1- radiation physics
1/68
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
69 Terms
definition of radiation
energy in transit
definition of ionization
removal of electrons from an atom → formation of an "ion pair”
what are orbitals
3D shapes of where electrons exist around a nucleus
what are the 6 types of orbitals
S, P, D, F, G, H
what’s the Z number of a nucleus
atomic # aka # of protons (P)
# of electrons in a neutral atom equals what
Z number
what’s A number of a nucleus
# of protons (P) + N
what’s electron binding energy
the attractive force that keeps electrons bound to the nucleus in their orbitals
what’s the relationship between Z number + electron binding energy
direct relationship

definition of electromagnetic radiation
movement of energy through space as a combination of electric + magnetic fields
7 types of electromagnetic radiation
gamma rays
x-rays
ultraviolet
visible light
infrared
microwaves
radio waves
what’s quantum theory
energy transfer in the form of “bundles” (or packets) of energy called photons (or “quanta”)
mass + charge of x-rays
no mass or charge
x-rays travel in zigzag or straight lines
straight
x-rays’ ability to ionize allows them to do what 2 things
affect photographic film
produce biological + chemical changes
x-rays’ range of wavelength
0.1 A to 0.5 A (1 A = 1/10 nm)
2 mechanisms of x-ray production
Bremsstrahlung: electron → nucleus interaction
characteristic radiation: electron → electron interaction
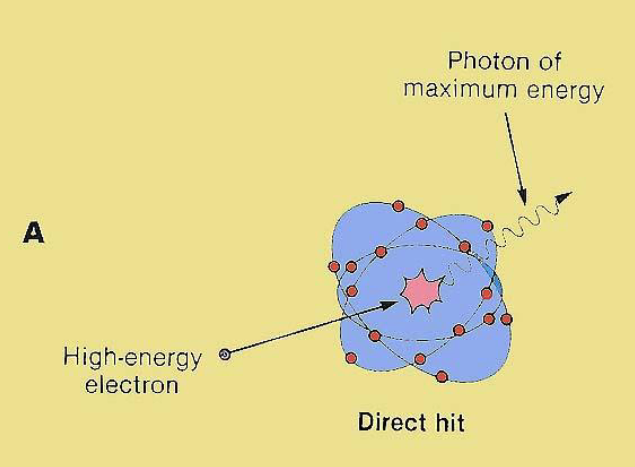
describe the Bremsstrahlung mechanism
high energy electron is decelerated by nuclei of high Z # material→ kinetic energy of high energy electron is converted into photon → x-ray is generated
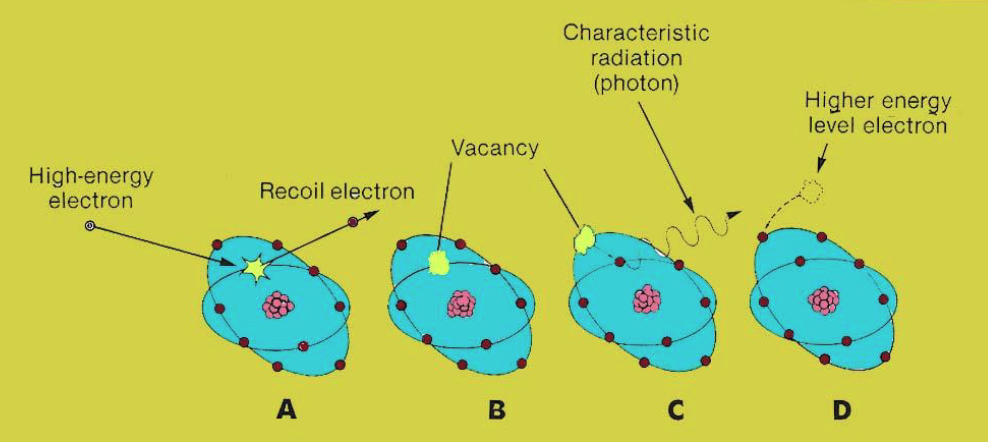
describe the characteristic radiation mechanism
high energy electron interacts w/ an inner shell electron + knocks it out of orbit → its vacancy is filled w/ an outer shell electron→ difference in energy level between outer + inner shell is released via x-ray photon
