Oxygenation - ABGs, ARDS, mechanical ventilation
1/46
Earn XP
Description and Tags
Test 2 - sem 3
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
47 Terms
What is ARDs
Acute respiratory distress syndrome
Sever inflammation process causing alveolar damage
Sudden pulmonary edema (fluid in the lungs)
Hypoxia, where oxygen supplements do NOT help!
Mortality rate = 36-44%
Mild → death
Muti-system damage/failure
Alveolar collapse
Atelectasis
No breath sounds
Is ARDS a controlled inflammatory response?
No
It is either direct or indirect
The result is respiratory failure and refractory hypoxia
Requires immediate medical interventions
There are three specific stages: exudative, proliferative, and fibrotic phase
Direct causes of ARDs
Aspiration
Chest trauma
PNA
Inhalation injury
Pulmonary embolus (PE)
Indirect causes of ARDs
SEPSIS
Shock
Pancreatitis
Burns
Mass blood transfusions
Cardiopulmonary bypass
Drug/alcohol overdose
Phase 1 of ARDs
Exudative in 72 hours of exposure/onset of the causative agent
Clinically you will see someone who can’t breath and additional O2 support does not improve their saturations
Respiratory distress
Air hungry
Protein is lost that helps keep fluid in cells → 3rd spacing
Phase 2 of ARDs
Proliferate in the repair process
1-3 weeks
Individualized and weaning off vent or transitioning to oxygen therapy
Frequent monitoring
Decreased blood pressure and cardiac output
Severe V/Q mismatch result in severe tissue hypoxia and lactic acidosis
After 2-3 weeks the damage is permeant
Phase 3 of ARDs
Fibrotic scarring causes impaired gas exchange
Pulmonary hypertension worsens
Positioning patient is a type of therapy (turning/positioning Q2H, repositioning of ET tube to prevent mouth ulcers)
Prone positions helps lung expansion, require planned teamwork
Even getting O2 on a patient with ARDs…
this doesn’t help patient and they will continue to get worse
Clinical manifestations
Patient experience one of the causative factors →
SEVERE DYSPNEA WITH RAPID ONSET (less than 7 days) →
SUPPLEMENTAL O2 INCREASES FO NOT IMRPOVE BREATHING →
Hypoxia, tachypnea, tachycardia (compensation) →
Bilateral infiltration of CXR
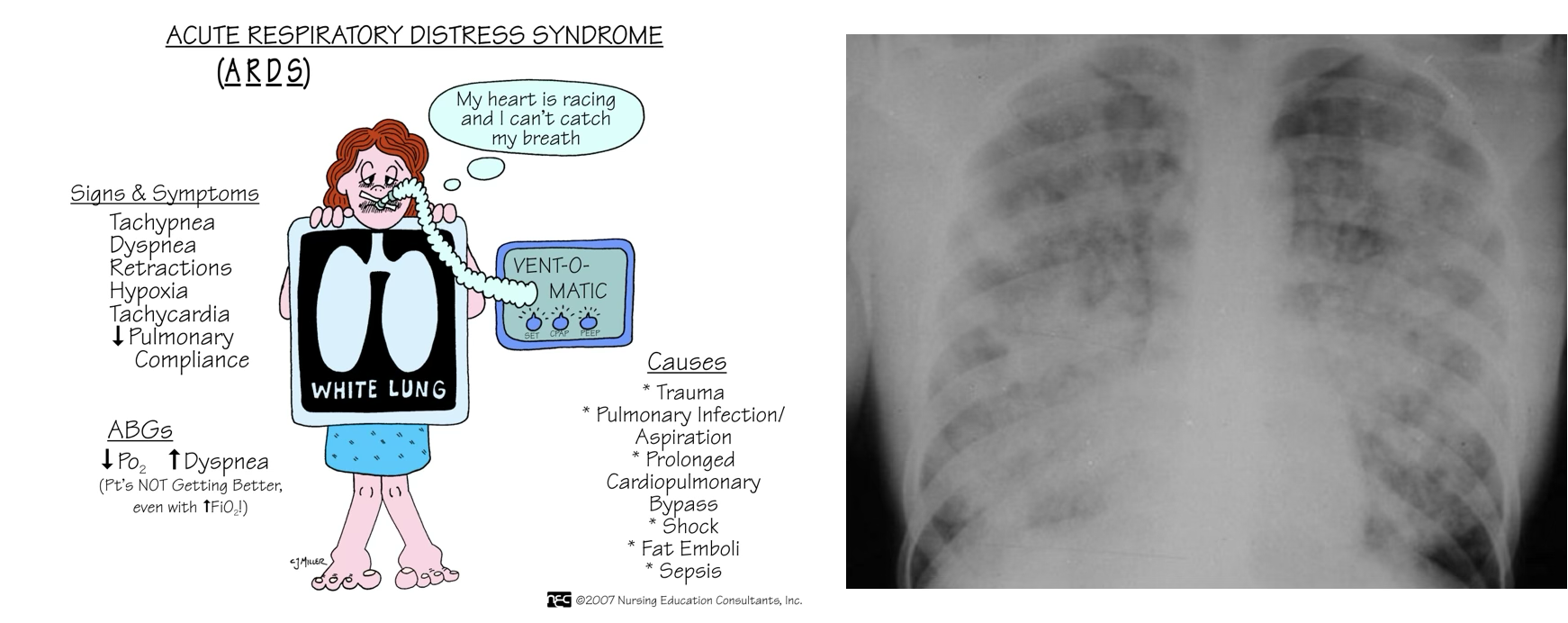
Diagnostic testing for ARDs
Intercostal retractions, crackles
BNP levels
Echo
ABG’s, CBC
Chest x-ray
Pulmonary artery catheterization
Transthoracic echocardiography (TTE)
Goal of ARD therapy
Identification and treatment of underlying condition
Aggressive, supportive care
Endotracheal intubation
Mechanical ventilation: peep support
Circulatory support
Appropriate fluid volume
Nutritional support
PaO2 >60mmhg, or O2 stat >90%
Get consult, HOB up, suction, steroids, antibiotics
ARDs nursing care/treatment
Close ICU monitoring: frequent oxygen saturation assessments, no improvement with supplemental O2 application
