1.4 Neonatal CPR
1/47
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
48 Terms
Neonatal CPR
10% of neonates require assistance.
1% necessitating extensive measures.
The initial hospitalization of a newborn is a critical period.
The moment of birth plays a pivotal role.
The current neonatal mortality rate is 4 per 1000 births.
Before birth, ask the obstetrician 4 questions:
Is it full-term?
How is the amniotic fluid?
Are there any additional risk factors?
What is the plan for the umbilical cord?
If a complicated birth is not anticipated …
there should be at least one person capable of providing neonatal CPR.
If there is any risk …
there should be at least two individuals trained in neonatal CPR.
Risk factors before birth:
Gestational age less than 36 weeks or more than 41 weeks.
Preeclampsia, eclampsia, or maternal hypertension.
Gestational diabetes.
Multiple gestation.
Fetal anemia.
Oligohydramnios or polyhydramnios.
Fetal macrosomia or intrauterine growth restriction.
Significant fetal malformations.
Risk factors during birth:
Emergency delivery.
Abnormal cardiotocographic recording.
Intrapartum bleeding.
Amniotic fluid with meconium.
Umbilical cord prolapse.
Shoulder dystocia.
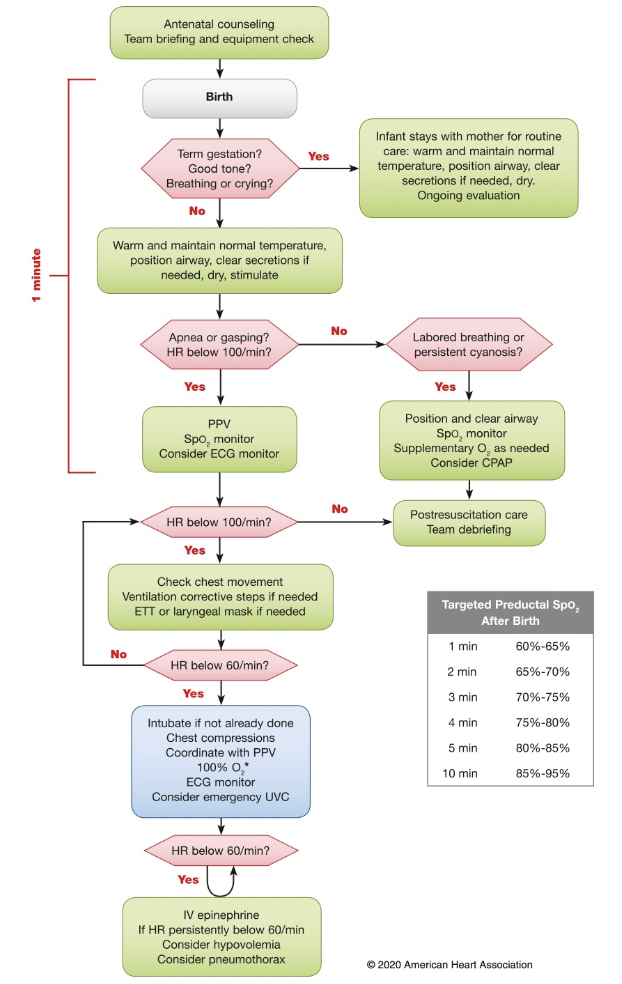
After birth, the following three questions should be asked:
Is the newborn full-term?
Is the newborn crying or breathing?
Does the newborn have good muscle tone?
If the answer is yes to all the questions:
The newborn stays skin-to-skin with the mother and is attended to on the mother's chest.
The baby is dried, stimulated, the airway is positioned, and the baby is covered with a blanket.
If the answer is no:
Any of the following actions will be performed within the first 60 seconds, also known as the 'golden minute':
Initial steps (warmth, drying, stimulation, positioning, suctioning)
Ventilation
Chest compressions
Epinephrine and/or plasma expanders
Assessment within the first minute includes:
Breathing
Heart rate
Once positive pressure ventilation is initiated, the following should be assessed:
Heart rate (a 3-lead EKG can be used)
Breathing
Oxygenation status
The most sensitive indicator of a successful response is …
elevation of the heart rate
Neonatal resucitation algorithm
Management of the Umbilical Cord
Delayed umbilical cord clamping for 30 to 60 seconds.
