T20 Anaerobic Bacteria
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
74 Terms
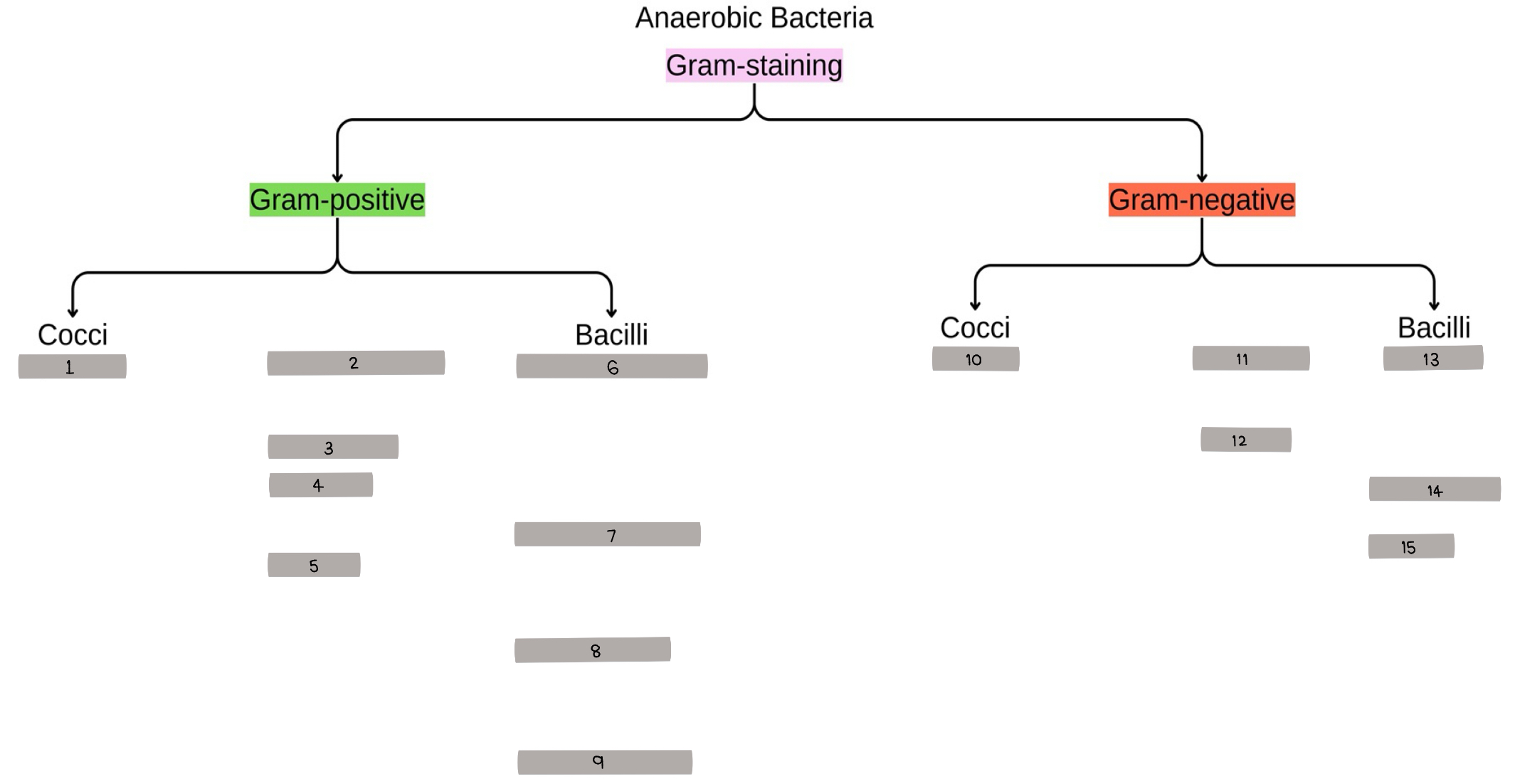
fill in the blank: 1
Peptococcus
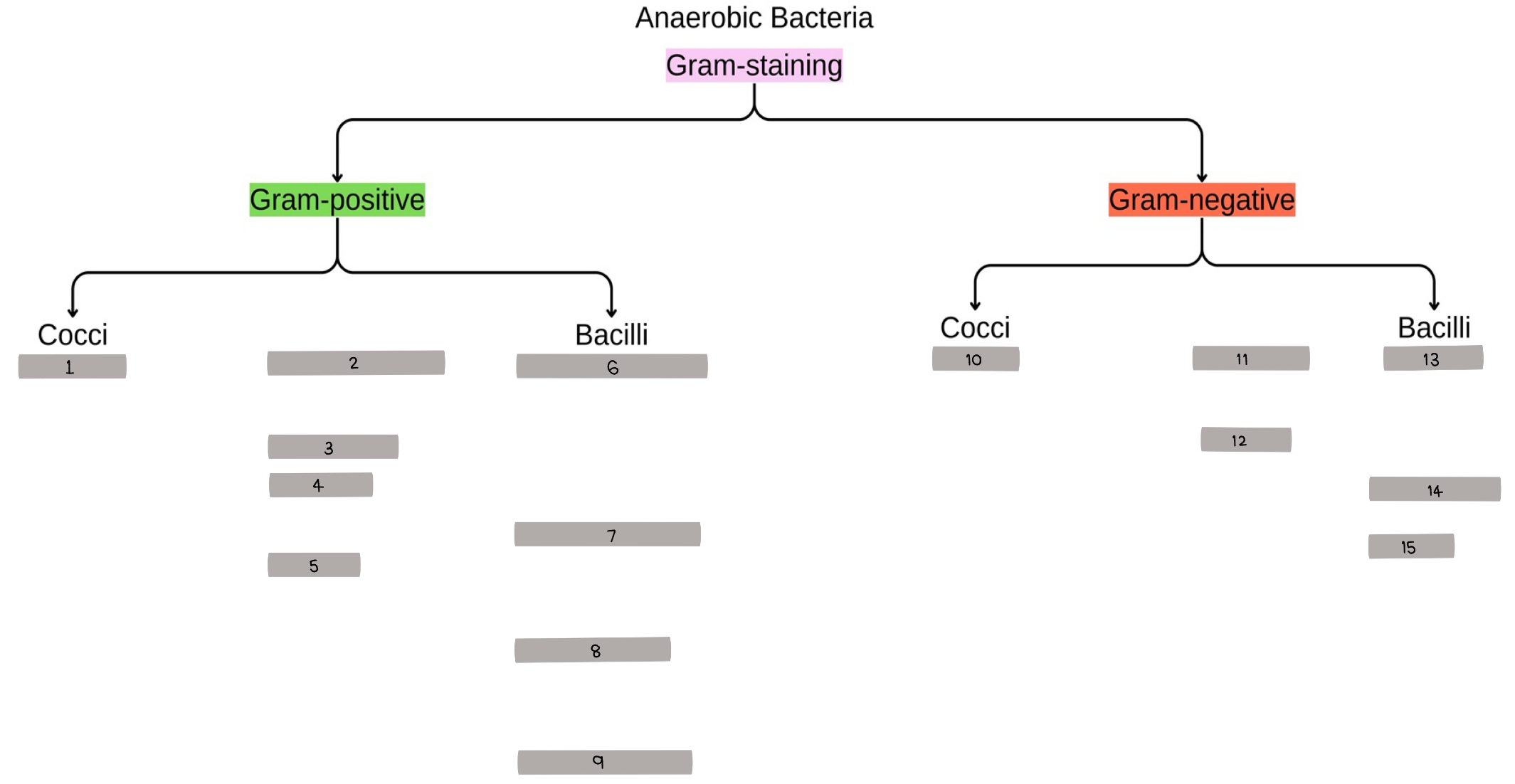
fill in the blank: 2-9
Clostridium perfringens, Clostridium botulinum, Clostridium tetani, Clostridioides difficile, Cutibacterium acens, Bifidobacterium, Lactobacillus, Actinomyces
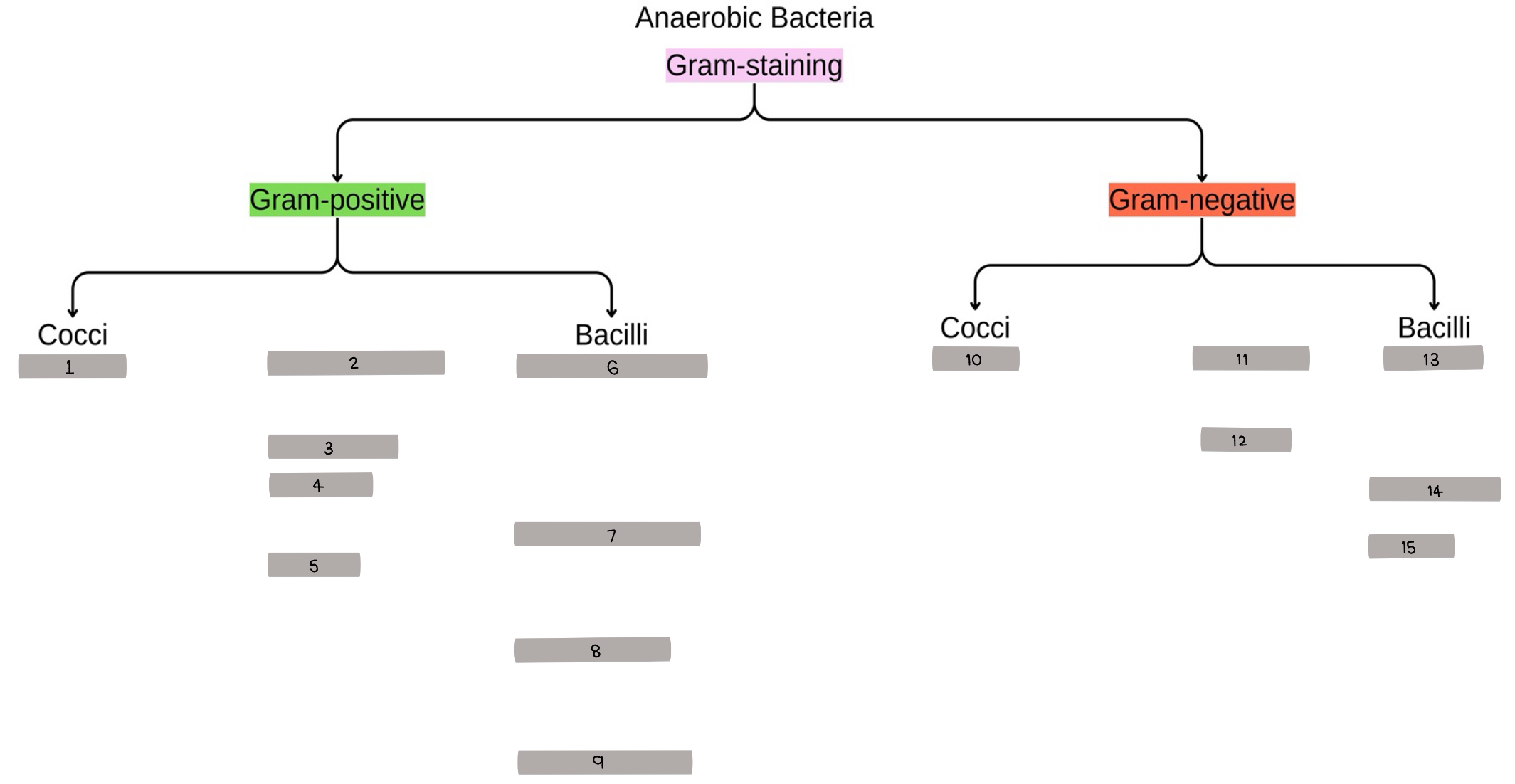
fill in the blank: 10
Veillonella
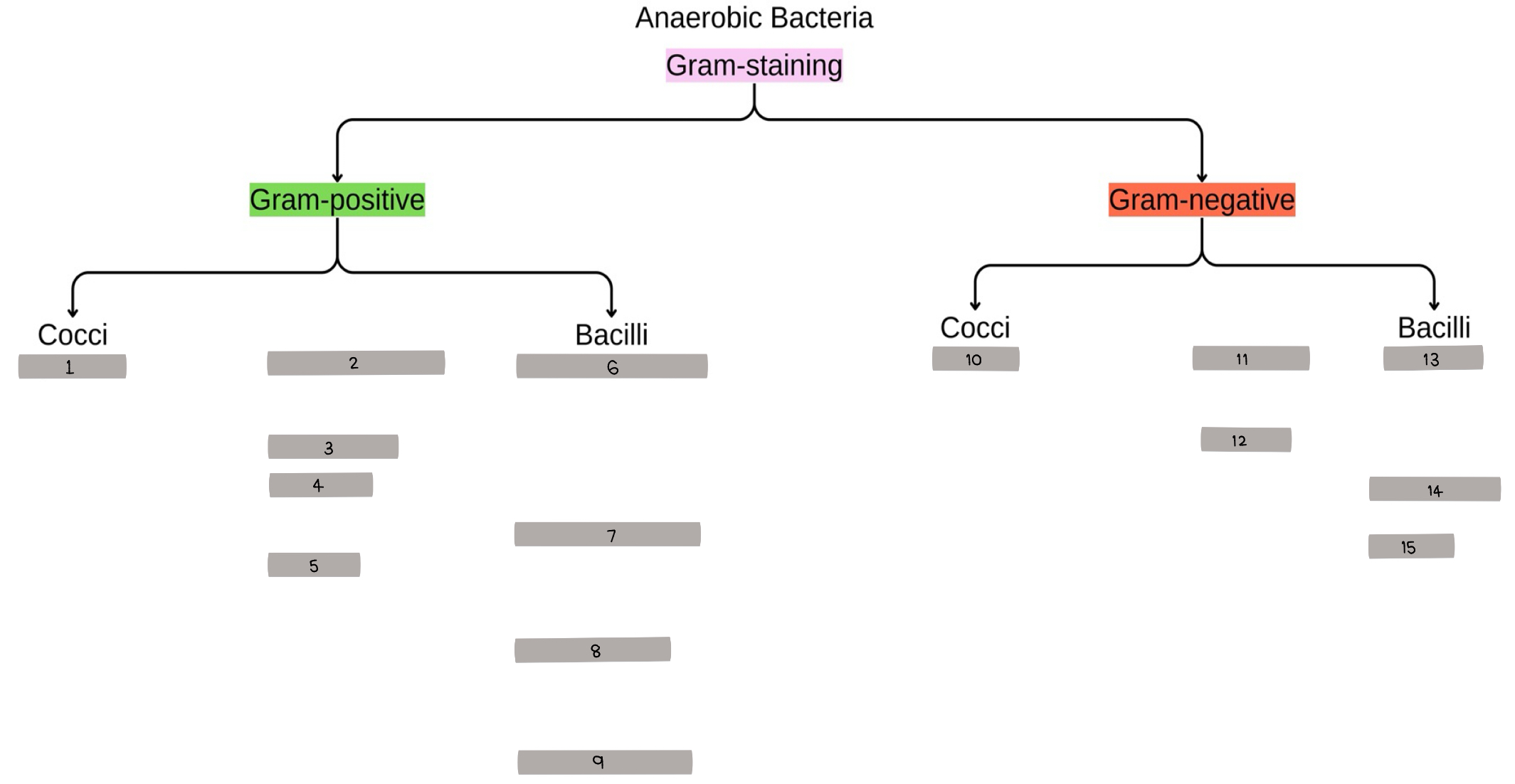
fill in the blank: 11-15
Fusobacterium, Gardnerella, Bacteroides, Porphyromonas, Prevotella
enzymes that allow aerotolerance
catalase
peroxidase
superoxide dismutase
superoxide reductase
anaerobic specimen transport
jar with sodium bicarbonate and sodium borohydride with methylene blue indicator
anaerobic bacteria - mediums
cook meat
thioglycolate broth
stuart’s amies with inert gas
symptoms of anaerobic bacteria infection
foul-smelling discharge from short-chain fatty acid
infection near mucosal surface
gas in tissues
polymicrobial
Peptococcus - normal flora
skin, oral cavity, respi, GI, female genitourinary
Peptococcus - diseases
deep skin and soft tissue infection: necrotizing fasciitis
brain abscess
Peptococcus - treatment
penicillin, carbapenems
Clostridium - common characteristic
endospore
Clostridium - reservoir
soil, water, sewage, GI
