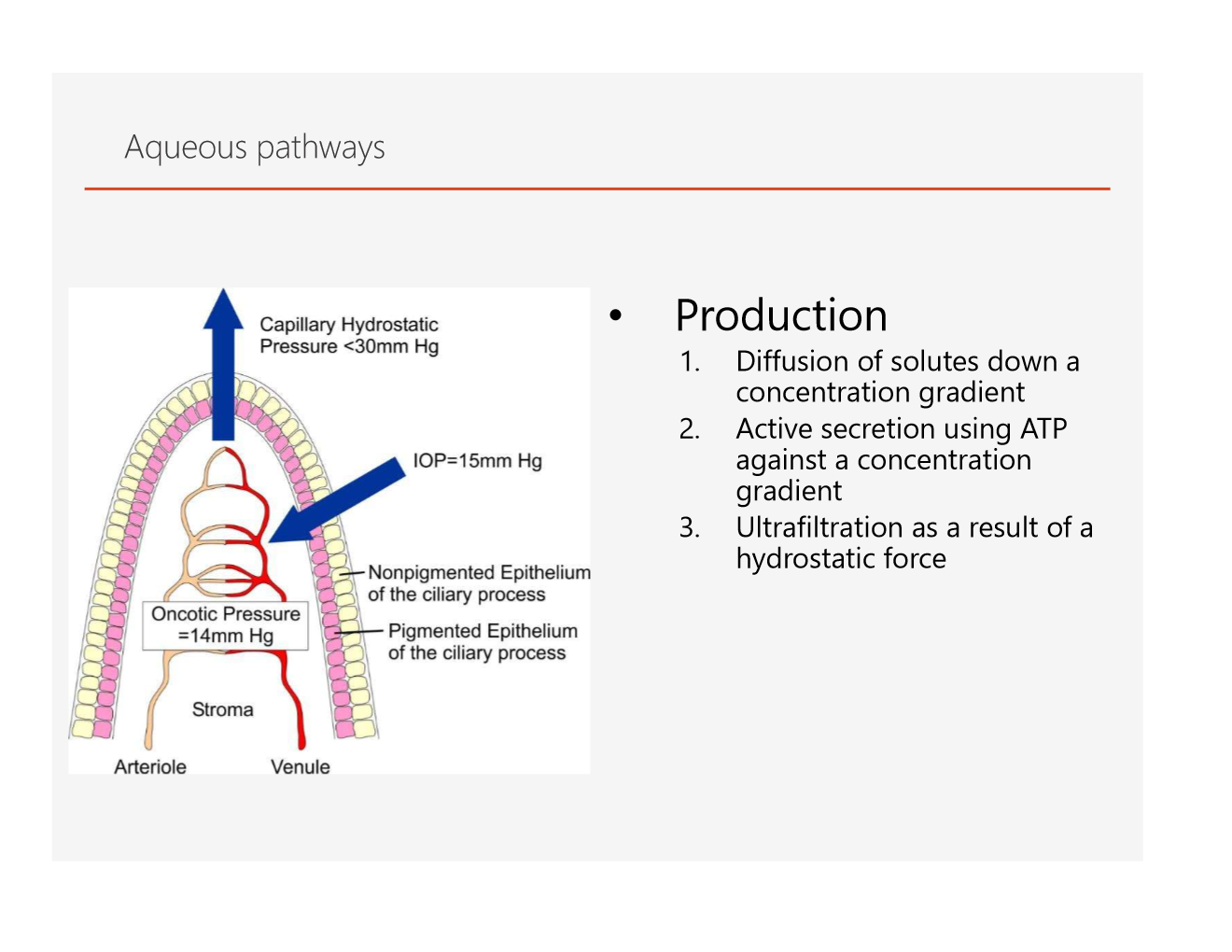
what is the normal intraocular pressure for most species?
15-25 mmhg
what are some causes of variation in intraocular pressure?
diurnal variation
age
blood pressure
drugs
ocular inflammation
position and restraint of animal
instrumentation used for mesurement
what is the pathology of glaucoma?
buphthalmia (increased globe size)
stretching of the ocular tunics
associated with
corneal ulceration
fractures of descemet’s membrane
equatorial staphyloma
lens subluxation/luxation
phthsis bulbi
pressure induced atrophy of the ciliary processes leading to:
decreased aqueous production
then, a reduction in globe size
Pathology of glaucoma in the cornea (categorized)
edema pathology?
enlargement pathology?
neovascularization pathology?
pigmentation pathology?
edema
>40mmHg stops endothelial pump from functioning efficiently
enlargement
stretching leads to fractures in descemet’s membrane- haab’s striae
neovascularization
deep “brush- border” of vessels at the limbus through 360 degrees
superficial branching vessels
pigmentation
associated with the chronic neovascularization
pathology of glaucoma in the sclera and iris?
sclera
scleral thinning
stretching of globe
iris
mydriasis
impaired neural or blood supply to the sphincter muscle of the iris
lack of sensory input due to retinal ganglion cell dysfunction
eventual iris atrophy
pathology of glaucoma in the ciliary body and anterior chamer angle/sclerociliary cleft?
ciliary body
advanced ciliary body atrophy will halt aqueous production leading hypotony
anterior chamber angle and sclerociliary cleft
secondary changes in the glaucomatous eye include narrowing and then closure of the iridiocorneal angle and collapse of the sclerociliary cleft
this is seen even in advanced primary open angle glaucoma
pathology of glaucoma in the choroid/tapetum and the lens?
choroid and tapetum
less of vascular perfusion in the choroid especially in acute glaucoma
due to poor autoregulaton of perfusion
tapetal thinning
tapetal fundus may be less affected initially than the non-tapetal fund
lens
changes initially affect new lens fibre formation, causing a cataract
lens luxation- primary or secondary
pathology of glaucoma in the vitrous and the retina/optic nerve head?
