anatomy final
0.0(0)
Card Sorting
1/116
Earn XP
Description and Tags
Last updated 5:11 PM on 12/5/22
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
117 Terms
1
New cards
excitation contraction coupling
Action potential reaches a triad (T tubule and
terminal cisternae of the sarcoplasmic reticulum). First step in excitation-contraction coupling is the
release of Ca2+ from the SR.Triggering contraction if: The myosin heads are in the high energy (primed)
position – ATP energy used to get myosin head in this position.
terminal cisternae of the sarcoplasmic reticulum). First step in excitation-contraction coupling is the
release of Ca2+ from the SR.Triggering contraction if: The myosin heads are in the high energy (primed)
position – ATP energy used to get myosin head in this position.
2
New cards
Contraction Cycle: step 1
Begins with arrival of Ca2+ to the zone of overlap in
the sarcomere (Ca2+ released from SR – why?)
the sarcomere (Ca2+ released from SR – why?)
3
New cards
Contraction Cycle: step 2
• Ca2+ binds to troponin
• Troponin shifts position of tropomyosin
• Exposes active sites (myosin binding sites) on F-actin strands
• Troponin shifts position of tropomyosin
• Exposes active sites (myosin binding sites) on F-actin strands
4
New cards
Contraction Cycle: step 3
Myosin heads (with ADP + Pi bound on it) bind to
exposed active sites on F-actin strands
• Forms cross-bridges
exposed active sites on F-actin strands
• Forms cross-bridges
5
New cards
Contraction Cycle: step 4
• Myosin head pivots, pulling F-actin strand along with
it (moving the F-actin strand closer to M line).
• Pivoting action known as the power stroke
• Power stroke causes ADP and Pi bound on myosin
head to be released (ATPase site on the myosin head is now empty)
it (moving the F-actin strand closer to M line).
• Pivoting action known as the power stroke
• Power stroke causes ADP and Pi bound on myosin
head to be released (ATPase site on the myosin head is now empty)
6
New cards
Contraction Cycle: step 5
ATP molecule binds onto myosin head
• Causes myosin head to detach from active site on
F-actin strand
• Causes myosin head to detach from active site on
F-actin strand
7
New cards
Contraction Cycle: step 6
Myosin head hydrolyze ATP to ADP and Pi
• Myosin head primed back to the high energy position (by using the energy released by ATP hydrolysis)
• If the myosin binding site on the adjacent F-actin is
still unblocked, myosin can bind onto it to continue
the contraction cycle
• Myosin head primed back to the high energy position (by using the energy released by ATP hydrolysis)
• If the myosin binding site on the adjacent F-actin is
still unblocked, myosin can bind onto it to continue
the contraction cycle
8
New cards
Rigor mortis
A fixed muscular contraction after
death (usually 2-7 hrs after death)
• Caused when:
• Ion pumps cease to function; ran out of ATP
• Calcium builds up in the sarcoplasm (Ca2+ leaks out
of SR)
• 1-6 days after death, rigor mortis ends bc muscle sarcomeres and proteins become damaged
death (usually 2-7 hrs after death)
• Caused when:
• Ion pumps cease to function; ran out of ATP
• Calcium builds up in the sarcoplasm (Ca2+ leaks out
of SR)
• 1-6 days after death, rigor mortis ends bc muscle sarcomeres and proteins become damaged
9
New cards
Muscle contraction: step 1
ACh is released at the neuromuscular junction and binds to. ACh receptors on the sarcolemma
10
New cards
Muscle contraction: step 2
An action potential is generated and spreads across the membrane surface of the muscle fiber and along the T tubules.
11
New cards
Muscle contraction: step 3
The sarcoplasmic reticulum releases stored calcium ions.
12
New cards
Muscle contraction: step 4
Calcium ions bind to troponin, exposing the active sites on the thin filaments. Cross-bridges form when myosin heads bind to those active sites.
13
New cards
Muscle contraction: step 5
The contraction cycle begins as repeated cycles of cross-bridge binding, pivoting, and detachment occur—all powered by ATP.
