Vitreous
1/9
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
10 Terms
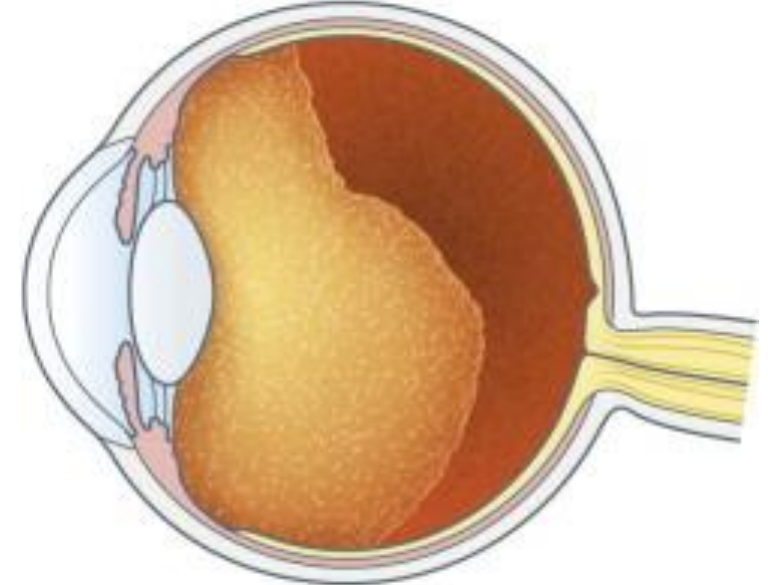
Vitreous
Gel-like structure
Fills the vitreous chamber
Spherical except for Patellar Fossa
80% of entire globe
Vitreous: Function
Physical Support
Holds retina in place next to choroid
Neural retina + choroid only connected at optic disc and ora serrata
Shock absorber
Protects retina during eye movements, physical activity
Transmit + Refract Light
Minimal light scatter due to:
High [water]
Hyaluronic acid/collagen complex spacing
Diffusion Barrier
Between anterior and posterior segments
Prevents topical medications from reaching the retina/optic nerve
Entrance of medications from bloodstream rarely make it to anterior segment
Metabolite Storage/Buffer
Reservoir for metabolites of:
Retina
Lens
Ciliary Body
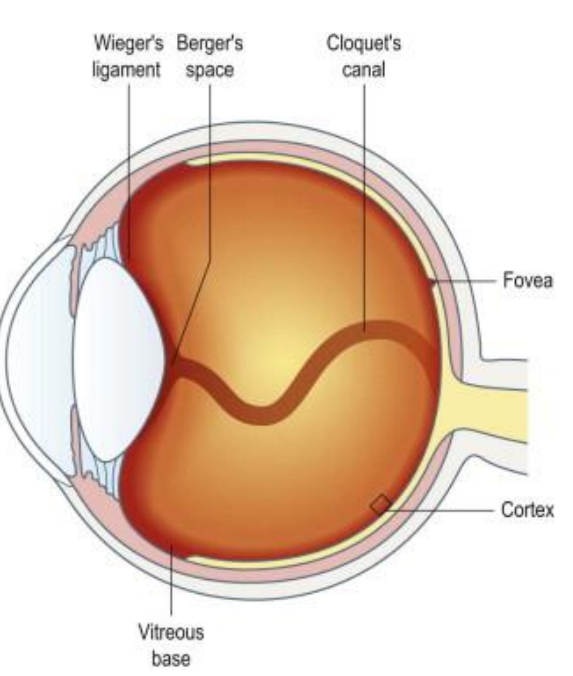
Vitreal Attachments
Strongest → Weakest
Vitreous Base
Strongest attachment (2)
At ora serrata (1)
1.5-2 mm anterior
1-3 mm posterior
Vitreal fibers embedded in BM of nonpigmented epithelium of the CB + ILM of retina
Posterior to lens
Hyaloideocapsular ligament (of Weiger)
Retrolental ligament
