Cartilage Histology
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
52 Terms
the musculoskeletal system comprises ___, ___, and ___
cartilage, bone, and skeletal muscle
cartilage and bone are ___ tissues
cartilage and bone are specialized connective tissues
cartilage is vascular/avascular?
avascular
primary functional component of cartilage tissue?
ECM (constitutes over 95% of cartilage volume)
what are chondrocytes?
Chondrocytes are mature cartilage cells derived from chondroblasts that are embedded in the extracellular matrix (lacunae), where they produce and maintain this matrix but can no longer divide.
ECM products include:
type II collagen (in all cartilages)
elastic fibres (only in elastic cartilage)
proteoglycans
contribute to compressive resistance and water retention
e.g.: aggrecan
glycoproteins
mediate. adhesion between chondrocytes and ECM components
e.g.: chondronectin
how does nutrient and waste exchange occur in cartilage?
Nutrient and waste exchange in cartilage occurs by passive diffusion through the hydrated extracellular matrix, sourced from perichondrial capillaries or synovial fluid, and aided by mechanical compression—a necessity due to the tissue’s avascular nature.
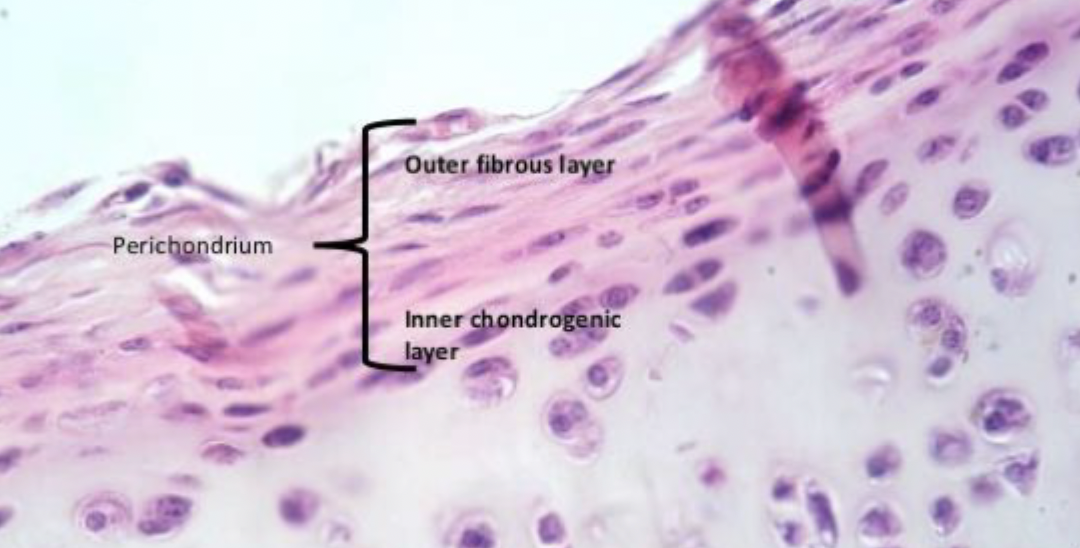
what is the perichondrium?
The perichondrium is a layer of connective tissue that surrounds elastic and extra-articular hyaline cartilage but not fibrocartilage nor articular hyaline cartilage. It is composed of:
Outer fibrous layer:
Composition: Dense irregular connective tissue (rich in type I collagen fibres), blood vessels, lymphatics, and nerves
Function: Provides mechanical protection and nourishment to the cartilage via diffusion
Inner chondrogenic (cellular) layer: contains progenitor cells that can regenerate cartilage.
Composition: Contains chondroprogenitor (mesenchymal) cells
Function: Responsible for appositional growth of cartilage by differentiating into chondroblasts, which produce new extracellular matrix
what types of cartilage are there?
hyaline cartilage
articular
extra-articular
related to structural support
related to bone growth
elastic cartilage
fibrocartilage
what is hyaline cartilage? what does it contain? where is it found? what are its functions?
what is hyaline cartilage?
it is the most abundant type of cartilage in the body
forms embryonic skeleton, which is later replaced by bone through endochondral ossification
what does it contain?
matrix containing primarily type II collagen fibres, along with GAGs, proteoglycans, and multi-adhesive glycoproteins
where is it found?
articular surfaces of synovial joints (articular cartilage)
nose, trachea, bronchi, costal cartilages
epiphyseal growth plates, temporary fetal skeleton
what are its functions?
