Critical Care NCLEX
1/250
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
251 Terms
What is the phlebostatic axis?
fourth intercostal space, midaxillary line. This is where we level to zero lines to ensure accurate numbers. This can be accomplished with the pt lying supine or HOB at 45. Lines should be zeroed every 4 hrs.
What is CVP and what does it measure?
Central Venous Pressure (or right atrial pressure): estimates central venous blood/fluid volume and right heart function. Normal is 2-6 mmhg
How can CVP be affected?
decreased cardiac output, forced exhalation, HF, hypovolemia, PEEP, pleural effusion, PE, fluid status
What is PAP and what does it measure?
Pulmonary Pressure: used to measure left ventricular filling pressures. This is displayed like a BP normal sys: 15-25mmhg normal diastolic: 8-15 mmhg
How can PAP be affected?
What is SVR and what does it measure?
Systemic vascular resistance: measures the resistance in the circulatory system that is used to create blood pressure.
how can SVR be affected?
vasoconstriction/vasodilation
What is Cardiac Index and how can it be affected?
Cardiac output divided by body surface area. This gives us a more patient specific number. This can be affected by preload, after load, contractility, and the patient's body surface area.
What is Cardiac Output and how can it be affected?
amount of blood pumped by each ventricle during a given period. This can be affected by after load, pre load, contractility.
What invasive lines can be used to measure hemodynamics?
arterial line or pulmonary artery catheter (swan Ganz)
What is the nursing care for a patient with an invasive line?
Assist with line insertion, monitor respiratory and cardiac status, maintain line patency and integrity, obtain hemodynamic readings from catheter, prevent infection.
What hemodynamic changes may occur with dysrhythmias?
low SV, CO, BP
What is included in the assessment of the patient with dysrhythmias/signs of altered cardiac output?
changes in LOC, chest pain, hypotension, weak pulses, fatigue, SOB, crackles, dizzy, restlessness
What is asystole?
flat line, no QRS present, no pulse, HR=0, no BP, lethal if not corrected in 3-5 minutes.
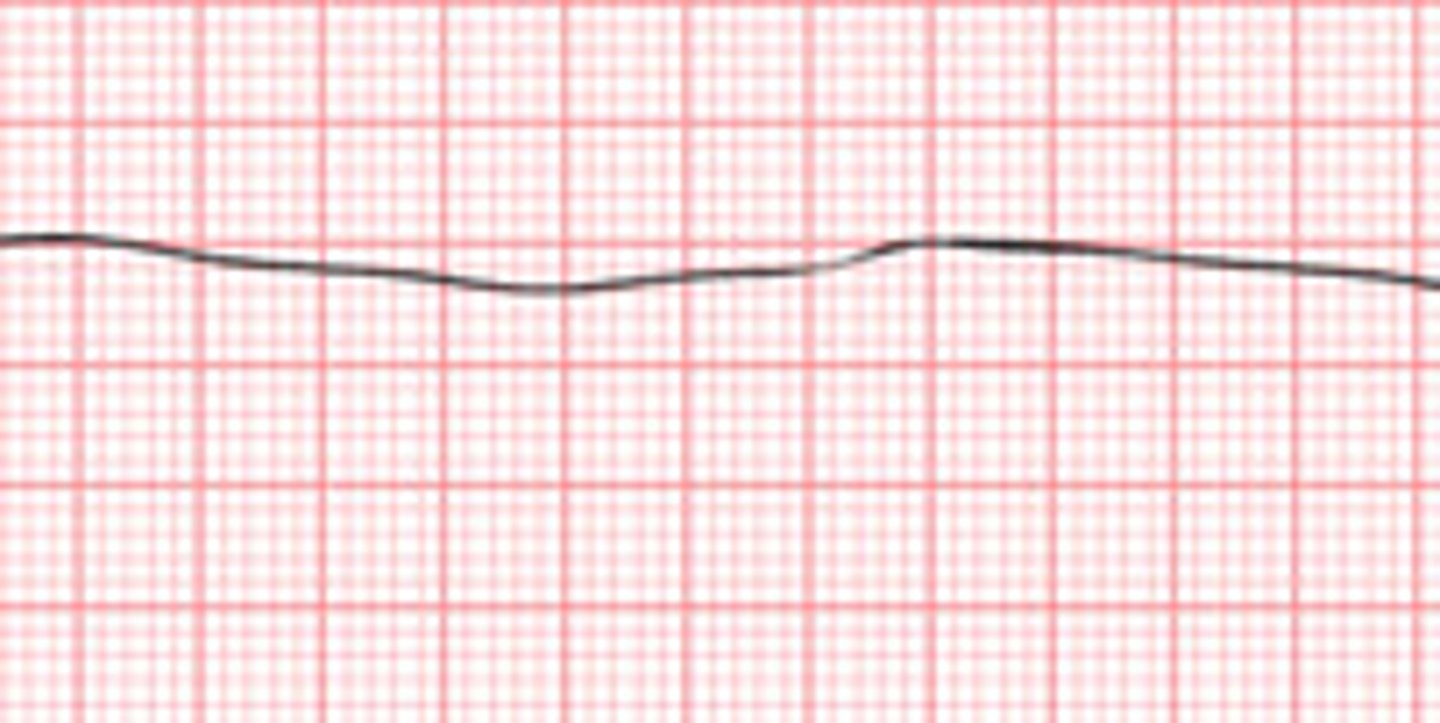
What is the treatment for asystole?
DO NOT SHOCK!!!!! CPR, check asystole in two leads, epinephrine, pacemaker, consider the causes.
What is sinus tachycardia?
100-150bpm. rhythm is normal but too fast. workload of the heart is increased while the perfusion is decreased. this is a normal response to the body's increased demand for O2
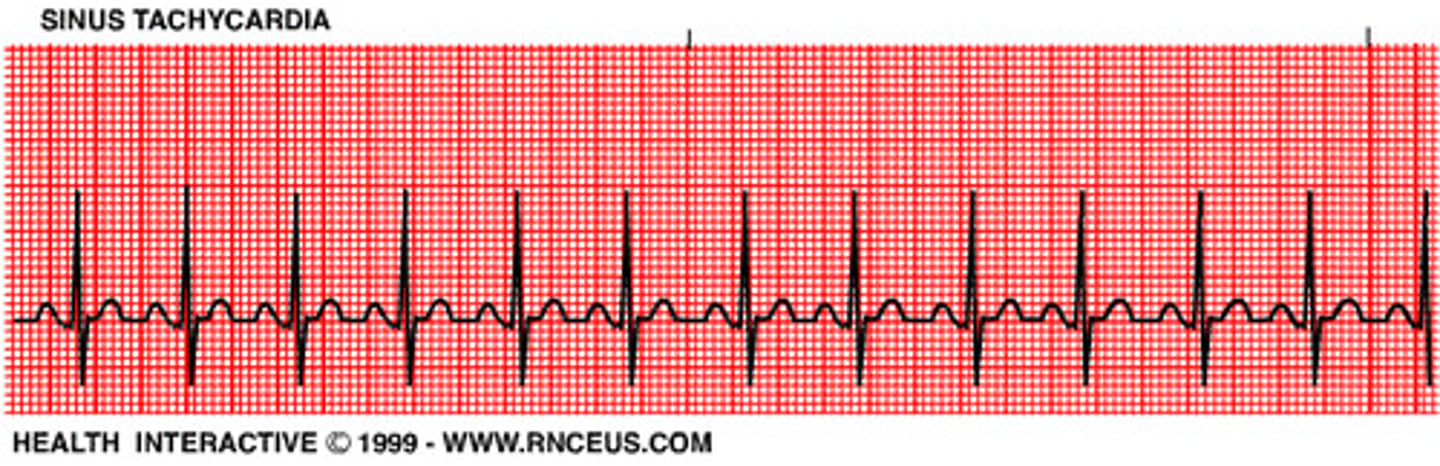
What is the treatment for sinus tachycardia?
treat the cause: pain, hypovolemia, fever, exercise, anxiety, medications that stimulate sympathetic response, stimulants, illicit drugs
What is sinus bradycardia?
sinus rhythm but the heart rate is below 60bpm. may be normal for athletes or during sleep, seen with inferior and posterior infarctions

What is the treatment for sinus bradycardia?
