Loop of Henle, DCT and the Collecting Duct
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
44 Terms
Which region of the kidney well generally have a higher osmolarity?
Renal medulla.
What is the osmolarity of the urine dependant on?
The osmolarity of the renal medulla.
What does the ability to concentrate filtrate depend on?
-The relative length of the loop of Henle
-The number of juxtamedullary nephrons
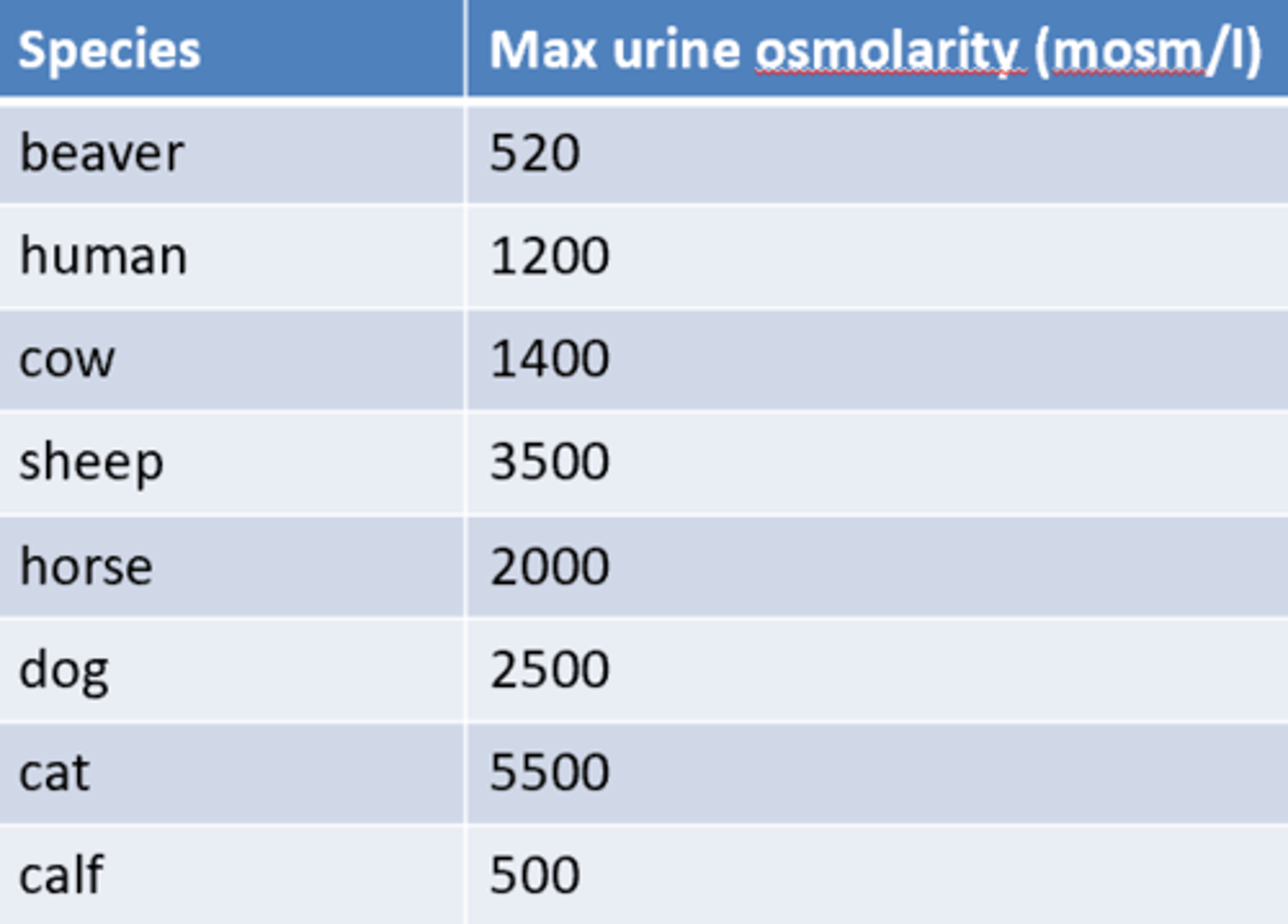
Is the maximum urine osmolarity constant across most species?
No, it varies relatively widely between species and animals of different ages (younger being worse at concentrating urine).
Why must there be a medullary osmotic gradient?
To give the kidney the capacity to concentrate urine.
What is the solute concentration of the fluid in the renal medulla?
High solute concentration so is hyperosmotic.
What is the solute concentration of the fluid in the renal cortex?
Low solute concentration so has a low osmolarity.