vitreous
liquification
important in relation to lens luxations allowing vitreous to interfere with the aqueous outflow pathways
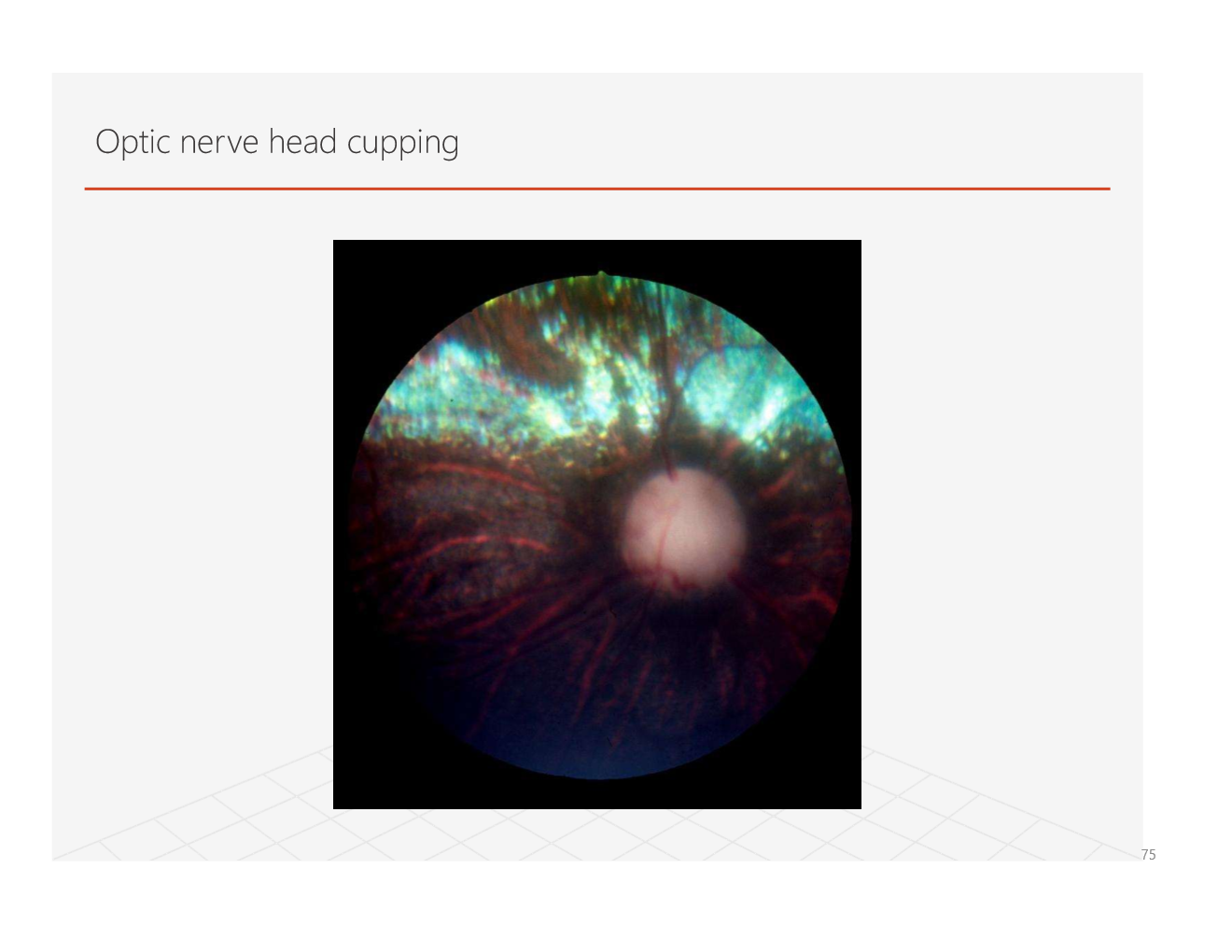
retina and optic nerve head
retinal ganglion cells are affected by:
multitude of factors
axonal degeneration and atrophy
shearing forces at the lamina cribosa
decreased axoplasmic flow
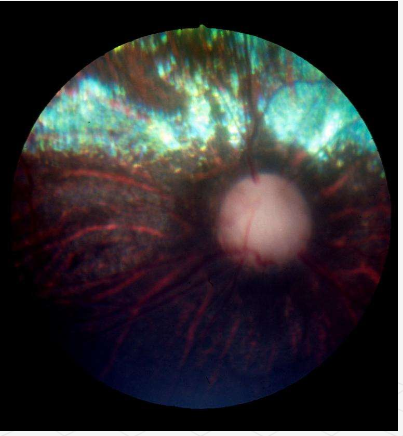
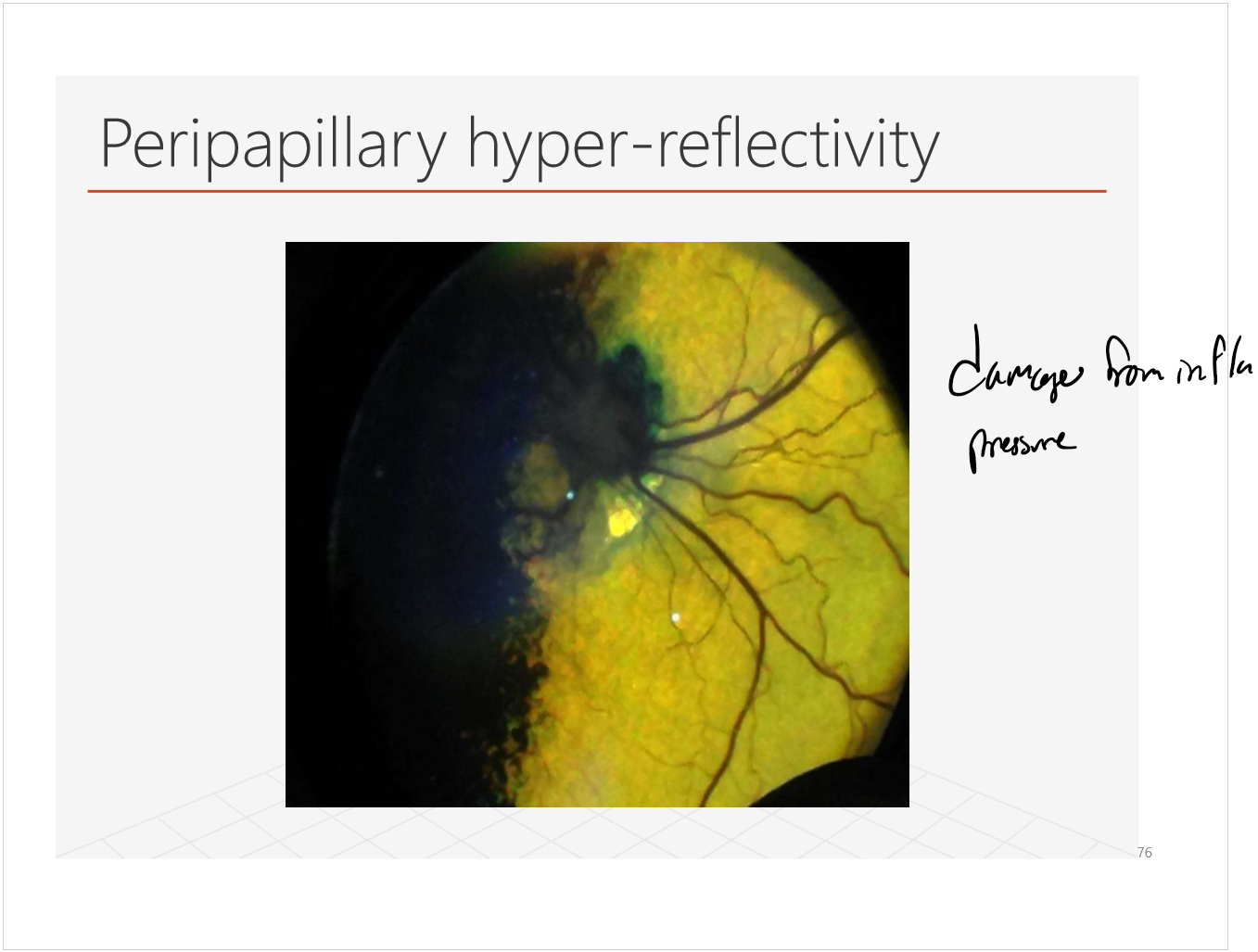
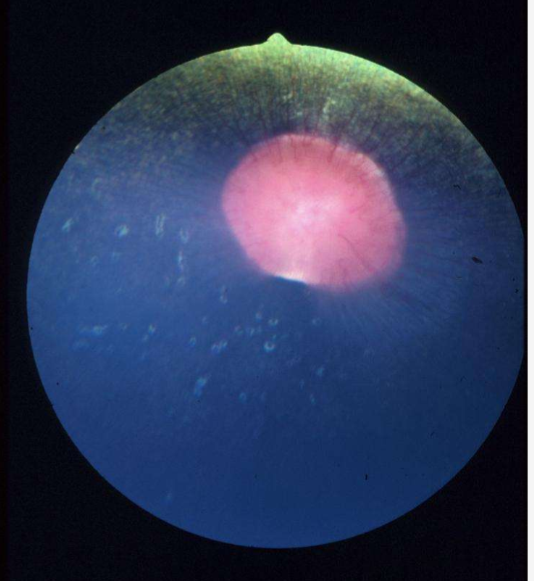
what is this?

what is this?
