HSS 390 Ch. 16 Special Senses
1/81
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
82 Terms
Sensory receptors
Anatomical structures specialized to detect a stimulus that act as transducers; may be simple in structure or a complex sense organ
Sense organ
Nerve tissue surrounded by other tissues that enhance response to a certain type of stimulus (e.g., the eye and cochlea)
Transduction
Process by which a stimulus energy is converted into electrical energy (an action potential); receptors will have a resting membrane potential (RMP) and stimulus will open a modality-gated ion channel specific to the receptor
Ion flow → AP → conducted toward CNS for perception & interpretation
Chemoreceptors
Detect chemicals dissolved in fluid (e.g., smell or taste of food; oxygen levels in blood)
Thermoreceptors
Detect changes in temperature (thermo- = heat; e.g., receptors in skin, hypothalamus)
Photoreceptors
Detect changes in light (photo- = light; e.g., in the retina of eye [vision])
Mechanoreceptors
Detect physical/mechanical distortion of cell membrane (e.g., touch, pressure, vibration, stretch receptors; hearing & equilibrium)
Nociceptors
Detect pain stimuli (noci- = pain; e.g., chemical, heat, or mechanical damage to tissues)
General sensory receptors
Simple structures distributed throughout the body
Somatic sensory receptors — monitor touch, pain, pressure, vibration, temperature, & proprioception
Visceral sensory receptors — found in tissue of organs; monitor stretch, chemical environment, temperature, & pain
Special sensory receptors
Specialized sensory receptors in complex sense organs of the head; detect 5 special senses — olfaction, gustation, vision, hearing, & equilibrium
Olfaction
Detection of odorants in the air (olfact- = smell), chemicals that, when dissolved in nasal mucus, are detected by chemoreceptors
Olfactory epithelium/mucosa
The sensory receptor organ for olfaction located in the roof of the nasal cavity; contains…
1st order neurons of smell: 10-20 million olfactory receptor cells (neurons) that detect odorants
Basal cells: act. as regenerating stem cells; replace olfactory receptor cells every 40-60 days
Supporting cells: act as glial cells to support olfactory receptor cells
1st order neurons of smell
Olfactory receptor cells (neurons) that detect odorants
Unique neurons — still undergo mitosis & are exposed to the environment
One end has cilia (“olfactory hairs”) with chemoreceptors embedded in mucus
Other end is the axon; axons collectively travel upwards as olfactory nerve (CN I)
2nd order neurons of smell
Located in olfactory bulb; their axons form the olfactory tract
Transduction of olfaction
Odorant dissolves in mucus → stimulates chemoreceptor on olfactory “hairs” (cilia) of olfactory receptor cell (1st order neuron)
G-protein in receptor cell activates adenylate cyclase, converts ATP to cAMP
cAMP opens ion channels for Na+ and Ca2+ (move INTO cell)
Depolarization → AP in axons of CN I → conducted to 2nd order neuron in olfactory bulb
Pathway of olfaction
Olfactory nerve (CN I — 1st order neuron)
Olfactory bulb (2nd order neurons; axons from olfactory tract)
Primary olfactory cortex (in temporal lobe)
Hypothalamus (salivation, hunger, increased stomach acid, gagging, vomiting) OR amygdala/hippocampus of limbic system (emotion/memory related to smells)
*Does NOT involve the thalamus; olfactory bulb acts as the thalamus (“router”)
Gustation
Detection of tastants, molecules/ions in food/drink (gust- = taste); when dissolved in saliva, are detected by chemoreceptors
Taste buds
The sensory receptor organ for taste located on the tongue; contain…
Taste/gustatory cells: modified epithelial cells that behave like neurons (but are NOT true neurons); detect tastants
Basal cells: act as regenerating stem cells; replace gustatory cells
Supporting cells: act as glial cells to support gustatory cells
Gustatory cells