Clostridium perfringens - morphology
gram variable
single/pairs boxcar shape
subterminal oval spores
Clostridium perfringens - virulence factors
toxin: alpha and enterotoxin
endospore
Clostridium perfringens - toxin effects
RBC, WBC lysis
increase vascular permeability
decrease bp
*swelling, muscle and tissue death
Clostridium perfringens - endospore invasion
only invades wounded skin
Clostridium perfringens - disease
gas gangrene (necrotizing fasciitis) with *foul-smell, crepitus, myonecrosis leading to shock, kidney failure, death within a week
Clostridium perfringens - diagnosis
litmus milk: stormy clot
target hemolysis
reverse CAMP test: S. agalactiae + C. perfringens = arrowhead
Nagler (Lecithinase) test: precipitating zone
Clostridium perfringens - treatment
debridement
hyperbaric oxygen therapy
Clostridium botulinum - found in
canned food
Clostridium botulinum - virulence factors
endospore
toxin AB
Clostridium botulinum AB toxin
inhibit muscle contraction (cleave SNARE → vesicle can’t fuse) → *flaccid paralysis
Clostridium botulinum - diseases
foodborne botulism
iatrogenic botulism
Clostridium botulinum - diagnosis
ELISA, lateral flow for toxin antigen
Clostridium botulinum - treatment
trivalent antitoxin
heat at more than 80 degrees for 20 minutes to destroy
Clostridium tetani - virulence factors
VAMP (synaptobrevin)
tetanospasmin
tetanolysin
endospore