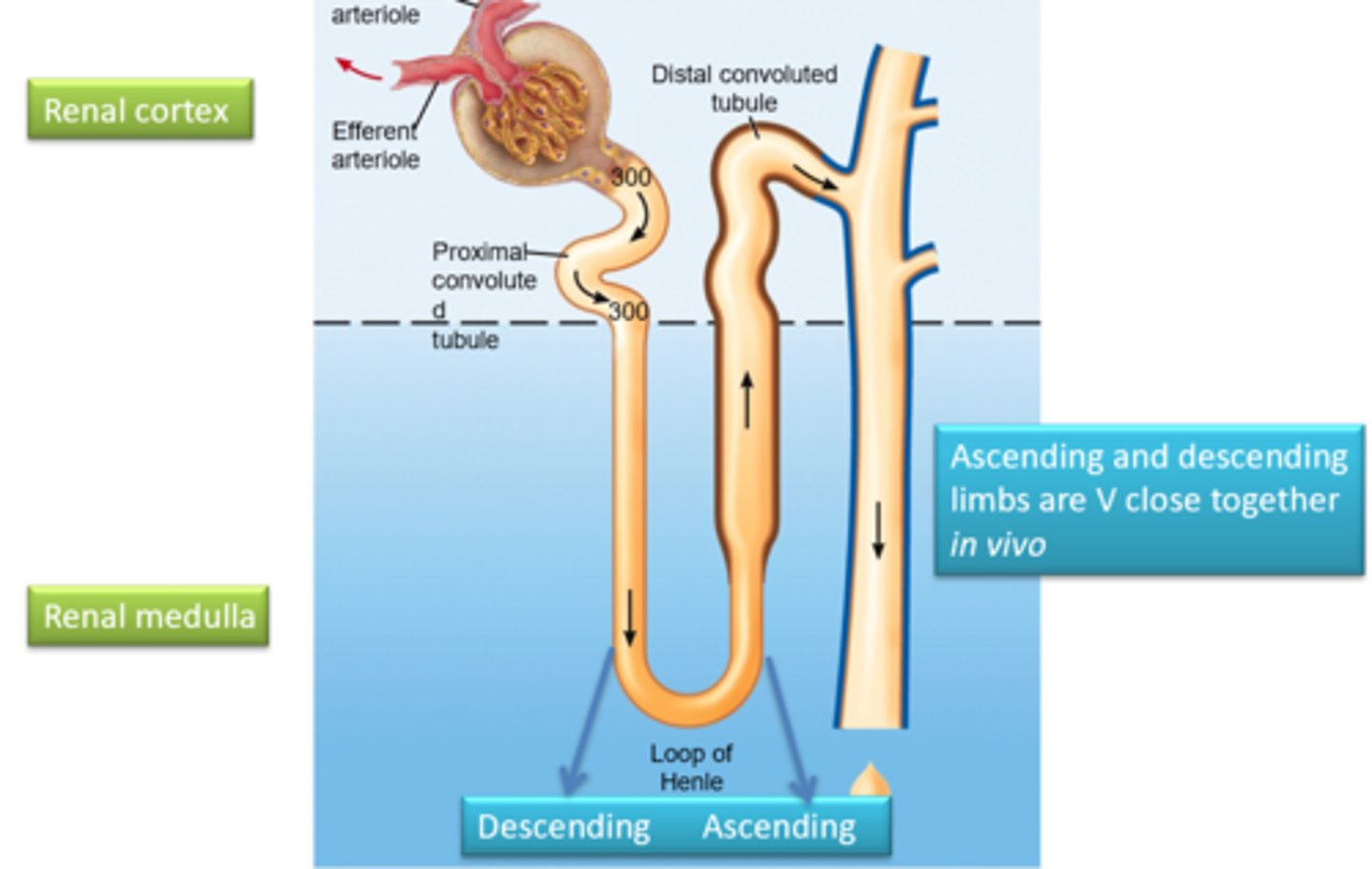
Describe the structure of the loop of Henle
Has a descending limb (attached to the PCT) and then curves round where it forms the ascending limb which joins the DCT.
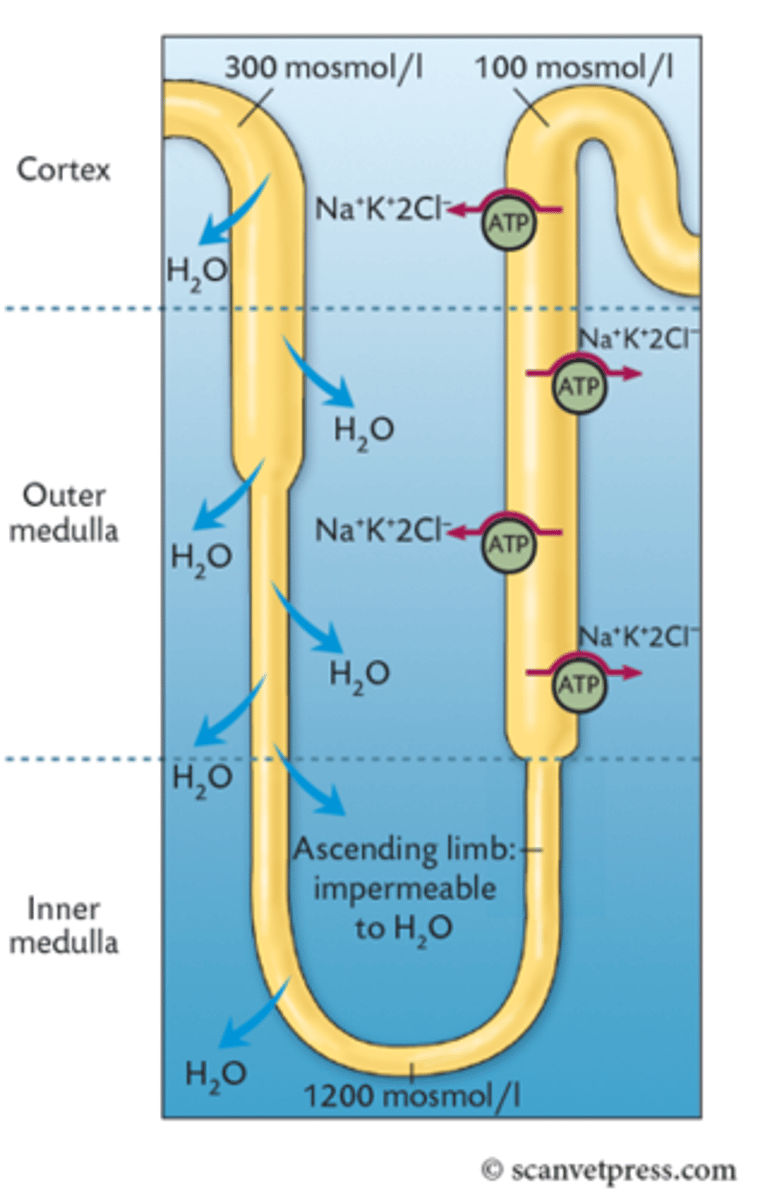
Describe the descending limb of the loop of Henle
-Lacks ion pumps
-Has many aquaporins so is very permeable to water
Describe the ascending limb of the loop of Henle
-Lacks aquaporins so is very impermeable to water
-Has many Na+K+2Cl- ion transporters and pumps many ions into the ISF from the filtrate
Describe how countercurrent multiplication creates hyperosmotic fluid in the inner renal medulla
-(Static Effect) In the ascending limb of the LOH, there are many ion transporters that transport solute out of the filtrate and into ISF raising its osmolarity
-This causes water to move out of the descending limb to equilibrate thus increasing the osmolarity of the filtrate within the descending limb
-(Fluid Flow) As fluid is constantly moving within the LOH, as fluid moves down it, more water is drawn out and hence the osmolarity raises towards the end of the loop