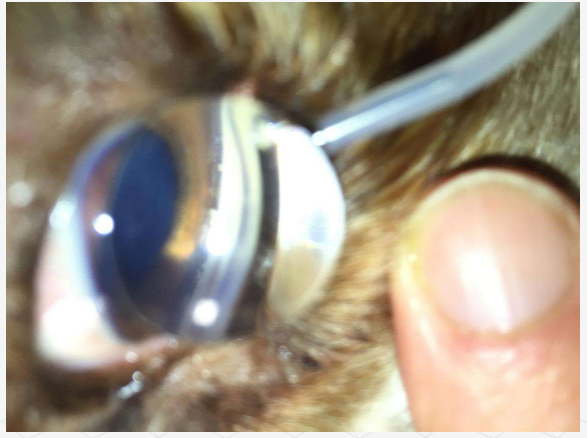
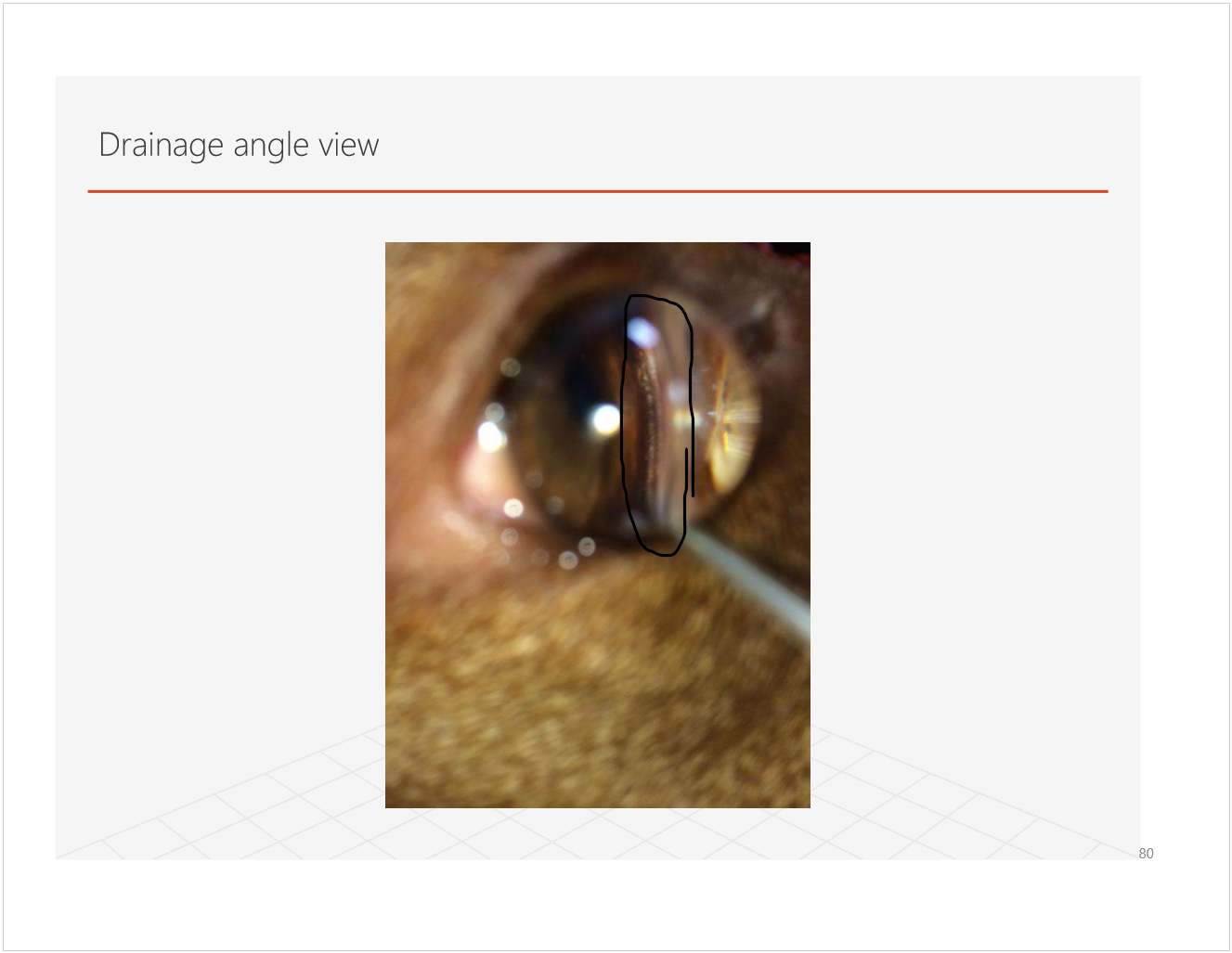
how do you asses drainage angle of the eye?
gonioscopoy
use a mirrored or convex lens to image the angle beneath the edge of the cornea at the limbus (arrows in pic show what you are trying to look at)
what is this?
pectinate ligament dysplasia
what a normal drainage angle looks like:
how do you classify glaucomas?
primary
open/normal angle
narrow/closed angle
secondary
blockage along aqueous pathway
lens luxation
iris bombe
drainage angle
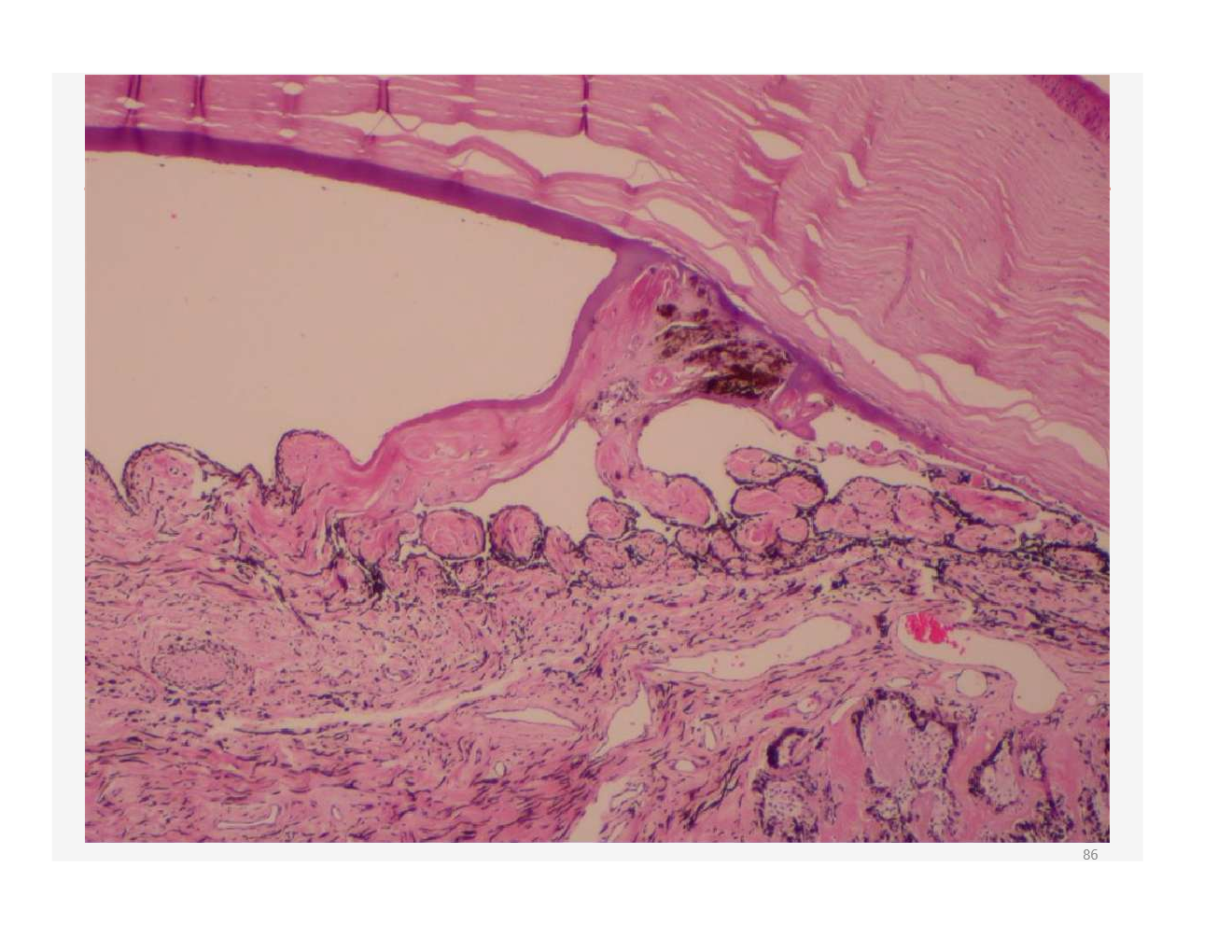
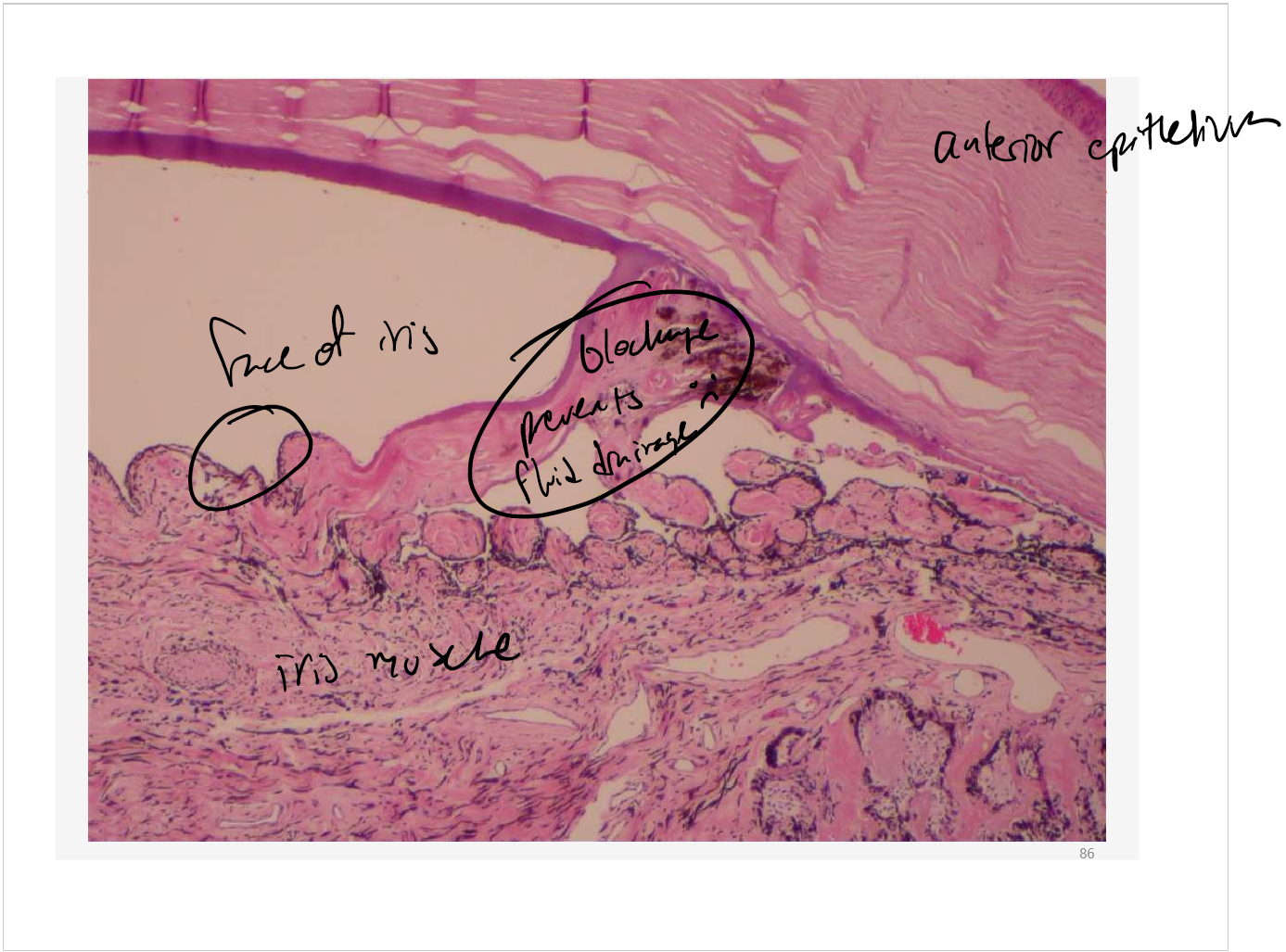
is this primary or secondary glaucoma?
secondary! it is a blockage
what diseases are there in the lens and vitreous
cataract
luxation
penetration/rupture
secondary effects on the globe
Note: congenital diseases not listed