tetanospasmin
inhibit inhibitory neurotransmitter (GABA)
tetanolysin
hemolysis
Clostridium tetani - disease
tetanus (lock jaw)
tetanus (lock jaw)
*masseter trismus (can’t open mouth) → intermittent spasms of respiratory and swallowing muscles → back contractions (opisthotonos) → respiratory failure
Clostridium tetani - treatment
antitoxin: only for unbound toxin
benzodiazepines
DPT vaccine
Clostridioides difficile - location
intestinal
Clostridioides difficile - virulence factors and effect
toxin A&B (TcdA&B)
hyaluronidase
lead to hemorrhagic death of intestine = *explosive diarrhea
Clostridioides difficile - disease
pseudomembranous colitis
pseudomembranous colitis - pathogenesis
ingestion of spore → bile salt induce germination → colonization → TcdA & B → inflammation and mucosal damage → pseudomembrane → colon wall slough → perforation → toxic megacolon
Clostridioides difficile - diagnosis
NAAT
enzyme immunoassay if have symptoms (toxins, glutamate dehydrogenase)
CCNA
Clostridioides difficile - agar
cycloserine cefoxitin frucose agar: vero cell spindle → round
requires heat shock at 80 degrees for 10 minutes to get rid of others
Clostridioides difficile - treatment
fecal transplant, nontoxigenic C. difficile for competitive exclusion
Cutibacterium acnes - characteristics
produce propionic acid
opportunistic nosocomial
Cutibacterium acnes - normal flora