14
New cards
Muscle contraction: step 6
ACh is broken down by acetylcholinesterase (AChE),
ending action potential generation
ending action potential generation
15
New cards
Muscle contraction: step 7
Sarcoplasmic reticulum reabsorbs Ca2+. As the calcium ions are reabsorbed, their concentration in the cytosol decreases.
16
New cards
Muscle contraction: step 8
Without calcium ions, the tropomyosin returns to its normal position and the active sites are covered again.
17
New cards
Muscle contraction: step 9
Without cross-bridge formation, contraction ends.
18
New cards
Muscle contraction: step 10
The muscle returns passively to its resting length.
19
New cards
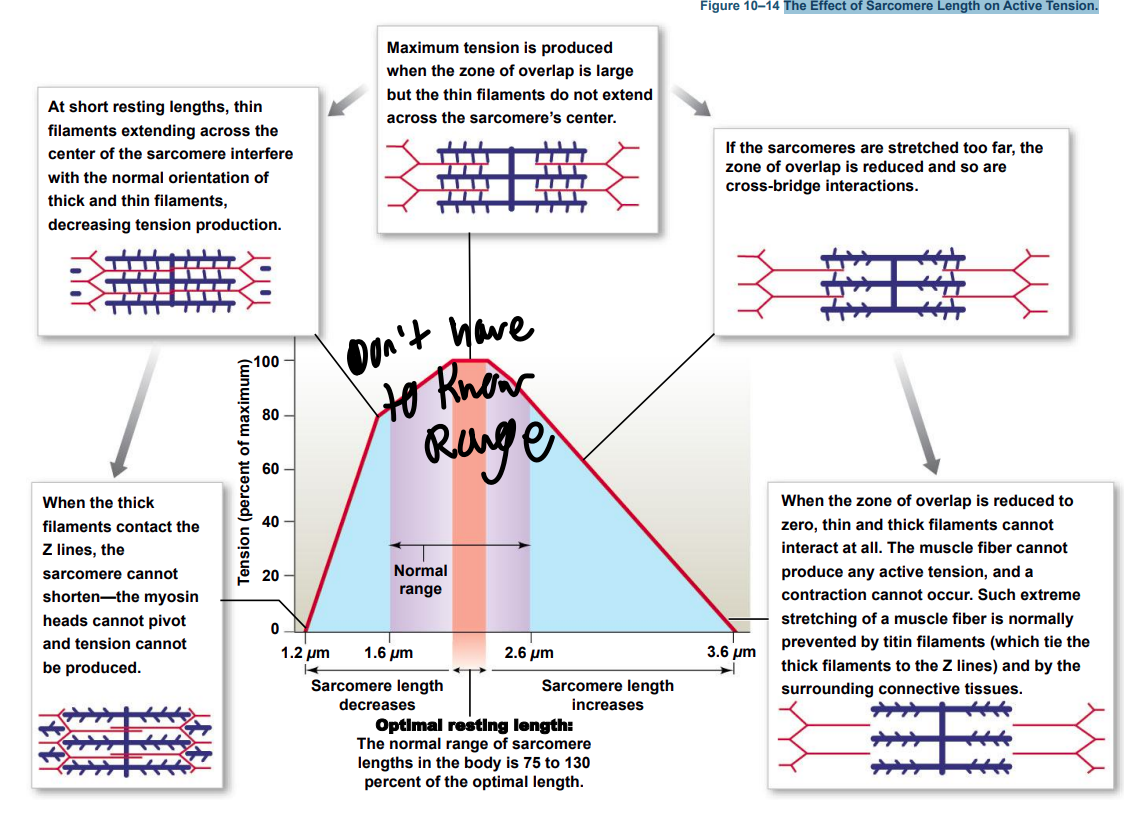
The Effect of Sarcomere Length on Active Tension.
20
New cards
Tension Production by Muscle Fibers: Latent period
– between muscle stimulation and
contraction phase
• The action potential moves through sarcolemma
• Causing Ca2+ release from?
contraction phase
• The action potential moves through sarcolemma
• Causing Ca2+ release from?