ONLY TREAT IF PT IS SYMPTOMATIC. treat the cause. Give O2, atropine, pacemaker, dopamine or epinephrine infusion, assess for hypotension
What is the treatment for a fib?
O2, anticoagulants, cardioversion (for new onset and symptomatic patients), meds to control the ventricular rate (diltiazem, digoxin, beta blockers), watch for symptoms of decreased CO/ HF, antiarrhythmics
What is a fib?
Atria is quivering but not contracting, AV node acts as a filter to protect the ventricle

What is supraventricular Tachycardia?
cannot identify p wave and narrow QRS. rapid heartbeat that develops when the normal electrical impulses of the heart are disrupted.
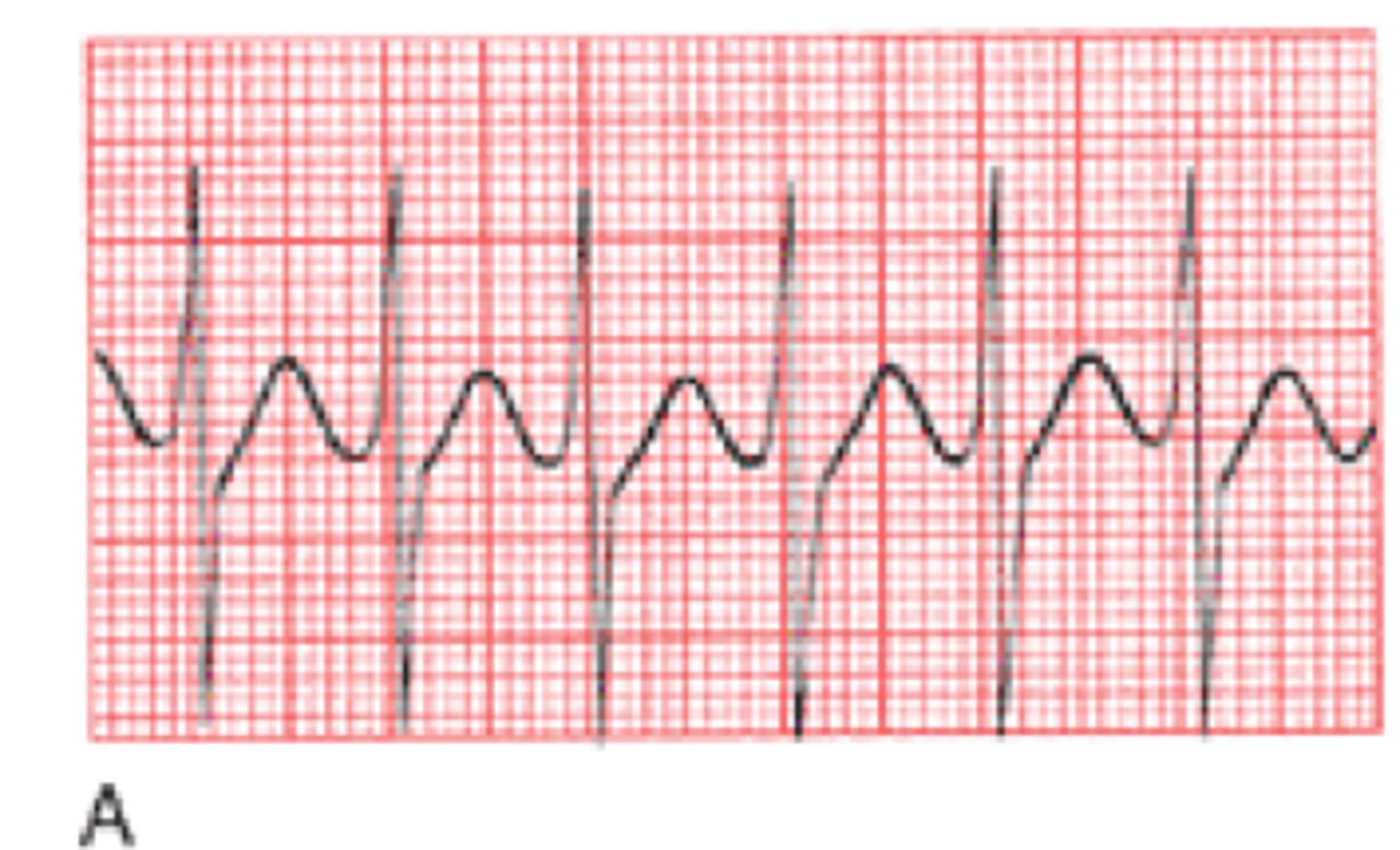
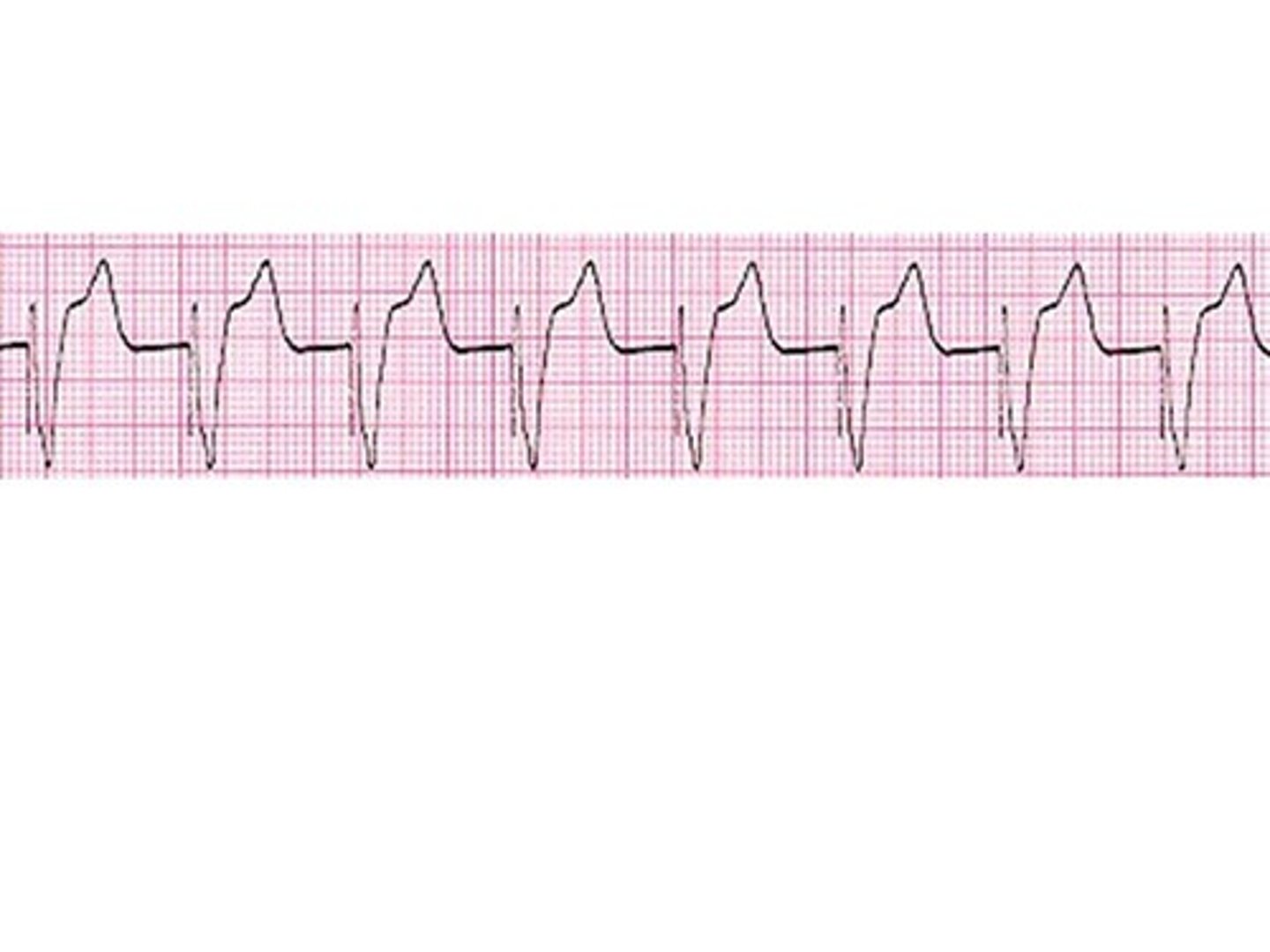
What is v tach?
