Airway Management Final Set
1/56
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
57 Terms
Rule Number One of Airway Management
Use the least amount of effort necessary
If the Airway is Patent
Leave it alone
If the Airway is Not Patent Consider
→ Reposition
→ Suction
→ Airway adjunct:
Oropharyngeal Airway (OPA)
Nasopharyngeal Airway (NPA)
→ Oxygen (O2)
→ Continuous Positive Airway Pressure (CPAP)
→ Bag Valve Mask (BVM)
→ Supraglottic Airway (SGA) (EMT-B only use this when cardiac arrest occurs)
→ ALS
Make-up of the Upper Airway
→ Anything above the larynx:
Nasopharynx
Oropharynx
Epiglottis
Laryngopharynx / Hypopharynx
Make-up of the Lower Airway
→ Anything below the larynx
Trachea
Bronchi
Lungs
Lobes of Left and Right Lungs
Right Lung (3 lobes)
Left Lung (2 lobes
Why can Pediatric Airways be Challenging
Smaller airway
Larger tongue relative to mouth
Structures are closer together (increasing risk of obstruction)
What is Ventilation (Respiration Process)
Mechanical process where the diaphragm contracts (moves downward) creating negative pressure so air moves into the lungs and relaxes (moves upward) pushing air out of the lungs
Diaphragm DOWN → air IN (inhale)
Diaphragm UP → air OUT (exhale)
What Drives Respiration
Carbon Dioxide (CO2) and PH drive respiration:
↑ CO₂ → ↓ pH (acidosis) → ↑ respiratory drive (hyperventilate)
↓ CO₂ → ↑ pH (alkalosis) → ↓ respiratory drive (hypoventilation)
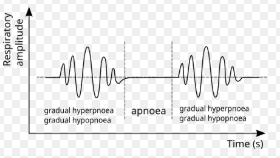
Cheyne Stokes Pattern
Breaths gradually become deeper, then become shallow, and are then followed by periods of apnea that repeat in this cycle
Cause: Brain injury (inter cranial pressure (ICP)) or neurological dysfunction
Shallow → deeper → deepest → shallower → pause → repeat
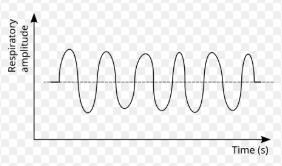
Kussmaul Pattern
Breaths are constant, deep, and fast with no pauses. The body is trying to blow off excess CO2
Cause: Metabolic acidosis
Fast + deep → fast + deep → fast + deep (no pause)
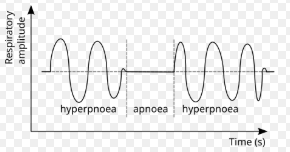
Biot’s Pattern
Irregular breathing pattern with clusters of breaths followed by periods of apnea (pause)
Cause: Injury to the medulla oblongata (brain stem)
Breathe → breathe → breathe → pause → breathe → breath → breath → pause (repeat)
Ataxic Pattern
Irregular breathing pattern with unpredictable rate, rhythm, and depth
Cause: Severe injury to the medulla oblongata (brain stem)

Abnormal Respirations Patterns
Cheyne-Stokes → brain injury
Kussmaul → metabolic acidosis (DKA)
Biot’s → Damage to medulla oblongata
Ataxic → Severe brain injury
What are Peripheral Tissues
Includes:
Muscles
Organs
Brain
Skin
All body Cells
Everything beside the lungs
Gas Exchange in Peripheral Tissues
Oxygen is delivered and carbon dioxide is picked up and removed as waste
Oxygen leaves the blood → enters the cell
Carbon dioxide leaves the cell → enters the blood
Gas exchange in lungs
Blood ↔ cells
Gas Exchange in the Lungs
Gas exchange occurs in the alveoli where oxygen moves from the air into the blood stream and carbon dioxide moves from the blood into the air
Lungs: air ↔ blood
Obstructions
Anything that interferes with ventilation or gas exchange
Types:
1.) Mechanical
2.) Disease-related
3.) Peripheral disease
Mechanical Obstructions
Physical problems preventing air from moving and out of the lungs (airflow)
→ Example: Chest wall injury, airway swelling, foreign body obstruction (choking)
Disease-related Obstructions
Lung conditions that impair gas exchange in alveoli
→ Examples: COPD, asthma, bronchitis, or pneumonia
Peripheral Disease Obstructions
Blood-flow issues that prevent oxygen from reaching body tissues
→ Example: Shock or hypoperfusion
Hypoxia (Mild and Severe)
Oxygen is not reaching the cell
→ Mild (patient is compensating)
Tachypnea
Dyspnea
Restlessness / anxiety
Agitation
Pale, cool, clammy skin
Accessory muscle use
*Mental status change is an early red flag
*Mild = restless and working
→ Severe (patient is decompensating)
Severe dyspnea
Tachypnea (worsening)
Cyanosis
Pale, cool, diaphoretic skin
LOC
Cardiac arrest
Respiratory arrest
*Cyanosis = late and dangerous
*Severe = blue, tired, and crashing
Airway Assessment - Airway
Look in the airway: physical obstruction (blood, vomit, teeth)
Listen to the airway: snoring, gurgling, stridor
Open the airway: Manual maneuvers
Airway Assessment - Breathing
Rate: ideal is 12 - 20 adult / 10 - 40 child
Rhythm: regular vs. irregular patterns
Quality: normal depth, non-labored, clear lung sounds
Conditions of Adequate Breathing
1.) Adequate respiratory rate
2.) Adequate tidal volume (depth)
Tidal Volume
Amount of air moved that is taken with each breath
Decision to Ventilate or Not Ventilate
Bad rate or bad depth = ventilate with BVM
“Under 8 then ventilate”
BVM Ventilation Rates (Adult w advanced airway and w/out)
Adult with no advance airway: 1 breath every 5-6 sec
Adult with ET tube/ i-gel: 1 breath every 6 secs
Complications of BVM
Drop in cardiac output → drops blood pressure (hypotension)
Gastric distention → increased risk of aspiration
Normal vs. Positive Airway Ventilations
In normal breathing and natural ventilations the diaphragm creates negative pressure in the thoracic cavity.
