Insulins
1/85
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
86 Terms
Main cause of diabetes
Dysfunction of the pancreas or burn out
Autoimmune disease that destroys pancreatic beta cells → little to no insulin produced; patient requires exogenous insulin; diagnosed in childhood (makes up 10% of cases)
T1DM
A combination of hyperglycemia and insulin resistance/lack of sensitivity. Pancreas “burns out” over time as insulin resistance develops
Patient’s caloric intake raises so much that body makes more insulin, and body become less responsive to insulin
Is also a supply & demand issue where body’s demand for insulin is high and supply can’t keep up; patient has chronic state of pumping out insulin which burns out pancreas
Makes up 90% of cases
T2DM
Pancreatic cells that produce and secrete insulin (lower BG)
Beta cells
Pancreatic cells that produce and secrete glucagon (raise BG)
Alpha cells
Pancreatic cells that produce and secrete somatostatin
S cells
Why does pancreas become dysfunctional in type 2 diabetes?
Patient’s caloric intake raises so much that body makes more insulin, and body become less responsive to insulin
Is also a supply & demand issue where body’s demand for insulin is high and supply can’t keep up; patient has chronic state of pumping out insulin which burns out pancreas/pancreas can’t keep up with high caloric intake
Patient develops insulin resistance
Insulin that your body (pancreatic beta cells) produces
Endogenous insulin
Insulin that is given as a medication
Exogenous insulin
Background insulin; insulin that remains in bloodstream and controls glycemic index throughout the day. DOES NOT account for glycemic spikes
prolonged duration; do not peak
Basal insulin
Type of insulin that is first line INSULIN for controlling hyperglycemia; has prolonged duration but does not peak; counteracts hormonal fluctuations (e.g. cortisol)
Basal insulin
A dose to control BG after consuming meals (post prandial); controls glycemic spikes; used in combination with basal insulin (that acts throughout the day)
Is fast acting
Can cause hypoglycemia more commonly
Bolus insulin (rapid/short-acting)
Bolus vs basal insulin
Bolus insulin → control BG after meals (glycemic spikes)
Can cause hypoglycemia more commonly; is faster acting
Basal insulin → control BG throughout the day
Insulin that has
O: 15 min or less
P: peaks at 30-90 min OR (1-2 hrs)
D: is 3-5 hrs
Rapid-acting insulin
Insulin that has
O: 30 min – 1 hr
P: peaks at 2-3 hrs OR 1.5 hrs
D: is 5-7 hrs
Regular/short-acting insulin
Insulin that has
O: 1-2 hrs
P: peaks at 8-12 hrs
D: is 18-24 (take half a day; take twice a day)
Intermediate-acting insulin (NPH)
Insulin that has
O: 1-2 hrs
P: does not peak
D: duration stays in background for 18-24 (some formulations can last longer; lasts all day)
Long-acting insulin (AKA basal insulin)
Examples of bolus dose insulin
Rapid-acting or regular/short-acting insulin
Why give rapid-acting or short-acting (regular) bolus insulin before meals?
Patient will be hypoglycemic if they don’t eat (e.g. BG 180). Check BG an hour before and after administration (for regular insulin, check 2 hrs after)
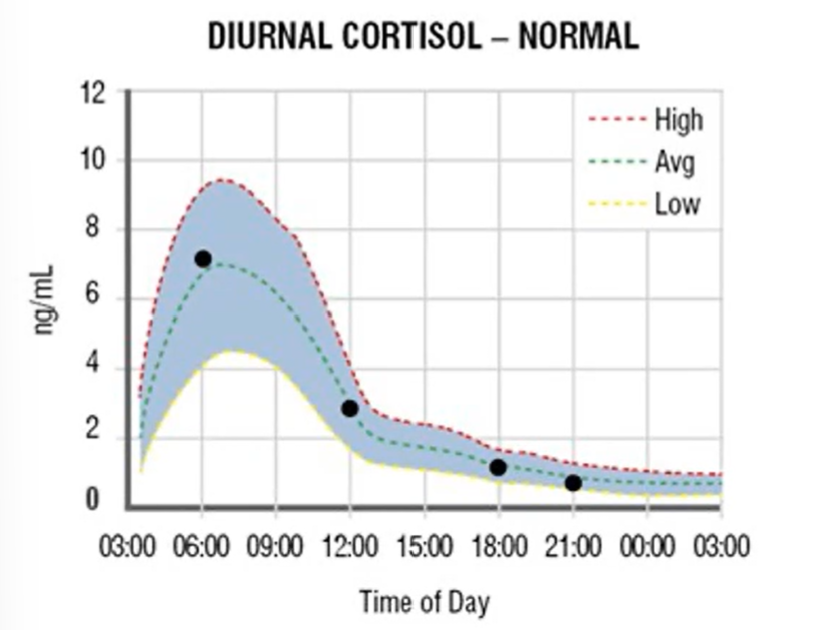
When does cortisol peak?