21
New cards
Tension Production by Muscle Fibers: contraction phase
Calcium ions bind to?
• Tension builds to peak as actin interacts with myosin
• Tension builds to peak as actin interacts with myosin
22
New cards
Tension Production by Muscle Fibers: relaxation fibers
Ca2+ levels fall – why?
• Active sites are covered and tension falls to resting
levels
• Active sites are covered and tension falls to resting
levels
23
New cards
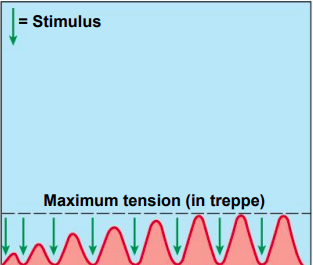
Treppe
A stair-step increase in twitch tension
• Repeated stimulations immediately after relaxation
phase
• Stimulus frequency < 50/second **
• Causes a series of contractions with increasing
tension
• Increase in tension caused by gradual increase in
Ca2+ concentration in the sarcoplasm (Ca2+ pumps not
fast enough to pump all of the previously released
Ca2+ back into the SR).
• Repeated stimulations immediately after relaxation
phase
• Stimulus frequency < 50/second **
• Causes a series of contractions with increasing
tension
• Increase in tension caused by gradual increase in
Ca2+ concentration in the sarcoplasm (Ca2+ pumps not
fast enough to pump all of the previously released
Ca2+ back into the SR).
24
New cards
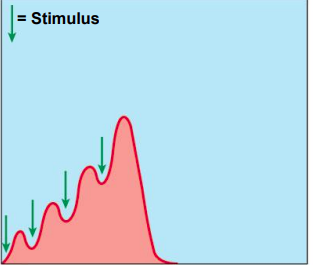
Wave summation
• Increasing tension or summation of twitches
• Repeated stimulations before the end of relaxation
phase
• Stimulus frequency > 50/second **
• Causes increasing tension or summation of
twitches
• Repeated stimulations before the end of relaxation
phase
• Stimulus frequency > 50/second **
• Causes increasing tension or summation of
twitches
25
New cards
Incomplete tetanus
• If rapid stimulation continues and muscle is not
allowed to relax completely, twitches reach maximum
level of tension but does not plateau
allowed to relax completely, twitches reach maximum
level of tension but does not plateau
26
New cards
Complete tetanus
• If stimulation frequency is high enough, muscle never begins to relax and is in continuous contraction
27
New cards
Clostridium tetani
disease tetanus “lockjaw” caused by toxin from bacterium that causes over activity of skeletal muscle motor neurons (by blocking inhibitory interneurons in spinal cord). Results in muscle stiffness, headaches, difficulty swallowing.
28
New cards
internal tension
produced by muscle fibers
29
New cards
external tension
exerted by muscle fibers on elastic extracellular fibers
30
New cards
motor units
Contain hundreds of muscle fibers that contract at
the same time
• These muscle fibers are all controlled by a single
motor neuron
the same time
• These muscle fibers are all controlled by a single
motor neuron
31
New cards
recruitment
In a whole muscle or group of muscles, smooth
motion and increasing tension are produced by
slowly increasing the size or number of motor
units stimulated
motion and increasing tension are produced by
slowly increasing the size or number of motor
units stimulated
32
New cards
muscle tone
The normal tension and firmness of
a muscle at rest
• Muscle units actively maintain body position,
without motion
• Increasing muscle tone increases metabolic energy
used, even at rest
a muscle at rest
• Muscle units actively maintain body position,
without motion
• Increasing muscle tone increases metabolic energy
used, even at rest
33
New cards
Isotonic contraction
Skeletal muscle changes length resulting in motion
• If muscle tension > load (resistance):
• Muscle shortens (concentric contraction)
• If muscle tension < load (resistance):
• Muscle lengthens (eccentric contraction)
• If muscle tension > load (resistance):
• Muscle shortens (concentric contraction)
• If muscle tension < load (resistance):
• Muscle lengthens (eccentric contraction)
34
New cards
isometric contraction
Skeletal muscle develops tension, but is prevented
from changing length. Weight is already on floor and you are trying to lift.