provides a low-friction surface in synovial joints and distributes applied forces to underlying bone
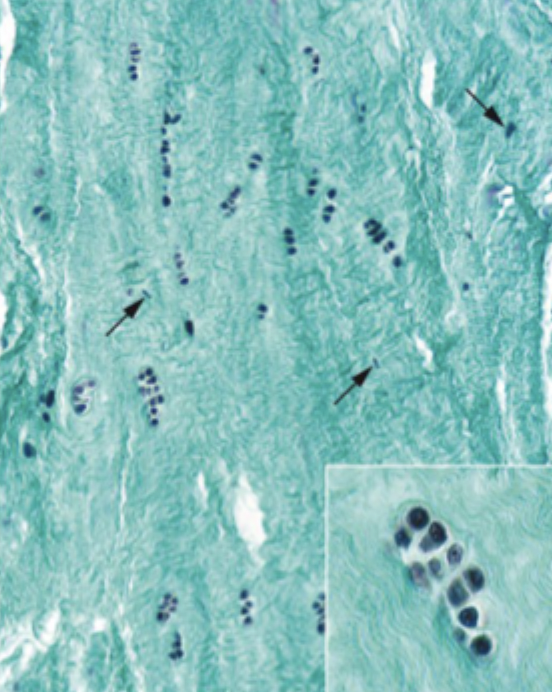
what is elastic cartilage
distinguished but the presence of elastic fibres and elastic lamellae within its matrix, in addition to components found in hyaline cartilage
chondrocytes, ECM (Type II collagen fibres, proteoglycans, glycoproteins)
forms a dense network of branching of anastomosing fibres and interconnecting sheets of elastic material
provides flexibility and support
found in external ear, walls of the external acoustic meatus, auditory (Eustachian) tube, and epiglottis of larynx
mnemonic: four Es
what is fibrocartilage
a strong, dense type of cartilage specialized for resistance to tensile forces. It is hard and nonelastic, making it the strongest type of cartilage.
characterized by a matrix containing abundant type I collagen fibres, as well as the matrix components of hyaline cartilage (chondrocytes, ECM {Type II collagen fibres, proteoglycans, glycoproteins})
no perichondrium
it is considered a combination of denser regular connective tissue and hyaline cartilage
locations: intervertebral discs, menisci of the knee joint, pubic symphysis
function: provides strong resistance to tensile and compressive forces, enabling shock absorption and structural support in load-bearing joints.
___ is the most abundant type of cartilage, while ___ is the strongest
hyaline cartilage is the most abundant type of cartilage, while fibrocartilage is the strongest
components of hyaline cartilage
type II collagen fibres (alongside smaller amounts of other types of collagen)
proteoglycans (e.g.: aggrecan)
GAGs + core protein
proteoglycan aggregates
proteoglycans + hyaluronic acid
multi-adhesive glycoproteins (including fibronectin)
what is the function of hyaline cartilage
to provide a low-friction surface in synovial joints and to distribute applied forces to underlying bone
hyaline cartilage forms the ___, which is later replaced by bone through ___ ossification
hyaline cartilage forms the embryonic skeleton, which is later replaced by bone through endochondral ossification
where is hyaline cartilage found in the body?
articular hyaline cartilage
articular surfaces of synovial joints
knee (tibiofemoral joint)
hip (femoroacetabular joint)
shoulder (glenohumeral joint)
extra-articular hyaline cartilage
structural support
nasal cartilage (nasal septum)
laryngeal cartilage (thyroid and cricoid cartilage)
costal cartilage
developmental cartilage
epiphyseal growth plates in growing bones
temporary embryonal/fetal skeleton pior to ossification
elastic cartilage is characterized by the presence of ___, and ___ in addiction to the typical components of hyaline cartilage (chondrocytes, type II collagen, proteoglycans, glycoproteins)
elastic fibres
elastic lamellae
What gives elastic cartilage its high resilience and flexibility?
Elastic cartilage contains an ECM with a threadlike meshwork of elastic fibers.