-Steps 1 and 2 are repeated in the LOH increasing the osmolarity of the ISF until the maximum osmolarity is reached (usually around 1200mOsm/L)
Why is the osmolarity of the distal convoluted tubule relatively low?
A large amount of ions have been pumped out (or moved down their electrochemical gradient) into the interstitial fluid from the ascending tubule of the LOH meaning the osmolarity of the filtrate decreases as it approaches the distal convoluted tubule.
Why is the osmolarity so high in the inner medullary region of the loop of Henle?
Due to the osmolarity of the interstitial fluid being so high (as the ascending tubule is pumping out ions into it) water freely moves out of the descending tubule without ions moving along with it (as there are no ion channels here). As fluid is continually moving through the LOH the osmolarity increases the further down the loop of Henle.
What is the name of the capillary network surrounding the loop of Henle?
The vasa recta.
What is special about the vasa recta?
-The capillaries run parallel with the limbs of the LOH
-Blood flows in the opposite direction to the filtrate and the hairpin loop slows blood flow down
-This ensures that the osmolarity inside the capillary is the same with the osmolarity of the ISF at any point in the medullary region
-Prevents the capillaries from removing the osmotic gradient created by the LOH
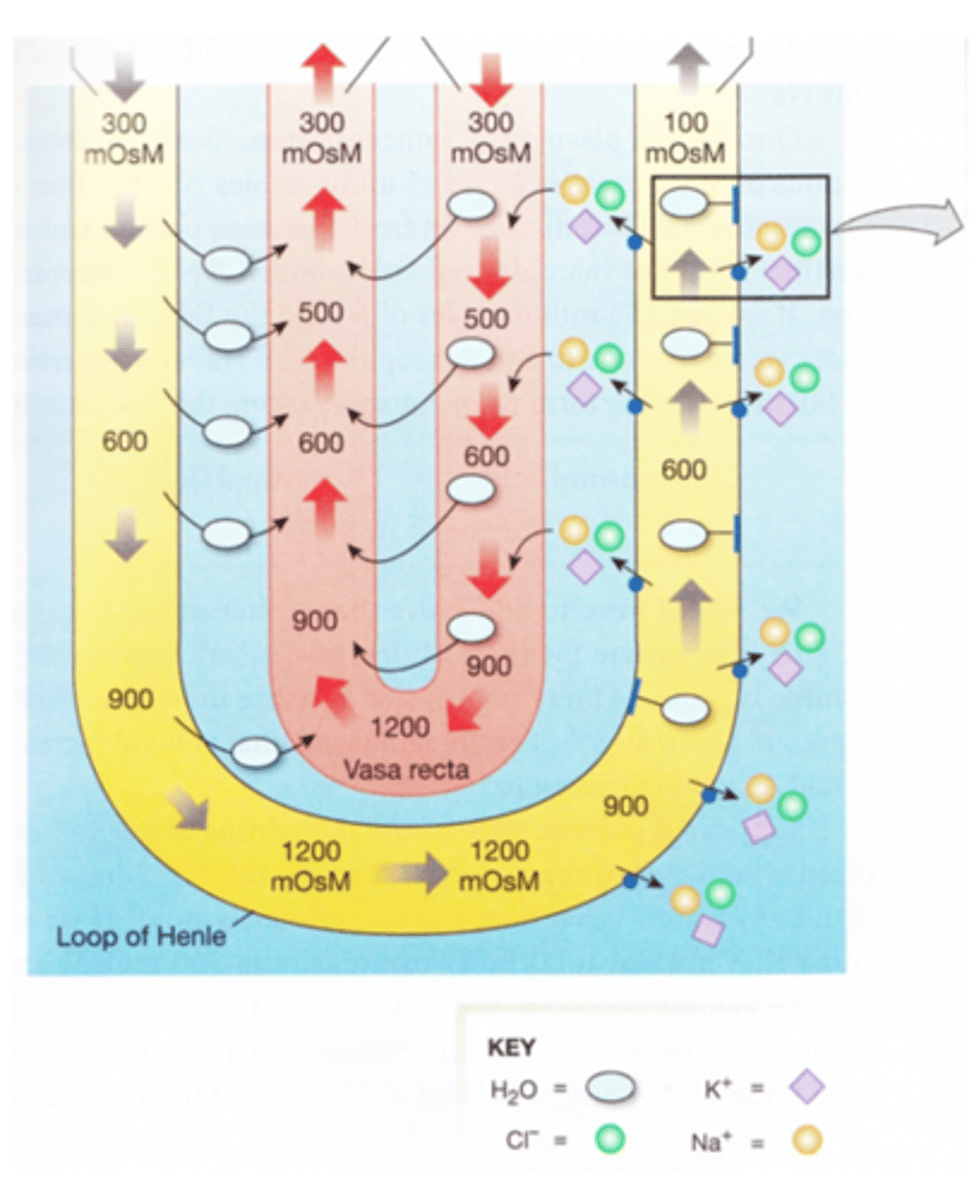
Describe the movement of fluid and ions in the vasa recta
-Blood (at 300 mosmol) enters the vasa recta.
-NaCl that has been reabsorbed by the thick ascending limb moves into the capillary and water moves out to the ECF (and ascending vasa recta).
-By the time the vasa recta reaches its U-bend, the plasma is extremely concentrated (typically 1200 mosmol in humans, more concentrated in carnivores).
-As the blood ascends, it draws in water that has left the thin loop (and also water from the descending vasa recta). So, it removes much of the water that has diffused out of the thin loop, so preventing dilution of the ECF.
-Removal of this water does not concentrate the filtrate
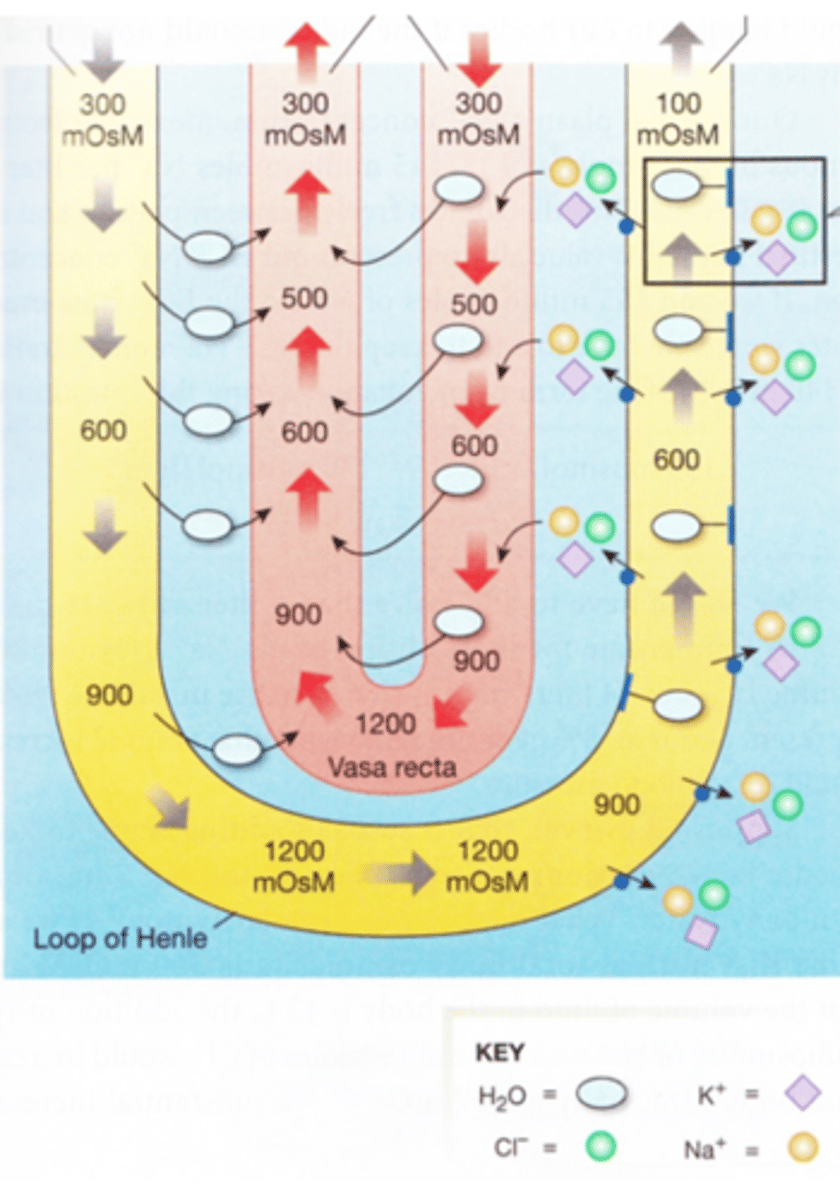
How would the osmolarity of the LOH be affected by sustained high blood pressure and flow rates?