• iso- = same, metric = measure
from changing length. Weight is already on floor and you are trying to lift.
• iso- = same, metric = measure
35
New cards
load and speed of contraction
Are inversely related
• The heavier the load (resistance) on a muscle:
• The longer it takes for shortening to begin
• And the less the muscle will shorten
• The heavier the load (resistance) on a muscle:
• The longer it takes for shortening to begin
• And the less the muscle will shorten
36
New cards
Recovery period
time required after exertion for muscles to return to normal
• Moderate activity can take several hours to
recover; sustained high activity can take up to a
week
• During recovery period: Oxygen becomes available. Mitochondrial activity resumes to replenish ATP stock
• Moderate activity can take several hours to
recover; sustained high activity can take up to a
week
• During recovery period: Oxygen becomes available. Mitochondrial activity resumes to replenish ATP stock
37
New cards
Cori Cycle
movement of lactic acid that was
generated in the muscle cell to the liver and
glucose transported back to muscle cell. Involves the removal and recycling of lactic acid by
the liver
generated in the muscle cell to the liver and
glucose transported back to muscle cell. Involves the removal and recycling of lactic acid by
the liver
38
New cards
Oxygen debt
excessive postexercise oxygen
consumption (EPOC). After exercise or other exertion:
• The body needs more oxygen than usual to
normalize metabolic activities
• Resulting in heavy breathing and deeper breaths
taken after exercise used to restores pre-exertion conditions in:
• Skeletal muscle – restores ATP, CP, and
glycogen
• Liver – converts lactic acid to glucose
consumption (EPOC). After exercise or other exertion:
• The body needs more oxygen than usual to
normalize metabolic activities
• Resulting in heavy breathing and deeper breaths
taken after exercise used to restores pre-exertion conditions in:
• Skeletal muscle – restores ATP, CP, and
glycogen
• Liver – converts lactic acid to glucose
39
New cards
force
The maximum amount of tension produced
40
New cards
Endurance
The amount of time an activity can be sustained
Force and endurance depend on:
• The types of muscle fibers
• Physical conditioning
Force and endurance depend on:
• The types of muscle fibers
• Physical conditioning
41
New cards
Fast Fibers
Contract very quickly
• Have large diameter, large glycogen reserves, few
mitochondria
• Contain low amounts of myoglobin (red pigments
that bind oxygen and act as an oxygen reservoir)
• Have low blood supply
• Have strong contractions but fatigue quickly
because has lots of myofibrils that uses ATP
•most skeletal muscle fibers in the body are
fast fibers
• Have large diameter, large glycogen reserves, few
mitochondria
• Contain low amounts of myoglobin (red pigments
that bind oxygen and act as an oxygen reservoir)
• Have low blood supply
• Have strong contractions but fatigue quickly
because has lots of myofibrils that uses ATP
•most skeletal muscle fibers in the body are
fast fibers
42
New cards
slow fibers
• Are slow to contract, slow to fatigue
• Have small diameter, numerous mitochondria to
support aerobic metabolism
• Have high oxygen supply because of a rich blood
supply (muscle appears dark red)
• Contain high amounts of myoglobin (slow fibers
have most amount of myoglobin compared to
other fiber types)
• Have small diameter, numerous mitochondria to
support aerobic metabolism
• Have high oxygen supply because of a rich blood
supply (muscle appears dark red)
• Contain high amounts of myoglobin (slow fibers
have most amount of myoglobin compared to
other fiber types)
43
New cards
intermediate fibers
• Are mid-sized
• Have low myoglobin
• Have more capillaries than fast fibers, slower to
fatigue
• Appearance (pale in color) more like fast fibers
than slow fibers
• Have low myoglobin
• Have more capillaries than fast fibers, slower to
fatigue
• Appearance (pale in color) more like fast fibers
than slow fibers
44
New cards
intermediate:fast