These fibers branch and anastomose, forming a dense, interconnected network that allows the tissue to bend and recoil without damage.
function and location of elastic cartilage
provides flexibility and support and is found in locations requiring such properties, including the external ear, walls of the external acoustic meatus, auditory (Eustachain) tube, and epiglottis of the larynx.
which types of cartilage are and aren't surrounded by a perichondrium?
perichondrium present
extra-articular hyaline cartilage
elastic cartilage
no perichondrium present
articular hyaline cartilage
fibrocartilage
unlike hyaline cartilage, the matrix of elastic cartilage does not ___ with aging, and elastic fibres can be highlighted using ___ staining
unlike hyaline cartilage, the matrix of elastic cartilage does not calcify with aging, and elastic fibres can be highlighted using orcein staining
fibrocartilage is considered a mixture of ___ and ____
fibrocartilage is considered a mixture of dense regular connective tissue and hyaline cartilage
contents of fibrocartilage
Fibroblasts: within extracellular matrix
Chondrocytes: Present in small numbers, embedded in lacunae.
Extracellular matrix (ECM):
Dense type I and type II collagen fibers: Provide high tensile strength and resistance to pressure.
Proteoglycans: Attract water and contribute to resistance against compression.
Glycoproteins: Such as chondronectin, which helps bind chondrocytes to the ECM.
fibrocartilage:
in histological sections, chondrocytes appear as ___, while fibroblasts show ___.
rounded nuclei with a small amount of surrounding amorphous matrix, embedded in lacunae
flattened or elongated nuclei within fibrous areas
function and location of fibrocartilage
provides tensile strength and resistance to compression
intervertebral discs, menisci of the knee, and the pubis symphysis
fibrocartilage does not have a ___, and relies on ___ from surrounding tissues for nutrient and waste exchange. therefore, it has a low ___
perichondrium
diffusion
regenerative capacity
which type of cartilage is the strongest?
fibrocartilage
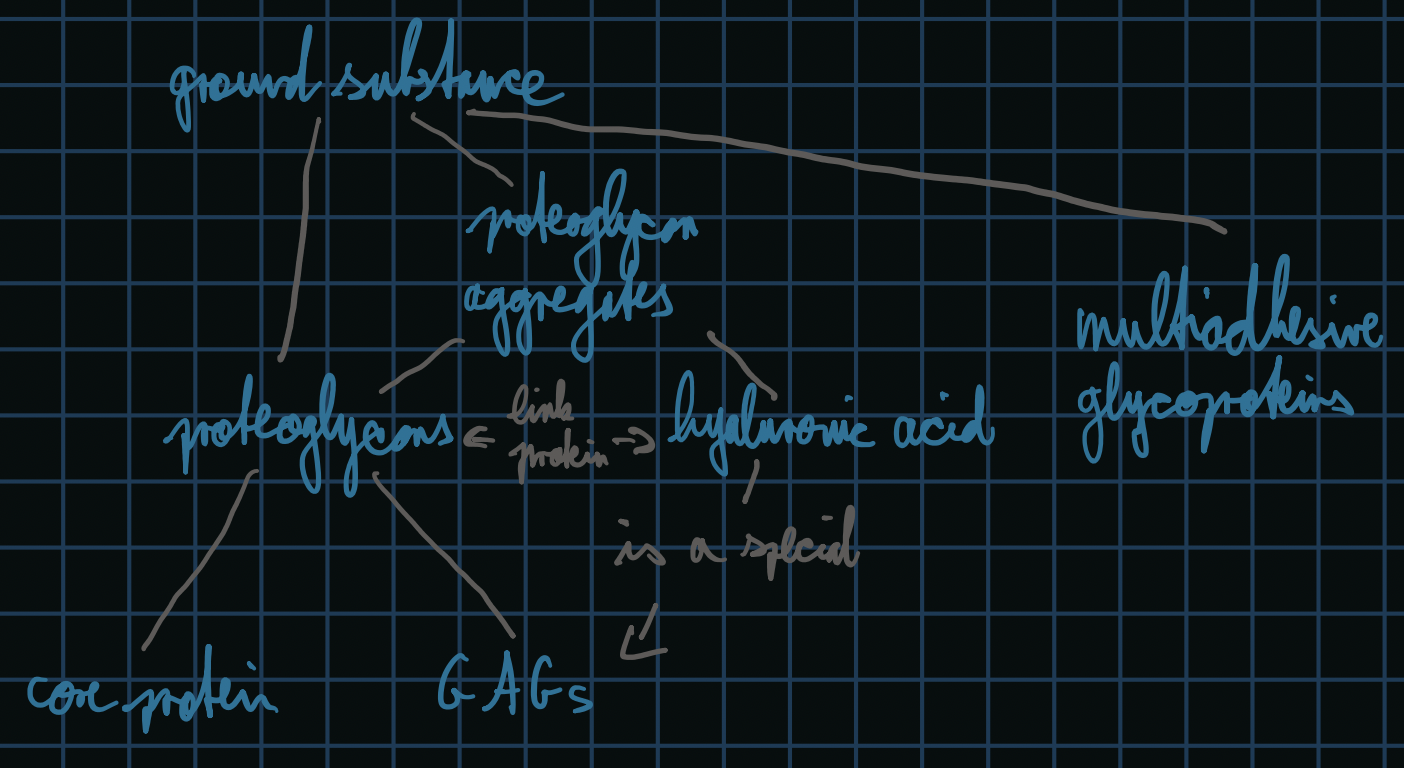
describe glycosaminoglycans (GAGs)
fundamental component of the ECM in connective tissues
unbranched polysaccharide chains
highly negatively charged → attracting water and forming a hydrated gel → ability to resist compression
bound to a protein core to form proteoglycans (such as aggrecan)
proteoglycan aggregates are formed from multiple aggregate molecules binding to hyaluronic acid (a GAG that does not attach to a core protein)
ground substance is composed of
Proteoglycans: Large molecules with glycosaminoglycan (GAG) side chains (e.g., aggrecan) that attract and retain water, contributing to cartilage’s resistance to compression.