The osmotic gradient would gradually become shallower and shallower due to a higher amount of ions being taken in by the blood.
What are the main components of the countercurrent multiplier?
-Specialised peritubular capillaries (vasa recta)
-Loop of Henle
Approximately how much of the created osmotic gradient in the renal medulla is created by the countercurrent multiplier system?
~50%.
Where is urea highest in concentration in a nephron?
Collecting duct.
Explain how urea can act as an osmotic particle to create the hyperosmotic gradient in the renal medulla
-Urea becomes more concentrated in the filtrate as it travels to the collecting ducts
-Urea is at its highest concentration in the collecting ducts
-Towards the terminal part of the collecting duct and at the terminal part of the descending limb of the LOH there are urea protein channels that allow its movement
-As urea is high in concentration in the collecting duct, it diffuses out into the ISF through its protein channels increasing the osmolarity of the ISF
-Urea is lower in concentration in the descending limb of the LOH and hence diffuses in through its protein channel increasing the osmolarity of the LOH further
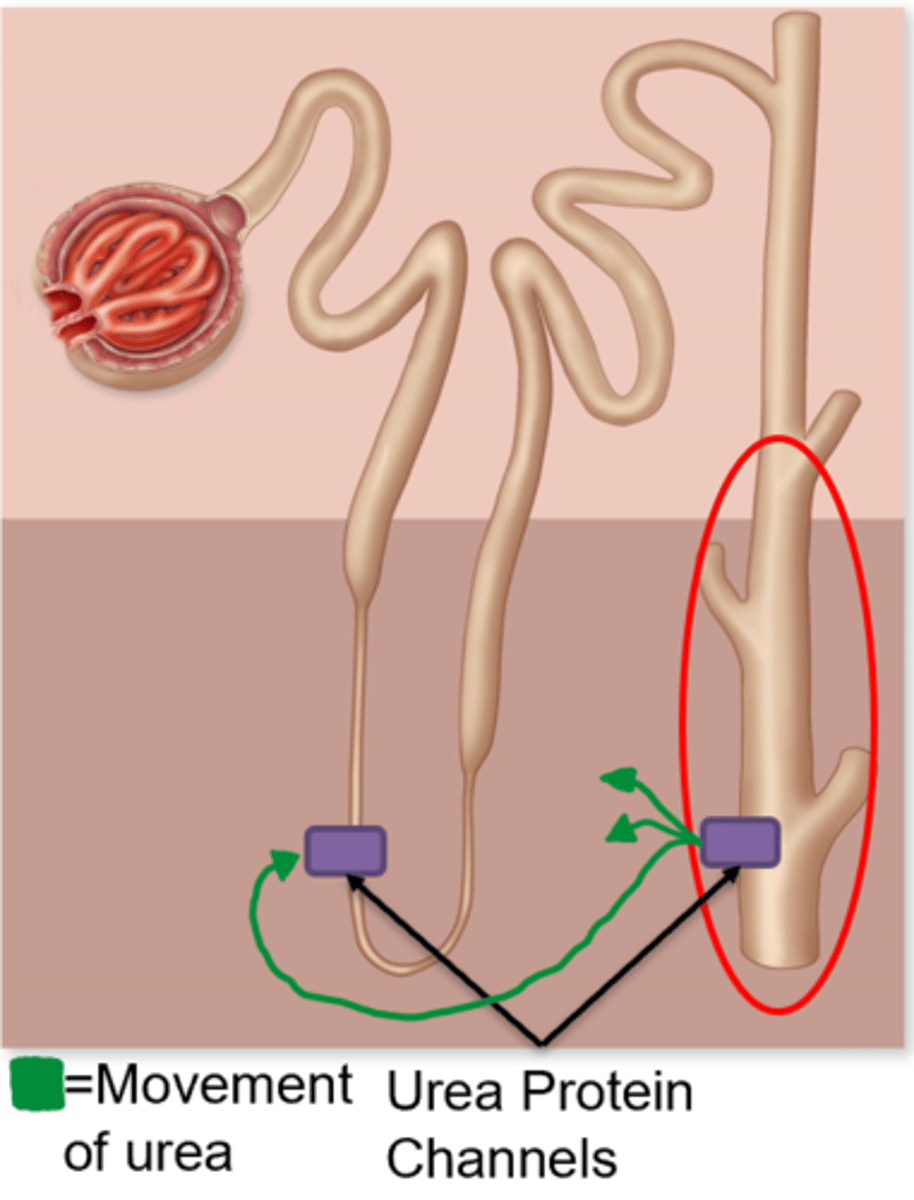
Approximately how much of the created osmotic gradient in the renal medulla is created by urea recycling?