Modified epithelial cells that behave like neurons and detect tastants; have microvilli (“taste hairs”) that contain chemoreceptors
Release neurotransmitters onto sensory nerve fibers at their base
Sensory nerves for taste belong to CN VII (ant. 2/3 of tongue) & CN IX (post. 1/3 of tongue)
Transduction of gustation
Tastant dissolves in saliva → stimulates chemoreceptors on taste “hairs” of gustatory cells → depolarization/AP depends on “tastant” causing taste sensation…
G-protein & cAMP = sweet, bitter, umami
Opening of ion channels = salty, sour
Once depolarization, gustatory cell releases neurotransmitter at its base, which excites sensory nerve fibers
Sweet
Taste produced by organic carbohydrate molecules
Depolarization through G-protein & cAMP
Bitter
Taste produced by organic molecules containing nitrogen, often with basic pH (e.g., unsweetened chocolate, nicotine, caffeine)
Depolarization through G-protein & cAMP
Umami
Taste associated with protein molecules producing meaty flavor
Depolarization through G-protein & cAMP
Salty
Taste produced by metal ions (e.g., Na+ and K+)
Depolarization through opening of ion channels
Sour
Taste associated with acids (H+ ions) (e.g., vinegar)
Depolarization through opening of ion channels
Pathway of gustation
Facial (CN VII) and glossopharyngeal (CN IX) nerves (formed by 1st order neurons found in ganglia)
Medulla oblongata (2nd order neurons)
THEN…
Thalamus (3rd order neurons)
Primary gustatory cortex (in insula)
OR…
Hypothalamus (salivation, hunger, gagging, vomiting) OR amygdala/hippocampus of limbic system (emotion/memory related to food)
Vision
Perception of objects, color, and movement in the environment by means of the light they reflect/emit); light rays must enter the eye and be focused on the photoreceptors found in the retina
Optical components
Transparent structures that admit light rays and focus them on the retina, includes the cornea, aqueous humor, lens, & vitreous humor
Tunics of the eye
“Cloaks/coverings” forming the wall of the eyeball; includes the fibrous tunic, vascular tunic, & retina
Fibrous tunic
Outer, fibrous, avascular layer; consists of the sclera & cornea
Sclera
Part of the fibrous tunic of the eye; the dense, collagen-rich “white “ of eye (sclera- = tough, hard)
Cornea
Part of the fibrous tunic of the eye; the transparent region of modified sclera in front of eye that admits and refracts light
Vascular tunic
Middle vascular layer of the eye; consists of the choroid, ciliary body, & iris
Choroid
Part of the vascular tunic of the eye; rich in capillaries & melanocytes (melano- = dark, black)
Capillaries nourish retina
Melanin pigment absorbs light & prevents scattering of light rays
Ciliary body
Part of the vascular tunic of the eye; an extension of the choroid that forms a muscular ring around the lens
Supports lens & iris
Secretes aqueous humor
Iris
Part of the vascular tunic of the eye; the colored diaphragm controlling size of pupil (opening)
Eye color is determined by the amount & type of melanin in melanocytes
Photopupillary reflex
Visceral reflex of the ANS in response to light (photo- = light); involves two sets of smooth muscle on the posterior iris
Light → contraction of pupillary constrictor muscle (parasympathetic preganglionic axons travel with CN III)
Narrows focus of light onto the center of the lens, where there is maximal curvature
Low light (or sympathetic stimulation) → contraction of pupillary dilator muscle
Retina
Inner, neural tunic (layer); consists of pigmented and neural layers (contains photoreceptors)
Pigmented layer of retina
Layer of the retina internal to the choroid that provides vitamin A and regenerates rhodopsin for photoreceptors; diffuses nutrients from choroid to neural layer
Has melanin to attract light rays & prevent them from reflecting off retina
Neural layer of retina
Houses photoreceptors and other neurons associated with vision
Photoreceptor cells