Forms retrolental space of Berger
Annular attachment
1-2 mm wide; 8-9 mm diameter
Firm attachment in youth, diminishes after age 35
Optic Disc (Peripapillary)
Also diminishes with age
Macular
3-4 mm in diameter
Retinal Vessels
Consists of fine strands that extend through ILM
May account for hemorrhages that occur with vitreoretinal traction
Vitreous Zones
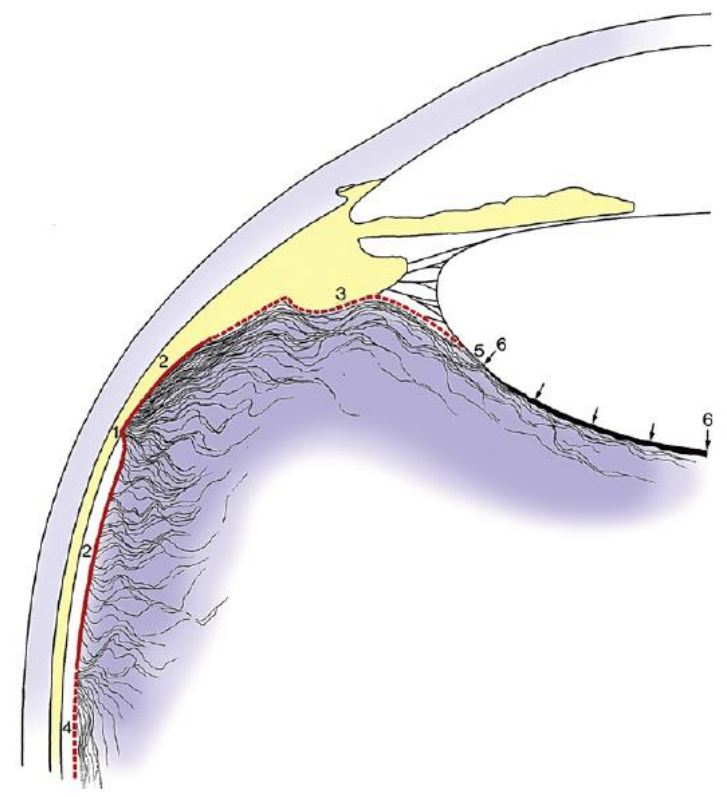
Vitreous Cortex
AKA: Hyaloid Surface
Outer zone
Tightly packed collagen fibrils
Parallel + perpendicular to retinal surface
Anterior Vitreous Cortex:
Anterior to vitreous base
Adjacent to CB, posterior chamber, + lens
Posterior Vitreous Cortex
Posterior to vitreous base
In contact with the retina
Contains transvitreal channels that appear as holes
Posterior Vitreous Cortex: Transvitreal Channels
Prepapillary hole
Premacular hole
Prevascular fissures
Intermediate Zone
Continuous + unbranched fine fibers
Run anteroposteriorly
Arise near vitreous base, insert into posterior cortex
Vitreous tracts
Areas having different fiber densities
Cloquet’s Canal
AKA hyaloid channel, retrolental tract
Center of vitreous body
Former site of hyaloid artery system
Arises in retrolental space