congenital diseases of the lens and vitreous
aphakia
microphakia
multi ocular defects
lenticonus/lentiglobus
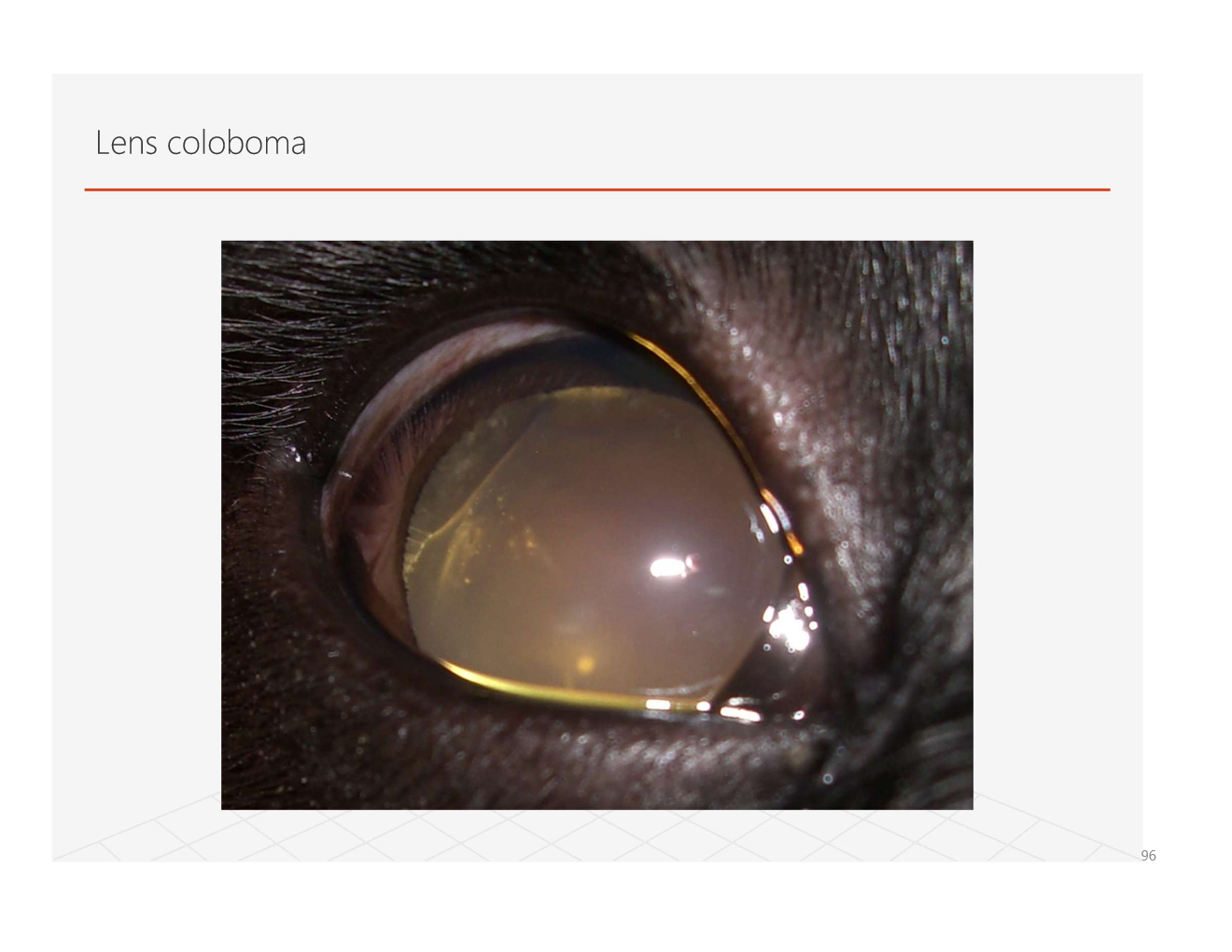
coloboma
notch at the equator
cataract
secondary to persistant pupullary membrane
disease involving the lens only
what are causes of microphthalmia? what are its effects on the lens?
causes
failure to develop a full sized lens placode
poor presentation of the optic vessel
reduced intraocular pressure
failure of the optic fissure to close on schedule
lens effects
microphakia, cataract, anterior segment dysgenesis
Why is a lens coloboma?
appears to be due to lack of zonules in a specific location
causes lack of growth of lens apposing affected area
what is anterior segment dysgenesis?
what are some vitreal defects?
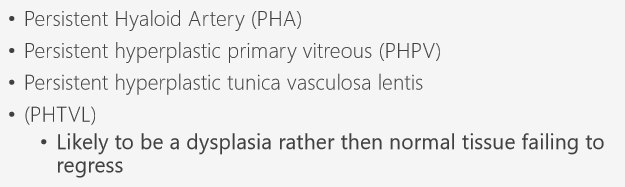
what are the grades of PHPH/PHTVL?
what grade is this?