Glycoproteins: Such as chondronectin, which facilitate adhesion between chondrocytes and the ECM.
Water: The ECM is highly hydrated, which supports diffusion and mechanical resilience.
what are proteoglycans
Proteoglycans are large molecules in the cartilage extracellular matrix composed of:
A core protein
Multiple glycosaminoglycan (GAG) side chains (e.g., chondroitin sulfate, keratan sulfate)
These structures:
Attract water due to their negative charge
Form aggregates (e.g., aggrecan with hyaluronic acid)
Provide compressive strength and resilience to cartilage
They are essential for maintaining the hydrated, gel-like consistency of cartilage ground substance.
what are glycosaminoglycans (GAGs)
Glycosaminoglycans (GAGs) are long, unbranched polysaccharide chains composed of repeating disaccharide units. They are:
Highly negatively charged, attracting water and cations
Hydrophilic, contributing to the gel-like, compressive-resistant nature of cartilage
Commonly found as side chains on proteoglycans (e.g., in aggrecan)
Examples include chondroitin sulfate, keratan sulfate, and hyaluronic acid.
relate ground substance, proteoglycan aggregates, GAGs, and proteoglycans to each other
contrast the different fibres found in different types of cartilage
Type II collagen
found in all cartilage types (highest amount found in hyaline cartilage)
provides tensile strength
produced by chondrocytes
Type I collagen
found mainly in fibrocartilage
adds additional strength
produced by fibroblasts
Elastic fibers
found only in elastic cartilage
provide flexibility and elasticity
produced by chondrocytes
what are multi-adhesive glycoproteins?
components of cartilage extracellular matrix that:
Link chondrocytes to the ECM by binding collagen fibers, proteoglycans, and cell surface receptors
Help organize ECM structure and mediate cell adhesion, migration, and signaling
Example: Chondronectin, which connects type II collagen and proteoglycans to chondrocytes
They are essential for maintaining the structural integrity and functional interactions within cartilage.
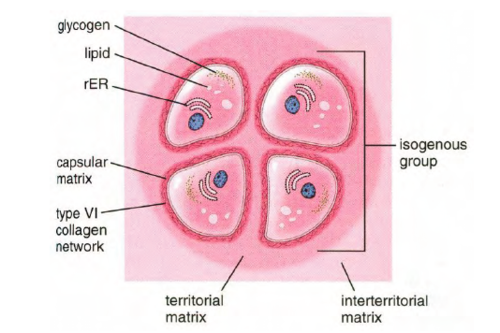
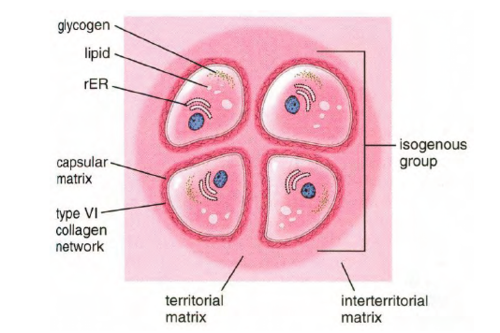
what are the three regions of hyaline cartilage matrix based on staining properties?