which mechanism is the primary source of radiation in the x-ray tube
Bremsstrahlung
describe each part of the x-ray tube and how it facilitates the 2 mechanisms
cathode: electron source
focussing cup: concentration of electrons
tube voltage (kVp) aka potential difference: mechanism to accelerate electrons
anode: target to stop electrons
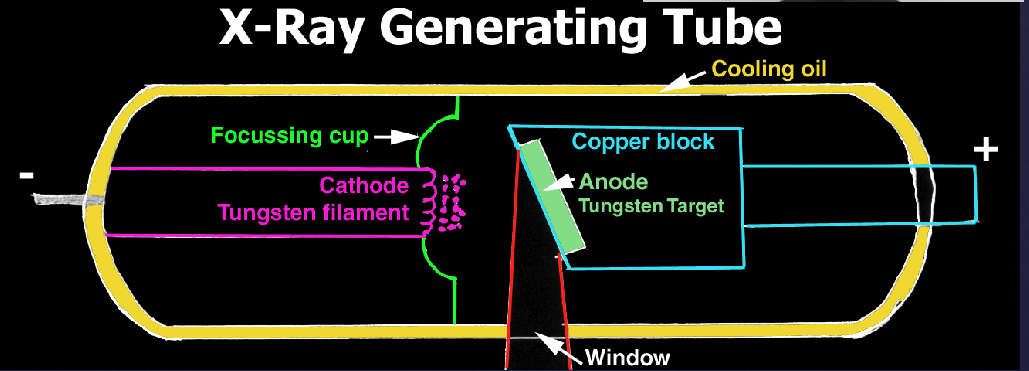
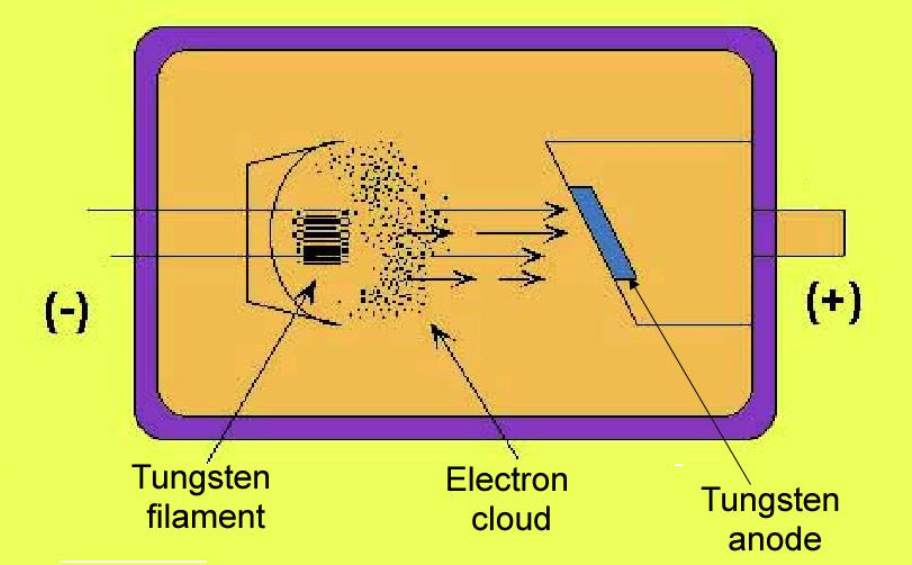
how does the cathode emit electrons
current heats up the cathode abt 2200o C → electrons emitted → formation of electron cloud
4 qualities of tungsten that make it a great anode
High atomic number
High melting point
Low vapor pressure ( to maintain vacuum)
High degree of thermal conductivity
6 factors that control the x-ray beam
tube voltage (kVp)
exposure time (S)
tube current (mA)
filtration
collimation
distance of x-ray tube from pt/receptor
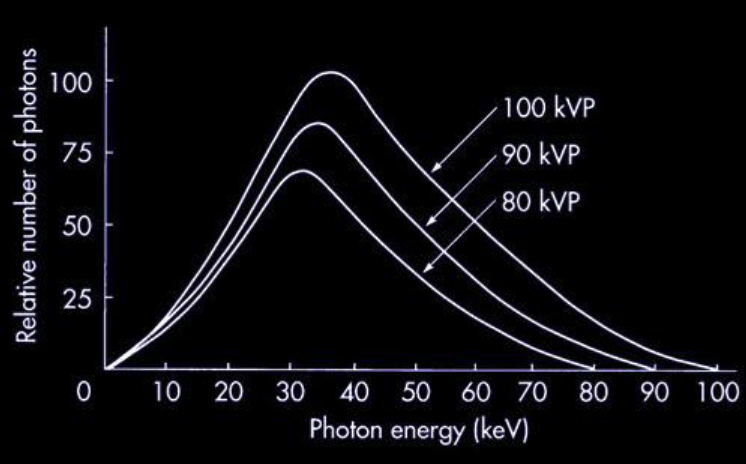
what does the highest point + lowest point of each curve represent
peak: mean photon energy (keV)
end of curve: KvP at which the x-ray beam was acquired
increasing kVp results in what
number of photons (keV) + max energy of the beam increases
describe how filtration affects the x-ray beam
removal of low energy photons from the x-ray beam → reduces patient risk + intensity of beam, therefore compensatory increase in exposure time needed
which components of the x-ray tube provide filtration
inherent filtration via glass, oil
added filtration via aluminum disk
what are the regulated required amounts of filtration for certain doses
50-70 kVp: 1.5 mm aluminum
above 70 kVp: 2.5 mm aluminum
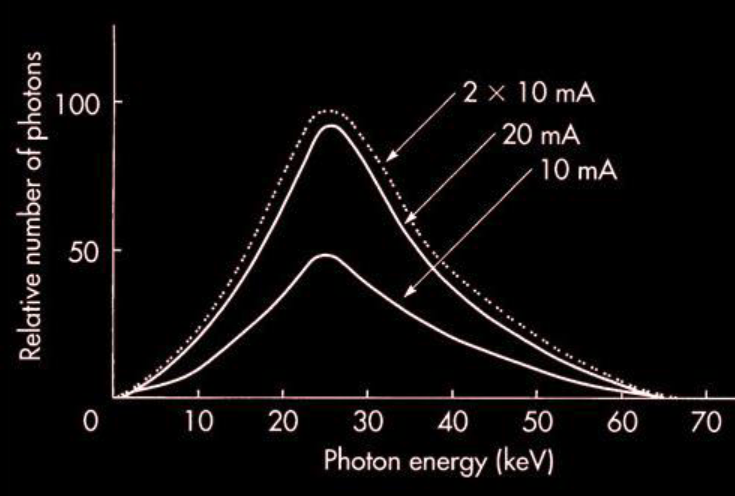
describe the relationship between tube current (mA) + photon energy
higher the current (mA) → higher number of photons
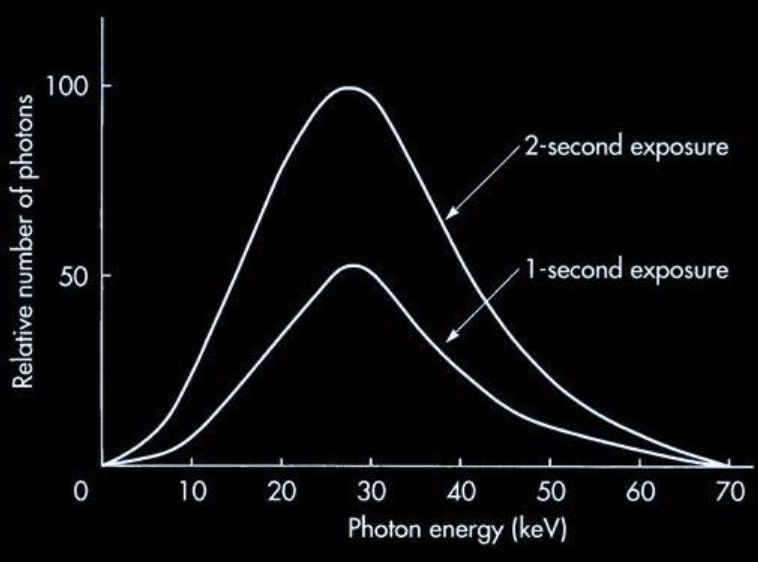
describe the relationship between exposure time + photon energy
longer exposure → higher number of photons