Grade 3
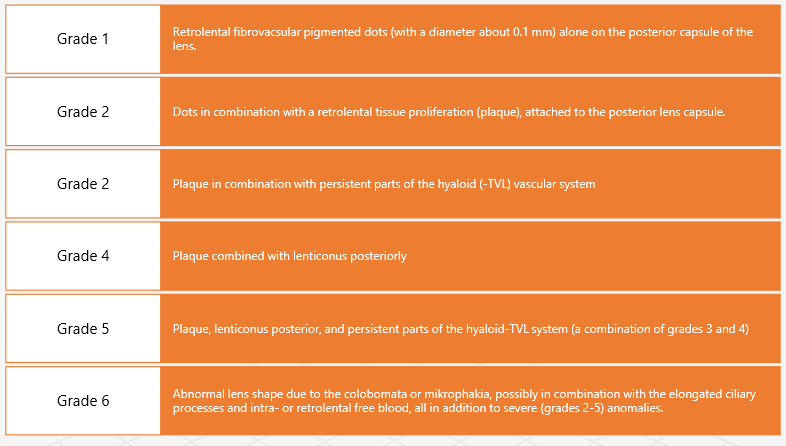
Define cataract? how are they classified?
what are the ages at onset of cataracts?
they can be congenital, juvenile (primary and possibly progressive), or senile
what age is this?

juvenile equine cataract
explain different etiologies of cataracts
Okay, theres the “most useful” classification of cataracts in relation to vision and secondary problems. name the classes and explain them
what class is this?

immature
what class is this?
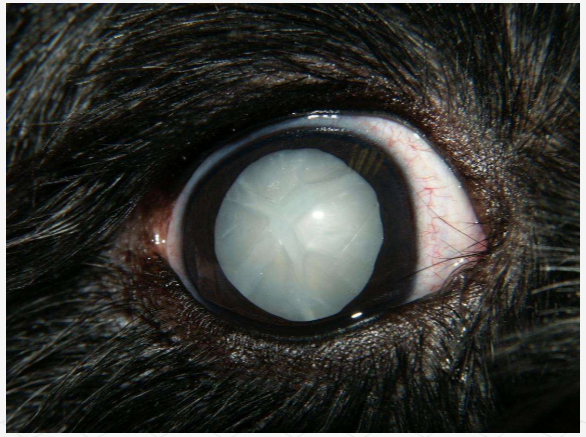
hypermature
what class is this?
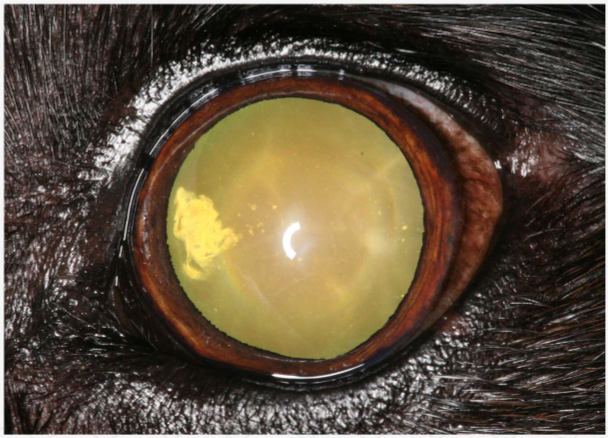
incipient
what class is this?
mature
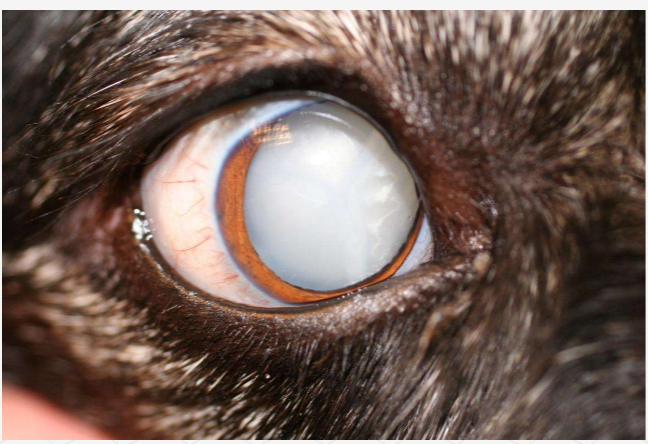
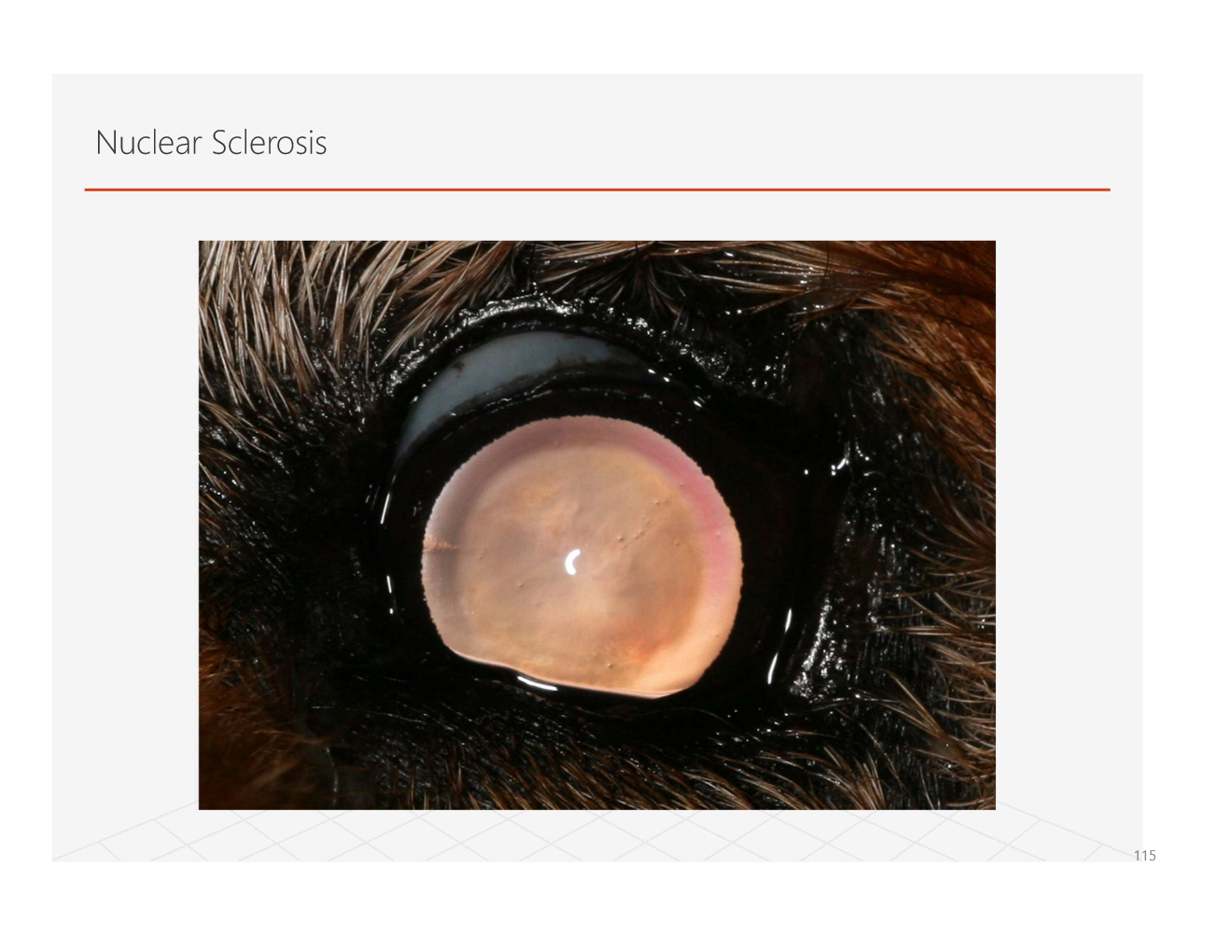
what is nuclear sclerosis? how does it affect how the eye appears? does it affect vision?
a continual production of lens epithelial cells leading to compression of the lens nucleus
appears blue/grey due to refractive index change
severe changes may affect vision
Note: owners often mistake for cataracts
what are the types of lens induced uveitis? how do they occur?