capsular (pericellular) matrix
territorial matrix
interterritorial matrix
capsular (pericellular) matrix
Thin ring surrounding each chondrocyte
Richest in glycosaminoglycans (GAGs) and type VI collagen
Stains darkest (most basophilic) due to high GAG content
Acts as a protective microenvironment, regulating nutrient exchange and mechanical stress
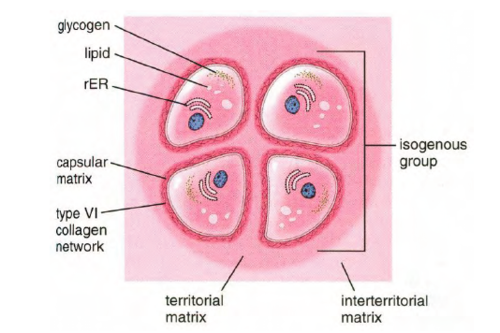
territorial matrix
Immediately surrounds isogenous groups (clusters of chondrocytes from the same progenitor)
Intermediate staining intensity
Contains more GAGs than the interterritorial matrix but less than the capsular matrix
Contains a moderate amount of collagen fibres (less than the capsular matrix)
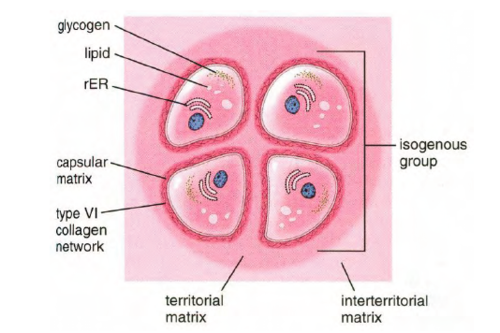
interterritorial matrix
Located between isogenous groups (forms bulk of cartilage tissue)
Lightest staining region
Rich in type II collagen, with lower GAG content
Provides tensile strength and resistance to compression
what are lacunae?
Lacunae are small cavities within the cartilage extracellular matrix where mature cartilage cells, known as chondrocytes, reside.
Chondrocytes become embedded in lacunae as they mature from chondroblasts.
The lacunae provide a protected space for chondrocytes to maintain and regulate the surrounding matrix.
These structures are especially visible in histological sections of cartilage.
what are isogenous groups?
Isogenous groups (also called isogenic groups) are clusters of chondrocytes that originate from a single chondroblast through cell division. These daughter cells:
Are genetically identical
Remain close together within a shared territorial matrix
Are housed in individual lacunae but appear grouped due to limited matrix separation
Isogenous groups are a hallmark of interstitial growth in cartilage, especially during development and in the epiphyseal growth plates.
what are fibroblasts?
Fibroblasts are the most common resident cells in connective tissue. They originate from mesenchymal stem cells and play a critical role in maintaining the extracellular matrix (ECM).
Key features:
Function: Synthesize and organize ECM components such as collagen and elastin
Morphology: Spindle-shaped, branching cells with abundant rough endoplasmic reticulum and a prominent Golgi apparatus
State: When metabolically less active, they are called fibrocytes
Fibroblasts are essential for tissue maintenance, repair, and wound healing.