BAD, ventricles are pumping too fast

What is the treatment for v tach?
Stable: O2, amiodarone, correct electrolyte imbalances
Unstable: cardioversion, O2
no pulse: defibrillate
What is v fib?
you are dead, ventricles are quivering, clients have no pulse/BP/RR. fatal if not terminated in 3-5 minutes. Want Coarse v fib rather than fine because there is more of a rhythm to shock.

What is the treatment for v fib?
defibrillation immediately, CPR, epinephrine/vasopressin, O2, Amiodarone (V-FIB = D-FIB)
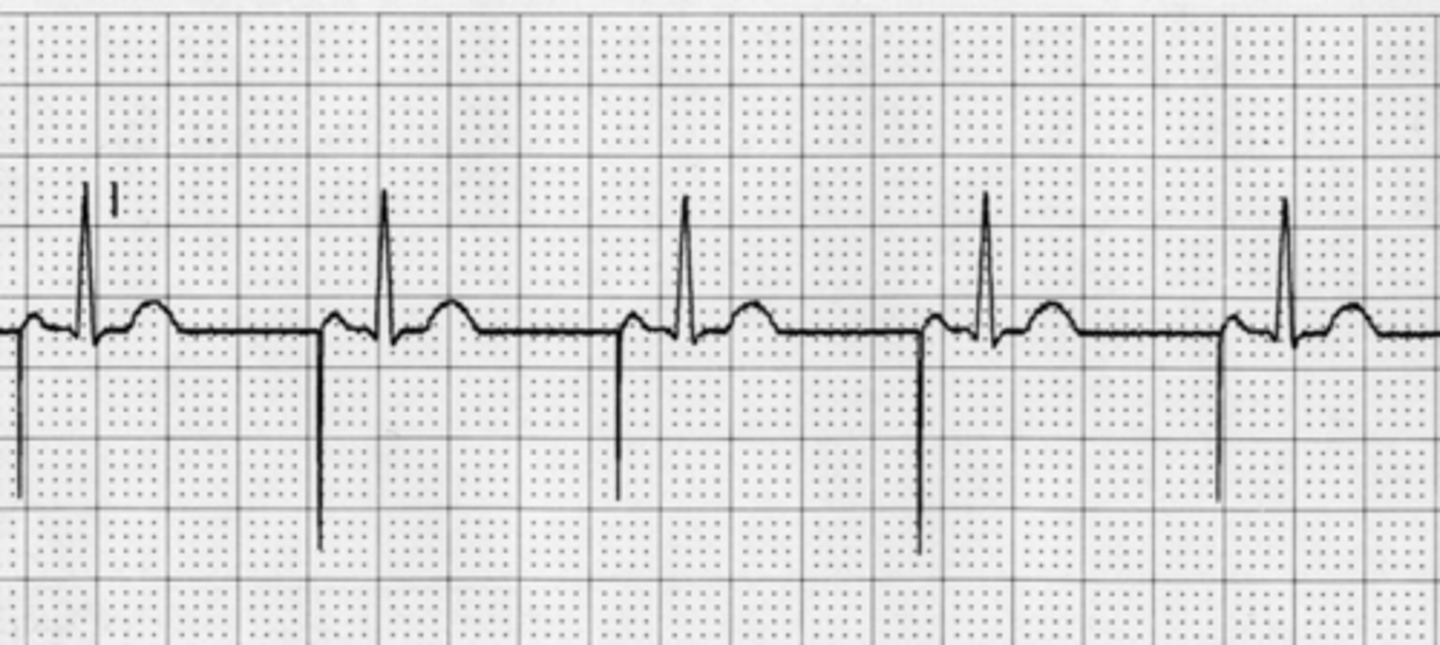
What is PEA?
patient has a rhythm but NO PULSE, heart muscle loses its ability to contract even though the electrical activity is preserved. This is treated like asystole.

What is the treatment for PEA?
Treat like asystole. CPR, epinephrine, rapid identification of the causes.
What is third degree heart block?
PR interval is regular but does not match up to QRS.

What is the treatment for third degree heart block?
pacemaker
What is fixed pacing?
Pacemaker will pace no matter what the intrinsic heart rate is doing.
What is demand pacing?
Lets the heart beat on its own as long as it is appropriate.
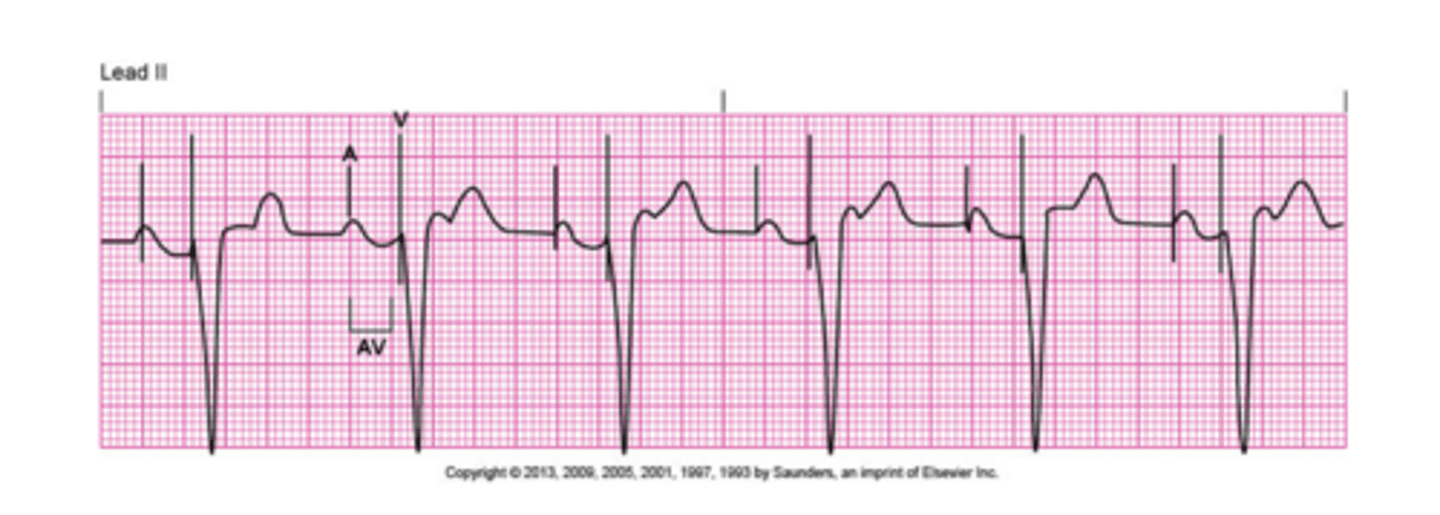
What is ventricular pacing?