NOT neurons — cells that absorb light using photopigments and initiate signal; include rods and cones
Rods
Highly sensitive photoreceptor cells that work well in reduced light and night vision; provide poor contrast in shades of gray
Contain the photopigment (light-absorbing molecule) RHODOPSIN
Cones
Photoreceptors that function in color, clarity, and day vision; they are less sensitive and require brighter light
Contain 3 types of photopigments (light-absorbing molecules) called PHOTOPSINS with sensitivity to light of different wavelengths (and therefore, color — red, green, & blue cones)
Colorblindness results when a photopsin is lacking or deficient due to genetic mutation (X-linked → higher probability in males)
Bipolar cells
First-order neurons of vision; dendrites synapse with rods & cones and axons synapse with ganglion cells
Ganglion cells
Second-order neurons of vision located in a single layer next to the vitreous body; axons from the optic nerve (CN II)
Pathway of light to the retina
Ganglion layer → bipolar layer → photoreceptors → pigmented layer
Opthalmoscope
Tool that is used to examine the fundus (rear) of the eye, namely the retina (ops- = eye; scope- = examine, observe, see)
Optic disc
Area on the fundus where blood vessels enter/exit and axons of ganglion cells (CN II) exit; no photoreceptors = “blind spot”
Macula lutea
Patch of cells in the center of the fundus containing the fovea centralis (macula- = little spot; lutea- = yellow)
Fovea centralis
Area in the center of the macula lutea; high density of cones with almost no rods → point of highest visual clarity/detail
Every other area of the retina contains primarily rods and functions well in low light
Refraction of light rays
Bending of light rays required to focus them on the fovea centralis; light rays are bent when they pass through the cornea and lens (shape of cornea does not change, but the lens curves as objects move closer to the eye)
Accomodation
The lens becomes increasingly curved/spherical as objects move closer to the eye; this bends light rays more & more to focus them on the fovea centralis
Far = lens is Flat
Close = lens is Curved
Ability of lens to curve lessens with age due to decrease in elastic fibers
Photopigments
Light-absorbing molecules in rods & cones; consist of opsin protein + light-absorbing retinal (made from Vitamin A)
Light adaptation (adjusting from low light → bright conditions)
Pupils constrict due to photopupillary reflex
Retinal is initially “bent” in cis-retinal form
Light rays → retinal straightens into trans-retinal form
Retinal separates from opsin (“bleaching” of retinal) — photopsin in cones is quickly regenerated; cones take over
Dark adaptation (return of sensitivity to low light after bright light)
Pupils dilate due to low light
Bleached retinal must be regenerated to cis-retinal (“bent”) form for rods to function again in low light
Cis-retinal rejoins with opsin; rhodopsin now functions again — may take 20-30 mins. for rhodopsin to be fully regenerated
All rods and cones use _____ with bipolar cells.
Glutamate
Use of glutamate in vision
All rods and cones use glutamate with bipolar cells
Glutamate release is continuous in the dark; when light “bleaches” the retina, glutamate release stops
Bipolar & ganglion neurons both have “on” and “off” versions that are excited or inhibited by glutamate; when light intensity changes, the shift in excitation (APs) is percieved as images
Pathway of vision (signal)
Bipolar cells/neurons (1st order neurons)
Optic nerve (CN II; axons of ganglion cells; 2nd order neurons)
Optic chaism (crossing half of the axons in each optic nerve)
Optic tracts to thalamus (3rd order neurons)
THEN…
Midbrain (superior colliculi for visual reflexes/nucleus of CN III for photopupillary reflex)
OR…
Primary visual cortex (occipital lobe)
Because of optic chiasm, damage to one occipital lobe will result in partial blindness in _____.