~50%
How does ADH effect urea recycling?
It upregulates urea channels in the inner medullary collecting ducts allowing more urea to flow passively into the interstitial fluid and then back into the thin descending limb of the LOH.
As a %, how much water is reabsorbed in the DCT and collecting duct?
4-9%
Does the collecting duct receive filtrate from one nephron or multiple?
Multiple.
What determines the final osmolarity of urine?
The relative permeability of the epithelial cells of the DCT and the collecting duct to water. The more permeable they are, the more water will leave the filtrate by osmosis.
What controls the water permeability of the epithelial cells in the DCT and collecting duct?
ADH.
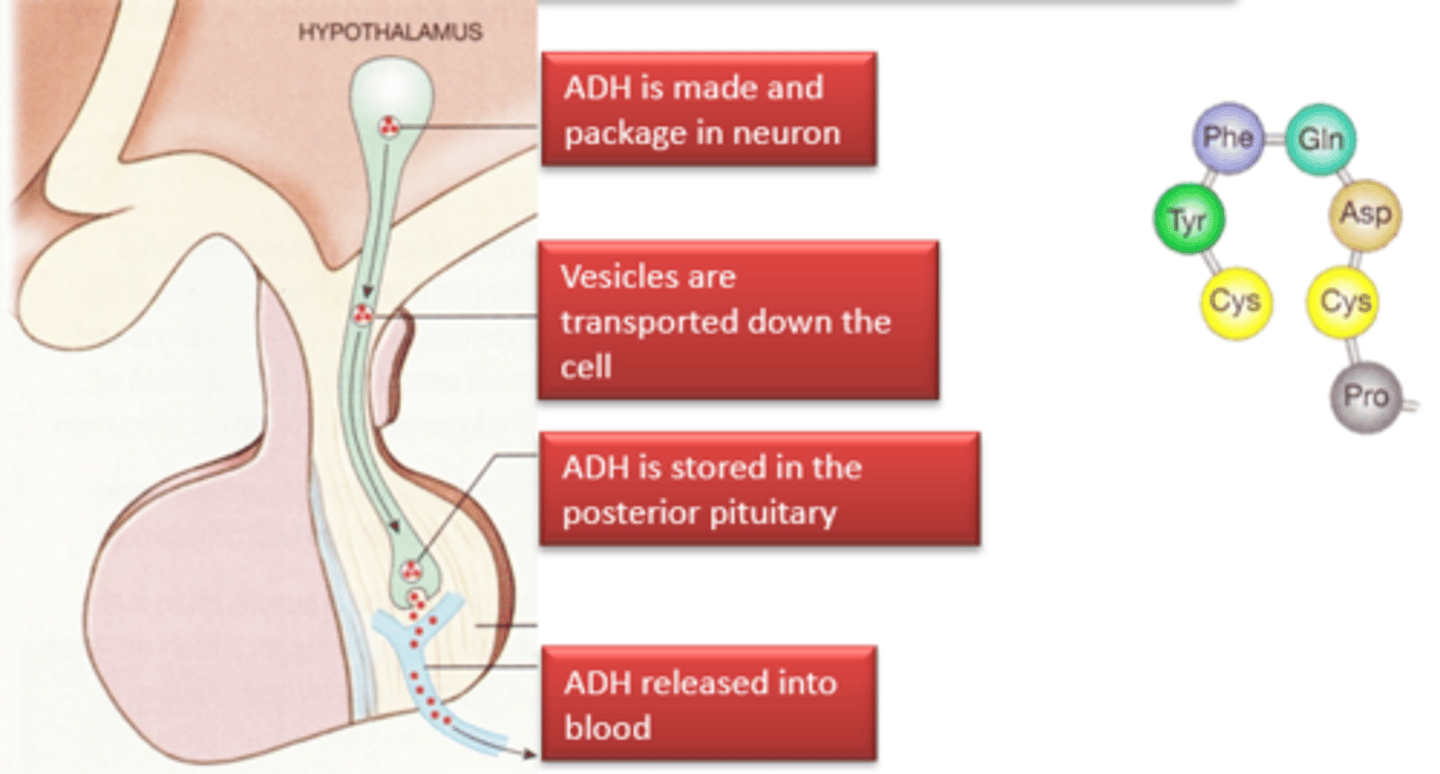
Describe the creation and transport of ADH
-Made and packaged in neurones in the hypothalamus
-Vesicles are transported down the cell
-It is then stored in the posterior pituitary gland
-Then it is released into the blood when it is needed