describe how collimation affects the x-ray beam
reduces size + modifies shape of beam
reduces volume of tissue irradiated
improves image quality
describe how distance from x-ray tube affects the x-ray beam
inverse square law: I (intensity) = 1/D2 (distance)
3 types of x-ray interaction w/ matter
coherent scattering
photoelectric effect
Compton scattering
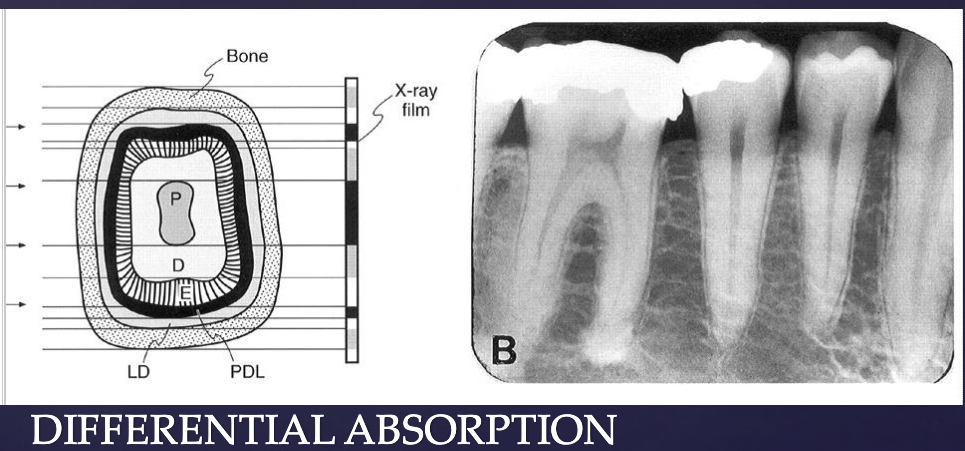
what’s the photoelectric effect
how images are formed:
photon collides w/ inner-shell electron → electron is ejected (ionization) → photon transfers all energy to the electron + photon ceases to exist → another electron from higher energy fills the vacancy → radiation is emitted
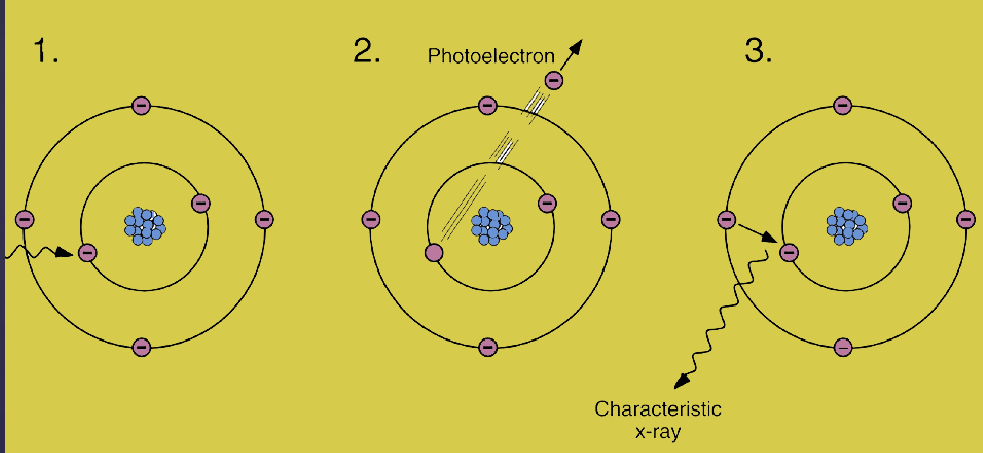
how is the photoelectric effect clinically significant
Z of bone is higher than Z of soft tissue → differential photoelectric absorption within different types of tissues makes production of a radiographic image possible
anything on the x-ray that’s black: received photons vs. white: no photons
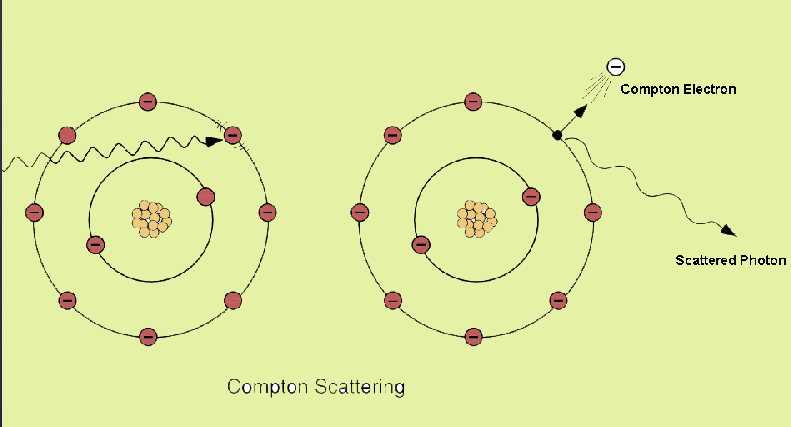
what’s Compton scattering
photon interacts w/ outer orbital electron → electron ejected from target atom → photon is deflected as a scatter photon w/ lower energy
each type of x-ray interaction makes up what % of interaction in an x-ray beam
coherent scattering: 7%
photoelectric effect: 27%
Compton scattering: 57%
definition of equivalent dose
measure of comparison of biological effectiveness of different types of radiation (Sievert, Sv)
definition of effective dose
estimates risk in humans by comparing different exposures, considering radiosensitivity of tissues + biologic effectiveness (Sievert, Sv)
7 types of ionizing radiation
x-ray
gamma ray
neutrons
beta particles
alpha particles
protons
heavy ions
2 mechanisms of radiation-induced cell injury
direct effect
indirect effect
which mechanism is responsible for 2/3 of radiation-induced biologic damage
indirect