When patient wakes up in the morning (6 AM) → High BG
Insulin indication
Diabetes → All of type 1; only some of type 2 (depends on genetic, caloric intake; when beta cells no longer produce endogenous insulin)
ESRD (management of acute hyperkalemia) + given with dextrose
As an antidote (CCBs + BBs)
All type 1 and type 2 diabetic patients need insulin. True or false?
False
Lab test used to diagnose someone with diabetes; is average glucose for the past 2-3 months
Hgb A1C
Hgb A1C is 5.7-6.4% =
Pre-diabetes stage; less than 5.7% = normal
Hgb A1C ≥ 6.5%
Formally diagnosed diabetes; beta cell function is diminished
First line treatment for diabetes
Lifestyle modifications (diet, exercise)
What does hyperglycemia do to the body?
High glucose in bloodstream cause blood to become sluggish/viscous → cause retinopathy, nephropathy, neuropathy, cardiovascular risk
Insulin ROA
Typically SubQ injection; Afrezza is inhaled; type 1 diabetics may have a pump
The only insulin that can be given IV
Regular (short-acting) insulin
SE of insulin
Hypoglycemia (most common/dangerous SE)
Assess for hypoglycemia depending on insulin type
S&S of hypoglycemia
Sweating
Pallor
Hunger
Irritability
Lack of coordination
Sleepiness
SPHILS (S&S of hyperglycemia
S – Sweating
P – Pallor
H – Hunger
I – Irritability/aggressive
L – Lack of coordination
S – Sleepiness
Interventions for hypoglycemia
Awake AAOx4 (responsive) patient → 15-15 rule
Unresponsive patient → if IV access present, give 25g D50 IV push; no IV → IM glucagon (patient may develop anxiousness, tachycardia, NV)
15-15 rule
For hypoglycemic awake AAOx4 patients and can tolerate PO
Give 15 g rapidly absorbed carb (e.g. juice, tsp of sugar, glucose products) → check BG in 15 mins
Repeat until BG WNL
Interventions to treat a hypoglycemic patient that is unresponsive, AMS, airway not protected, can’t swallow
If IV access → administer a 25-50% glucose solution such as 25g D50 IV push (could develop hyperglycemia)
If no IV → IM 0.5 OR 1 mg glucagon (patient may develop anxiousness, tachycardia, NV)
FREQUENT monitoring
Diabetes is a major, if not the major cause of
Acquired vision loss
Kidney failure
Non-traumatic lower extremity amputation
S&S of hyperglycemia (diabetes)
Common symptoms: polyuria, polydipsia, polyphagia, neurological symptoms
T1DM: DKA → diabetic ketoacidosis; acetone → fruity body odor
T2DM: Hyperosmolar hyperglycemic non-ketotic syndrome (HHNK) → no acetone, no fruity body odor
Autoimmune diabetes; patient is young; moderate genetic disposition, no insulin = ketosis, usually not obese. Needs insulin to live
T1DM
T2DM has a
Strong genetic disposition, patient is usually obese
No oral drugs are currently approved to treat T1DM. True or false?
True
Diabetes insipidus is a type of DM. True or false?
False
Hormonally active, may increase insulin resistance
Fat cells
Carry nutrients, contain potassium
RBCs
Criteria for diabetes
Hgb A1c ≥ 6.5%
Fasting glucose (nothing eat/drink for 8 hrs) > 126
OGTT (2hr after administering sugary drink) > 200 mg/dL
A1C values
Normal < 5.7%
Prediabetes ≥ 5.7-6.4%
Diabetes ≥ 6.5%
FBG values
Taken 8 hrs after no meals/drinks
Normal < 100 mg/dL
Prediabetes ≥ 100 mg/dL
Diabetes ≥ 126 mg/dL
OGTT values
Normal < 140 mg/dL
Prediabetes ≥ 140 mg/dL
Diabetes ≥ 200 mg/dL
Insulin therapy is always needed in T1DM (AKA IDDM). True or false?
True
Insulin therapy is sometimes, or eventually needed in NIDDM or T2DM
Up to 1/3 of the time
Name the rapid-acting insulins
AKA the “logs”
Lispro (HumaLOG)
Aspart (NovoLOG)
Glulisine (Apridra)
LAG (rapid-acting insulins)
L – Lispro (HumaLOG)
A – Aspart (NovoLOG)
G – Glulisine (Apridra)
Rapid-acting insulin indication
For post-prandial hyperglycemia (mimic bolus insulin dose)
The only insulin appropriate for acute management of
DKA
HHS (Hyperosmolar Hyperglycemic State; leads to dehydration)
Acute hyperkalemia
IV regular insulin (short-acting insulin)
Short-acting insulin indication
Only insulin for acute management of DKA, HHS, acute hyperkalemia (IV form)
Only insulin that can be given IV
Name the intermediate acting insulins
NPH, (Humulin N, Novolin N)
Intermediate acting insulins is cloudy, this is abnormal. True or false?
