MCB4271
0.0(0)
Card Sorting
1/137
Earn XP
Description and Tags
Last updated 4:58 AM on 12/11/22
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
138 Terms
1
New cards
Viral characteristics
- contain a signle type of nucleid acid (either RNA or DNA)
- contain a protein coat that surrounds the nucleic acid
- enveloped: the presence of an envelope makes viruses more susceptible to disinfectants. non-enveloped are highly resistant to desinfectants
- multiply inside living cells by using the synthesizing machinery of the cell.
- obligatory intracellular parasites (absolutely require host cell to replicate)
- cause the synthesis of specialized structures that can transfer the viral nucleic acid to other cells
- contain a protein coat that surrounds the nucleic acid
- enveloped: the presence of an envelope makes viruses more susceptible to disinfectants. non-enveloped are highly resistant to desinfectants
- multiply inside living cells by using the synthesizing machinery of the cell.
- obligatory intracellular parasites (absolutely require host cell to replicate)
- cause the synthesis of specialized structures that can transfer the viral nucleic acid to other cells
2
New cards
How can we kill something that does not live? how can we kill viruses?
- spikes are involved in the host recognition and attachment.
- surface proteins trigger the host immune response
- genes that coat for these surface proteins are highly susceptible to mutations, so they can change their structure often and evade the immune system.
PROBLEMS:
- not too many targets: viruses have very simple structures so there are not many targets compared to bacteria
- high replication rate= high mutation rate. this means there's a fast evolution of resistance.
- surface proteins trigger the host immune response
- genes that coat for these surface proteins are highly susceptible to mutations, so they can change their structure often and evade the immune system.
PROBLEMS:
- not too many targets: viruses have very simple structures so there are not many targets compared to bacteria
- high replication rate= high mutation rate. this means there's a fast evolution of resistance.
3
New cards
Viral replication: lytic cycle
Lytic: viral replication results in death and lysis of host cells
Lysogenic: viral DNA gets incorporated into the host genome and remains latent until activated
1. attachment: phage attaches to the host cell
2. penetration: phage penetrates host cell and injects the DNA.
3. Biosynthesis: Phage DNA directs synthesis of viral components by the host cell.
4. Maturation: viral components are assembled into virions
5. Release: host cell lyses and new virions are released.
Lysogenic: viral DNA gets incorporated into the host genome and remains latent until activated
1. attachment: phage attaches to the host cell
2. penetration: phage penetrates host cell and injects the DNA.
3. Biosynthesis: Phage DNA directs synthesis of viral components by the host cell.
4. Maturation: viral components are assembled into virions
5. Release: host cell lyses and new virions are released.
4
New cards
Common human viruses
- Hepatitis B virus
- HPV
- Human Cytomegalovirus
- Herpes Simplex Virus
- Varicella Simplex Virus
- Hepatitis C virus
- Respiratory Syncytial virus
- HPV
- Human Cytomegalovirus
- Herpes Simplex Virus
- Varicella Simplex Virus
- Hepatitis C virus
- Respiratory Syncytial virus
5
New cards
Common zoonotic viruses
- Influenza
- Human Immunodeficiency Virus
- Human Immunodeficiency Virus
6
New cards
William Prusoff
developed the first antiviral drug, iodouridine.
- he codeveloped stavudine, an antiviral against HIV
- he codeveloped stavudine, an antiviral against HIV
7
New cards
Types of antiviral drugs
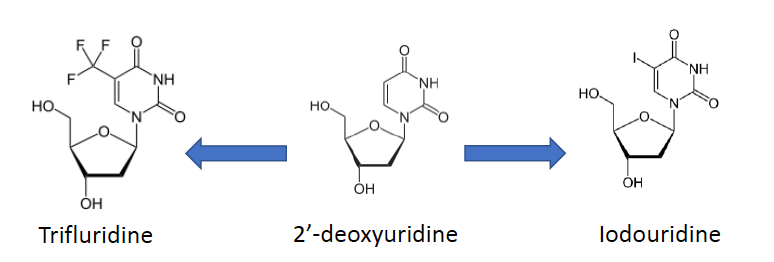
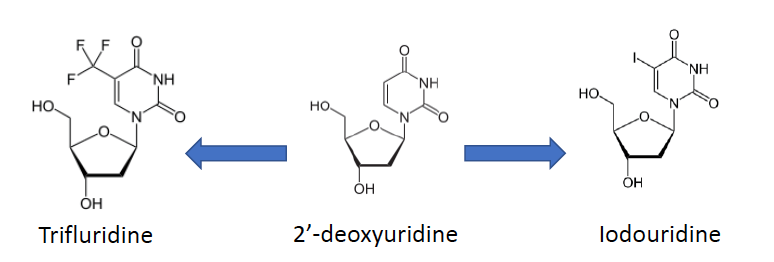
5-substituted 2'-deoxyuridines
5-substituted 2'-deoxyuridines
- Iodouridine and trifluridine are variants of deoxyuridine
- trifluridine and Iodouridine are functional analogs of 2'-deoxyuridine that get incorporated into the viral dna
- these drugs arrest base pairing which leads to viral replication inhibition
- these were first used as cancer treatments and also used against infections for HSV infection
- trifluridine and Iodouridine are functional analogs of 2'-deoxyuridine that get incorporated into the viral dna
- these drugs arrest base pairing which leads to viral replication inhibition
- these were first used as cancer treatments and also used against infections for HSV infection
8
New cards
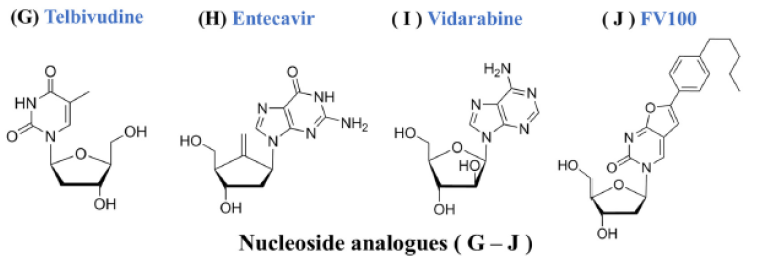
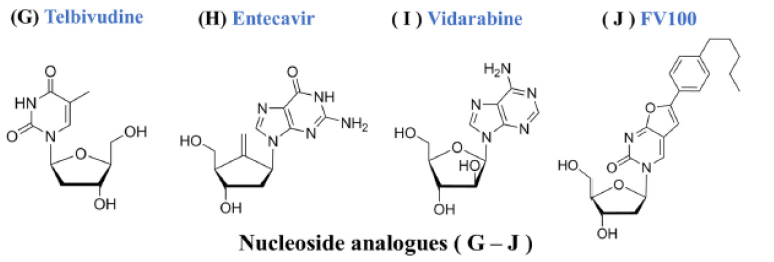
Antiviral drugs
Nucleoside and nucleotide analogs
Nucleoside and nucleotide analogs
- bind to and inhibit viral DNA
- originally developed as cancer treatments
- Telbivudine, Entecavir, Vidarabine and FV100
9
New cards
Antiviral drugs
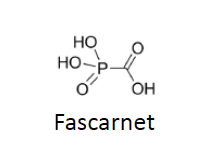
Pyrophosphate analogs
Pyrophosphate analogs
- one example is Fascarnet
- they have broad-spectrum activity against many viruses and they target viral DNA polymerases
- Fascarnet reversibly binds to the pyrophosphate binding site of the viral DNA
- they have broad-spectrum activity against many viruses and they target viral DNA polymerases
- Fascarnet reversibly binds to the pyrophosphate binding site of the viral DNA
10
New cards
Antiviral drugs
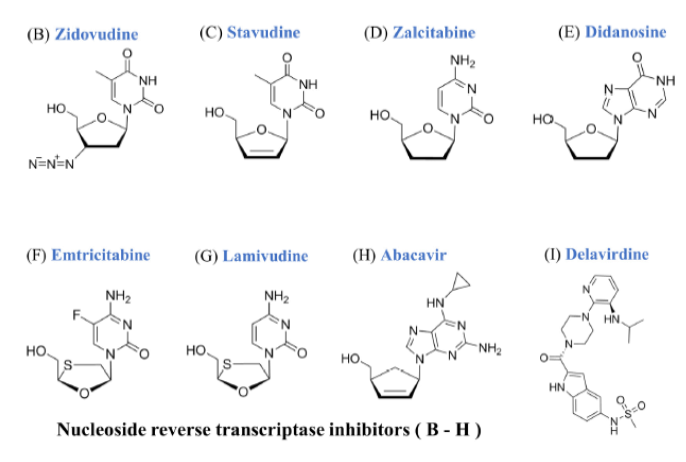
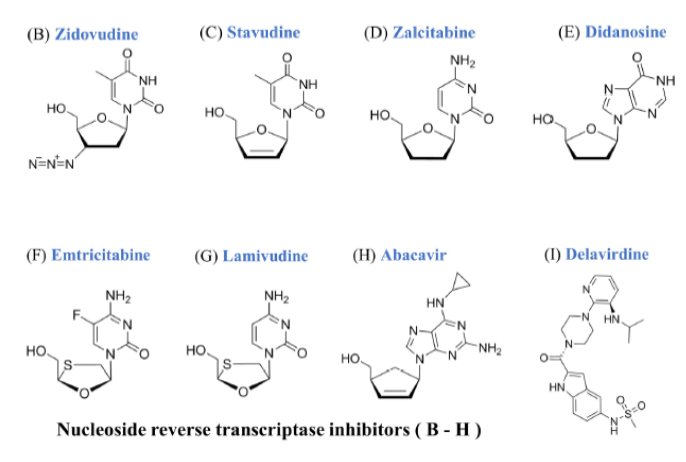
Nucleoside reverse transcriptase inhibitors (NRTIs)
Nucleoside reverse transcriptase inhibitors (NRTIs)
- target HIV and HBV reverse transcriptase
- NRTIs need to be phosphorylated to 5'- triphosphate
- act as chain terminators
- target and inhibit reverse transcriptases of RNA
- NRTIs need to be phosphorylated to 5'- triphosphate
- act as chain terminators
- target and inhibit reverse transcriptases of RNA
11
New cards
Antiviral drugs
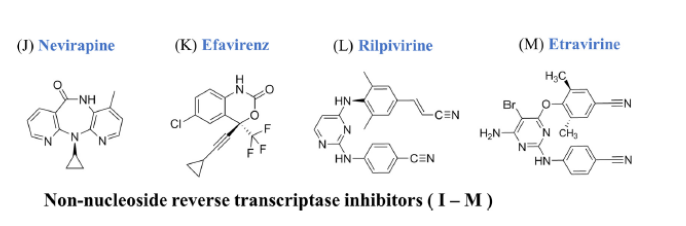
Nonnucleoside reverse transcriptase inhibitors
Nonnucleoside reverse transcriptase inhibitors
- Anti-HIV-1. does not work for HIV-2 (HIV-2 is a less virulent strain found mainly in Africa. doesn't work because the reverse transcriptase of HIV-1 is different than that of HIV-2.