contrast articular and extra-articular cartilage in terms of location, function, and presence of a perichondrium
Articular Hyaline Cartilage
Location: Covers bone surfaces in synovial joints (e.g., femoral condyles, humeral head)
Function:
Reduces friction
Absorbs mechanical shock
Enables smooth joint movement
Perichondrium: Absent
Extra-articular Hyaline Cartilage
Location: Found outside joints (e.g., tracheal rings, nasal septum, costal cartilages)
Function:
Provides structural support
Maintains shape with some flexibility
Perichondrium: Present
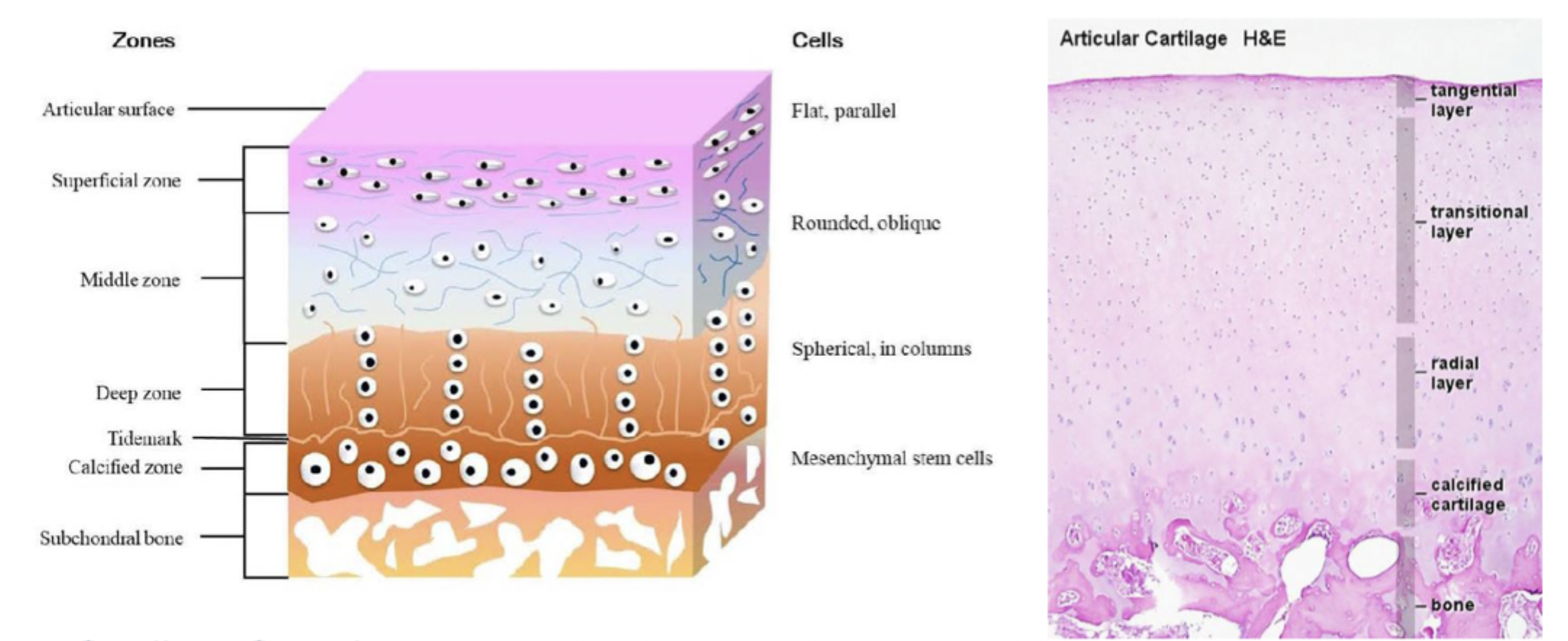