Athletic training can increase the ratio of intermediate fibers to fast fibers (fast fibers “convert” to intermediate and become more resistant to fatigue)
45
New cards
muscle hypertrophy
Muscle growth from heavy training causes increases in: Diameter of muscle fibers (not number of muscle fibers/cells), Number of myofibrils, Mitochondria, glycogen reserves
46
New cards
muscle atrophy
• Lack of muscle activity. Reduces muscle size, tone, and power. Occurs in paralysis, broken bone (limb immobilized in cast). Reversible at first, but permanent in extreme atrophy
47
New cards
anaerobic exercises
(Ex: 50-meter dash, weightlifting) – supported by only glycolysis and ATP and CP reserves (ATP and CP provides energy for first 10-20 seconds, after that, glycogen breakdown and glycolysis provides additional energy). Use fast fibers. Fatigue quickly (within 2 mins) with strenuous activity. Improved by frequent, brief, intensive workouts. Causes muscle hypertrophy
48
New cards
Aerobic activities
prolonged activity. Supported by mitochondria. Require oxygen and nutrients continuously supplied by bloodstream – athletes “carbo-load” before events to increase glucose supply during event. Improves endurance by training fast fibers to be more like intermediate fibers (Ex: Jogging, distance
swimming). Does not cause muscle hypertrophy. Increases cardiovascular performance
swimming). Does not cause muscle hypertrophy. Increases cardiovascular performance
49
New cards
fibrosis
increase in fibrous connective tissue
occurs
occurs
50
New cards
cardiac muscle cells (cardiocytes)
- Are small, and typically branched at the ends
- The cell length can be up to 100 mm while skeletal muscle cells can be up to 12 inches (304,800 mm)
- Have a single nucleus (skeletal muscle have multiple)
- Have short, wide T tubules (run along Z line of sarcomeres)
- Have SR with no terminal cisternae, thus they lack triads (skeletal muscle have triads)
- Are aerobic (high in myoglobin, mitochondria)
- Have intercalated discs
- The cell length can be up to 100 mm while skeletal muscle cells can be up to 12 inches (304,800 mm)
- Have a single nucleus (skeletal muscle have multiple)
- Have short, wide T tubules (run along Z line of sarcomeres)
- Have SR with no terminal cisternae, thus they lack triads (skeletal muscle have triads)
- Are aerobic (high in myoglobin, mitochondria)
- Have intercalated discs
51
New cards
intercalated discs
Are specialized contact points between cardiocytes. Join cell membranes of adjacent cardiocytes (gap junctions, desmosomes)
Functions of intercalated discs
- Maintain structure, stabilize position of adjacent cells and maintain 3D structure of tissue
- Enhance molecular and electrical connections
Conduct action potentials
- Coordinates cardiocytes, links them mechanically, chemically, and electrically to make heart function as a single, fused mass of cellsin
Functions of intercalated discs
- Maintain structure, stabilize position of adjacent cells and maintain 3D structure of tissue
- Enhance molecular and electrical connections
Conduct action potentials
- Coordinates cardiocytes, links them mechanically, chemically, and electrically to make heart function as a single, fused mass of cellsin
52
New cards
Automaticity
Contraction without neural stimulation. Controlled by pacemaker cells (located at right atrium of heart)
53
New cards
Non-striated
due to different internal organization of actin and myosin. Actin attached to dense bodies which are attached to sarcolemma or intermediate filaments. Different functional characteristics – contraction causes the smooth muscle to shorten and “thicken”
54
New cards
Excitation–Contraction Coupling
- Free Ca2+ in cytoplasm triggers contraction (Ca2+ enter sarcoplasm from extracellular fluid and SR).
- Ca2+ binds with calmodulin (instead of troponin as found in skeletal muscle cells) in the sarcoplasm.
- Activates myosin light chain kinase – enzyme that breaks down ATP, initiates contraction. Activation of myosin light chain kinase required for myosin head to attach to actin
- Ca2+ binds with calmodulin (instead of troponin as found in skeletal muscle cells) in the sarcoplasm.