- targets HIV-1 reverse transcriptase
- bind near the RT catalytic site and induce conformational changes that inhibit RT function
- targets HIV-1 reverse transcriptase
- bind near the RT catalytic site and induce conformational changes that inhibit RT function
12
New cards
Antiviral drugs
Protease inhibitors (PIs)
Protease inhibitors (PIs)
- HIV -targeting
-HCV targeting
- PIs have peptide-like scaffolds that allow them to bind to viral proteases and mimic the actual substrate as a result inhibiting the function of viral proteases
- they are administered with other drugs that enhance bioavailability and stability.
-HCV targeting
- PIs have peptide-like scaffolds that allow them to bind to viral proteases and mimic the actual substrate as a result inhibiting the function of viral proteases
- they are administered with other drugs that enhance bioavailability and stability.
13
New cards
Antiviral drugs
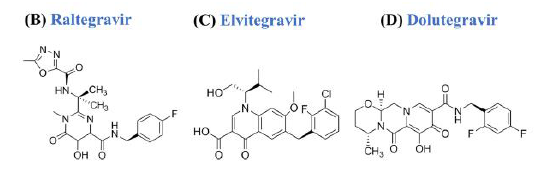
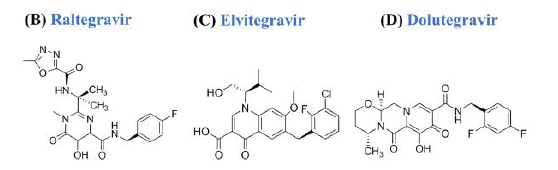
Integrase inhibitors
Integrase inhibitors
- viral integrases insert viral DNA into the host genome of the host
- integrase inhibitors bind to the catalytic site of HIV integrase and prevent the incorporation of the viral DNA into the host genome
- integrase inhibitors are much more effective than NRTIs and PIs.
- block insertion of HIV DNA. into CD4 cell DNA
note about elvitegravir: it looks similar to tetracycline, some may say that tetracycline derivatives exhibit inhibitory effects on viral integrases.
- integrase inhibitors bind to the catalytic site of HIV integrase and prevent the incorporation of the viral DNA into the host genome
- integrase inhibitors are much more effective than NRTIs and PIs.
- block insertion of HIV DNA. into CD4 cell DNA
note about elvitegravir: it looks similar to tetracycline, some may say that tetracycline derivatives exhibit inhibitory effects on viral integrases.
14
New cards
Antiviral drugs
Entry inhibitors
Entry inhibitors
target...
- membrane fusion
- endocytosis
- genetic injection
- membrane fusion
- endocytosis
- genetic injection
15
New cards
Entry inhibitors examples (4 classes)
- Biomimetic peptides (Enfuvirtide)
- Receptor antagonists (Maraviroc)
- Neutralizing antibodies (Palivizumab)
- Broad lipid-enveloped virus entry inhibitor (Doconasol)
- Receptor antagonists (Maraviroc)
- Neutralizing antibodies (Palivizumab)
- Broad lipid-enveloped virus entry inhibitor (Doconasol)
16
New cards
Biomimetic peptides
- Enfuvirtide
- blocks virus-host membrane fusion
- blocks virus-host membrane fusion
17
New cards
Receptor antagonists
- Maraviroc
- blocks host cell surface receptors that interact with viral particles prior to entry
- this is necessary for the proper internalization of a viral particle.
- blocks host cell surface receptors that interact with viral particles prior to entry
- this is necessary for the proper internalization of a viral particle.
18
New cards
Neutralizing antobodies
- Palivizumab
- block viral receptor and prevent anchoring to the host cell
- block viral receptor and prevent anchoring to the host cell
19
New cards
Broad lipid-enveloped virus entry inhibitor
- Docosanol
- thought to interact with epithelial cell surface receptors
- this prevents viral entry
- it's the only OTC medication for cold sores and fever blisters
- thought to interact with epithelial cell surface receptors
- this prevents viral entry
- it's the only OTC medication for cold sores and fever blisters
20
New cards
Antiviral Drugs
Acyclic guanosine analogues
Acyclic guanosine analogues
- inhibitor of the viral DNA polymerase
- some are phosphorylated by host kinases while other are phosphorylated by viral thymidine kinase.
- once phosphorylated, they compete with the endogenous dGTP to bind to and inhibit viral DNA polymerase
- these are all prodrugs. their activation is accomplished by phosphorylation by either host or viral kinases
- some are phosphorylated by host kinases while other are phosphorylated by viral thymidine kinase.
- once phosphorylated, they compete with the endogenous dGTP to bind to and inhibit viral DNA polymerase
- these are all prodrugs. their activation is accomplished by phosphorylation by either host or viral kinases
21
New cards
Antiviral drugs
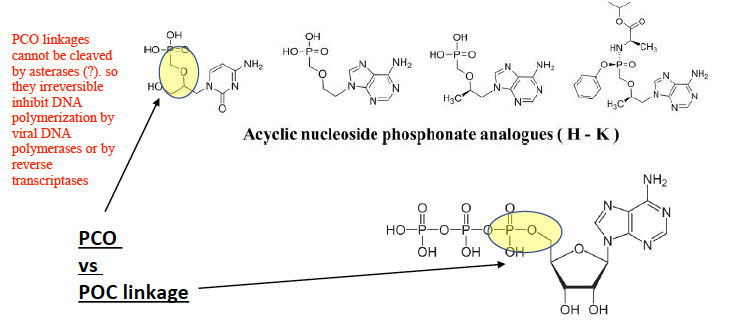
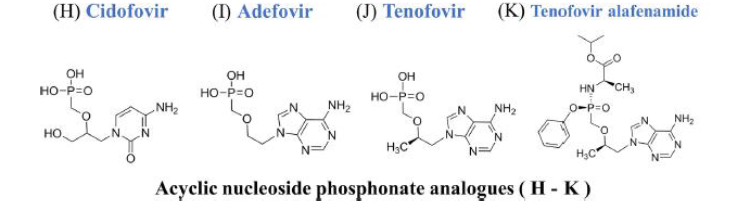
Acyclic nucleoside phosphonate (ANP) analogues
Acyclic nucleoside phosphonate (ANP) analogues
- inhibit viral DNA polymerases and reverse transcriptases
- their mechanism of action is dependent on phosphate linkages
- PCO linkages cannot be cleaved by asterases, so they irreversibly inhibit DNA polymerization by viral DNA polymerases or by reverse transcriptases
- PCO linkage vs. POC linkage
- their mechanism of action is dependent on phosphate linkages
- PCO linkages cannot be cleaved by asterases, so they irreversibly inhibit DNA polymerization by viral DNA polymerases or by reverse transcriptases
- PCO linkage vs. POC linkage
22
New cards
Antiviral drugs
HCV NS 5A/NS 5B inhibitors
HCV NS 5A/NS 5B inhibitors
NS5A: essential for HCV genome replications
NS5B: HCV RNA polymerase
- a combination of NS5A and B inhibitors completely cures patients infected with certain HCV genotypes.
- mechanism of action of HCVNS5A is not understood. we just know that it blocks viral RNA replication
NS5B: HCV RNA polymerase
- a combination of NS5A and B inhibitors completely cures patients infected with certain HCV genotypes.
- mechanism of action of HCVNS5A is not understood. we just know that it blocks viral RNA replication
23
New cards
Antiviral drugs
Influenza virus inhibitors
Influenza virus inhibitors
- Matrix 2 inhibitors (amantadine and rimantadine)
- Amantadine - 1st anti-influenza A drug approved
- Amantadine blocks proton transport through the Matrix 2 (M2) ion channels into the interior of viral particles, a process that is essential for viral uncoating within the endosomes.
- Amantadine is only effective in adults (not children or elderly)
- Neuraminidase inhibitors inhibit viral replication. Neuraminidase are enzymes required for viral release from the host cell. drugs that target neuraminidases inhibit viral replication
- Polymerase inhibitors
- Inhibition of GTP biogenesis
- Amantadine - 1st anti-influenza A drug approved
- Amantadine blocks proton transport through the Matrix 2 (M2) ion channels into the interior of viral particles, a process that is essential for viral uncoating within the endosomes.