skin, hair follicle
Cutibacterium acnes - disease
acne
acne - pathogenesis
shed keratin and sebum accumulate in follicle → P. acnes proliferation → inflammation
Cutibacterium acnes - treatment
erythromycin, clindamycin
probiotic bacteria
Bifidobacterium
Lactobacillus
Lactobacillus - normal flora
vagina and intestine
Lactobacillus - disease
dental caries: L. acidophilus
transient bacteremia: after birth, gynecologist
endocarditis
Lactobacillus - treatment
penicillin, aminoglycoside
Actinomyces - gram
gram-positive
Actinomyces - normal flora
oral cavity
Actinomyces - disease
granulomatous
cervicofacial: jaw/oral infections after dental caries
cervicothoracic/thoracoabdominopelvic infections (chronic empyema, fistulas)
Actinomyces infection characteristic
discharge with sulfur granules (yellow clumps)
Actinomyces - treatment
prolonged antibiotics
anaerobic gram-negative bacilli - treatment regimen
resist penicilin and cephalosporin
use: azthreonam, imipenem, ceftrixone
or: beta-lactamase inhibitors: clavulonate, sulbactam
Bacteroides fragilis - aerotolerance
superoxide dismutase
Bacteroides - virulence factors
NOT LPS: no lipid A so not toxic
enzymes: collagenase, fibrinolysin, heparinase, hyaluronidase
B. fragilis toxin (zinc metalloprotease) → *diarrhea
Bacteroides - diseases
appendicitis
endocarditis
intra-abdominal abscess
Bacteroides - agar