Terminates in area of Martegiani
Funnel-shaped space at optic nerve
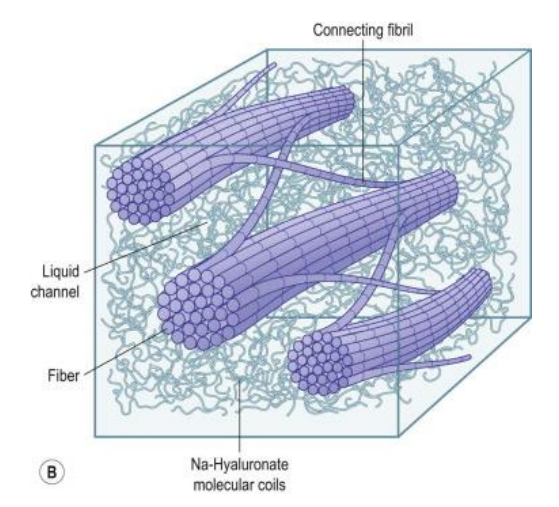
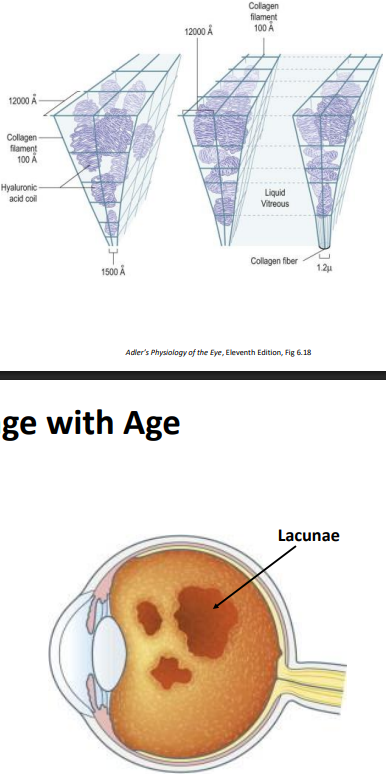
Vitreal Composition
98.5-99.7% water
Dilute solution of salts, soluble proteins, + hyaluronic acid
Collagen meshwork (insoluble protein)
Three major components (besides water):
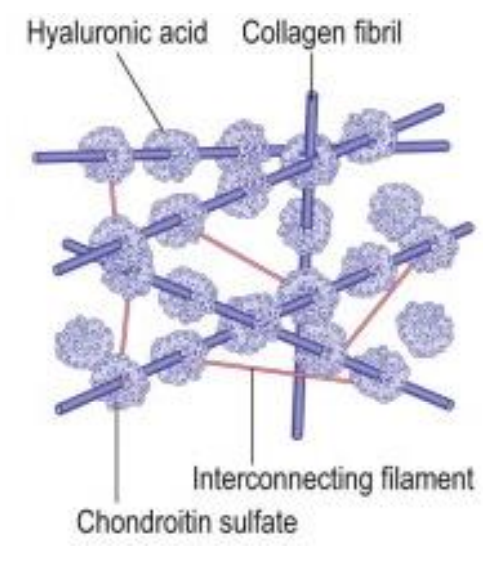
Collagen
Collagen content highest:
Vitreous base > posterior cortex > anterior cortex > center
Mostly Collagen Type II
3 identical α-chains form a triple helix
Collagen fibrils interconnect with hyaluronic acid
Hyaluronic Acid
Glycosaminoglycan
Long, unbranched coiled molecule
Hydrophilic
Maintains wide spacing between fibrils
Stabilizes the network formed by collagen strand
Concentration distribution similar to collagen
Hyalocytes
Vitreal cells (specific to vitreous)
Single, widely spaced layer in cortex near vitreal surface
Synthesize hyaluronic acid & Glycoproteins
Phagocytic properties- break down metabolic waste
Fibroblasts also located in vitreous base,
May be mistaken for hyalocytes
Synthesize collagen fibrils
Active in pathology
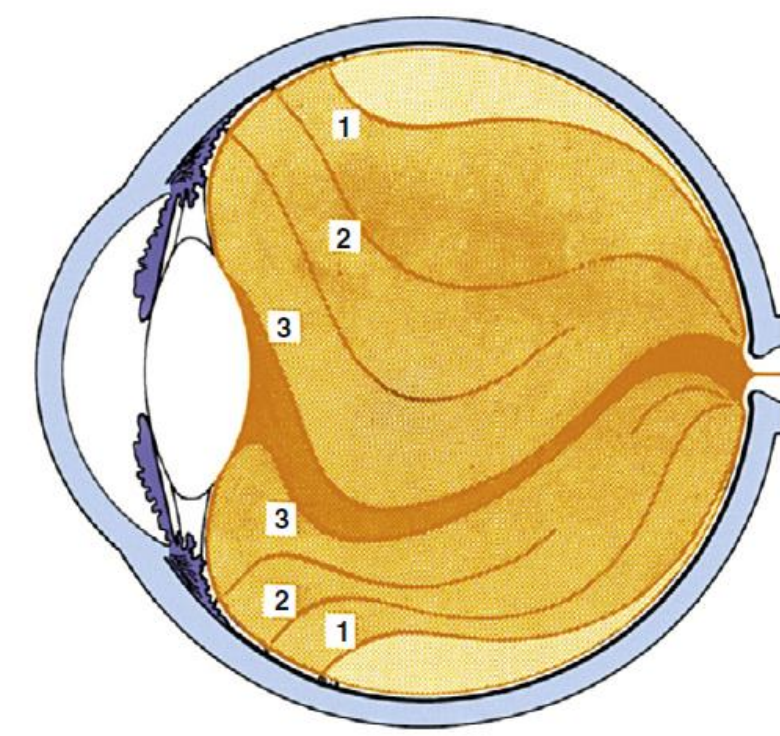
Vitreal Composition: Change with Age