Each eye (both eyes)
Hearing
Perception of sound (waves) due to vibrations; relies on mechanoreceptors and signals are transported via vestibulocochlear nerve (CN VIII)
Equilibrium
Awareness and monitoring of head position; relies on mechanoreceptors and signals are transported via vestibulocochlear nerve (CN VIII)
Combines visual and proprioception inputs
Maintains coordination, balance, and orientation in 3-D space
Sections of ear
Outer, middle, and inner ear
Outer & middle — transmit vibrations (sound detection)
Inner ear — vibrations cause fluid pressure waves, which is converted to APs
Outer/external ear
Consists of the auricle and external acoustic meatus, which funnel sound waves inward to the tympanic membrane (vibrates when sound waves hit it)
Middle ear
An air-filled cavity containing the auditory ossicles and auditory tube
Auditory (Eustachian) tube
Passage extending from middle ear to nasopharynx; yawning, swallowing, & chewing allows air movement through the tube & equalizes pressure on either side of the tympanic membrane
Middle ear infections (otitis media) often result from infections spreading from the throat to the middle ear through the auditory tube
Auditory ossicles
Three tiny bones of the middle ear; tympanic membrane is attached to malleus, which vibrates the incus, which vibrates the stapes (MIS)
Stapes moves in and out of oval window, initiating pressure waves in the inner ear fluid
Inner ear
A bony labyrinth of spaces carved out of the temporal bone consisting of membrane-lined, fluid-filled tubes; three main regions — cochlea, vestibule, semicircular canals
Cochlea
Part of the inner ear responsible for hearing (cochlea- = snail shell); consists of three fluid-filled chambers separated by membranes
Cochlear duct
Middle chamber of the cochlea filled with endolymph and containing spiral organ; separated from…
Scala vestibuli by vestibular membrane
Scala tympani by basilar membrane
Spiral organ
A sensory epithelium containing “hair cells” sitting on the basilar membrane; found within the cochlear duct contains mechanoreceptors for hearing
Hairs cells are NOT neurons, but they release neurotransmitter onto dendrites of neurons associated with CN VIII
Hair cells have microvilli (“stereocilia”) covered by a gelatinous tectorial membrane
Primary/1st order neurons of CN VIII are in spiral ganglion
Inner hair cells
Located in a single row within the spiral organ & act as main mechanoreceptors; communicate with 90% of the dendrites in CN VIII
Outer hair cells
Located in three rows within the spiral organ; act to “tune” the inner hair cells and can tense the basilar membrane
Scala vestibuli
Superior chamber of the cochlea filled with perilymph; begins at oval window and spirals up to apex
Scala tympani