Pacing is done within the ventricle. Firings are sent before the QRS.
What is atrial pacing?
Pacing is done within the atria. Firings are sent before the p wave.
What is dual pacing?
Combination of both atrial and ventricular pacing.
What are some issues that can happen with a pacemaker?
Failure to pace: no pacemaker spikes. check connections and power to pacemaker.
Failure to sense: pacemaker spikes are not aligning with QRS and not pacing appropriately, ensure it is set to correct mode and does not need an increase in sensitivity.
Failure to capture: pacemaker spike is being produced but not capturing a QRS.
What is atropine?
use: symptomatic bradycardia
action: increases HR by increasing SA and AV conduction.
adverse affects: tachycardia, headache, ischemia of heart
What is adenosine?
use: SVT
action: acts as a "hard reset" for the heart. The heart will stop for a few seconds then hopefully begin back into a normal rhythm. This is done by decreasing AV conduction.
adverse affects: lightheadedness, headache, dizziness, dyspnea, chest pain.
What is amiodarone?
use: dysrhythmias, during a code 300mg loading dose is given and then 150mg can be given 3-5 minutes later.
action: reduces membrane excitability.
adverse affects: bradycardia, headache, hypotension.
What is dopamine?
use: symptomatic hypotension.
action: vasoconstrictor used to increase BP and contractility.
adverse affects: chest pain, SOB, may cause dysthymia.
What is Dobutamine?
use: cardiogenic shock and distributive shock.
action: increases contractility and volume.
adverse affects: chest pain.
What is epinephrine?
use: v fib, PEA, pulseless V tach, asystole.
action: Potent vasoconstrictor to increase contractility, BP, HR, and perfusion. Given every 3-5 minutes during a code.
adverse affects: tachycardia, hypertension.
What is Vasopressin?
use: given 2nd line after epi during codes, one time dose of 40 units. V fib, pulseless V tach.
action: intense vasoconstriction at high doses.
What is lidocaine?
use: antidysrhythmic
action: suppresses ventricular ectopy.
adverse affects: toxicity, watch for lethargy, confusion, muscle twitch, seizures
What is Primacor (milrinone)?
use: improves CO and treats cardiogenic shock.
action: increases contractility
What is defibrillation?
used for v fib and v tach with no pulse. Delivers a shock that is not synched to QRS. Can be implanted as long term care to prevent v tach and cardiac arrest.
What is cardioversion?
used for a fib/flutter, SVT, v tach with a pulse, and offered when symptomatic. shocks are synched with the QRS.
it is important to anticoagulant beforehand because it could dislodge a clot or embolism.
What EKG changes might occur with hyperkalemia?
ST depression, peaked t waves, wide/flat QRS, prolonged PR interval.
Seen with third degree AV block, asystole, v fib, and v tach.
What EKG changes might occur with hypokalemia?
wide t waves, st depression, possible U wave.
seen with torsade's or v fib.
What EKG changes might occur with hypomagnesemia?
tall t waves, long QT/PR interval.
seen with torsade's v tach
What EKG changes might occur with hypermagnesemia?
peaked t wave, wide QRS
rare, can cause AV block and asystole
What EKG changes might occur with hypercalcemia?
short QT, long QR
seen with bradycardia or v-fib
What EKG changes might be seen with hypocalcemia?
lengthened QT, short QRS
Dysthymias unlikely, maybe A-fib or torsade's
What dysrhythmias are seen with the SA node?
sinus tachy and sinus Brady
What dysrhythmias are seen with the AV node?
junctional rhythms, SVT, A fib
What dysrhythmias are seen in the ventricles?
PVC, V tach, tosades, v fib
How does perfusion apply to cardiogenic shock?
there is a decrease in perfusion because the heart is failing to pump efficiently, this causes less fluid to be perfused through the body.
How does perfusion apply to hypovolemic shock?
there is a decrease in perfusion because of loss of intravascular volume (fluid or blood).
How does perfusion apply to distributive/vasogenic shock?
there is a decrease in perfusion die to widespread vasodilatation that leads to decreased blood flow to organs.
What is the pathophysiology with cardiogenic shock following an MI?
cardiogenic shock usually follows an anterior wall infarction which leads to the heart being unable to pump
What is the initial stage of shock?
occurs when there is hypo perfusion in the body. there are usually no obvious signs and symptoms. During this stage the body is compensating okay and it can be reversed.
What is the compensatory stage of shock?
This stage occurs when there is a sustained reduction in tissue perfusion. symptoms become apparent and it presents as hyperventilation, high HR, low BP, uncontrollable blood sugars and changes in LOC.
What is the progressive stage of shock?
This stage begins when compensatory mechanisms begin to fail and the body starts shunting blood to the vital organs (brain, heart, lungs). This presents as edema, dysrhythmias, low BP with narrow pulse pressure, tachypnea, cold/clammy skin, absent bowel sounds, lethargy.
What is the refractory stage of shock?
This stage of shock is usually not reversible. organs begin to fail and we see presentation as dysrhythmias, cerebral changes, pt becomes unresponsive, basically everything is shutting down.
What is hypovolemic shock?
Causes: hemorrhage, trauma, surgery, vomiting, diarrhea, burns, anything that causes a major blood or fluid loss.
Hemodynamics: high HR, low BP, low CVP, low preload, low CO, low SVO2, high RR, low UO, AMS, flat neck veins.
Treatment: Fluid replacement and treat the cause. Give blood or crystalloids (NS/LR), want MAP to be sustained between 60-70.
What is cardiogenic shock?
Causes: MI, cardiomyopathy, myocarditis, severe HF.
Hemodynamics: high HR, low BP, low CO, high CVP, low SVO2
Treatment: promote contractility. decrease myocardial O2 demand by providing supplemental O2, give diuretics or vasodilators (depending on BP).
What is obstructive shock?
Causes: tension pneumo, cardiac tamponade, any compression of the great veins, pericarditis, impaired diastolic filling.
Hemodynamics: low CO, high CVP, high SVR, high PAP, low SVO2, low BP high HR.
Treatment: remove obstruction
What is neurogenic shock?
Causes: imbalance between sympathetic and parasympathetic stimulation, direct or indirect insults to the neuro system, spinal cord injuries.
Hemodynamics: HR/BP/CO are all normal to low, low SVR, low perfusion.
Treatment: hemodynamic stabilization
What is anaphylactic shock?
Causes: allergies to food, bugs, meds, ect.
Hemodynamics: high HR, dysrhythmias, low BP, low CO, low SVO2
Treatment: Epinephrine
What is septic shock?
Causes: immunosuppression, bacteremia.