what are the zones of articular cartilage?
superficial (tangential) zone
middle (transitional) zone
deep (radial) zone
calcified zone
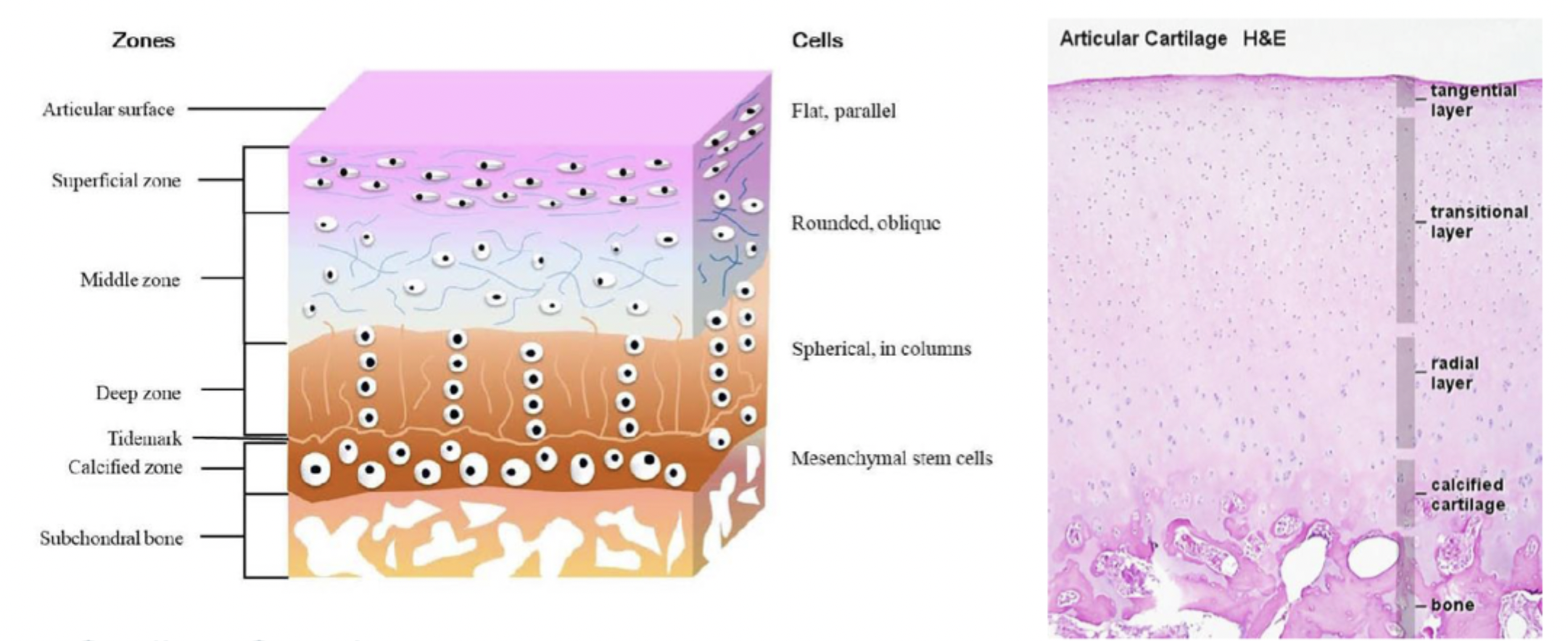
describe the superficial (tangential) zone of articular cartilage
Closest to joint surface
Flattened chondrocytes
Collagen fibers aligned parallel to the surface
Provides a smooth, gliding surface and resists shear forces
Why “tangential”?
The collagen fibers here run parallel (tangential) to the articular surface.
This arrangement helps resist shear forces during joint movement.
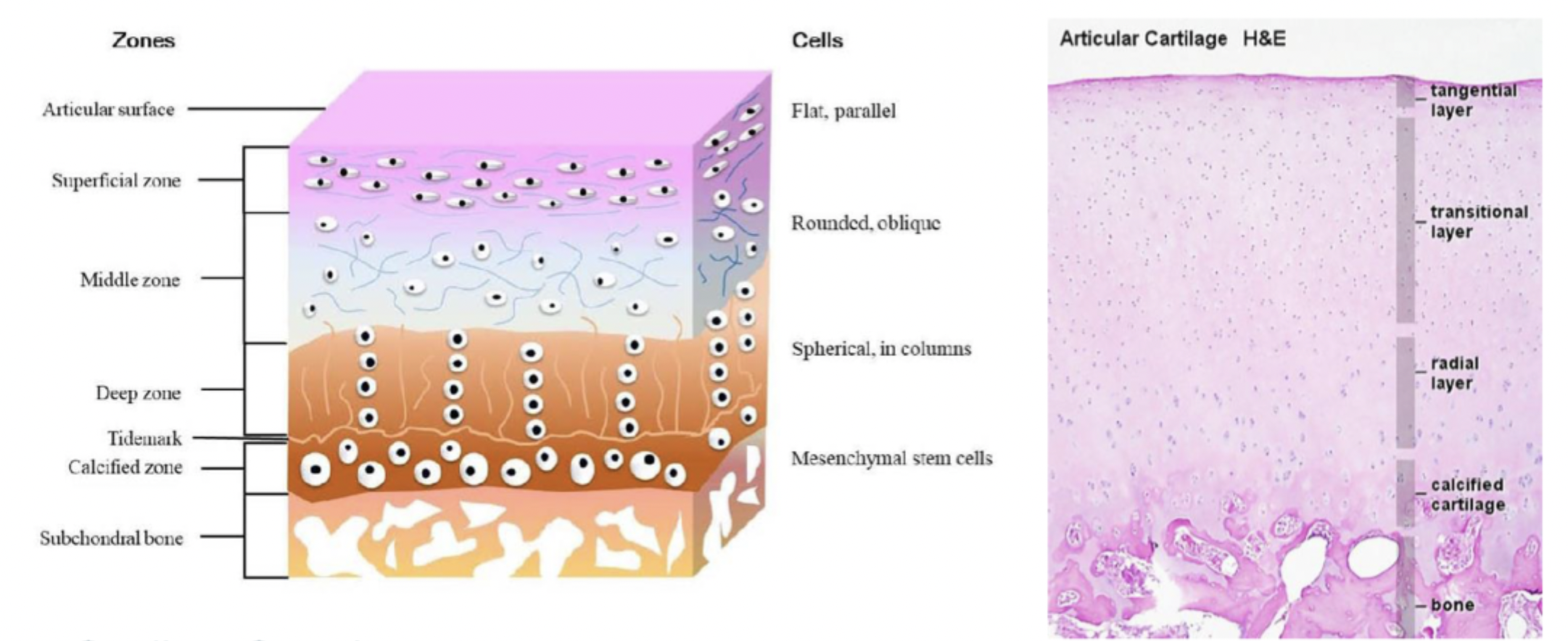