Inferior chamber of the cochlea filled with perilymph; begins at apex and spirals down to round window
Transduction of sound
Inner hair cels contain K+ ion channels at their tips and tip link proteins that connect them
Surrounding endolymph is HIGH in K+
Every time the basilar membrane moves up, hair cells and pushed into tectorial membrane & their tips are tilted
Physical distortion of tip links pulls open K+ ion channels (mechanically-gated channels)
K+ will diffuse INTO the hair cell and depolarize it
Hair cell releases neurotransmitter from its base, exciting the sensory neuron of CN VIII, leading to an AP
When the basilar membrane moves down, the process reverses, ion channels close, and neurotransmitter release stops
Pathway of hearing
CN VIII (cochlear branch of vestibulocochlear nerve; 1st order neurons in spiral ganglion)
Cochlear nucleus (in medulla oblongata; 2nd order neurons)
Midbrain (inferior colliculi for startle response & reflex turning of head to sound; 3rd order neurons)
Thalamus (4th order neurons)
Primary auditory cortex (located in temporal lobe)
**Excessive decussation/crossing of axons; rarely unilateral hearing loss if one cortex is damaged
Vestibular apparatus
Contains the mechanoreceptors for equilibrium; consists of the vestibule and semicircular ducts
Vestibule
Part of the vestibular apparatus that detects orientation when head is erect (“static equilibrium”) vs. tilted and linear acceleration (e.g., riding in an elevator or accelerating in a car)
Consists of two chambers — saccule and utricle
Receptors are found in macula
Macula
Within the utricle & saccule; patches of hair cells with stereocilia and one kinocilium projecting into gel called the otolithic membrane
Otolithic membrane contains calcium carbonate crystals that give it weight and make it responsive to gravity/motion (e.g., head erect = minimal movement of otolithic membrane and minimal stimulation of hair cells)
Hair cells are synapsing with the vestibular branch of VIII
Semicircular ducts
Part of the vestibular apparatus that detects rotational/angular acceleration (e.g., spinning in a chair or shaking your head “no”)
3 semicircular ducts are oriented in a different plane, to detect different planes of rotation
Receptors are found in ampulla
Ampulla
A dilated sac within each semicircular duct; each ampulla has a mound of hair cells called the crista ampullaris
Contains stereocilia and kinocilium embedded in a gel called the cupula
When head rotates, endolymph pushes against cupula, bending stereocilia
If stereocilia bend toward kinocilium, the hair cell depolarizes
If stereocilia bend away from kinocilium, the hair cell repolarizes
Hair cells are synapsing with the vestibular branch of VIII
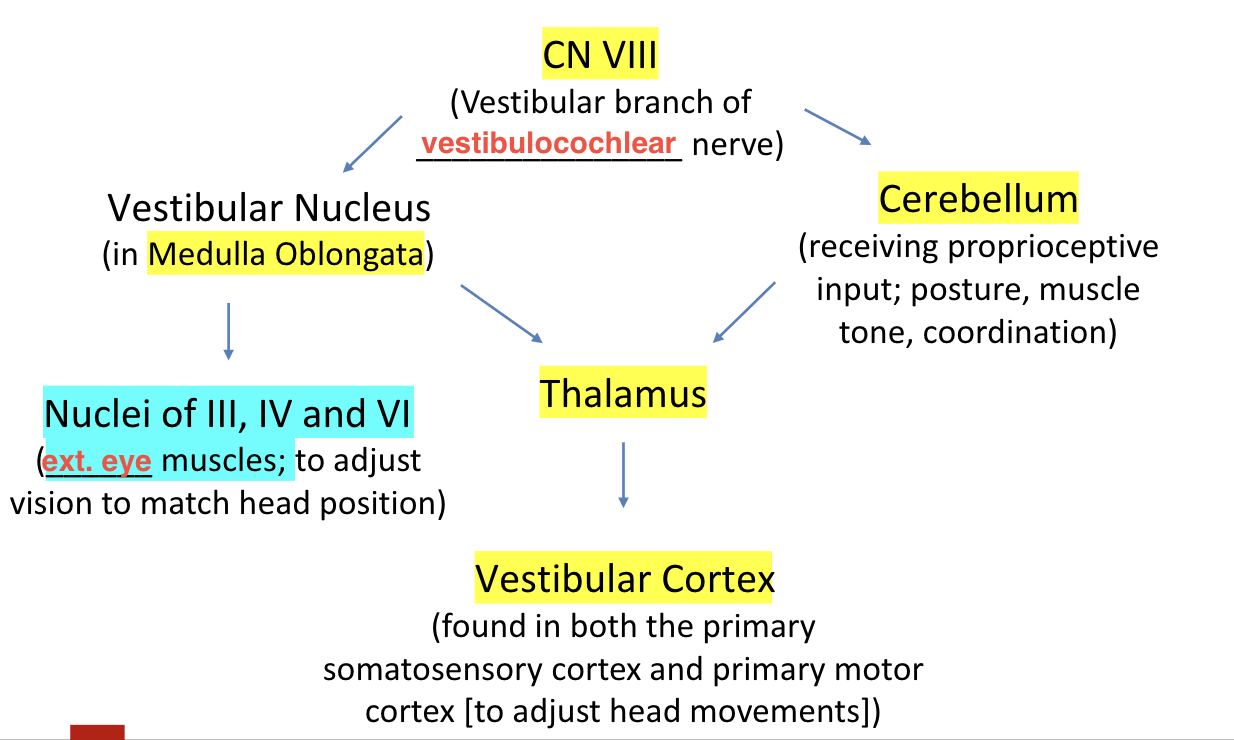
Pathway of equilibrium