- Activates myosin light chain kinase – enzyme that breaks down ATP, initiates contraction. Activation of myosin light chain kinase required for myosin head to attach to actin
55
New cards
lengthen-tension relationships
- Thick and thin filaments are scattered (not organized into sarcomeres)
- Resting length not related to tension development
- Functions over a wide range of lengths (plasticity). Contract over a range of lengths four times greater than that of skeletal muscle. Important in areas where size changes dramatically (Ex: Stomach, digestive tract)
- Resting length not related to tension development
- Functions over a wide range of lengths (plasticity). Contract over a range of lengths four times greater than that of skeletal muscle. Important in areas where size changes dramatically (Ex: Stomach, digestive tract)
56
New cards
Length–Tension Relationships
- Thick and thin filaments are scattered (not organized into sarcomeres)
- Resting length not related to tension development
- Functions over a wide range of lengths (plasticity). Contract over a range of lengths four times greater than that of skeletal muscle. Important in areas where size changes dramatically (Ex: Stomach, digestive tract)
- Resting length not related to tension development
- Functions over a wide range of lengths (plasticity). Contract over a range of lengths four times greater than that of skeletal muscle. Important in areas where size changes dramatically (Ex: Stomach, digestive tract)
57
New cards
Multiunit smooth muscle cells
Connected to motor neurons similar to skeletal muscle motor units, but each smooth muscle cell can be connect to multiple motor neurons – Ex: Iris of eye, walls of large arteries, arrector pili
58
New cards
visceral smooth muscles cells
- Not connected to motor neurons
- Muscles arranged in sheets or layers
- Rhythmic cycles of activity controlled by pacesetter cells
- Cells connect to each other by gap junctions to spread contraction – responds to initial motor neuron, chemicals, hormones, etc. – Ex: Digestive/urinary system
- Muscles arranged in sheets or layers
- Rhythmic cycles of activity controlled by pacesetter cells
- Cells connect to each other by gap junctions to spread contraction – responds to initial motor neuron, chemicals, hormones, etc. – Ex: Digestive/urinary system
59
New cards
smooth muscle tone
- Normal level of background activity
- Maintains normal levels of activity (found in multiunit and visceral smooth muscle tissue)
- Modified by neural, hormonal, or chemical factors. Ex: Hypoxia at tissue causes relaxation of smooth muscles regulating capillaries that bring blood to those tissues. When O2 levels restored to normal, smooth muscle regains normal muscle tone and constrict to lower blood flow to that tissue
- Maintains normal levels of activity (found in multiunit and visceral smooth muscle tissue)
- Modified by neural, hormonal, or chemical factors. Ex: Hypoxia at tissue causes relaxation of smooth muscles regulating capillaries that bring blood to those tissues. When O2 levels restored to normal, smooth muscle regains normal muscle tone and constrict to lower blood flow to that tissue
60
New cards
tissue
collection of specialized cells and cell products that perform a specific, limited function
61
New cards
Epithelial tissue
- Covers exposed surfaces (Ex: Skin)
- Lines internal passageways (Ex: Digestive tract)
- Forms glands (Ex: Sweat glands, endocrine glands)
- Lines internal passageways (Ex: Digestive tract)
- Forms glands (Ex: Sweat glands, endocrine glands)
62
New cards
connective tissue
- Fills internal spaces (Ex: Adipose)
- Stores energy (Ex: Adipose)
- Supports other tissues (Ex: Bone)
- Transports materials (Ex: Blood)
- Stores energy (Ex: Adipose)
- Supports other tissues (Ex: Bone)
- Transports materials (Ex: Blood)
63
New cards