- Amantadine is only effective in adults (not children or elderly)
- Neuraminidase inhibitors inhibit viral replication. Neuraminidase are enzymes required for viral release from the host cell. drugs that target neuraminidases inhibit viral replication
- Polymerase inhibitors
- Inhibition of GTP biogenesis
24
New cards
Development of antiviral drug resistance
if an antiviral is 50% effective, it will almost certainly lead to the selection and expansion of a resistant population.
25
New cards
Antiviral drug resistance
5-substituted 2'- deoxyuridines
5-substituted 2'- deoxyuridines
- first antiviral drug was Iodouridine
- no mechanisms of resistance in clinical settings
(iodouridine is a non-functional analog of 2' deoxyuridine that inhibits base pairing, iodouridine and trifluridine are effective antivirals and no mechanisms of resistance were detected in clinical settings.
- no mechanisms of resistance in clinical settings
(iodouridine is a non-functional analog of 2' deoxyuridine that inhibits base pairing, iodouridine and trifluridine are effective antivirals and no mechanisms of resistance were detected in clinical settings.
26
New cards
Antiviral drug resistance
Nucleoside and nucleotide analogs
Nucleoside and nucleotide analogs
mechanism of resistance: drug-target modification: amino acid substitutions
27
New cards
Antiviral Drug resistance
Nucleoside reverse transcriptase inhibitors (NRTIs)
Nucleoside reverse transcriptase inhibitors (NRTIs)
mechanism of resistance: drug-target modification: amino acid substitutions
- this abolishes their binding to a reverse transcriptase enzyme
- one viral advantage is that reverse transcriptase has a very poor proofreading activity, so these enzymes allow the introduction of random mutations into other viral proteins which create a high variability in protein sequences.
(usually target HIV reverse transcriptase and act as chain terminators).
- this abolishes their binding to a reverse transcriptase enzyme
- one viral advantage is that reverse transcriptase has a very poor proofreading activity, so these enzymes allow the introduction of random mutations into other viral proteins which create a high variability in protein sequences.
(usually target HIV reverse transcriptase and act as chain terminators).
28
New cards
Antiviral drug resistance
Nonnucleoside reverse transcriptase inhibitors (NNRTIs)
Nonnucleoside reverse transcriptase inhibitors (NNRTIs)
mechanism of resistance: drug-target-modification: amino acid substitutions
( usually are anti-HIV-1 only and target HIV-1 reverse transcriptase. bind near the RT catalytic site and induce conformational changes that inhibit RT function).
( usually are anti-HIV-1 only and target HIV-1 reverse transcriptase. bind near the RT catalytic site and induce conformational changes that inhibit RT function).
29
New cards
Antiviral Drug Resistance
Protease Inhibitors (PIs)
Protease Inhibitors (PIs)
mechanism of resistance: drug-target modification: amino acid substitutions
high risk for developing resistance
primary mutation: mild, followed by a strong secondary mutation. primary mutations only minimally contribute to resistance. during continous PI therapy, secondary mutations arise and lead to stronger resistance.
(usually are HIV-targeting and HCV-targeting. they have peptide-like scaffolds that allow them to bind to viral proteases and mimic the actual substrate, which inhibits the function of viral proteases)
high risk for developing resistance
primary mutation: mild, followed by a strong secondary mutation. primary mutations only minimally contribute to resistance. during continous PI therapy, secondary mutations arise and lead to stronger resistance.
(usually are HIV-targeting and HCV-targeting. they have peptide-like scaffolds that allow them to bind to viral proteases and mimic the actual substrate, which inhibits the function of viral proteases)
30
New cards
Antiviral drug resistance
Integrase inhibitors
Integrase inhibitors
mechanism of resistance: drug-target modification: amino acid substitutions
viruses have developed resistance to almost all of these 3 drugs by introducing resistant mutations
viruses have developed resistance to almost all of these 3 drugs by introducing resistant mutations
31
New cards
Antiviral drug resistance
Entry inhibitors
Entry inhibitors
Mechanism of resistance: drug-target modification: amino acid substitution
all the mechanisms of resistance against viral drugs rely on target modification and all of these are amino acid substitutions with the exception of docosanol (no resistance as of today)
(usually target membrane fusion, endocytosis, and genetic injection. they can be...
- biomimetic peptides
- receptor antagonists
- neutralizing antibodies
- broad lipid-enveloped virus entry inhibitors)
all the mechanisms of resistance against viral drugs rely on target modification and all of these are amino acid substitutions with the exception of docosanol (no resistance as of today)
(usually target membrane fusion, endocytosis, and genetic injection. they can be...
- biomimetic peptides
- receptor antagonists
- neutralizing antibodies
- broad lipid-enveloped virus entry inhibitors)
32
New cards
Antiviral drug resistance
Acyclic guanosine analogues
Acyclic guanosine analogues
mechanism of resistance: drug-target modification: amino acid substitutions.
(usually inhibit viral DNA polymerase. some are phosphorylated by host kinases. others are phosphorylated by viral thymidine kinases. once phosphorylated, they compete with the endogenous dGTP to bind to and inhibit viral DNA polymerase)
(usually inhibit viral DNA polymerase. some are phosphorylated by host kinases. others are phosphorylated by viral thymidine kinases. once phosphorylated, they compete with the endogenous dGTP to bind to and inhibit viral DNA polymerase)
33
New cards
Antiviral drug resistance
Acyclic nucleoside phosphonate (ANP) analogues
Acyclic nucleoside phosphonate (ANP) analogues
mechanism of resistance:
- drug-target modification: amino acid substitutions
- DNA polymerase mutations reduce viral fitness (this gives the immune system the advantage to kick in and target the infection)
(usually inhibit DNA polymerases and reverse transcriptases. mutations in viral DNA polymerases and RT always cause resistance to multiple drugs)
- drug-target modification: amino acid substitutions
- DNA polymerase mutations reduce viral fitness (this gives the immune system the advantage to kick in and target the infection)
(usually inhibit DNA polymerases and reverse transcriptases. mutations in viral DNA polymerases and RT always cause resistance to multiple drugs)
34
New cards
Antiviral drugs
HCV NS 5A/NS 5B inhibitors
HCV NS 5A/NS 5B inhibitors
mechanism of resistance:
- drug-target modification: amino acid substitutions
- DNA polymerase mutations reduce viral fitness
(this antiviral drug is usually essential for HCV genome replications. this other antiviral drug is important for HCV RNA polymerase. a combination of these two drugs completely cures patients infected with certain HCV genotypes)
- drug-target modification: amino acid substitutions
- DNA polymerase mutations reduce viral fitness
(this antiviral drug is usually essential for HCV genome replications. this other antiviral drug is important for HCV RNA polymerase. a combination of these two drugs completely cures patients infected with certain HCV genotypes)
35
New cards
Antiviral drug resistance
Influenza virus inhibitors
Influenza virus inhibitors
mechanism of resistance:
- drug-target modification: amino acid substitutions
- DNA polymerase mutations reduce viral fitness
- only a single amino acid substitution results in the M2 proton channel having 90% resistance to both inhibitors.
(usually one of these antivirals blocks proton transport through the Matrix2 ion channels into the interior of viral particles, a process that is essential for viral uncoating within the endosomes. this is effective only in adults.
usually one of these antivirals inhibits viral replication)
- drug-target modification: amino acid substitutions
- DNA polymerase mutations reduce viral fitness
- only a single amino acid substitution results in the M2 proton channel having 90% resistance to both inhibitors.
(usually one of these antivirals blocks proton transport through the Matrix2 ion channels into the interior of viral particles, a process that is essential for viral uncoating within the endosomes. this is effective only in adults.
usually one of these antivirals inhibits viral replication)
36
New cards
Strategic National Stockpile
- done by the ASPR (Assistant Secretary for Preparedness and Response)
- stockpiles contain millions of antivirals, antibiotics and vaccines.
- they are hidden in secret warehouses scattered throughout the country.
- there are 6 stockpiles locations.
- inventory is estimated at $7 billion of medications and emergency supply equipment
- stockpiles contain millions of antivirals, antibiotics and vaccines.
- they are hidden in secret warehouses scattered throughout the country.
- there are 6 stockpiles locations.
- inventory is estimated at $7 billion of medications and emergency supply equipment
37
New cards
Types of fungi
(Yeast vs. Mold vs. Dimorphic)
(Yeast vs. Mold vs. Dimorphic)
Yeast
- single cells
- can be pathogenic
Mold (mycelium)
- Hyphae (branching filaments)
- can be pathogenic
Dimorphic
- they can switch back and forth between mold and yeast
- single cells
- can be pathogenic
Mold (mycelium)
- Hyphae (branching filaments)
- can be pathogenic
Dimorphic
- they can switch back and forth between mold and yeast
38
New cards
Temperature-mediated fungal dimorphism
- a body temperature of 37C selects for yeast morphology
- pathogenic fungi can be dimorphic
- they can switch from mycelial to yeast form and this is temperature-dependent (once it reaches 37C).
- dimorphism is used for rapid identification of infections
- pathogenic fungi can be dimorphic
- they can switch from mycelial to yeast form and this is temperature-dependent (once it reaches 37C).
- dimorphism is used for rapid identification of infections
39
New cards
Fungal virulence mechanisms
Allergic immune responses (hypersensitivities)
- environmental fungi
- asthma
Toxic production
- aflatoxins (produced by Aspergillus flavus) are linked to the development of liver cancer. this fungus is common in hot and humid climates. it's a decomposer.
Mycoses
- host infection
- environmental fungi
- asthma
Toxic production
- aflatoxins (produced by Aspergillus flavus) are linked to the development of liver cancer. this fungus is common in hot and humid climates. it's a decomposer.