describe the mechanism of direct effect radiation-induced injury
ionization of biologic macromolecules directly by a photon of ionizing radiation
describe the mechanism of indirect effect radiation-induced injury
water in tissues absorbs photon → ionization of water to form free radicals (radiolysis of water)
free radicals interact w/ macromolecules → biologic changes
what’s the primary target for cell damage from radiation
DNA, at risk for double-strand + single strand break
2 types of radiation injury
tissue rxns (deterministic effects): large # of cells killed → erythema, cataract formation
stochastic effects: sublethal damage to cells → carcinogenesis or heritable mutation
which type of radiation injury’s severity is independent of dosage
stochastic effects
2 factors that influence radiation damage
host: radiosensitivity of cell/tissue, stage in cell cycle, reproductive capability, age, O2 + temp (higher = greater damage), volume of tissue
radiation: type of radiation/LET (higher LET = more damage), dose, dose rate
the most radiosensitive cells have which 3 characteristics
Law of Bergonie + Tribondeau:
have high mitotic rate (actively proliferating)
undergo many future mitoses (younger cells)
undifferentiated/non-specialized in structure + function (immature cells)
what’s an exception to the Law of Bergonie + Tribondeau
small lymphocytes + oocytes (mature in differentiation yet sensitive to radiation)
rank organs/tissue types from most → least sensitive to radiation
bone marrow (lymphoblasts, lymphocytes, plasma cells, erythroblasts), intestines (epithelial stem cells), oral mucous membrane (basal cells), spermatogenic cells
skin + other organs w/ epithelial linings, inner enamel epithelium
fine vasculature
salivary glands, kidneys, liver, pancreas
muscles (striated muscle cells), brain (neurons), spinal chord, erythrocytes
2 major effects of radiation on embryo/fetus