False
Insulins that mimic bolus insulins
Rapid-acting & short-acting (regular) insulin; negate post-prandial BG spike
Insulins that provide basal dosing
Intermediate and long-acting insulins
Long-acting insulin has a peak. True or false?
False
Hypoglycemia is defined as BG < ______ mg/dL
70
Can occur with rapid correction of BG by antidiabetics/insulin
Patient may have AMS (confused, agitated)
Can be life-threatening → prompt recognition and treatment
Hypoglycemia
Hallmarks of T2DM
3 Ps; Polyuria, polydipsia, polyphagia,
Blurred vision (retinopathy), neurological symptoms
How to mix intermediate insulin (NPH) and and regular insulin
(CLEAR BEFORE CLOUDY) or RN
Clean both vials
Inject air into cloudy (NPH)
Inject air into regular
Withdraw regular
Withdraw NPH
Give patient insulin at night, patient experiences S&S of hypoglycemia (jittery, nauseous, irritable) during the night. Patient experiences rebound effect during the morning and experiences massive hyperglycemia. 2 am or 3am; nurse should check BG. If it’s very low, and then high in morning = Somogyi effect → treat by giving patient a snack such as crackers just before patient sleeps
Somogyi effect
Patient gets insulin at night, but patient gets rebound hyperglycemia during the morning. Patient does not have an episode of hypoglycemia during the night.
Dawn phenomenon
S&S of hypoglycemia
Sweating
Hungry
Lethargic
Irritable/AMS
Pallor
Sleepy
SHLIPS (S&S of hypoglycemia)
S – Sleepy
H – Hungry
L – Lethargic
I – Irritable/AMS
P – Pallor
S – Sweating
What insulins can be mixed?
Rapid or regular can be mixed with intermediate
Rapid/regular mix doesn’t make sense → both are bolus
DO NOT mix long-acting → give alone
NPH (intermediate-acting insulin) considerations
Ideally taken BID. If patient needs 10 units, give ⅔ dose in the morning, and ⅓ in the evening
Only insulin that’s normally cloudy
Can be mixed with regular or rapid insulin
Cloudy regular insulin =
Expired/spoiled → replace
RN =
Regular before Intermediated (clear before cloudy when mixing)
Brand name and drug class for metformin
Glucophage; biguanide
Diagnosing diabetes
FBG > 126 mg/dL
OGTT > 200 mg/dL (after 2 hrs)
Hgb A1C > 6.5%
Random glucose ≥ 200 mL/dL
T1DM vs T2DM presentation
T1DM = Usually thinner, younger
T2DM = Obese, acanthosis nigricans, ↑ triglycerides
A cluster of findings that increase r/o
T2DM
CVD
Stroke
Metabolic Syndrome
Diagnostic criteria for metabolic syndrome
Abdominal obesity
Increased triglycerides
Decreased HDL
HTN
Elevated FBG
Treatment of DKA
Replace fluids/fluid resuscitation FIRST
IV regular insulin 0.1 units/kg/hr
Replace K+ (insulin pulls glucose AND potassium with it)
Treatment of HHS
6+ liters of 0.9% NS (treat profound dehydration)
IV regular insulin
Name the long-acting insulins
Glargine (Lantus/SoloStar)
Detemir (Levemir)
Degludec (Tresiba)
Semglee (Glargine)
Basaglar (Glargine)
Long-acting insulin that lasts ultra-long
Degludec (Tresiba)
When to take intermediate-acting insulin doses?
BID
2/3 dose in the morning
1/3 at night
Complication of T1DM
Breakdown of fats/muscles to use as fuel (bc absence of insulin)
Acetone
B-hydroxybutyrate
Metabolic acidosis
Hyperglycemia
Abd pain (unique to DKA)
Dehydration/diuresis
DKA
Complication of T2DM
Still have some insulin
Have just enough insulin to stay out of DKA
Blood sugar creeps up (slow onset)
No ketones
Glucose > 500, 600, 700
More profound dehydration
Neurological manifestations (unique to HHS)
HHS
Name the short-acting (regular) insulins
End in R: Humulin R & Novolin R
Nursing considerations for rapid-acting insulin
Meal must be IN SIGHT
Food must be at bedside
Highest r/o hypoglycemia
Regular insulin ROA
SubQ, IM, IV