This practice is applied to both term and stable preterm newborns.
After birth, the baby is kept skin-to-skin, and vital signs are monitored.
Umbilical cord clamping benefits:
Reduced intraventricular hemorrhage
Improved blood pressure and blood volume
Lower need for transfusions
Decreased incidence of necrotizing enterocolitis
Initial steps
These should be performed in approximately 30 seconds:
Provide warmth: use a radiant warmer to maintain the newborn's body temperature.
Dry: gently dry the baby to prevent heat loss.
Tactile Stimulation: promote responsiveness and initiate breathing.
Airway Positioning: positioning the baby's head in a neutral position.
Clear Airway Secretions (if necessary)
After performing the initial steps, monitor:
• Breathing
• MuscleTone
• Activity of the newborn
• Coloration
• Temperature
The newborn's temperature should be maintained between:
36°C to 37.5°C.
Skin-to-Skin Contact: encourage placing the baby skin-to- skin with the mother, which helps regulate the baby's temperature.
Very Low Birth Weight Newborn (<1500g):
These infants are at higher risk of hypothermia.
Preheat the room to 26°C and use plastic covers, radiant warmers
Other techniques such as preheating surfaces and skin-to- skin contact.
Airway suctioning: clear amniotic fluid
Suctioning should be approached cautiously, as it can potentially lead to bradycardia.
In infants who are intubated suctioning can reduce compliance, oxygenation, and cerebral blood flow.
Aspiration should only be performed …
in babies with a clear airway obstruction or those requiring positive pressure ventilation (PPV).
Airway suctioning: meconium in amniotic fluid
Aspiration during birth can lead to Meconium Aspiration Syndrome (MAS).
The practice of intubation and aspiration with laryngoscopy has not shown a decrease in the incidence of MAS or mortality.
The current recommendation is to no longer intubate and aspirate meconium in newborns who are depressed.
Do we need oxygen?
The assessment of the baby's coloration is subjective.
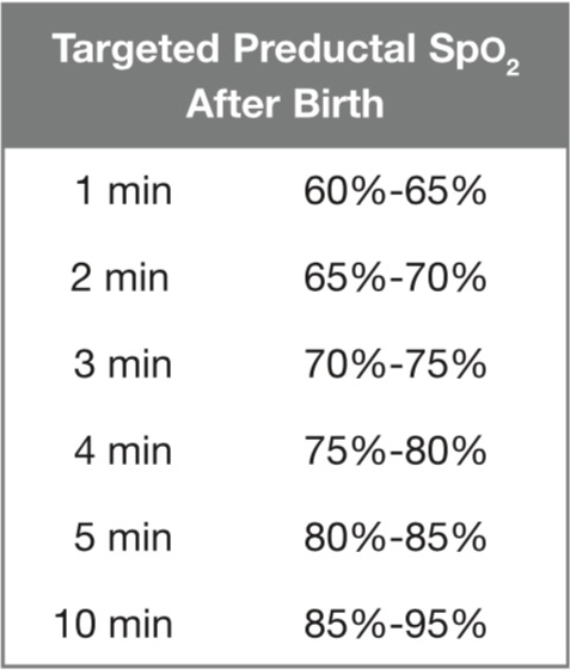
Oxygenation levels do not stabilize until after10 minutes (85 to 95%).
Excess oxygen is harmful.
Pulse oximeter in the obstetric room.
Tables with normal postpartum values.
Reliable reading in 1 to 2 minutes.
Preductal oxygenation.
Oxygen Saturation (SpO2) after birth
For newborns over 32 weeks, resuscitation begins with …
FiO2 21%
For those under 28 weeks, resuscitation begins with …
FiO2 30%
For preterm infants between 28 and 31 weeks, resuscitation starts with …
FiO2 21 to 30%.
If the heart rate is <60 for >90 seconds …
FiO2 100% will be given.
Positive Pressure Ventilation (PPV)
The goal is to increase the heart rate
Most babies will initiate spontaneous breathing within 30 to 60 seconds, especially during tactile stimulation.
Do not delay the initiation of Positive Pressure Ventilation (PPV) for more than 60 seconds.
PPV indications
Poor respiratory effort or apnea
Heart rate < 100 per minute
Target respiratory rate: 40 to 60.