Mycoses
- host infection
40
New cards
Types of mycoses
Superficial mycoses: skin layer, hair, nail
Subcutaneous: deep tissue
Systemic:
- internal organs (most dangerous type)
- primary (can affect healthy individuals)
- secondary (opportunistic. develops when the immune system is compromised. antibiotics do this because they kill the bad bacteria but also good microbiota)
*studies have found a relationship between antibiotic use and fungal infections*
*each fungus causes a specific type of infection*
Subcutaneous: deep tissue
Systemic:
- internal organs (most dangerous type)
- primary (can affect healthy individuals)
- secondary (opportunistic. develops when the immune system is compromised. antibiotics do this because they kill the bad bacteria but also good microbiota)
*studies have found a relationship between antibiotic use and fungal infections*
*each fungus causes a specific type of infection*
41
New cards
Superficial mycoses
- most common
- easily transmissible: contact with contaminated surfaces
- recurrent and persistent
- not a serious health threat
- treated with topical anti-fungal agents (often OTC)
- they can infect anyone despite the status of their immune system.
- easily transmissible: contact with contaminated surfaces
- recurrent and persistent
- not a serious health threat
- treated with topical anti-fungal agents (often OTC)
- they can infect anyone despite the status of their immune system.
42
New cards
Subcutaneous mycoses
- high rates among specific occupations that are in contact with soil: (agricultural workers, miners, gardeners)
- an example is Sporotrichosis or Rose-gardener's disease. Sporotrichosis can enter the body through a cut in the skin. it's found in leaves and wood. it decomposes organic matter
- treated with oral anti-fungal like Azoles (ketoconazole and fluconazole)
- an example is Sporotrichosis or Rose-gardener's disease. Sporotrichosis can enter the body through a cut in the skin. it's found in leaves and wood. it decomposes organic matter
- treated with oral anti-fungal like Azoles (ketoconazole and fluconazole)
43
New cards
Systemic mycoses
- most often acquired in the environment
3 major systemic mycoses:
- Histoplasmosis
- Coccidioidomycosis (Valley Fever)
- Blastomycosis
- these 3 mycoses are found in the environment and mainly affect immunocompromised individuals
3 major systemic mycoses:
- Histoplasmosis
- Coccidioidomycosis (Valley Fever)
- Blastomycosis
- these 3 mycoses are found in the environment and mainly affect immunocompromised individuals
44
New cards
Histoplasmosis
- most common mycosis
- associated with rural areas
- can cause lung infections. once the fungus is in the lung it can spread to other organs
- spores found in bird and bat dropping
- common in the Mississippi and Ohio River valleys
- healthy individuals do not get infected
- effective treatments are available. fatal if not treated
- associated with rural areas
- can cause lung infections. once the fungus is in the lung it can spread to other organs
- spores found in bird and bat dropping
- common in the Mississippi and Ohio River valleys
- healthy individuals do not get infected
- effective treatments are available. fatal if not treated
45
New cards
Coccidioidomycosis (Valley fever)
- spores found in soil (most common in the SW of the US)
- impossible to prevent infection in areas of high risk because spores spread easily through the air
- healthy individuals do not get infected
- impossible to prevent infection in areas of high risk because spores spread easily through the air
- healthy individuals do not get infected
46
New cards
blastomycosis
- least common mycosis
- found in most soil and in decomposing wood and leaves
- spores are ubiquitously found in moist soil and on decomposing wood and leaves
- healthy individuals do not get infected
- found in most soil and in decomposing wood and leaves
- spores are ubiquitously found in moist soil and on decomposing wood and leaves
- healthy individuals do not get infected
47
New cards
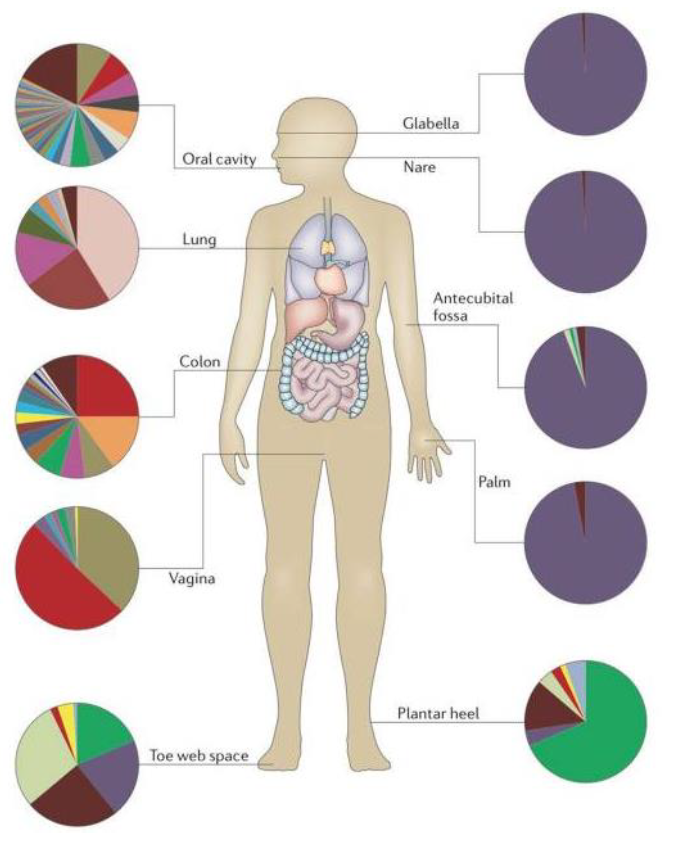
Human mycobiota
even though most are commensal fungi, some of them are opportunistic pathogens because they are associated with diseases
- candida is the most abundant fungi in the body
- candida is the most common cause of hospital-acquired bloodstream infections
- penicillin also makes up to 20% of samples
- candida is the most abundant fungi in the body
- candida is the most common cause of hospital-acquired bloodstream infections
- penicillin also makes up to 20% of samples
48
New cards
Candida spp.
almost all fungal infections are caused by opportunistic pathogens
- deadly, drug-resistant Candida yeast infection spreads in the US
- 53 people were infected in NY and 27 people were infected in other states
- all of the cases were HAI and all the patients had serious medical conditions
- 98% isolates were resistant to fluconazole (most common anti-fungal
- 1/3 of isolates were resistant to 2 anti-fungals and some strains were resistant to all anti-fungals
- nearly half the patients died within 3 months of the diagnosis
- this strain is very virulent and drug-resistant
- deadly, drug-resistant Candida yeast infection spreads in the US
- 53 people were infected in NY and 27 people were infected in other states
- all of the cases were HAI and all the patients had serious medical conditions
- 98% isolates were resistant to fluconazole (most common anti-fungal
- 1/3 of isolates were resistant to 2 anti-fungals and some strains were resistant to all anti-fungals
- nearly half the patients died within 3 months of the diagnosis
- this strain is very virulent and drug-resistant
49
New cards
CDC closely monitors C. auris infections
outbreaks in Illinois, New Jeersey and New York. hospitals have been getting shut down to control the outbreaks
50
New cards
Characteristics of Candida auris
- Emerging MDR yeast (some strains are pan-resistant)
- high mortality
- can indefinitely colonize patients' skin
- can survive in the environment for extended periods of time
- resistant to certain disinfectants
- easily disseminated
- associated with extended hospital stays and recent use of antibiotics/antivirals
- high mortality
- can indefinitely colonize patients' skin
- can survive in the environment for extended periods of time
- resistant to certain disinfectants
- easily disseminated
- associated with extended hospital stays and recent use of antibiotics/antivirals
51
New cards
What fueled fungal drug resistance?
1960s --> introduction of birth control led to increase in STDs, especially HIV and AIDS
1970s --> evolution of immunosuppressive medications contributed to an increase in fungal infections & resistanc
1980s --> the AIDS epidemic contributed to an increase in fungal infections because more people were immunosuppressed.
1970s --> evolution of immunosuppressive medications contributed to an increase in fungal infections & resistanc
1980s --> the AIDS epidemic contributed to an increase in fungal infections because more people were immunosuppressed.