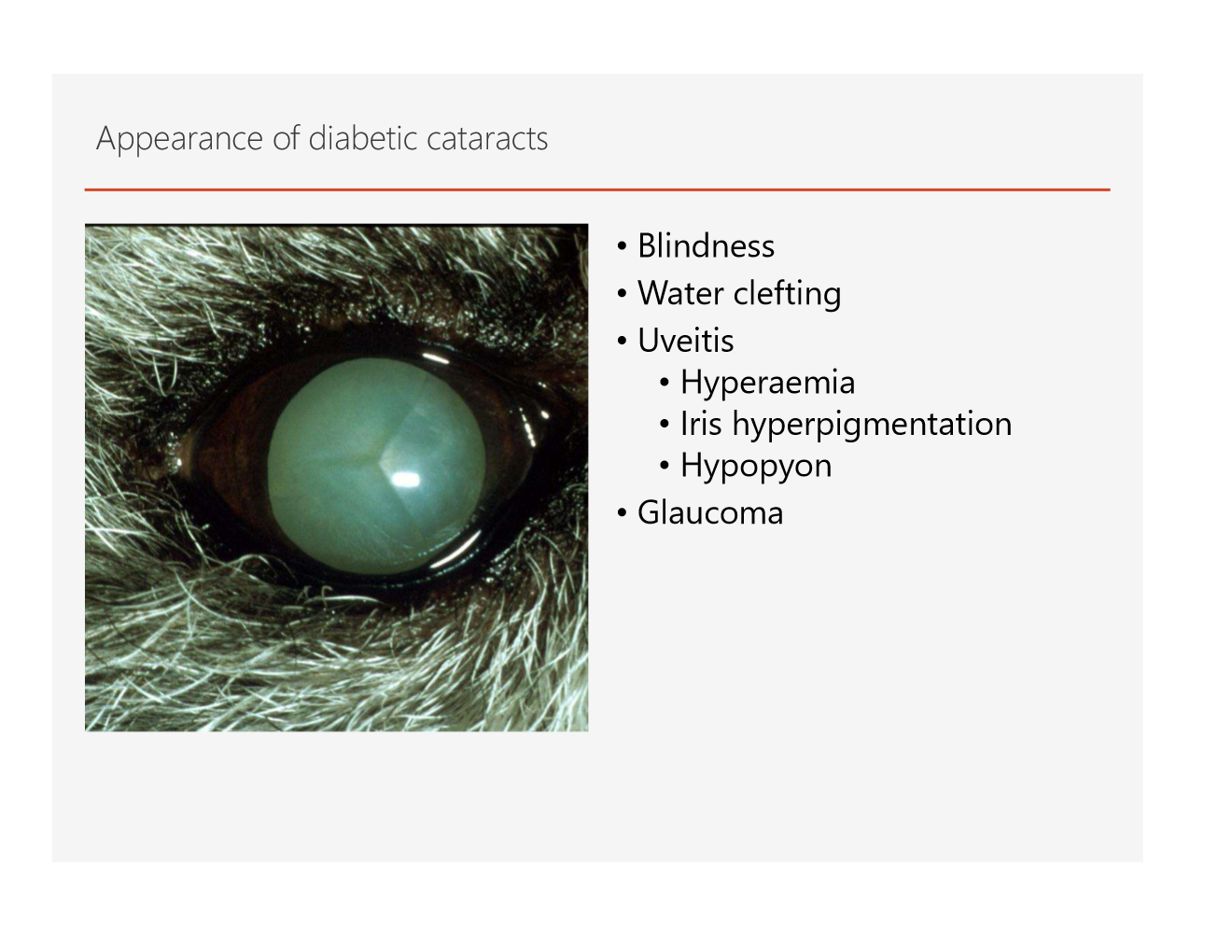
what are some diabetic ocular diseases
Note: cats do not get diabetic cataracts, dogs do
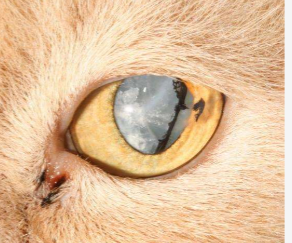
is this a diabetic cataract?
no! its secondary to trauma
what features show this is a diabetic cataract?

Ultrasound is especially helpful
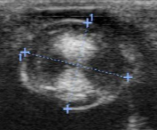

diabetic cataract has the hourglass appearance on ultrasound
what is the etiology/predisposition of lens subluxation/luxation?
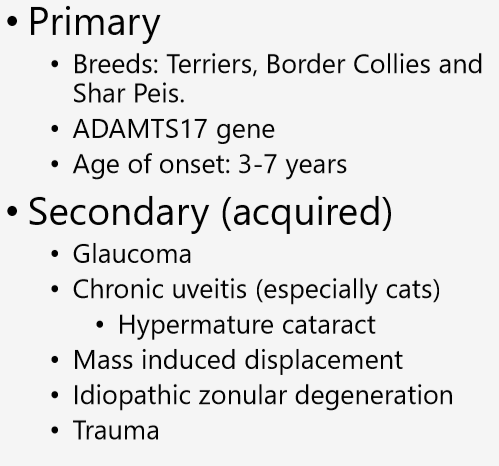
why do lenses luxate?
what are clinical signs of luxations?
what are secondary causes of glaucomas?
pupil block
uveitis
drainage angle occlusion
what is asteroid hyalosis of the vitreous
an aging change that does not affect vision
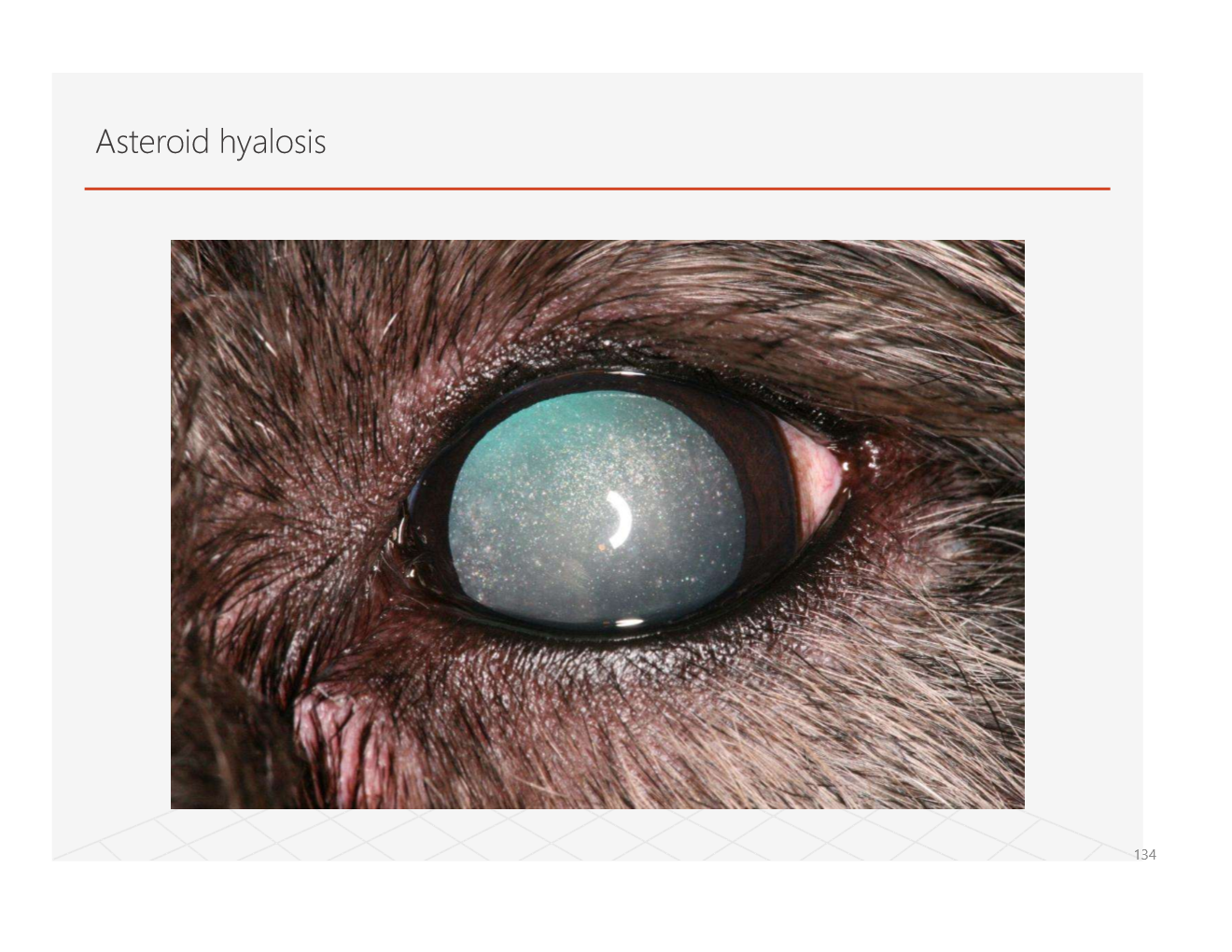
lowk looks kinda pretty ngl
what is synchysis scintillans?