Explain what circulating ADH does to collecting duct cells
-Firstly ADH binds to vasopressin receptors on the basolateral membrane of collecting duct cells (CDC)
-This causes the receptor to active the cAMP secondary messenger system leading to the movement of stored aquaporins towards the apical membrane
-When the aquaporins arrive at the apical membrane, they are incorporated
-This allows water to move via osmosis through the CDC into the blood
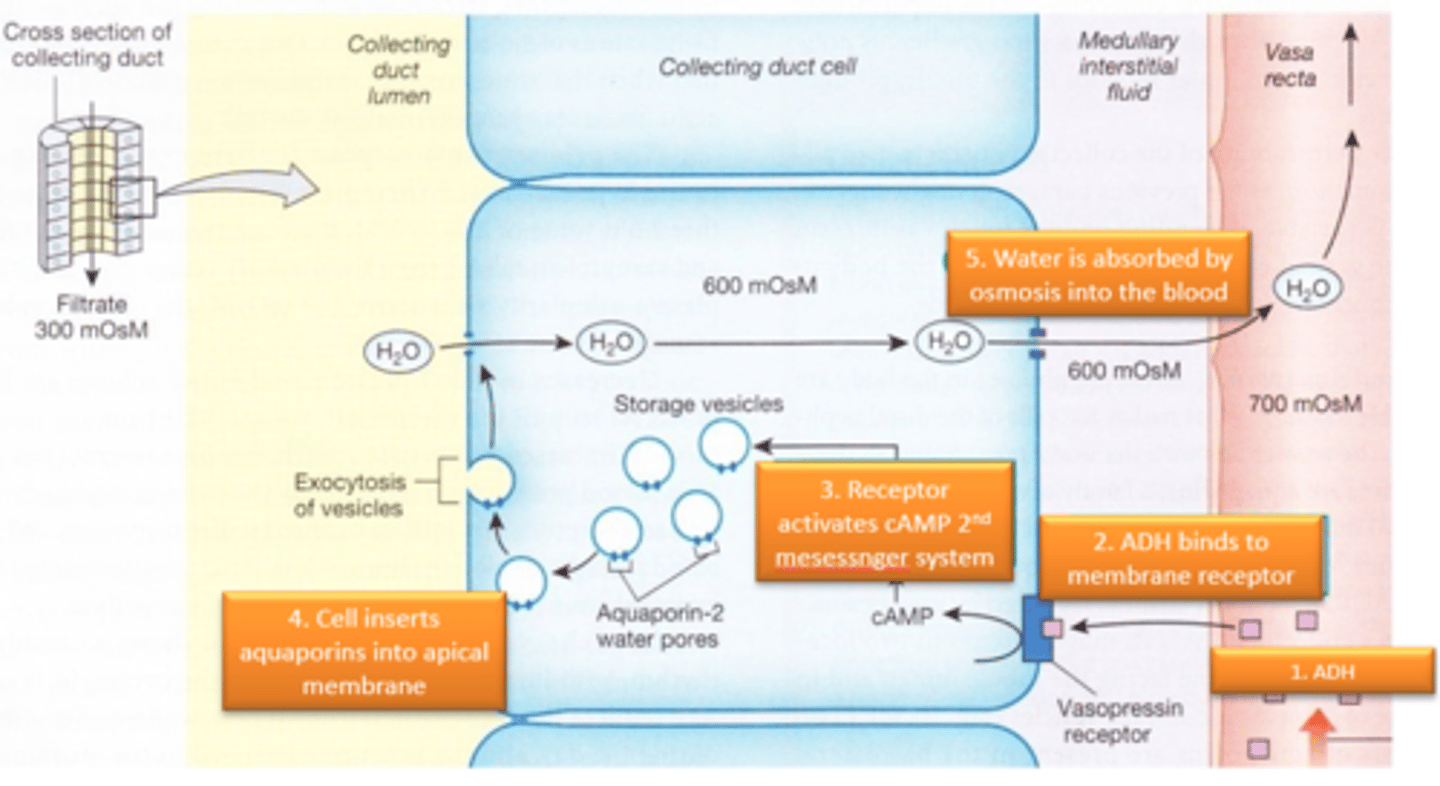
Does a high level of ADH in the blood cause dilute or concentrated urine?
Concentrated as more water leaves the filtrate.
What are the levels of ADH in an animal which is excessively hydrated?
Low/none.
What are the levels of ADH in an animal which is dehydrated?
High.
How is the concentration of urine controlled?
By the level of circulating ADH in the blood which effects how much water is reabsorbed from the filtrate in the DCT and collecting duct (hence determining how concentrated the urine is).