52
New cards
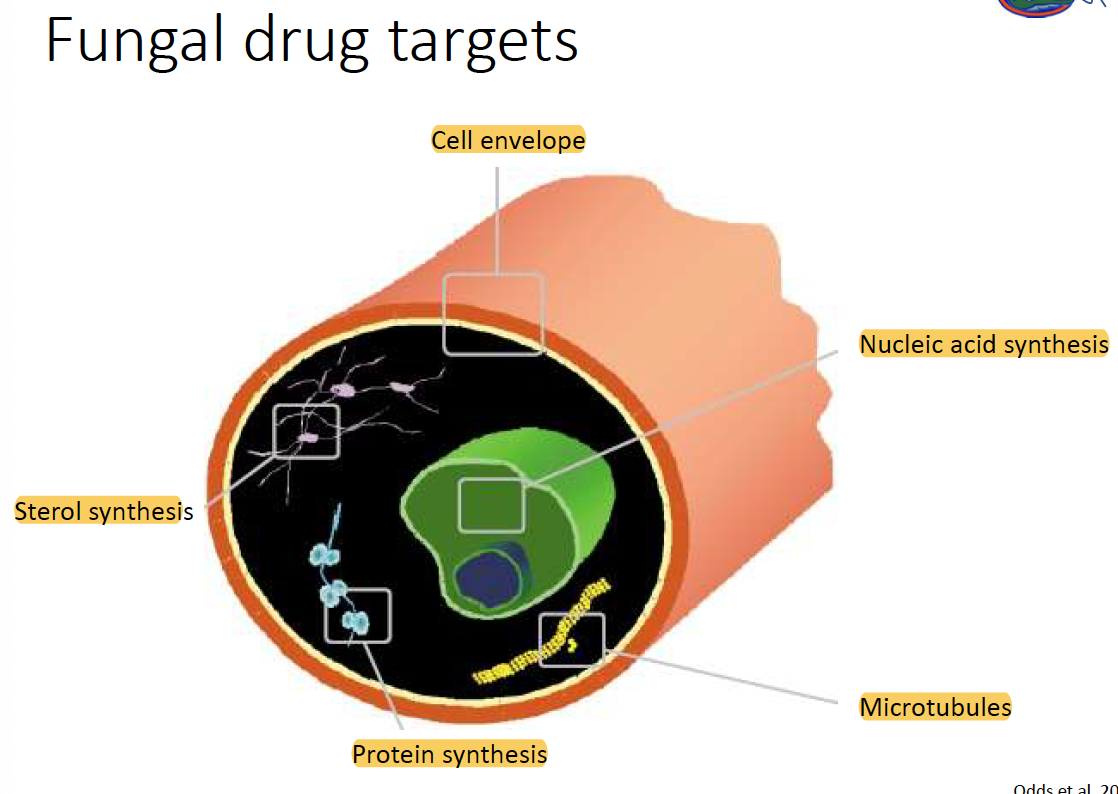
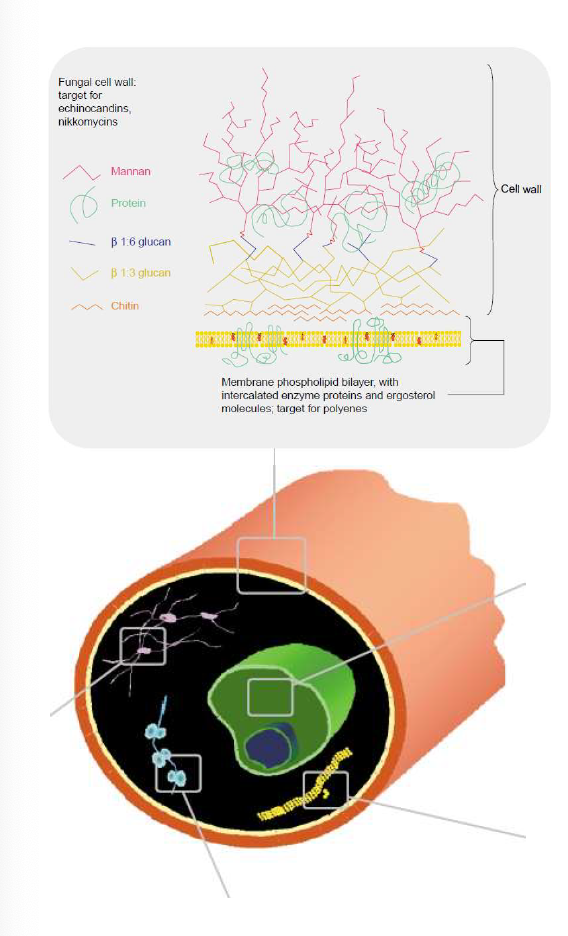
Fungal drug targets
- cell envelope
- nucleic acid synthesis
- sterol synthesis
- protein synthesis
- microtubules
- nucleic acid synthesis
- sterol synthesis
- protein synthesis
- microtubules
53
New cards
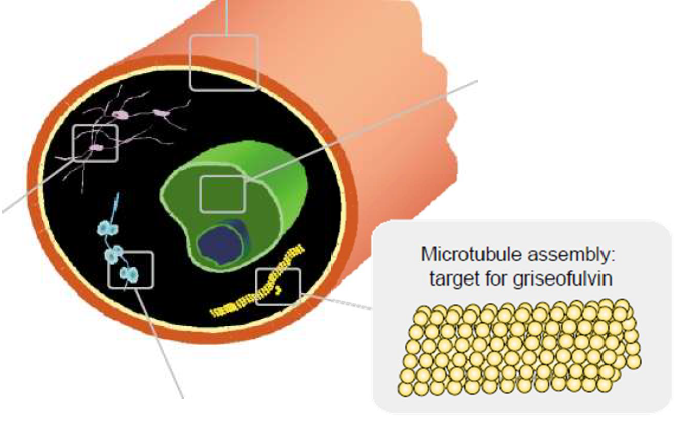
Antifungal drug: griseofulvin
- inhibits microtubule assembly
- mechansim remains unknown
- fungistatic
restricted to dermatophyte fungi: ringworm and athlete's foot
Resistance: decrease in energy-dependent drug intake
- mechansim remains unknown
- fungistatic
restricted to dermatophyte fungi: ringworm and athlete's foot
Resistance: decrease in energy-dependent drug intake
54
New cards
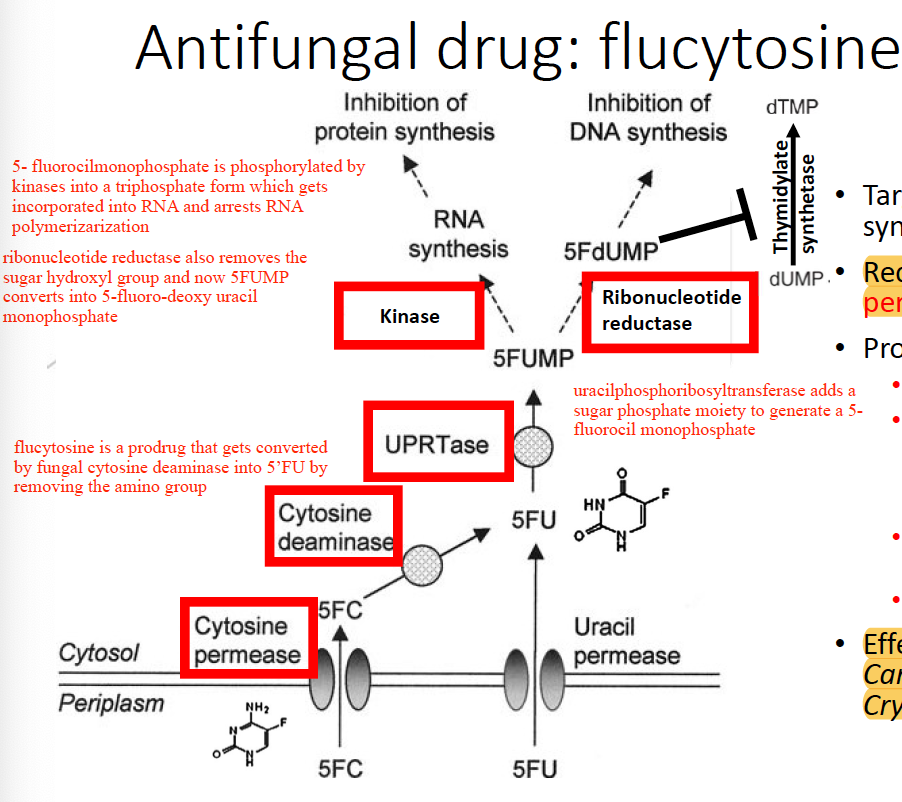
Antifungal drug: flucytosine
- targets nucleic acid synthesis
- REQUIRES cytosine permease for uptake. take into cell.
- effective against yeast Candida and Cryptococcus spp
- used in combination with other antifungals
- fungi rapidly develop resistance against flucytosine
prodrug that REQUIRES:
- cytosine deaminase
- uracil phosphoribosyl transferase (UPRTase)
- ribonucleotide reductase
- kinase
- for flucytosine to be effective it must have CYTOSINE PERMEASE and CYTOSINE DEAMINASE.
- REQUIRES cytosine permease for uptake. take into cell.
- effective against yeast Candida and Cryptococcus spp
- used in combination with other antifungals
- fungi rapidly develop resistance against flucytosine
prodrug that REQUIRES:
- cytosine deaminase
- uracil phosphoribosyl transferase (UPRTase)
- ribonucleotide reductase
- kinase
- for flucytosine to be effective it must have CYTOSINE PERMEASE and CYTOSINE DEAMINASE.
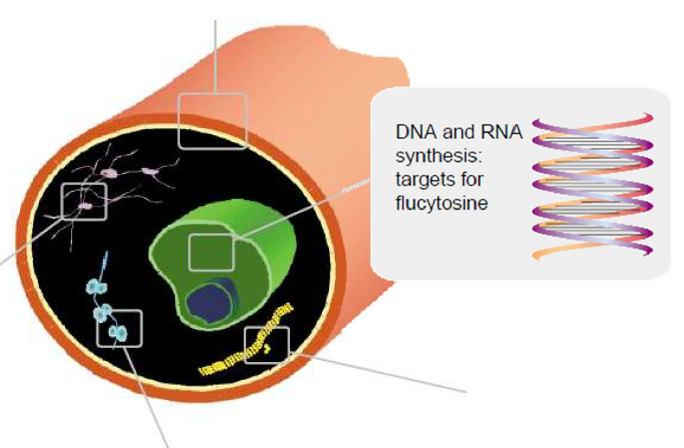
55
New cards
flucytosine mechanism of action
56
New cards
how can fungi develop resistance against flucytosine?