epithelia
Layers of cells covering internal or external surfaces
- Internal – lines digestive, respiratory, reproductive, and urinary tracts
- External – surface of the skin (Ex: epidermis)
- Internal – lines digestive, respiratory, reproductive, and urinary tracts
- External – surface of the skin (Ex: epidermis)
64
New cards
functions of epithelial tissue
- Provide Physical Protection
- Control Permeability – can be regulated and modified in response to stimuli (Ex: Hormones can affect transport across epithelia, physical labor forms calluses on skin)
- Provide Sensation
- Produce Specialized Secretions (glandular epithelium)
- Control Permeability – can be regulated and modified in response to stimuli (Ex: Hormones can affect transport across epithelia, physical labor forms calluses on skin)
- Provide Sensation
- Produce Specialized Secretions (glandular epithelium)
65
New cards
Neuroepithelium
epithelium specialized to perform a specific sensory function (Ex: Smell, taste, sight, hearing, equilibrium)
66
New cards
exfoliative cytology
epithelial cells or fluids produced from epithelial lining are removed and checked for abnormal cellular changes (Ex: Pap test, amniocentesis)
67
New cards
characteristics of epithelia
1. Cellularity (are interconnected by cell junctions)
2. Polarity (apical and basal surfaces) – apical = superior, basal = inferior
3. Attachment (base of epithelia are attached to the basement membrane or basal lamina) – basement membrane produced by: basal surface of epithelium
and underlying connective tissue
4. Avascularity (lacks blood vessels)
5. Regeneration (continuously replaced through the division of stem cells
2. Polarity (apical and basal surfaces) – apical = superior, basal = inferior
3. Attachment (base of epithelia are attached to the basement membrane or basal lamina) – basement membrane produced by: basal surface of epithelium
and underlying connective tissue
4. Avascularity (lacks blood vessels)
5. Regeneration (continuously replaced through the division of stem cells
68
New cards
CAM (cell adhesion molecules)
transmembrane proteins that bind large areas of the plasma membrane to other cells or to extracellular materials
69
New cards
cell junctions
specialized areas of membrane that form bonds with other cells or extracellular material.
70
New cards
tight junctions
interlocking membrane proteins connecting the plasma membrane of two cells.
- Prevents passage of water and solutes between the connected cells
- Isolates wastes, acids, and enzymes in the lumen of digestive tract (prevents those items from escaping out of the lumen by seeping between cells)
- Prevents passage of water and solutes between the connected cells
- Isolates wastes, acids, and enzymes in the lumen of digestive tract (prevents those items from escaping out of the lumen by seeping between cells)
71
New cards
gap junctions
holds two cells together by channel proteins (junctional proteins called connexons)
- Allow rapid communication (allows ions to pass from one cell to another)
- Important in coordinating contractions in heart muscle
- Allow rapid communication (allows ions to pass from one cell to another)
- Important in coordinating contractions in heart muscle
72
New cards
desmosomes
very strong, can resist stretching, bending, twisting, compression (Ex: found in epithelial cells of the skin). CAMs (cell adhesion molecules) connect adjacent plasma membranes
73
New cards
spot desmosomes
small discs connected to intermediate filaments of each cell. Tie cells together, stabilizes cells but allows bending and twisting
74
New cards
Hemidesmosomes
“half of a spot desmosome”, attach cells to the basement membrane to anchor it to underlying tissue
75
New cards
special simple squamous epithelium
lines chambers and passageways that do NOT communicate with the outside world.