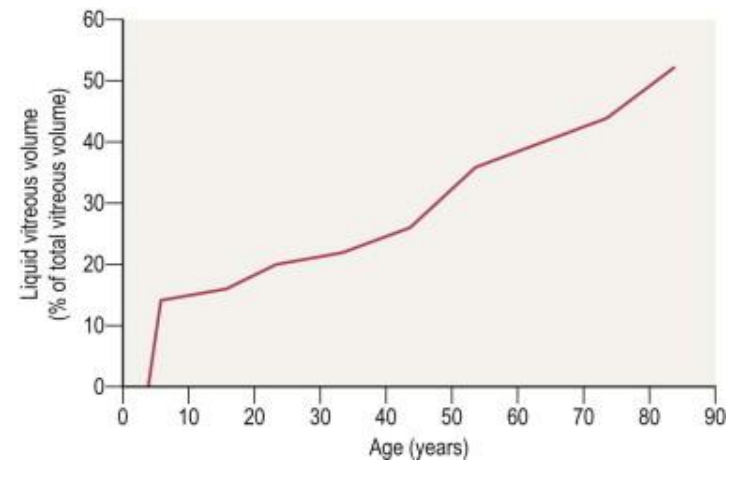
Liquefaction
Infant vitreous: homogenous gel
With age, gel volume decreases & liquid volume increases
40 yrs: 80% gel/20% liquid
80 yrs: 50% liquid
Exact molecular mechanism unclear
Hyaluronic acid is redistributed from the gel to the liquid
Most liquefaction in center, where there is the least amount of collagen
Gel dissolves and is replaced with lacunae
Lacunae melt together over time
Age-related vitreal changes are associated with age related ocular disease:
Nuclear sclerotic cataract
Diabetic retinopathy
Intact, normally composed vitreous provides “protection”
Brings nutrients to ocular structures
Takes waste, metabolites, bad stuff away
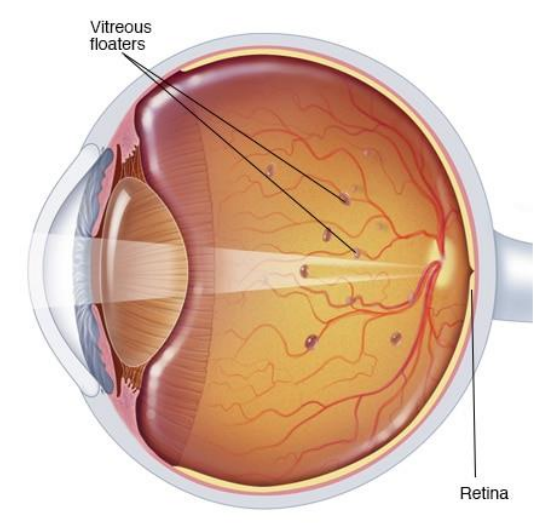
Clinical Connection: Floaters
As vitreous gel liquefies, collagen complexes form clumps & bundles
Shadows cast on retina, seen as floating spots
Most noticeable on white wall/blue sky
May be a sign of retinal pathology
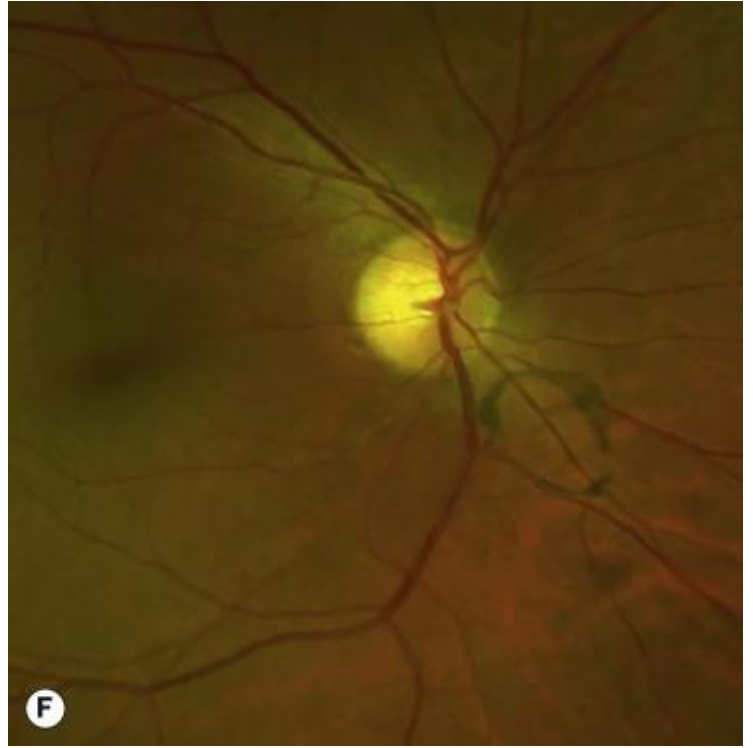
Clinical Connection: Posterior Vitreous Detachment (PVD)
Collapse of the vitreous body
Cortex sinks to center
Due to normal liquefaction and age changes