- loss of permease activity
- increased synthesis of pyrimidines which compete with flucytosine metabolic products
- defective deaminase or defective UPRTase (deaminase and uracil phosphoribosyltransferase are not essential proteins)
- increased synthesis of pyrimidines which compete with flucytosine metabolic products
- defective deaminase or defective UPRTase (deaminase and uracil phosphoribosyltransferase are not essential proteins)
57
New cards
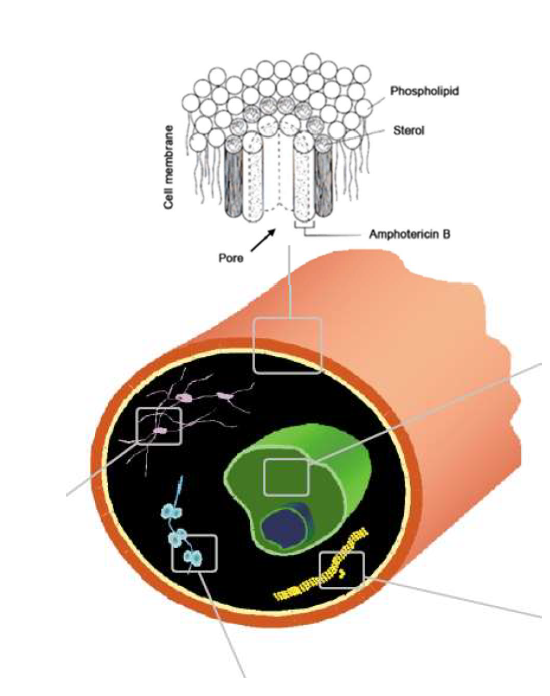
Antifungal drug: polyene
- Amphotericin B & Nystatin
- isolated from Streptomyces
- bind to ergosterol (membrane sterol essential for the stability of fungal cell membranes) and forms a pore that disrupts membrane integrity
- leads to oxidative damage
- nephrotoxic
- polyenes have a high affinity for ergosterol but not for cholesterol
- isolated from Streptomyces
- bind to ergosterol (membrane sterol essential for the stability of fungal cell membranes) and forms a pore that disrupts membrane integrity
- leads to oxidative damage
- nephrotoxic
- polyenes have a high affinity for ergosterol but not for cholesterol
58
New cards
How can fungi develop resistance to polyene?
- alterations in membrane sterols
- activation of antioxidative responses
- defects in sterol biosynthesis
- membrane composition
- orientation of ergosterols within the membrane
- activation of antioxidative responses
- defects in sterol biosynthesis
- membrane composition
- orientation of ergosterols within the membrane
59
New cards
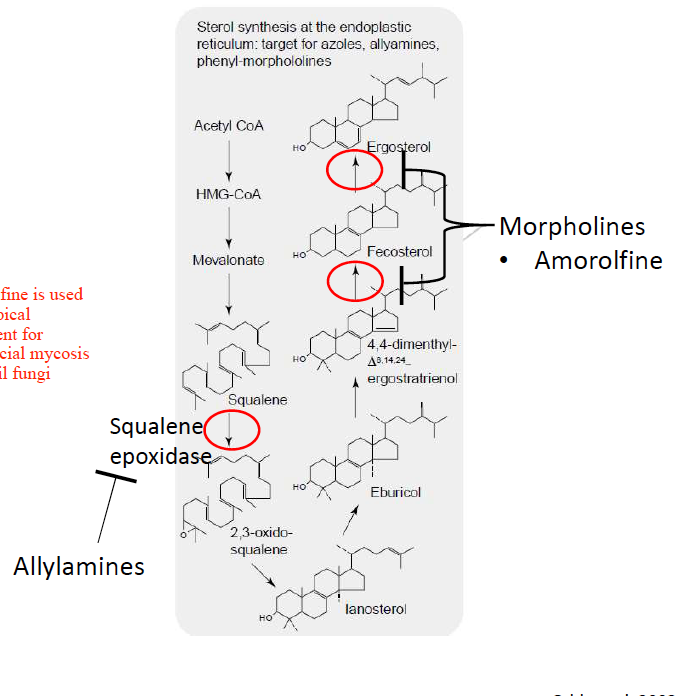
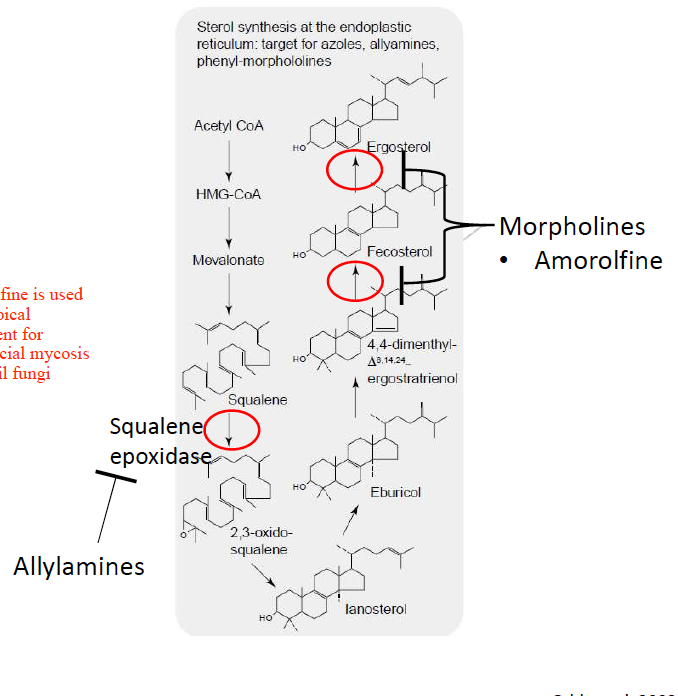
Antifungal drug: Azoles
- largest class of antifungal (Ketoconazole, fluconazole) and new triazoles (voriconazole, ravuconazole, itraconazole). triazoles have small structural differences but have increased potency, spectrum and bioavailability.
- targets ergosterol biosynthesis: inhibits demethylation of lanosterol (lanosterol demethylase)
- target broad-spectrum of mycoses (Candida, Cryptococcus, dimorphic fungi and molds).
*lanosterol demethylase is a cytochrome P450 enzyme responsible for demethylation of lanosterol. this causes the cell membrane structure to be altered and causes cell death.
- targets ergosterol biosynthesis: inhibits demethylation of lanosterol (lanosterol demethylase)
- target broad-spectrum of mycoses (Candida, Cryptococcus, dimorphic fungi and molds).
*lanosterol demethylase is a cytochrome P450 enzyme responsible for demethylation of lanosterol. this causes the cell membrane structure to be altered and causes cell death.
60
New cards
How do fungi develop azole resistance?
- target modification: mutation in lanosterol demethylase that decreases azoles' binding affinity
- efflux: over-expression of efflux pumps
- decrease in the uptake of Azole drugs
- alteration of the sterol biosynthesis pathway that allows utilization of intermediated even in the presence of azoles
- biofilms and persister cells
- efflux: over-expression of efflux pumps
- decrease in the uptake of Azole drugs
- alteration of the sterol biosynthesis pathway that allows utilization of intermediated even in the presence of azoles
- biofilms and persister cells
61
New cards
Antifungal drug: Allylamines
- Terbinafine inhibits early steps of the ergosterol pathway by targeting squalene epoxidase
- inhibit squalene epoxidase
squalene epoxidase confer the conversion of squalene to 2,3-oxido-squalene
- inhibit squalene epoxidase
squalene epoxidase confer the conversion of squalene to 2,3-oxido-squalene
62
New cards
Antifungal drug: Morpholines
- Amorolfine inhibits reductase and isomerase enzyme
- used as a topical treatment for superficial mycosis like nail fungi
- Amorolfine prevents the conversion of 4,4-dimethyl-ergostratrienol to fecosterol and the conversion of fecosterol to ergosterol.
- used as a topical treatment for superficial mycosis like nail fungi
- Amorolfine prevents the conversion of 4,4-dimethyl-ergostratrienol to fecosterol and the conversion of fecosterol to ergosterol.
63
New cards
Antifungal drug: echinocandins
- natural cyclic lipopeptides (Caspofungin, Micafungin, Anidulafungin)
- inhibit B-glucan synthase
- B glucan synthase is an enzyme responsible for the biosynthesis of beta-glucan polysaccharides that are constituents of the fungal cell wall
- inhibit B-glucan synthase
- B glucan synthase is an enzyme responsible for the biosynthesis of beta-glucan polysaccharides that are constituents of the fungal cell wall
64
New cards
How can fungi develop resistance to Echinocandins?
- no known efflux pumps
- resistance is not common and if observed it's associated with mutations in B-glucan synthase
- no cross- resistance between echinocandins. this means that even though these drugs are similar in structure and share the same target, the resistance that a fungi has to one drug does not mean there will be resistance to another drug
- paradoxical resistance to caspofungin
- resistance is not common and if observed it's associated with mutations in B-glucan synthase
- no cross- resistance between echinocandins. this means that even though these drugs are similar in structure and share the same target, the resistance that a fungi has to one drug does not mean there will be resistance to another drug
- paradoxical resistance to caspofungin
65
New cards
Antifungal drug: Nikkomycin
Nikkomycin Z:
- antifungal molecule produced by Streeptomyces
- chitin synthase inhibitor (chitin is a cell wall component)
- not in clinical use
- being developed for Valley Fever
- antifungal molecule produced by Streeptomyces
- chitin synthase inhibitor (chitin is a cell wall component)
- not in clinical use
- being developed for Valley Fever
66
New cards
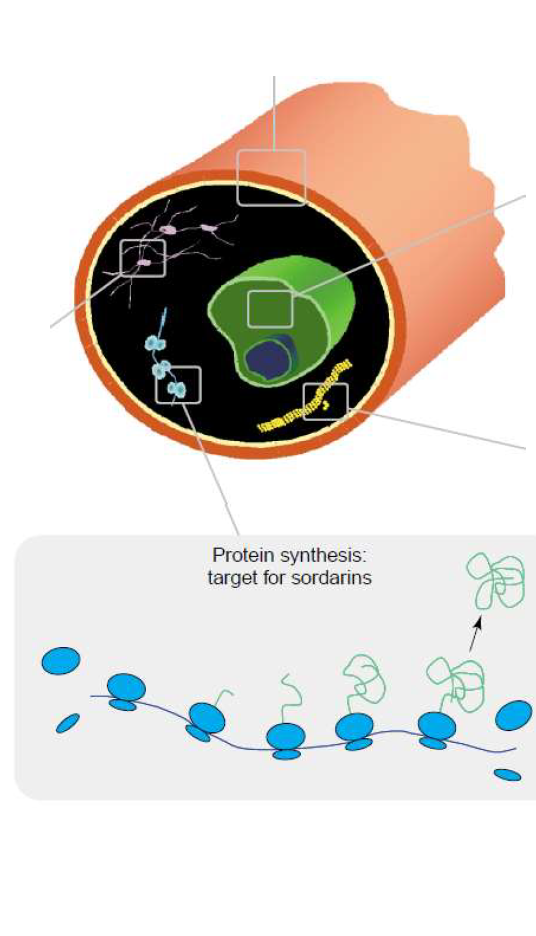
Antifungal drug: Sordarins
- Protein synthesis inhibitors: target fungal translation Elongation Factor 2 (EF2).