76
New cards
endothelium
lines inner surface of heart chambers and blood vessels
77
New cards
mesothelium
lines body cavities
Ex: Pleura (lungs), pericardium (heart), peritoneum (abdominopelvic cavity)
Ex: Pleura (lungs), pericardium (heart), peritoneum (abdominopelvic cavity)
78
New cards
endocrine glands
ductless glands. Release hormones (chemical messengers) into the interstitial fluid which then enters into the bloodstream. Ex: Thyroid gland, pituitary gland, etc
79
New cards
exocrine glands
glands with ducts. Produce secretions that are released through ducts onto an epithelial surface. Ex: Sweat from sweat glands, milk from mammary glands, digestive glands
80
New cards
mecocrine secretion
most common mode. Produced in Golgi apparatus. Released by vesicles (exocytosis). Ex: sweat glands, mucins (when mixed with water, mucins form mucus)
81
New cards
apocrine secretion
Produced in Golgi apparatus. Released by shedding of the cytoplasm – apical section of the cell is lost (along with the cytoplasm and inclusions within that section). Ex: mammary glands release milk by a combination of apocrine and merocrine secretions
82
New cards
holocrine secretion
Released by cells bursting, killing the gland cells. Entire cell fills with the secretory products before it bursts. Gland cells replaced by stem cells. Ex: sebaceous glands found at hair follicles
83
New cards
connective tissue proper
functions to connect and protect
Ex: Tendons and adipose tissue
Ex: Tendons and adipose tissue
84
New cards
fluid connective tissue
functions in transportation
Ex: Blood and lymph
Ex: Blood and lymph
85
New cards
supporting connective tissue
provides structural strength
Ex: Cartilage and bone
Ex: Cartilage and bone
86
New cards
fibroblasts
The most abundant cell type in connective tissue. Found in all connective tissue proper. Secrete proteins and hyaluronan (cellular cement)
87
New cards
fibrocytes
The second most abundant cell type – develops from fibroblasts. Found in all connective tissue proper. Maintain the fibers of connective tissue proper
88
New cards
white fat
Most common. Stores fat. Absorbs shocks. Slows heat loss (insulation)
89
New cards
brown fat
more vascularized. Widespread in fetus and infants, only small amounts in adults. Adipocytes have many mitochondria. When stimulated by nervous system, fat breakdown accelerates, releasing energy as heat. Surrounding tissues absorbs heat to quickly warm circulating blood
90
New cards
mesenchymal cells
found in many connective tissue. Stem cells that respond to injury or infection. Differentiate into fibroblasts, macrophages, or other connective tissue cells in response to injury or infection
91
New cards
Embryonic Connective Tissue (Mesenchyme)
The first connective tissue in embryos. Gives rise to all other connective tissues. Are not found in adults (though many adult connective tissues do have mesenchymal stem cells for tissue repair)
92
New cards
lymph
-Extracellular fluid collected from interstitial space (lymph is leftover fluid in tissue that is not reabsorbed back into the capillaries)
-Taken in and transported by lymphatic (lymphoid) system
-Monitored by immune system
-Lymph fluid is ultimately returned to venous system (cardiovascular system) – lymph is dumped back into venous blood (blood carried in veins) and mixes with it-
-Taken in and transported by lymphatic (lymphoid) system
-Monitored by immune system
-Lymph fluid is ultimately returned to venous system (cardiovascular system) – lymph is dumped back into venous blood (blood carried in veins) and mixes with it-
93
New cards
cartilage
- produced by chondrocytes
- Avascular (no blood vessels!)
- Chondrocytes produce antiangiogenesis factor, prevents the formation of new blood vessels, slows down repair since low blood flow = fewer nutrients arriving at tissue
- Avascular (no blood vessels!)
- Chondrocytes produce antiangiogenesis factor, prevents the formation of new blood vessels, slows down repair since low blood flow = fewer nutrients arriving at tissue
94
New cards
bone / osseus tissue
maintained by osteocytes. Strong (matrix of calcified calcium salt deposits). Resists shattering (has flexible collagen fibers imbedded in bone matrix). 2/3 calcium phosphate
95
New cards
mucous membrane
Line passageways that have external connections. In digestive, respiratory, urinary, and reproductive tracts. Epithelial surfaces must be moist. To reduce friction. To facilitate absorption and excretion
96
New cards
lamina propria
areolar connective tissue component that supports the epithelial tissue superior to it
97
New cards
serous membrane
composed of mesothelium supported by areolar tissue. Line cavities not open to the outside. Are thin but strong
Have two layers:
- A parietal portion covering the cavity
- A visceral portion (serosa) covering the organs
- Have fluid transudate (serous fluid) to reduce friction between the parieal and visceral layers
Have two layers:
- A parietal portion covering the cavity
- A visceral portion (serosa) covering the organs
- Have fluid transudate (serous fluid) to reduce friction between the parieal and visceral layers
98
New cards
electrochemical gradient
For a particular ion (Na+, K+) is the sum of chemical and electrical forces acting on the ion across a plasma membrane. The electrochemical gradient represents a form of potential energy
99
New cards
resting potential
-70mv
100
New cards
passive/leak channels
Are always open. Permeability changes with conditions