teratogenic effects (deterministic): death in 1st week of pregnancy, intra-uterine growth retardation, congenital malformations, developmental abnormalities
stochastic: childhood cancer
2 factors influencing probability of radiation effects on embryo
dose
stage of gestation @ time of exposure
radiogenic effects for an embryo 0-9 days old
all or none
radiogenic effects for an embryo 10 days-6 weeks old
congenital anomalies + growth retardation
radiogenic effects for an embryo 6-40 weeks old
growth retardation
microcephaly
mental retardation
dose threshold of radiation to the fetus required to produce birth defects
100-250 mSv
4 acute radiation syndromes + their dosages
prodromal syndromes: 1-2 Gy
hematopoietic syndrom: 2-7 Gy
GI syndrome: 7-15 Gy
CNS syndrome: 50 Gy
radiation therapy is used in the oral cavity for what
malignant oral lesions that are radiosensitive
dosage for radiation therapy to oral cavity
total 64-70 Gy in 6-7 weeks
5 structures in the oral cavity that can be affected by radiation therapy
oral mucous membrane
taste buds
teeth
salivary glands
bone
which oral cavity structures can heal from radiation therapy
oral mucous membrane: after 2 months
taste buds: after 60-120 days
describe the effect of radiation therapy on the oral mucous membrane
desquamation
inflammation/pain
white/yellow pseudomembrane
secondary fungal infections
long term: atrophic, thin, avascular mucosa
describe the effect of radiation therapy on taste buds
lowered taste acquity
describe the effect of radiation therapy on teeth
tooth bud destroyed
malformations, arrested growth
T/F: erupted teeth are radioresistant (resistant to irradiation)
true
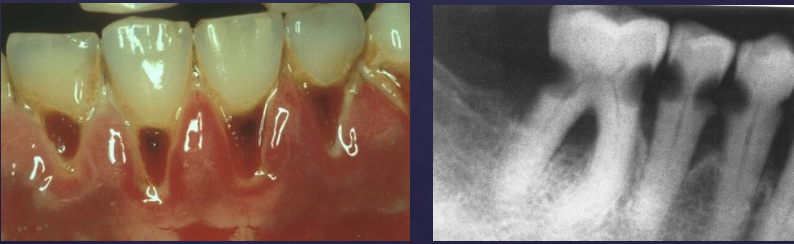
describe the effect of radiation therapy on salivary glands
xerostomia
pH altered → decalcificaition of enamel
radiation caries
describe the effect of radiation therapy on bone of the oral cavity
osteoradionecrosis: damage to vasculature of periosteum + cortical bone, destruction of osteoblasts