Hemodynamics: high HR, high RR, low BP, temp can be high or low, widened pulse pressure, high CO, low RAP
Treatment: stopping further development, finding source and treating it, timely identification, control BG (<180), control temp.
What are the causes of elevated ICP?
increased brain volume (cerebral edema), increase in CSF, or an increase in blood volume.
How is Cerebral Perfusion Pressure (CPP) calculated?
MAP-ICP=CPP
What is the Glasgow Coma Scale?
A scale used to assess a patient's neuro function by assessing their eye opening, verbal response, motor response.
What GCS score is consistent with a coma?
3-8
As the nurse what should you do if your pt has a GCS of less than 5?
call the Indiana donor network (IDN) for possible organ donation.
What is decorticate posturing?
Hands pulled to chest and hyper-extended. Internal rotation and adduction of the arms with flexion of the elbows, wrists & fingers.
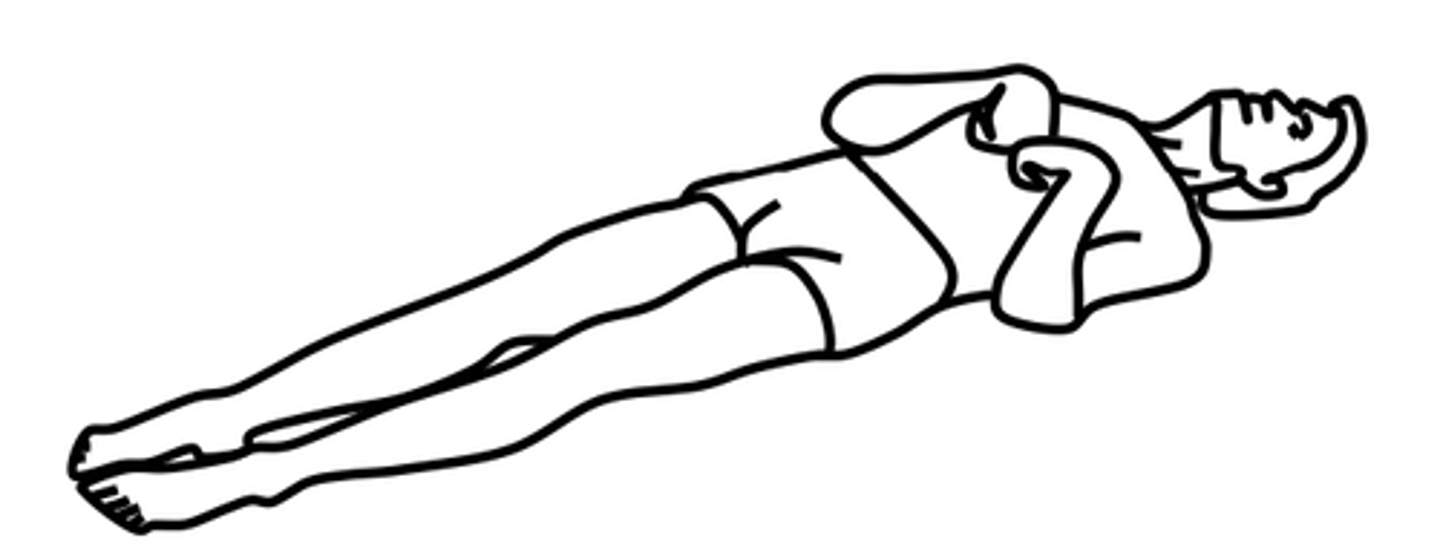
What is decerebrate posturing?
Abnormal body posture involves the arms and legs being extended straight out, the total is being pointed downward, and the head and neck being arched backwards.
What is the care of a client with an ICP monitoring device?
positioning: head of bed elevated to 30 degrees if appropriate. avoid trendelenburg's position.
moving: prevent flexion of the neck and hips. maintain neutral position of the head, prevent shivering.
stimulation: decrease environmental stimuli.
What is the normal value of ICP?
0-15 mmhg
What is considered an elevated ICP?
greater than 20 mmhg for 5 minutes or more
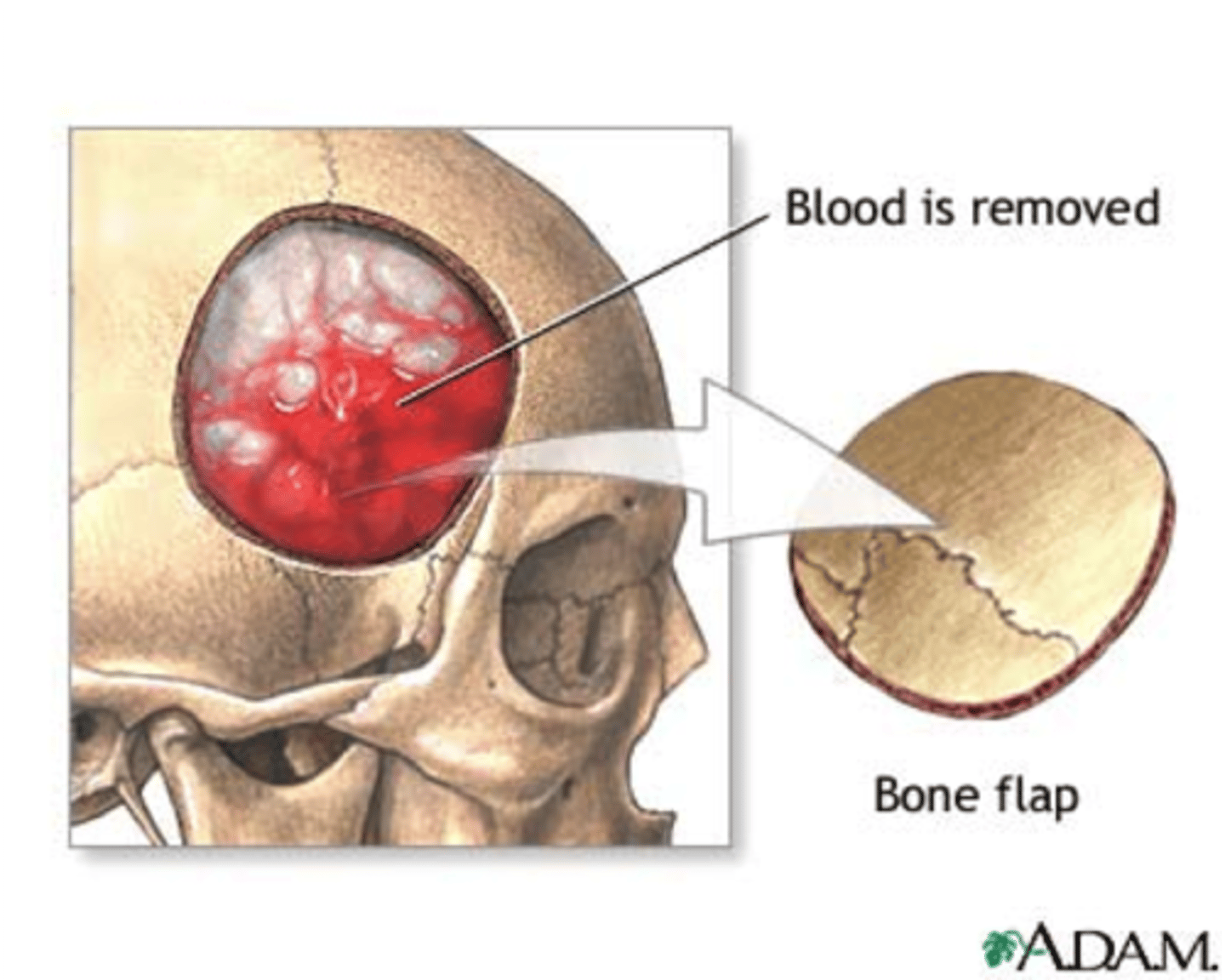
What is a craniotomy?
evacuate hematomas, remove bone fragments, remove foreign objects, by removing a portion of the skull to expose the brain
What is mannitol?
osmotic diuretic used to lower ICP. works by pulling water from the extracellular space into the vasculature. causes diuresis.