brain-heart infusion agar (BHIS): with vitamin K and hemin
bacterioides bile esculin agar (BBE): brown
Bacteroides - treatment
metronidazole
Porphyromonas - diseases
periodontitis
arthritis: cross reaction to joint
breast, axillary, perianal, male genital infections
Prevotella melaninogenica - disease
upper respiratory and oral infections
Prevotella bivia, Prevotella disiens - disease
female genital infections
Prevotella - disease
brain, lung abscess, empyema, pelvic inflammation
Fusobacterium necrophorum - morphology
long rod
Fusobacterium nucleatum - morphology
fusiform
Fusobacterium - disease
fusospirochetosis: combine with Treponema vincentii
Vincent’s angina/Trench mount
Lemierre’s disease (Fusobacterium necrophorum)
Vincent’s angina/Trench mount
acute necrotizing ulcerative gingivitis
Lemierre’s disease
septic emboli after infections of head and neck
Gardnerella - gram
gram variable
Gardnerella - virulence factors
surface hydrophobicity: attachment
metalloprotease: digestive enzyme
vaginolysin
Gardnerella - disease
bacterial vaginosis
bacterial vaginosis - criteria
Amsel criteria
clue cells (vaginal epithelium covered with many gram variable bacilli) >20%
thin mucus discharge pH > 4.5
fish odor when + 10% KOH → whiff test
bacterial vaginosis - caused by
decreased lactobacilli, trichomonad, yeast
Gardnerella - treatment
metronidazole