Describe the secretion and absorption of sodium by the time the filtrate has entered the DCT
-100% filtered
-~90 reabsorbed in total
--~70% reabsorbed in the PCT
--~20% reabsorbed in the LOH
Describe the secretion and absorption of potassium by the time the filtrate has entered the DCT
-100% filtered
-100% reabsorbed
--~70% reabsorbed in the PCT
--~30% reabsorbed in the LOH
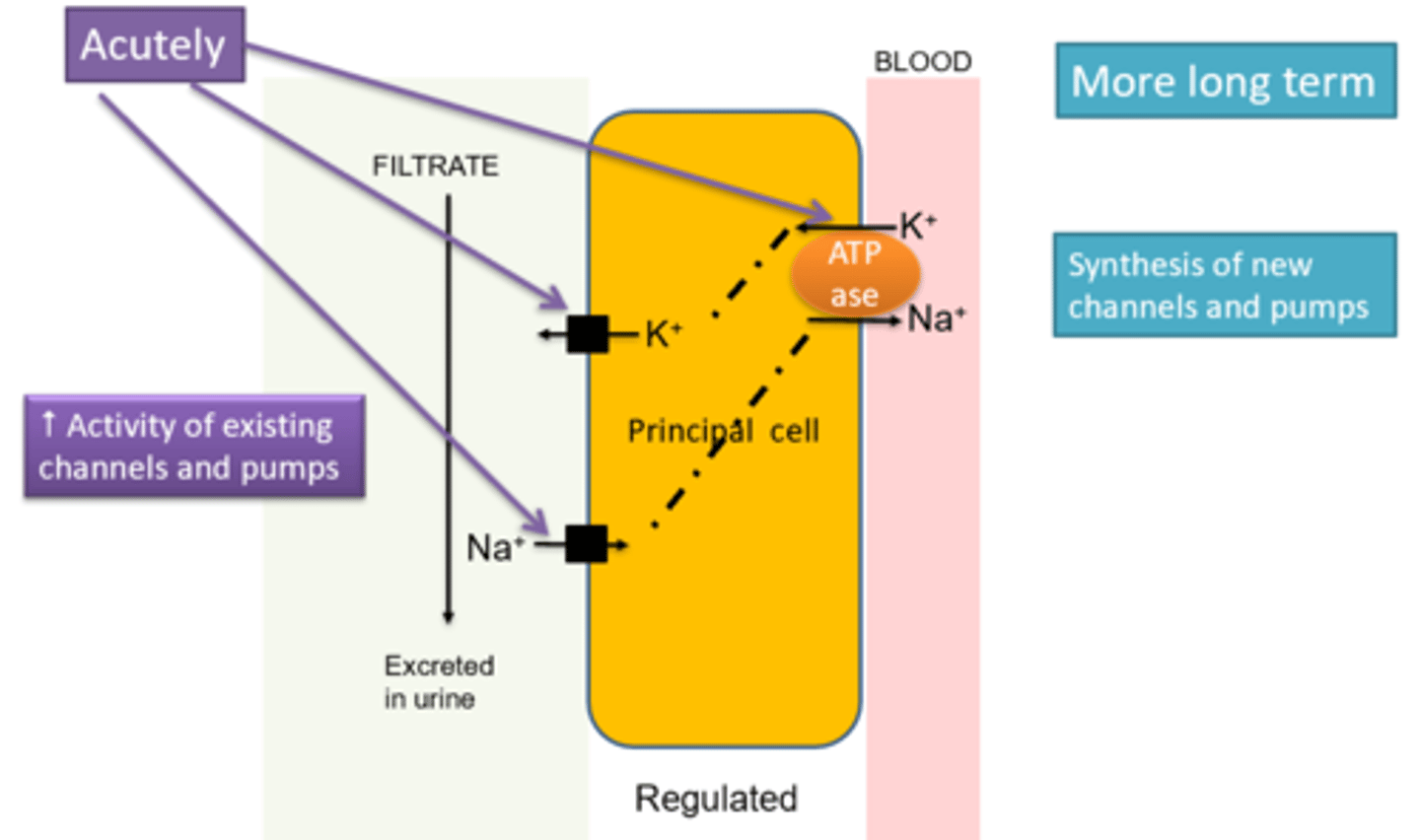
Describe how principal cells absorb and secrete ions
-They have asymmetrical arrangements of Na+K+ATPase that allow the secretion of K+ and the absorption of Na+
--Creates an electrochemical gradient for other ions to move down
-They have no aquaporins so it allows movement of Na+ independent of water
-The action of their ion pumps is modulated by aldosterone
What is the difference between principal cells in the DCT and CD and the tubular cells of the PCT
-Principal cells have no villi (as they deal with lower volumes of fluid)
-Principal cells are under hormonal control (by aldosterone)
Describe how aldosterone affects principle cells in the DCT and collecting duct
-Increases the activity of the Na+K+ATPase pump acutely
--In the long term it can increase the number and activity of existing pumps and channels
-Hence more K+ is secreted and more Na+ is absorbed in the presence of aldosterone
Where is aldosterone produced?
Zone glomerulosa of the renal cortex.

What is the effect of increased aldosterone secretion on ion levels in the blood and urine?
-Increases Na+ concentration in the blood
-Decreases K+ concentration in the blood
-Decreases Na+ concentration in the urine
-Increases K+ concentration in the urine
Describe the secretion and absorption of calcium by the time the filtrate has entered the DCT
-50% is bound to albumin so only 50% is free and filtered
-~70% reabsorbed in the PCT
-Selective reabsorption of Ca2+ in the DCT and CD under hormonal control
-Normally 1-2% filtered Ca2+ is excreted
Describe the secretion and absorption of phosphate by the time the filtrate has entered the DCT
-100% filtered
-Reabsorption in PCT by Na+ co-transport under hormonal control
--Not reabsorbed in the DCT and CD
-Dietary excess is excreted via the kidney
What hormone regulates the level of calcium and phosphorus in the blood?
Parathyroid hormone (PTH).
Describe the action of parathyroid hormone in the kidney
-Released in response to decreased Ca2+ levels in the blood
-Causes decreased reabsorption of P in the PCT
-Causes increased reabsorption of Ca2+ in the ascending limb of the LOH, DCT and CD