What are corticosteroids?
used to stabilize the cell membrane and reduce the leakiness in the blood-brain barrier. this decreases cerebral edema. clients must be tapered off of corticosteroids
What are anticonvulsants used for in ICP?
given prophylacticly to avoid seizures. examples of med: phenytoin, fosphenytoin, levetiracetam
Why are antipyretics and muscle relaxers given for ICP?
given to decrease temperature, decrease metabolism, decrease shivering.
examples of meds: acetaminophen, diazepam
Why are vasoconstrictors given for ICP?
given to maintain good cerebral perfusion pressure (above 70 is goal).
example of meds: norepinephrine, dopamine
What paralytic agents are given for ICP and what is the assessment for them?
cisatracurium. train of four assessment is done and 2 out of 4 twitches are goal.
What are the sedation agents given for ICP and what assessment is done for them?
propofol, lorazepam. BIS monitoring is done for these medications and goal is 40-60
What are the analgesics given for ICP and what assessments are done for them?
fentanyl, codeine. pain assessments are done for these medications using the FLACC scale. Respiratory assessments are also important.
What are the different types of ICP monitors?
Intraventricular catheter/ external ventricular drain (allows drainage), subarachnoid bolt (no drainage), epidural sensor (no drainage), Parenchymal Fiberoptic Catheter.
What is a subarachnoid bleed?
A brain bleed in the subarachnoid space caused by a traumatic injury, this increases the risk of vasospasm.
What is an uncal herniation?
most common.
unilateral lesions forces uncus of temporal lobe to displace and compress on the midbrain.
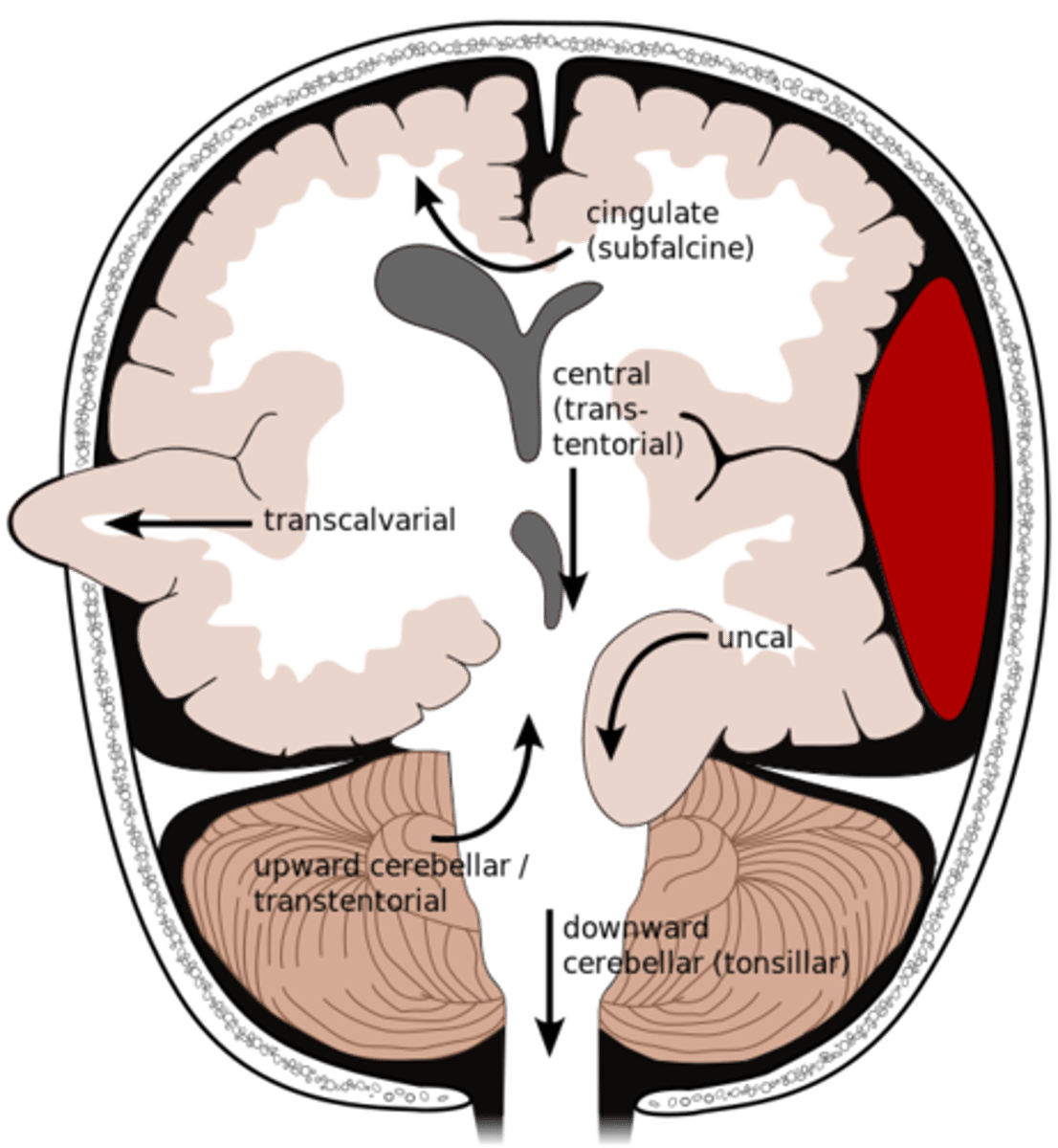
What is a central herniation?