When initiating PPV, a pulse oximeter should be placed on the right hand.
If there is no improvement in heart rate within the first 15 seconds of PPV …
evaluate chest movement.
If there is no chest movement …
Apply corrective steps:
Mask adjustment or repositioning
Reposition the airway
Suction secretions from the mouth and nose
Open the airway
Pressure: Increase ventilation pressure
Alternate: Consider attempting a laryngeal mask or endotracheal tube.
Positive End-Expiratory Pressure (PEEP)
Experts recommend CPAP in newborns with good effort but respiratory distress.
Advantages include a decrease in broncho pulmonary dysplasia, intubation needs, neonatal death, and surfactant use.
PEEP is beneficial and should be provided if the appropriate equipment is available.
It should not be provided with a self-inflating bag.
Assisted Ventilation
Effective ventilation can be provided with self-inflating bags with an escape valve.
The valve depends on the air flow.
Laryngeal masks
Effective in neonates weighing > 2000g.
Limited information is available for those weighing < 2000 g or born before 34 weeks of gestation.
When ventilation is not successful or when intubation is not possible.
Their use has not been evaluated in the presence of meconium or for medication administration.
Endotracheal Tube(ETT):
Used when bag ventilation is inefficient or prolonged.
Before initiating chest compressions.
Special situations: diaphragmatic hernia.
An increase in heart rate is the best indicator of proper ETT placement.
Capnography is the best method for confirmation.
Chest compression indications:
Heart rate <60 beats per minute despite good ventilation for 30 seconds.
Reassess heart rate, oxygenation, and breathing every 60 seconds.
Avoid frequent interruptions.
Suspend compressions if heart rate is >60per minute.
Before initiating compressions, ensure:
Previous steps are appropriate.
An airway device is in place.
Electrodes are placed to monitor heart rhythm.
FiO2 is set to 100%.
Compression-to-ventilation ratio:
3:1 (90 compressions and 30 ventilations)
Compressions 15:2 or 30:2 are more effective in …
cardiac origins.
Medication indications:
Medications are rarely used in term newborns.
Bradycardia is a result of poor oxygenation.
If heart rate is < 60 despite 30 seconds of ventilation achieving chest rise and 60 seconds of cardiac compressions with FiO2 100%.
Administer positive pressure ventilation (PPV) via endotracheal tube or laryngeal mask.
IV Epinephrine
Preferred
It can also be given intraosseously (IO).
Dose: 0.02mg/kg/dose
Range: 0.01 to 0.03 mg/kg/dose
Followed by a 3 mL saline flush.
Epinephrine vía endotracheal tube
Dose: 0.1 mg/kg/dose
Range: 0.05 to 0.1 mg/kg/dose
Unreliable absorption.
Less effective than IV or IO route.
Volume Expanders
When there is suspicion of blood loss and there is no good response to resuscitation
Pale skin, poor perfusion, weak pulses
Solutions: crystalloids or blood: 10mL/kg
Caution in preterm infants due to an increased incidence of intraventricular hemorrhage (IVH).
Post-Resuscitation Care
Evaluate vital signs, glucose, electrolytes, urine, neurological status.
Avoid overheating the baby.
Naloxone
Not recommended for use in the obstetric room.
Induced hypothermia
Hypothermia (33.5°C to 34.5°C) in neonates >36 weeks gestation with moderate to severe hypoxic- ischemic encephalopathy (HIE):
Reduces mortality and neurodevelopmental impairment at 18 months.
Whole-body (systemic) and head cooling.
Initiate within the first 6 hours of life and continue for 72 hours.
Gradual rewarming over 4 hours.
When not to initiate CPR?
Gestation, birthweight, or congenital anomalies associated with early death and/or high morbidity:
<23 weeks gestational age and/or weight <400g
Anencephaly
Trisomy13
If survival is high with acceptable morbidities, resuscitation will be initiated.
If the prognosis and/or survival are unknown, the wishes of the parents will be taken into account.
When to stop CPR?
If after 20 minutes, no detectable heart rate is present, and all resuscitation steps have been performed, it is appropriate to consider discontinuing resuscitation.
The decision to continue is based on etiology, gestational age, complications, the potential for hypothermia use, and the parents' wishes.