Positive airway ventilation involves using an external source (BVM) to create positive pressure that pushes oxygen into the lungs and forces them to expand and contract
Normal (negative pressure) = pull
Positive pressure = push
Head tilt / chin-lift (how and when we use it)
We tilt the head back and lift the chin forward which moves the tongue away from the back of the throat
We use this in patients with NO trauma
DO NOT USE IN TRAUMA PATIENTS
Jaw Thrust (how and when we use it)
Keeping the head and neck neutral (no movement) place your hands on the side of the patients mandible and push the jaw forward to open the airway
We use this in patients with trauma
Recovery Position (how and when we use it)
Lay the patient on their side to maintain a patent airway and let fluids drain
We use this when the patient is unconscious and breathing on their own and voting or secretions are present
Breathing but out = on their side
Assisted Ventilations on a Conscious Patient
Explain the procedure and synchronize bagging with the patient’s inhalations while providing adequate tidal volume
Assisting Ventilations on a Unconscious Patient
For an unconscious or apneic patient, open the airway, apply a mask, and ventilate with a BVM at one breath every 5 seconds with adequate chest rise
Flow Rate of a Non-rebreather
15 liter per minute (LPM)Nasal
Flow Rate of a Nasal Cannula
2 to 6 liters per minute (LPM)
Flow Rate of Bag Valve Mask (BVM)
Up to 25 liters per minute (LPM)
Flow Rate of Continuous Positive Airway Pressure (CPAP)
The flow rate is device-driven
Flow Rate of a Blow-by
15 liter per minute (LPM)
Trick About Remembering Oxygen Tank Sizes
The tank gets bigger as you progress through the alphabet
Oxygen Tank Sizes
D → Smallest
E → Standard and Portable (anchor)
M → Ambulance-sized
G / H / K → Very large
*All oxygen tanks are full at 2,000 PSI
Rules of Suctioning
Eye Protection
Only what we see
Max 15 seconds
Equipment Needed for Suctioning
Sterile water
Suction unit
Catheter
Yankauer (rigid)
French (flexible)
Yankauer Catheter (when its used and sizing)
Use: A rigid catheter used to suction the mouth and upper airway
Sizing: Comes in two sizes adult and pedi
French Catheter (when its used and sizing)
Use: used for suctioning in the nose or if a patient has a tracheostomy (can only suction at a length about 2/3rds of your pinky)
Sizing: Sized in French use an approbate size for the patient and their airway
Snoring (indication, common cause, and intervention)
Indicates a partial upper airway obstruction
Common cause: Tongue
Intervention: Reposition and if that does not work OPA (no gag reflex) or NPA (gag reflex)
Snoring = tongue problem → reposition
Gurgling (indication, common cause, and intervention)
Indicates fluid in the airway
Common cause: Blood, vomit, secretions
Interventions: suction and then reassess the airway
Gurgling = fluid → suction
Stridor (indication, common cause, and interventions)
High-pitched and hard sound heard on inhalation indicating narrowing or obstruction of the upper airway
Common causes: Anaphylaxis or infection (croup, epiglottis)
Oropharyngeal Airway (OPA) (Indications, contraindications, and sizing)
Indications: Patient is unconscious with has no gag reflex AND needs help waiting a patent airway
Contraindications: Patient has a gag reflex, patient is conscious
Sizing: from the corner of the mouth to the ear lobe How to
How do You Place an OPA
Size it correctly by measuring from the corner of the mouth to the ear lobe, then insert it upside down into the mouth until the soft palate meets the hard palette, and rotate it 180 degrees
Nasopharyngeal Airway (NPA) (Indications, contraindications, and sizing)
Indications: Patient is consciousness or unconsciousness with a gag reflex
Contraindications: Patient has facial trauma
Sizing: Measure from the tip of the nose to the side of the mouth
How Do You Place a NPA
Size it correctly, lubricate it, and gently insert it into the nostril with the bevel facing the septum, then advance until the flange rests at the nostril
Continuous Positive Airway Pressure (CPAP)
Delivers constant air pressure through a tight fitted mask keeps the alveoli open between breaths allowing oxygen to flow in more easily and preventing collapse
It essentially holds the alveoli open and reduces the work needed to breath adequately
CPAP (Indications and contraindications)
Indications: Patient is an adult who is alert, breathing on their own. They have a systolic BP equal to or greater than 120, a respiratory rate less than 24, and O2 Sat at or above 94%, and is in respiratory distress
CPAP is for alert, self-breathing patients with good BP and failing O2
Contraindications: CRASH
C - Conscious altered (AMS)
R - Ruptured lung (suspected pneumothorax)
A - Airway not protected
S - Soft tissue facial trauma
H - Hypotension
If they CRASH, NO CPAP
Advanced Airways - (I-gel / supraglottic airway)
EMT-Bs may place advanced airways ONLY in unconsciousness, pulseless cardiac-arrest patients
If a Patient has Trauma to the Nose and Mouth What Do We Place
An OPA may be used in an unconsciousness patient without a gag reflex even when facial trauma is present. We are not ignoring the trauma but airway patency takes priority