Downward shift of cerebral hemisphere, compressing the brainstem
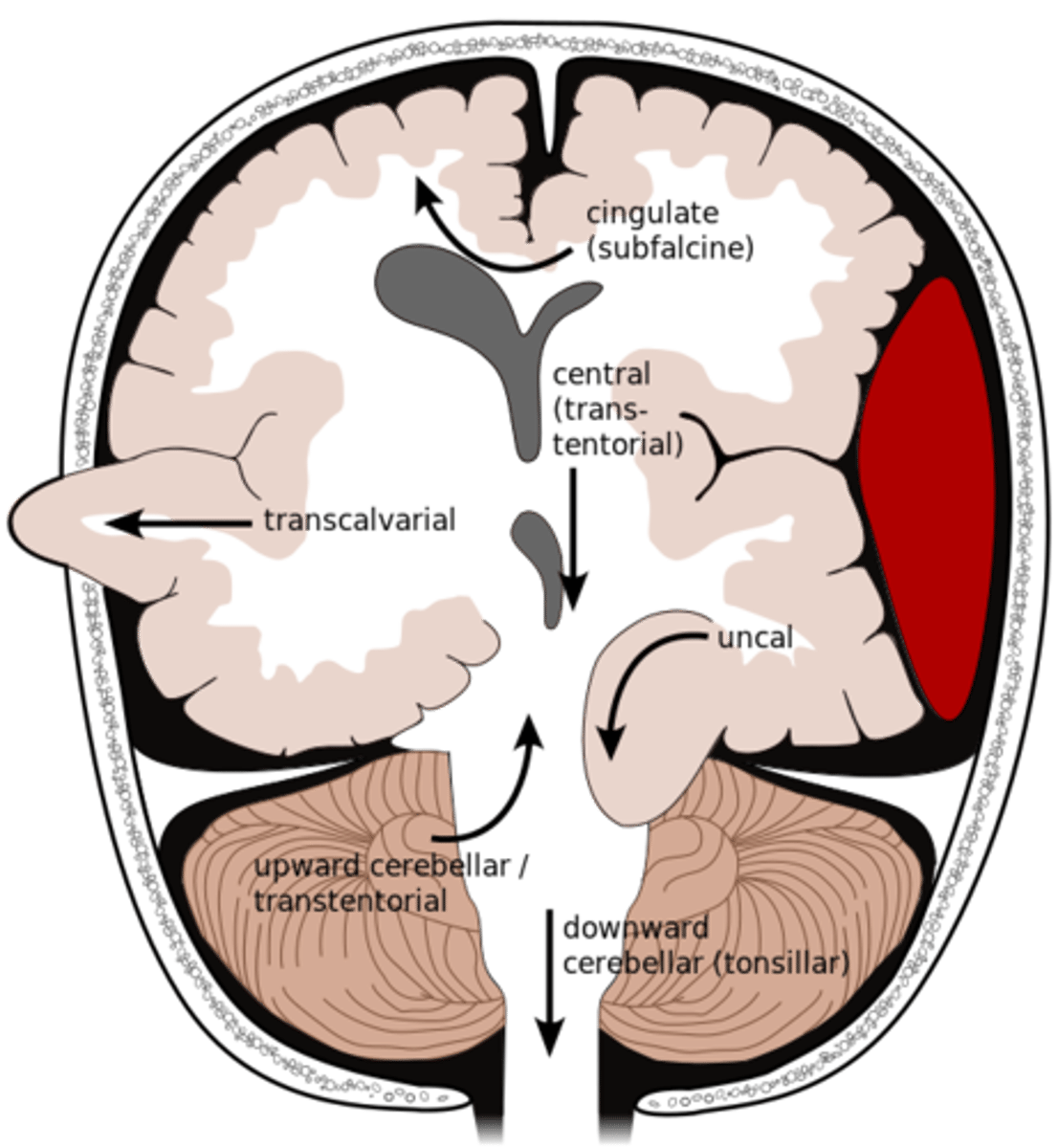
What is a cingulate herniation?
shift of brain tissue from one hemisphere to the other. Compress anterior cerebral artery.
Ischemic stroke may occur
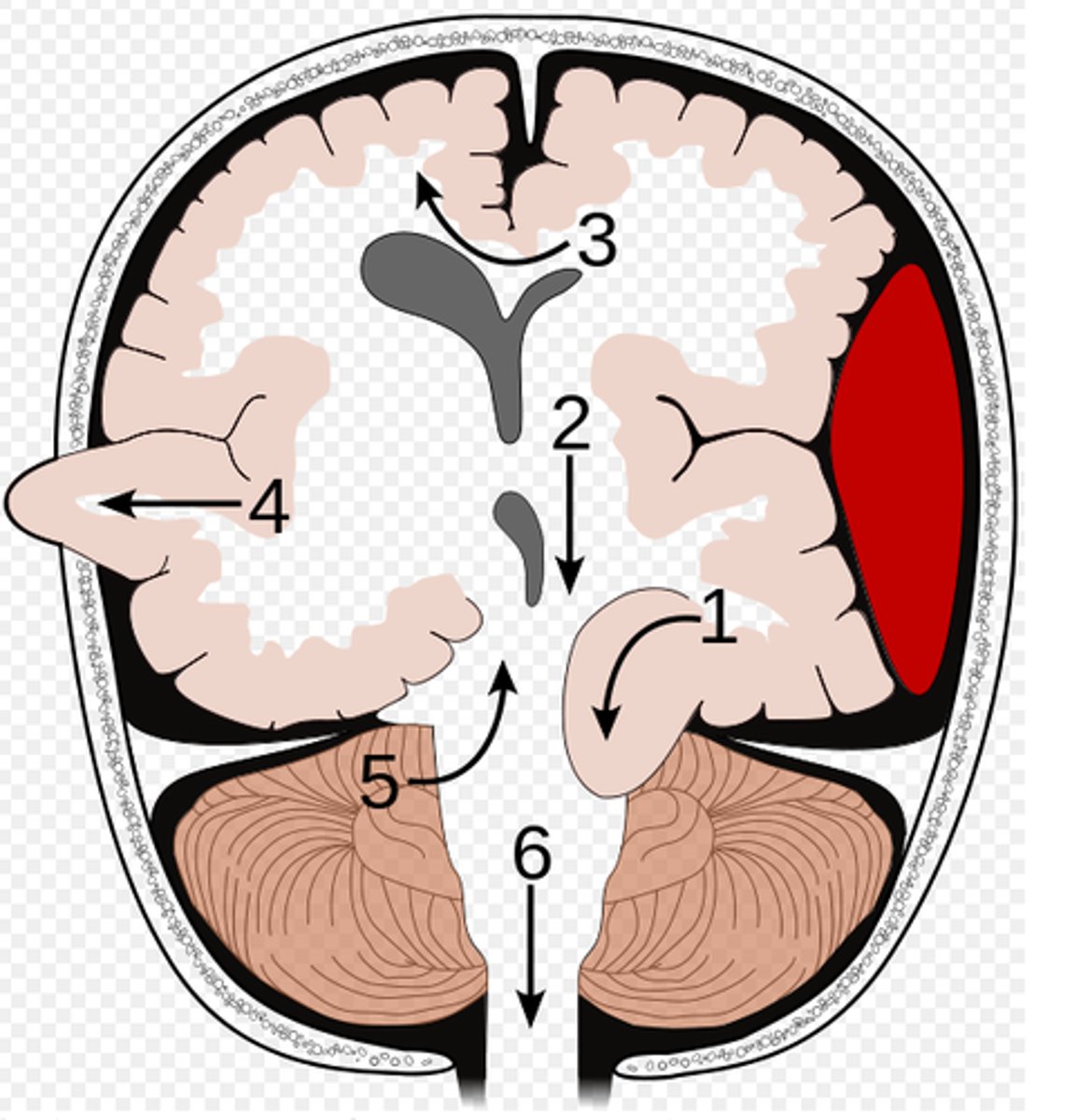
What is a transcalvarian herniation?
brain begins to herniate outside of the skull. the brain will squeeze out of fractures, burr holes, or surgical incisions.