Posterior vitreous detaches from the retinal internal limiting membrane at the peripapillary ring
May occur prematurely in cases of trauma, high myopia, etc.
Weiss Ring (Senile Annular Ring)
Glial tissue from peripapillary attachment may remain in vitreous after PVD
Appears as a circular ring on examination, just over the nerve
Patient may see large floaters for days/weeks after detachment
During acute PVD stage, patients may notice an increase in floaters
If there is a particularly strong attachment between the posterior hyaloid and the ILM of the retina, a PVD may result in:
A retinal break (tear, hole)
Vitreo-retinal traction, especially in the foveal region
Monitor patients 4-6 weeks after PVD onset for retinal complications
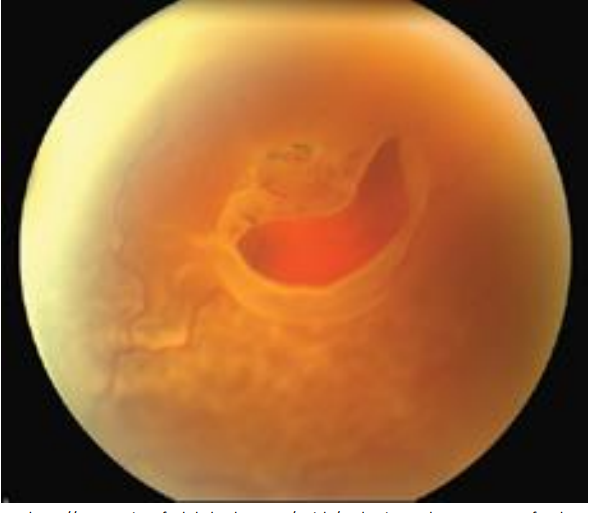
Clinical Connection: Vitreoretinal Traction
The Vitreoretinal Interface
Vitreous cortex attached to ILM at :
Vitreous base
Optic disc
Macula
Vessels
Strongest in youth
Traction may occur with
Liquefaction changes
Trauma
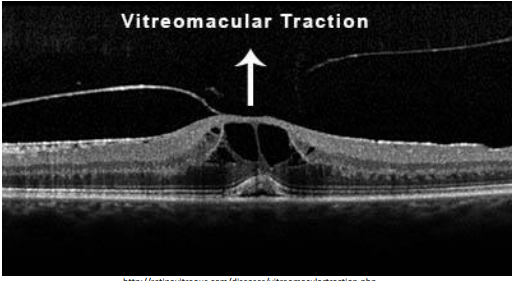
Clinical Connection: Vitreoretinal Traction + Floaters
Treatment
Monitor
Vitrectomy
Medication/Injectables
Laser surgery- target disruptive floaters but not recommended