- Not in clinical use
- lab resistance observed in EF2 amino acid substitution
- Not in clinical use
- lab resistance observed in EF2 amino acid substitution
67
New cards
Antifungal that affects microtubules
Griseofulvin
68
New cards
Antifungal that inhibits nucleic acid synthesis
Flucytosine
69
New cards
Antifungal that interferes with the cell membrane
Polyenes: (Amphotericin B, Nystatin)
70
New cards
Antifungal that inhibits Sterol Synthesis
- Azoles (Ketoconazole, fluconazole; triazoles: voriconazole, ravuconazole, itraconazole)
- Allylamines (Terbinafine)
- Morpholies (Amorolfine)
- Allylamines (Terbinafine)
- Morpholies (Amorolfine)
71
New cards
Antifungal that inhibits cell wall formation
- Echinocandins
- Nikkomycins
- Nikkomycins
72
New cards
Antifungal that inhibits protein synthesis
Sordarins
73
New cards
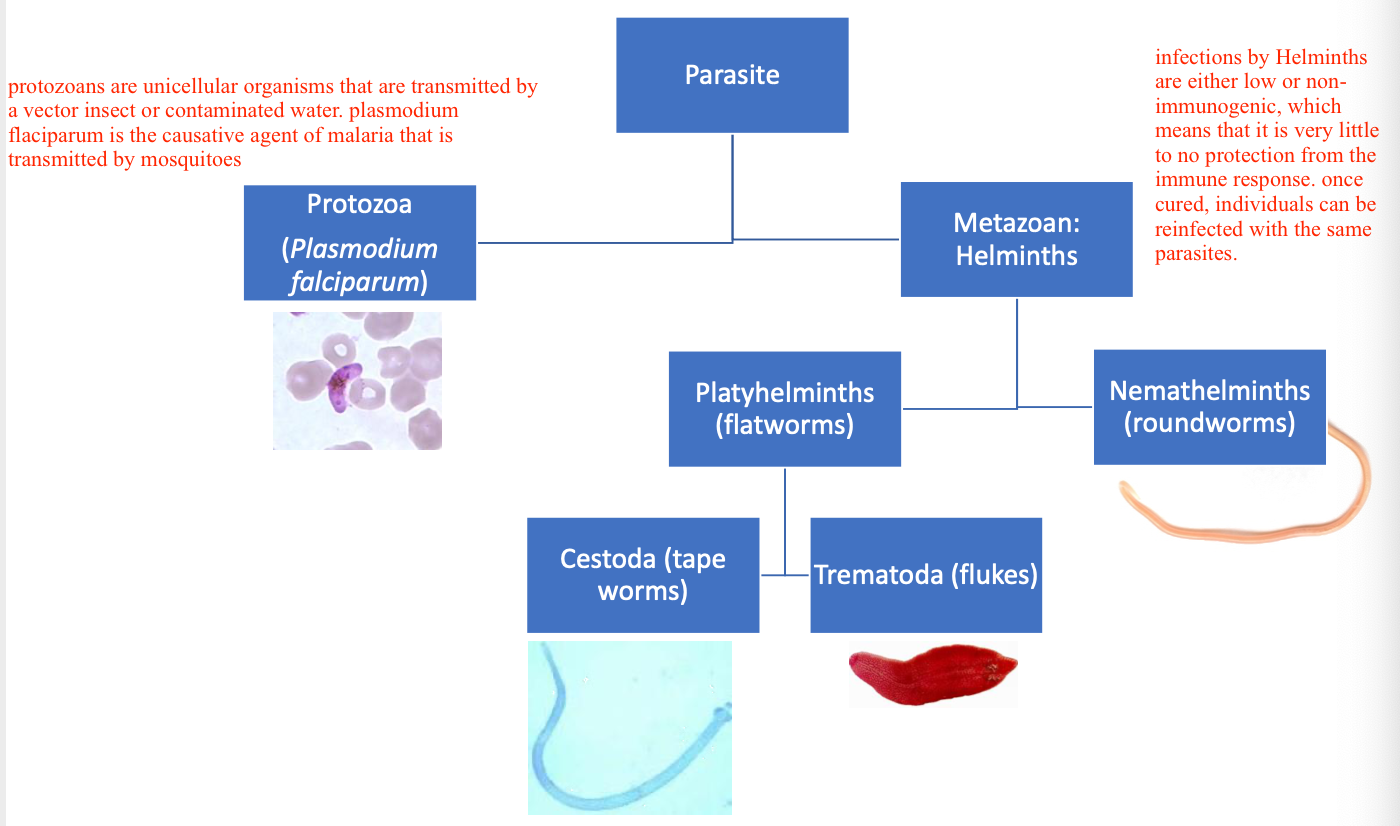
Parasitic infections types
Parasite --> Protozoa (Plasmodium falciparum) or Metazoan: Helminths
Metazoan --> Platyhelminths (flatworms) or Nemathelminths (roundworms)
Platyhelminths (flatworms) --> Cestoda (tape worms) or Trematoda (flukes)
Metazoan --> Platyhelminths (flatworms) or Nemathelminths (roundworms)
Platyhelminths (flatworms) --> Cestoda (tape worms) or Trematoda (flukes)
74
New cards
Protozoa (Pasmodium falciparum)
Unicellular organisms that are transmitted by a vector insect or by contaminated water.
Plasmodium falciparum is the causative agent of malaria that is transmitted by mosquitoes
Plasmodium falciparum is the causative agent of malaria that is transmitted by mosquitoes
75
New cards
Metazoan: Helminths
Low or non-immunogenic infections. There is little to no protection by the immune system, so individuals can be reinfected with the same parasite
76
New cards
Human parasitic diseases are most prevalent in tropical regions
Many parasites are transmitted by insects that don't hibernate in the tropical regions so they have a high prevalence.
It's difficult to know the prevalence of these diseases because the areas where they are common lack surveillance
1.5 billion people are infected by parasites
It's difficult to know the prevalence of these diseases because the areas where they are common lack surveillance
1.5 billion people are infected by parasites
77
New cards
Examples of parasitic diseases prevalent in tropical regions
- Ascaris (0.8-1.2B)
- Hookworms (0.56-0.74B)
- Whipworms (0.6-0.8B)
- Filarial worms (120M)
- Malaria (219M)
- Schistosomes (207M)
- Amebiases (50M)
- Taenia tapeworms (50M)
- Clonorchis (20M)
- Chagas disease (15M)
- Hookworms (0.56-0.74B)
- Whipworms (0.6-0.8B)
- Filarial worms (120M)
- Malaria (219M)
- Schistosomes (207M)
- Amebiases (50M)
- Taenia tapeworms (50M)
- Clonorchis (20M)
- Chagas disease (15M)
78
New cards
Neglected Tropical Diseases
almost all of the parasitic diseases are classified as neglected tropical diseases.
- caused by bacteria, viruses, protozoa and helminths
- Communicable diseases affect 149 tropical and subtropical countries
- Poorest regions with inadequate access to clear water, sanitation, and living with close contact with infected animals
- "neglected" = not considered a threat in wealthier countries
- not all parasitic diseases are NTD. malaria is not an NTD
- caused by bacteria, viruses, protozoa and helminths
- Communicable diseases affect 149 tropical and subtropical countries
- Poorest regions with inadequate access to clear water, sanitation, and living with close contact with infected animals
- "neglected" = not considered a threat in wealthier countries
- not all parasitic diseases are NTD. malaria is not an NTD
79
New cards
Ascariasis
roundworm disease that leads to growth and cognition impairment
- Neglected Tropical disease
- Neglected Tropical disease
80
New cards
Chagas
kissing-bug diseases that leads to swollen lymph nodes and organ damage.
- NTD
- chagas is not uncommon in the US
- infected individuals can be asymptomatic for decades, but eventually this disease leads to heart-threatening heart complications
- NTD
- chagas is not uncommon in the US
- infected individuals can be asymptomatic for decades, but eventually this disease leads to heart-threatening heart complications
81
New cards
Hookworm
contracted by walking barefoot on soil contaminated with feces. Can lead to blood loss and anemia
- NTD
- NTD
82
New cards
Human African trypanosomiasis
transmitted by parasite-infected tsetse flies. Can lead to fever, weakness, stiffness and death
- NTD
- NTD
83
New cards
Lymphatic filariasis
parasitic worm spread by mosquitoes. can lead to body disfiguring and swelling known as elephantiasis
- NTD
- NTD
84
New cards
Onchocerciasis
Parasitic worm transmitted by black flies. Can cause extreme itching, blindness and skin lesions
- NTD
- NTD
85
New cards
Schistosomiasis
Parasitic worm transmitted by fresh water snails. Can lead to blood in the urine, growth impairment and disfunction of kidneys, liver and spleen.