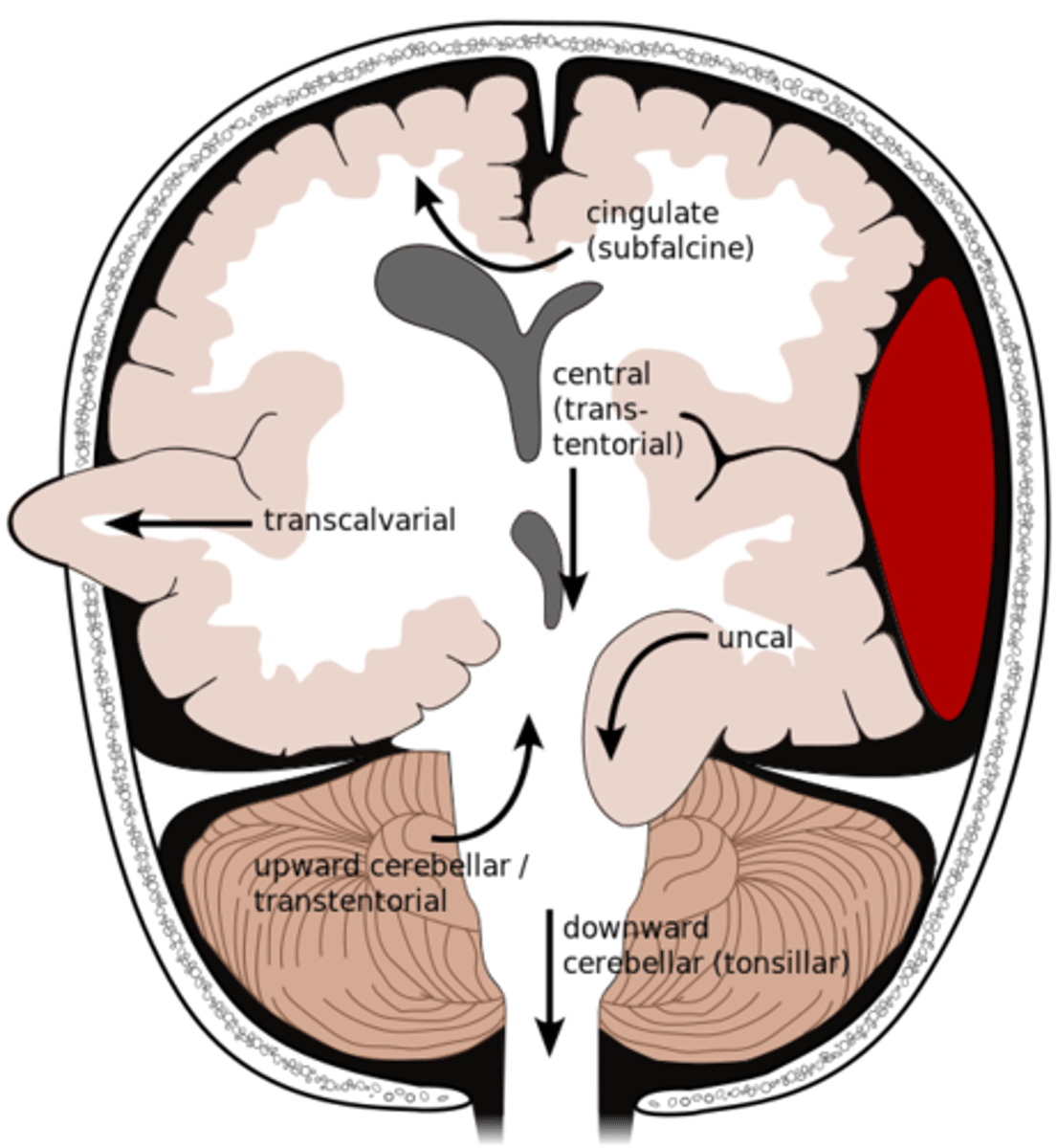
What is an upward herniation?
displacement of the cerebellum upward
What is a cerebellar Tonsillar herniation?
displacement of cerebellar tonsils downward this compressing the pons/medulla
s/s: alterations in resp. and cardiac functions- rapidly progressing to cardiac arrest, Headache and neck stiffness, reduced muscle tone
What are dolls eyes and what does it tell us?
turn patient's head side to side while eyes are open, reflex is intact if eyes move opposite direction of head, reflex is if they do not move their eyes.
What are the most concerning signs and symptoms of a closed head injury?
abnormal respiratory patterns,
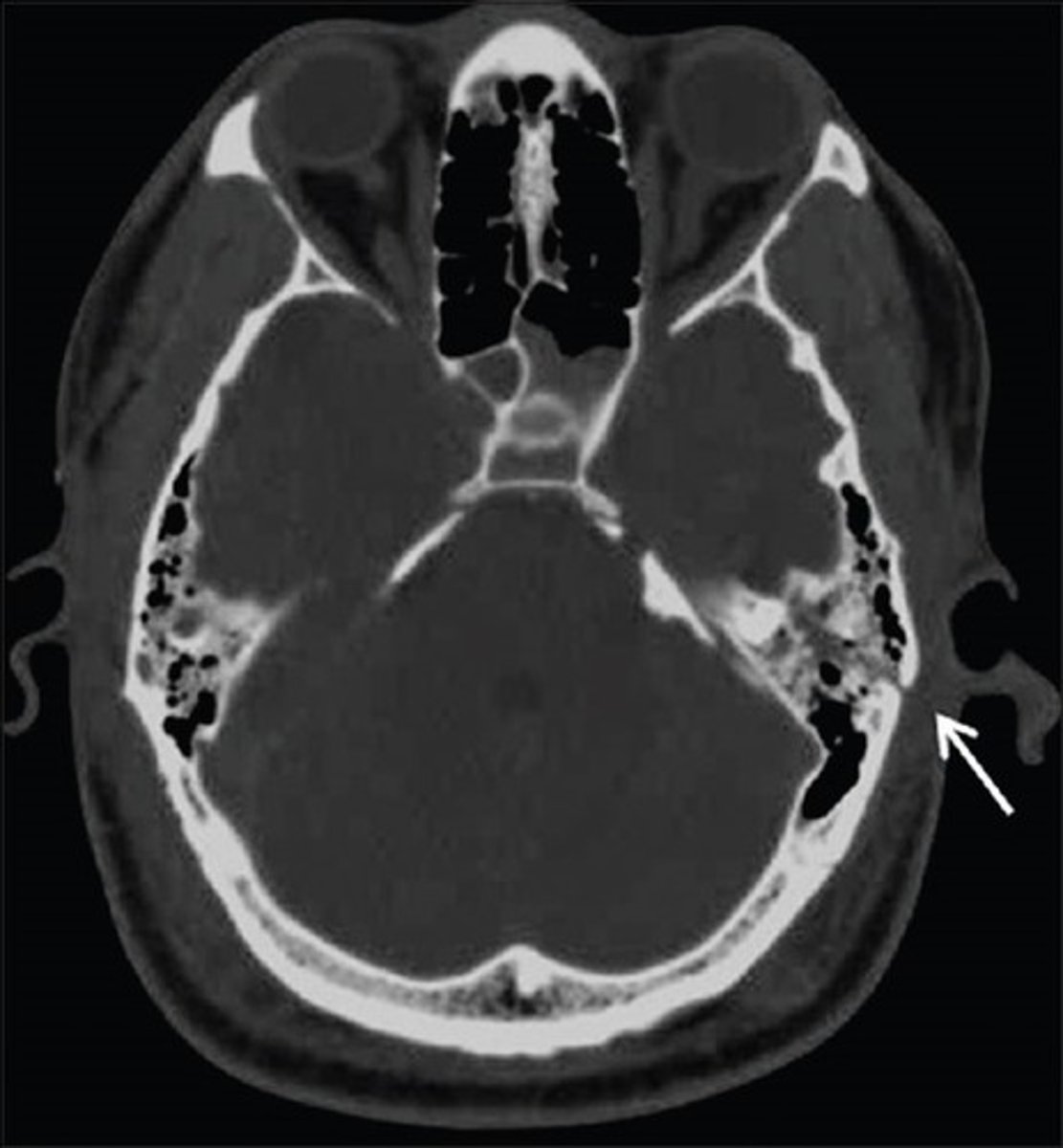
What is basilar skull fracture?
linear fracture at the base of the skull