Frequent assessment: worsening lung sounds; rales/rhonchi present-intubation
Management of underlying cause
Anticipate and prepare for intubation
Nursing diagnosis
Impaired gas exchange
Anxiety
Imbalance nutrition, less than body requirements
Potential skin breakdown
What is PEEP
Positive End Expiratory Pressure
How to provide PEEP
PEEP at the end of each breathe to ensure alveoli does not collapse
Routes:
CPAP
BiPAP
Mechanical Ventilation
Vent modes
Synchronized Intermittent Mandatory Ventilation (SIMV)
Assist Control (AC) mode
*The use of PEEP helps increase functional residual capacity and reverse alveolar collapse by keeping the alveoli open, resulting in improved arterial oxygenation and reduction in the severity of the ventilation-perfusion imbalance
*After 2 weeks - the talk of tube coming out and trac going in
RN role during intubation
Know your patient directives
Anticipate the need for intubation
Know where the emergency equipment is located and the process for emergency situations
Ensure patient receives all the care you have available to provide (current orders and scope of practice)
Talk to your patient, tell them what is going on, why it’s happening, what we are doing to “fix” it, and that you’ve got their back
Ensure that they providers and the respiratory therapist know the changing patients status and have the supples they need
Nursing care on intubation
Close ICU monitoring
Oxygen administration
Nebulizer therapy
Proper positioning
Frequent turing
Oxygen monitoring
Pain management
Hemodynamic monitoring
Medications
Paralytic (so they don’t move)
General anesthetic
Antipyretics
Antibiotics
Diuretic
Ventilatory management
Control patient anxiety - “fighting” the vent
Potential sedation:
lorazepam (Ativan)
midazolam (Versed)
propofol (Diprivan)
Short-acting barbiturates
Potential paralytics (neuromuscular blocking)
Prone positioning
“Good” lung down
Laying on stomach
Un-prone when they stop responding well
Can still do everything like normal
Face to the side
Nutrition
35-45 kcal/kg/day to meet caloric requirements
TPN and lipids/external feeding
Tube feeding is preferred due to gut being the best absorption, but if it isn’t working then we go through the central/PICC line
ARDs phonetic
Atelectasis
Refractory hypoxemia
Decrease lung compliance
Surfactant decreased
Normal pH level
7.35-7.45
Acidosis
>7.35
Alkalosis
<7.45
PaCO2
35-45
Lungs
HCO3
22-26
Kidneys
Respiratory buffers
Takes minutes-hours to kick in
Control H+ levels with CO2
Renal buffers
Takes slower to kick in, but lasts longer
Control H+ levels with HCO3
Hyperventalation
Blowing off CO2
Decreases H+ ions
Hypoventilation
Holding on to CO2
Increase H+ ions
How do kidneys increase H+ ions
Reabsorb HCO3, so hydrogen is excreted