clinically similar to asteroid hyalosis but particles are cholesterol deposits in a liquified vitreous
globe movement results in snowglobe type of movement of the deposits before they settled back down
what causes pigment migration?
caused by pigment dispersal syndromes like pigmentary uveitis
hemorrhage into vitrous can eventually present as vitreal pigmentation as hemorrhage removed from vitreous
what can cause hemorrhage of the vitreous?
what is vitritis? is it usually primary or secondary?
inflammation of the vitrous
rarely primary
can be secondary to inflammation of adjacent intraocular structures
infectious causes: crypto and brucellosis
what are vitreal membranes?
consequence of long term vitreal inflammation and hemorrhage
what larvae can migrate to the vitreous?
dirofilaria and toxocara
what is vitreal attachment?
what can cause vitreal detachment? what can it be mistaken for?
what breed is predisposed to vitreal prolapse?
whippets
there are a dozen pics of what a normal retina looks like slides 147-162. it doesnt make sense for me to put them all in
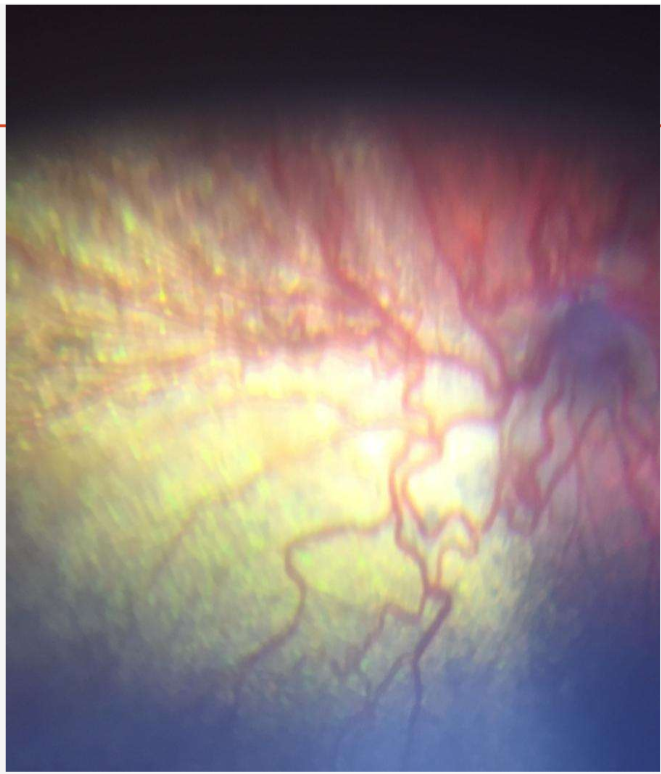
what are developmental conditions of the retina?
collie eye anomaly/choroidal hypoplasia
abnormal mesodermal differentiation
NEHJ1 gene deletion
hypoplasia lateral to optic nerve head
optic nerve head coloboma
retinal detachment
posterior segment hemorrhage
what is this?
micropapilla/optic nerev coloboma
small or imperfectly formed optic nerve head
what are types of retinal dysplasia?
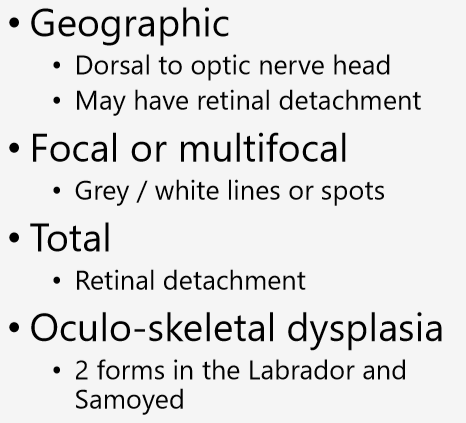
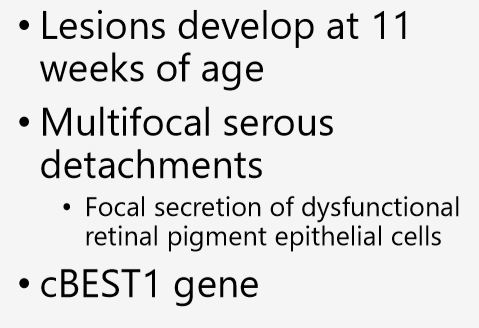
what occurs in canine multifocal retinopathy?
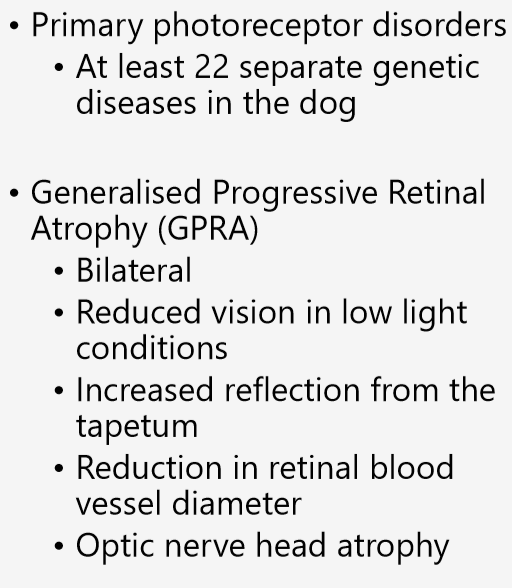
what are some inherited retinopathies
how does retinal pigment epithelial dystrophy occur?
loss of the blood retinal barrier
increase in vascular porosity
loss of tight junction integrity in retinal pigment epithelium
allows cellular migration in to the retina and vitreous
it is a genetic disease predisposed in english cocker spaniels
low vit E (supplements can delay)
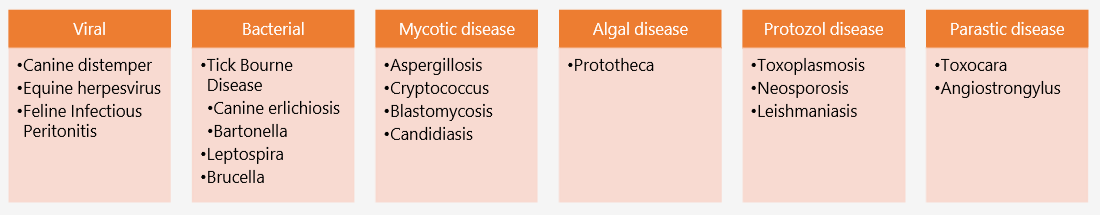
which of thes are acute and chronic chorioretinitis?