- NTD
- NTD
86
New cards
Important people who have battled parasitic diseases
- William C. Campbell
- Satoshi Omura
- Tu Youyou
- Satoshi Omura
- Tu Youyou
87
New cards
Avermectin
lowered prevalence of River Blindness and Lymphatic Filariasis
- developed by William C Campbell, Satoshi Omura and Tu Youyou
- developed by William C Campbell, Satoshi Omura and Tu Youyou
88
New cards
Artemisinin
saved millions of lives from Malaria
- developed by William C Campbell, Satoshi Omura and Tu Youyou
- developed by William C Campbell, Satoshi Omura and Tu Youyou
89
New cards
World's deadliest animal
Mosquito (725,000 deaths a year)
90
New cards
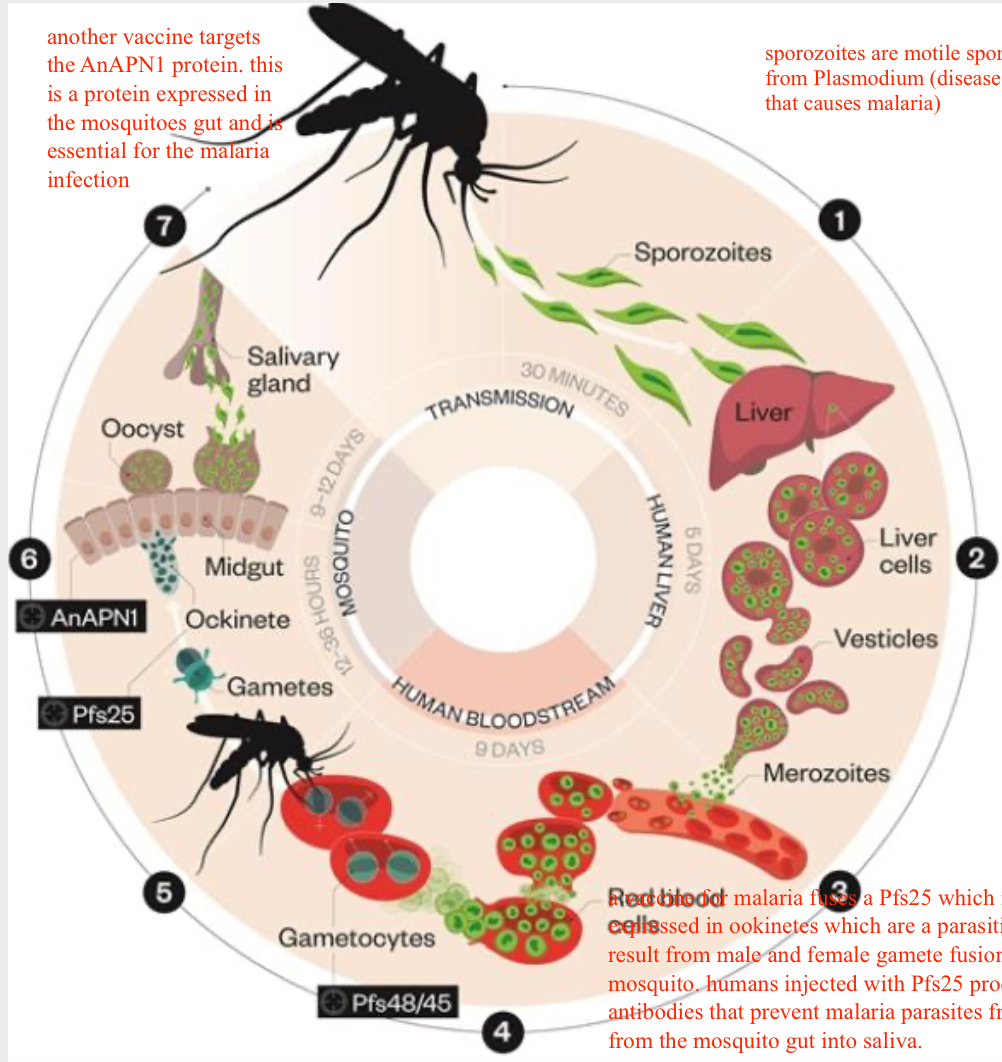
Malaria infection cycle
1. Anopheles mosquito releases sporozoites. Sporozoites are motile spores from Plasmodium (disease that causes malaria)
2. Sporozoites reach the liver and divide into invasive merozoites. Sporozoites reach the liver in 30 minutes.
3. Merzoites leave the liver and infect RBCs
4. Merozoites can differentiate into male and female gametocytes. they divide asexually inside RBCs until the cell bursts
5. Gametocytes are taken up by a biting mosquito. Male gametes fertilize female gametes which develop into ookinetes
6. Oocysts rupture releasing sporozoites that migrate into mosquito's salivary glands which causes reinfection
2. Sporozoites reach the liver and divide into invasive merozoites. Sporozoites reach the liver in 30 minutes.
3. Merzoites leave the liver and infect RBCs
4. Merozoites can differentiate into male and female gametocytes. they divide asexually inside RBCs until the cell bursts
5. Gametocytes are taken up by a biting mosquito. Male gametes fertilize female gametes which develop into ookinetes
6. Oocysts rupture releasing sporozoites that migrate into mosquito's salivary glands which causes reinfection
91
New cards
Vaccines for malaria
- one vaccine fuses Pfs25 which is a protein expressed in ookinetes which are a parasitic form that results from male and female gamete fusion in the msoquito. Humans injected with Pfs25 produced antibodies that prevent malaria parasites from migrating from the mosquito gut to the saliva.
- another vaccine targets the AnAPN1 protein. this is a protein expressed in the mosquito's gut and is essential for the malaria infection
- another vaccine targets the AnAPN1 protein. this is a protein expressed in the mosquito's gut and is essential for the malaria infection
92
New cards
Antimalarial drugs 4 types
- Quinolone derivatives
- Antifolates
- Antimicrobials: tetracycline, doxycycline, clindamycin, azithromycin, fluoroquinolones
- Artemisinins and derivatives
- Antifolates
- Antimicrobials: tetracycline, doxycycline, clindamycin, azithromycin, fluoroquinolones
- Artemisinins and derivatives
93
New cards
Antimalarial drugs: Quinolone-derivatives. Chloroquine
- highly effective at killing blood-stage Plasmodium
- inhibits heme detoxification -- toxic heme byproducts are released by plasmodium. chloroquine interferes with this process and leads to a buildup of heme-mediated toxicity
- inhibits heme detoxification -- toxic heme byproducts are released by plasmodium. chloroquine interferes with this process and leads to a buildup of heme-mediated toxicity
94
New cards
Resistance of quinolone-derivatives
Expression of transporter proteins:
- P. falciparum chloroquine-resistance transporter (Pfcrt)
- P. falciparum multidrug transporter (PfMDR1)
- these two proteins are present in resistant strains of malaria. those mutations lead to an increased IC50 values of chloroquine
- P. falciparum chloroquine-resistance transporter (Pfcrt)
- P. falciparum multidrug transporter (PfMDR1)
- these two proteins are present in resistant strains of malaria. those mutations lead to an increased IC50 values of chloroquine
95
New cards
Antimalarial drugs: Quinolone-derivative. Quinine
- alkaloid compound
- isolated from Cinchona tree bark
- one of the most effective malaria treatments
- acts on the erythrocytic stage
- interferes with parasite's ability to digest human hemoglobin. the actual mechanism is not known
- affect heme polymerization, but also block DNA replication and transcription to RNA
- isolated from Cinchona tree bark
- one of the most effective malaria treatments
- acts on the erythrocytic stage
- interferes with parasite's ability to digest human hemoglobin. the actual mechanism is not known
- affect heme polymerization, but also block DNA replication and transcription to RNA
96
New cards
Resistance of quinolone-derivative Quinine
- drug use was replaced by artemisinin in 2006
- Mechanism of resistance not well understood but thought to be associated with point mutations in Pfmdr1, Pfmrp and Pfnhe1. also related to upregulation of Pfmdr1.
- Mechanism of resistance not well understood but thought to be associated with point mutations in Pfmdr1, Pfmrp and Pfnhe1. also related to upregulation of Pfmdr1.
97
New cards
Antimalaria drugs: Quinolone-derivative. Primaquine
- Effective on liver-and-blood-stage
- induces oxidative damage to the cell and as a result disrupts the mitochondrial electron transport- but the exact mechanism is not known
- this drug is dangerous for people with a glucose-6-phosphate dehydrogenase deficiency because they are very sensible to oxidative and it causes extreme hemolysis
- induces oxidative damage to the cell and as a result disrupts the mitochondrial electron transport- but the exact mechanism is not known
- this drug is dangerous for people with a glucose-6-phosphate dehydrogenase deficiency because they are very sensible to oxidative and it causes extreme hemolysis
98
New cards
Resistance to quinolone-derivative Primaquine
Rare and not understood
99
New cards
Antimalaria drugs: antifolates
- Sulfadoxine
- mimics PABA
- inhibits dihydropteroate synthase
- this is a sulfa drug that targets and inhibits Plasmodium dihydropteroate synthase
- Sulfamethoxazole is also an antibiotic that inhibits Dihydropteroate synthase
- mimics PABA
- inhibits dihydropteroate synthase
- this is a sulfa drug that targets and inhibits Plasmodium dihydropteroate synthase
- Sulfamethoxazole is also an antibiotic that inhibits Dihydropteroate synthase
100
New cards
Antimalaria drugs: antifolates. Pyrimethamine
- inhibits DHFR
- Trimethoprim also inhibits DHFR
- Trimethoprim also inhibits DHFR