How do kidneys decrease H+ ions
Excreted HCO3, so hydrogen is absorbed
PaCO2 and HCO3 both abnormal…
Respiratory
Opposite
Metabolic
Equivalent/Equal
Fully compensated
The pH has returned to the normal range, but both CO2 and HCO3 are abnormal
The body has successfully corrected the imbalance, though the “fingerprints” of compensation remain
Partially compensated
The pH is still abnormal, but both CO2 and HCO3 are abnormal, showing that the body is trying to fox the problem
The compensatory system (lungs or kidneys) is working, but it hasn’t fully corrected the imbalance yet
Uncompensated
The pH is abnormal and either CO2 or HCO3 is abnormal but the other value is still normal
The body has not yet started to correct the imbalance
What is cystic fibrosis
Autosomal recessive genetic mutation
Get it from parents (1/4 children have it with parents that have it or carry it)
Disruption in the transport of chloride, sodium and water → build up of mucous
Effect the pancreas and lungs
How many people does CF effect
30,000 people in the US
1 in every 3,500 babies (prenatal screening)
What happens in CF
Mucosal surface alteration
Exocrine gland dysfunction
Sweat glands = more chloride → salty sweat and electrolyte imbalance
GI tract
Pancreas = absorption is blocked → malnutrition
Respiratory tract
Males = infertile
Females = hard for sperm to enter due to thick cervical mucous
Water transplant abnormalities
THICK, TENACIOUS SECRETIONS
Nursing assessment for CF
Health history
Salty taste to skin
Abdominal pain
Difficulty passing stool
Poor weight gain despite diet
Chronic cough
Respiratory infection
Fever
Pulmonary meds
Bone pain
Physical examination:
Inspection (barrel chest, clubbing nails)
Auscultation (diminished lung sounds, tachycardia, bowel sounds)
Percussion
Palpation (asymmetrical chest with atelectasis, tender liver)
Labs/diagnostic tests
Increase chloride
Decreased O2 stat
Chest x-ray → hyperinflatration
Pulmonary function test
Bronchial walls thicken
Nursing management for CF
Minimize pulmonary complications
Promote growth and development
Mobilize secretions multiple times a day
Maintain patent airway
brochodilators, antibiotics, CPT, bilateral lung transplant
Prevent infection
Pulmonary hygiene
NO CURE
Respiratory medication management
Bronchodilators
Albuterol, Levalbuterol
Mucolytics
Dornase Alpha, Hypertonic Saline
Antibiotics
Aerosolized Antibiotics
Tobramycin
Dilate → mucolytics → mucous clearance → inhale antibiotics
Maintaining growth
Pancreatic Enzyme Supplements: Pancrealipase
Every time you eat
High fat, high protein diet; ADEK Vitamins
Tube feeds/TPN
Increase calories
Promoting family coping
Daily interventions
Frequent hospitalizations
Surgical management
Relationship strain
Anticipatory grieving