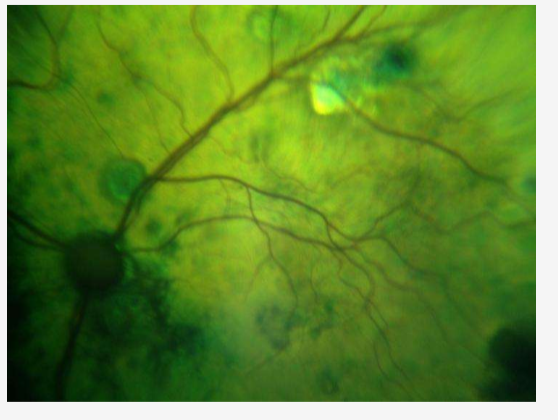
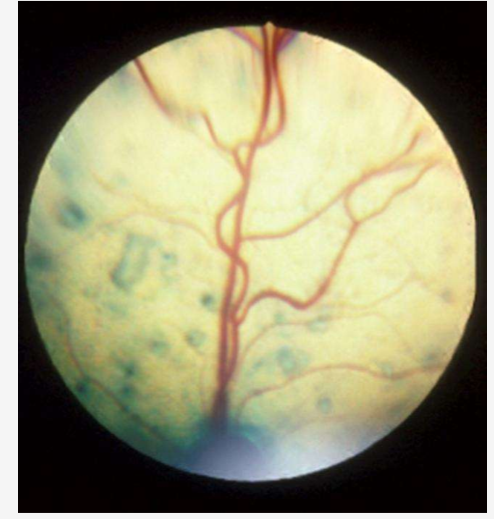
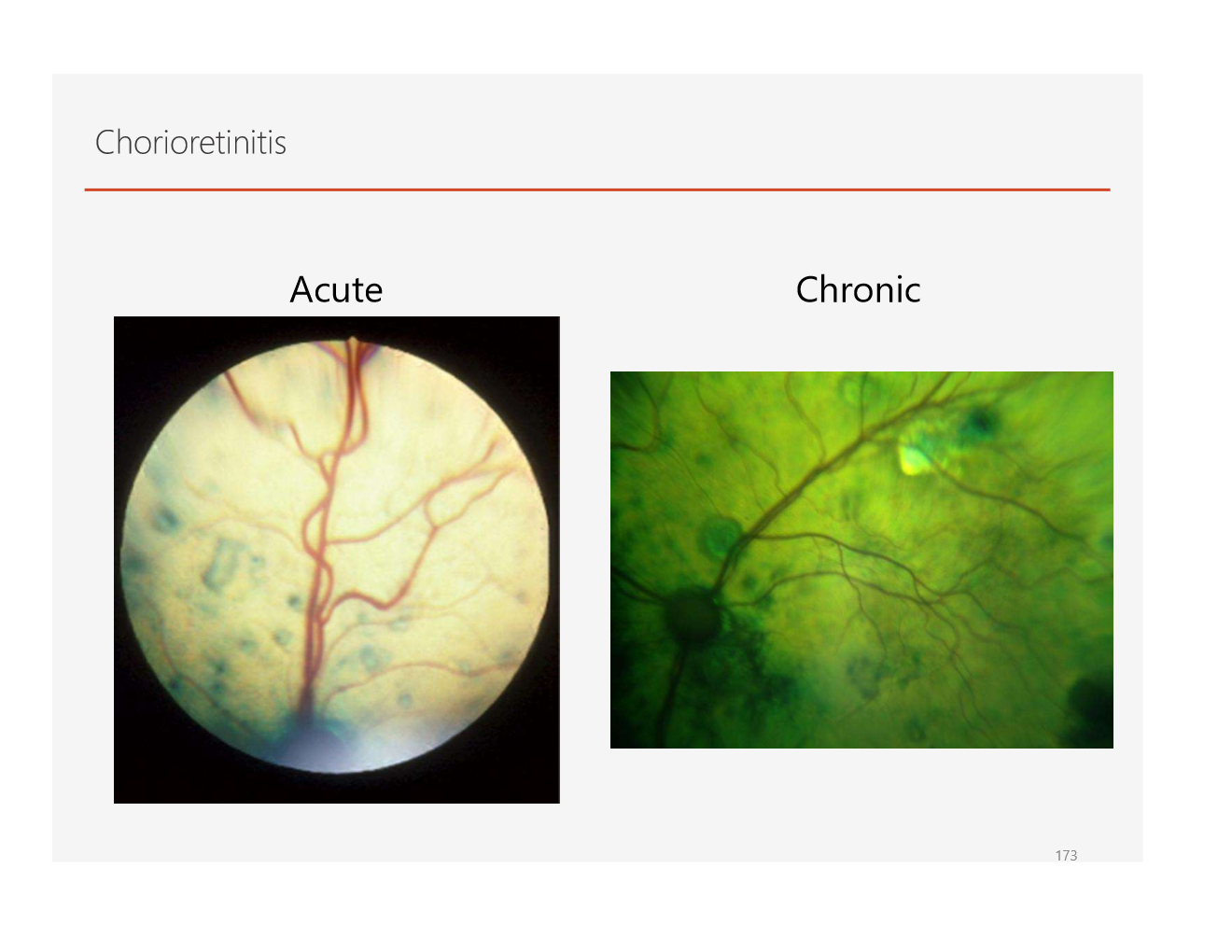
what are some infectious diseases that can cause retinal issues?
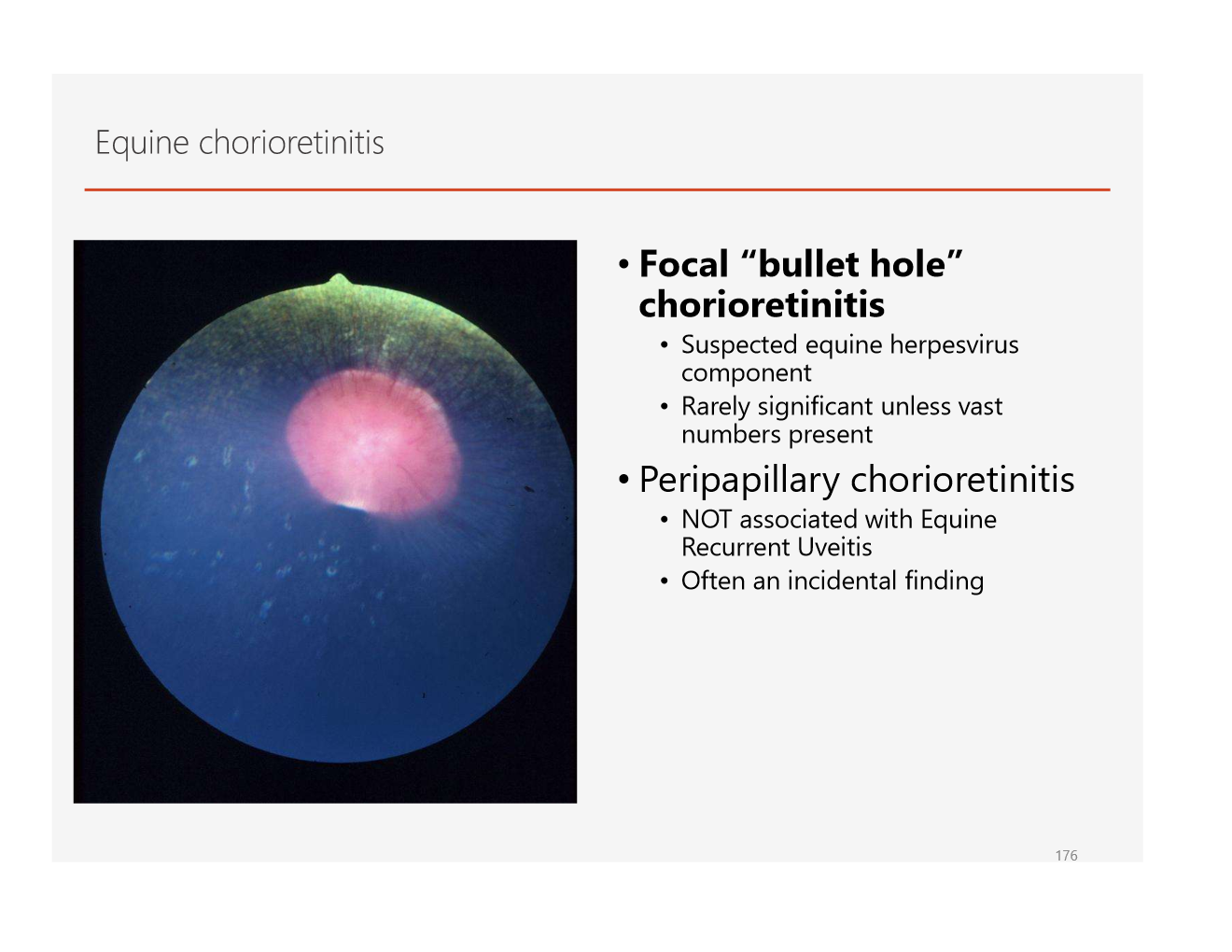
what disease has a characteristic “bullet hole” appearance?
tell me anything you know about sudden acquired retinal degeneration syndrome
How does tuarine deficiency affect the retina?
causes retinal degeneration