describe the middle (transitional) zone of articular cartilage
Rounder chondrocytes
Random orientation of collagen fibers
in between superficial (tangential) and deep (radial) zone
Serves as a transitional layer; absorbs compressive forces
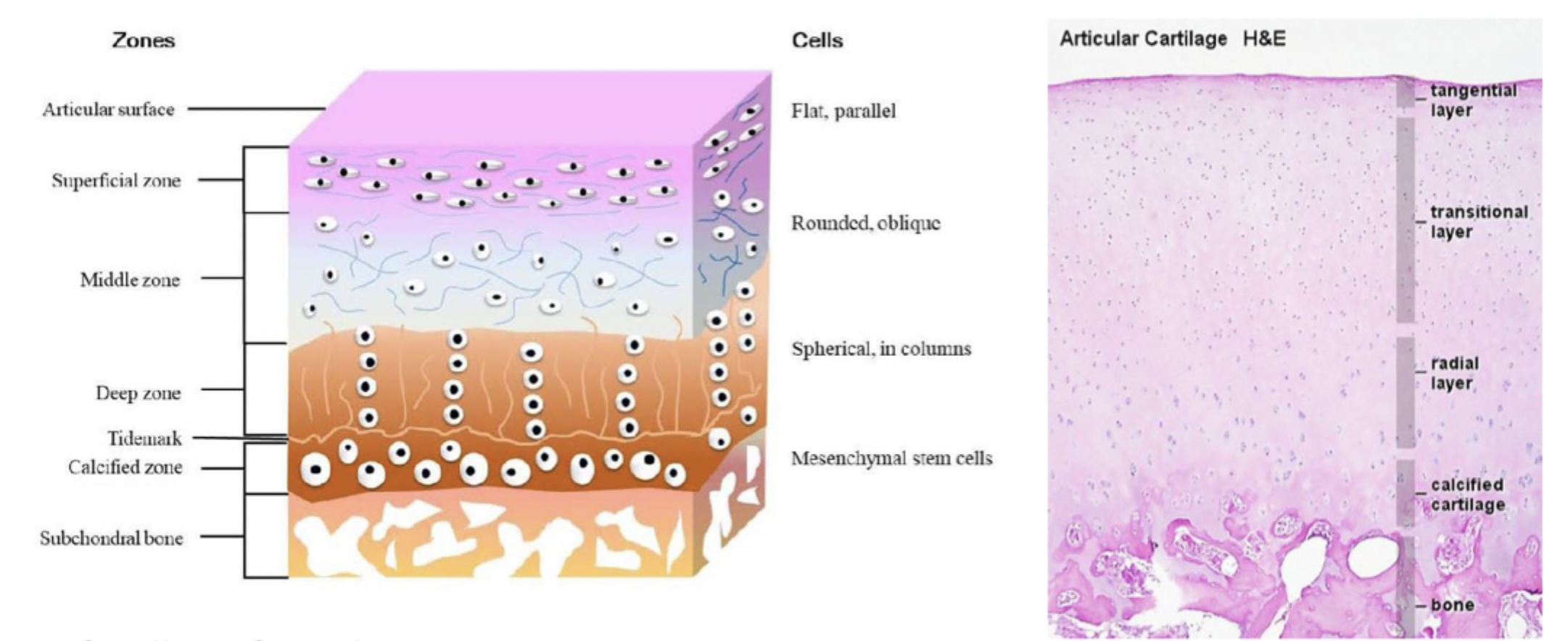
describe the deep (radial) zone of articular cartilage
Chondrocytes arranged in columns
Collagen fibers perpendicular to the surface
Provides the greatest resistance to compressive loads
Why “radial”?
The collagen fibers are oriented perpendicularly (radially) to the articular surface.
This orientation resists compressive forces transmitted through the joint.
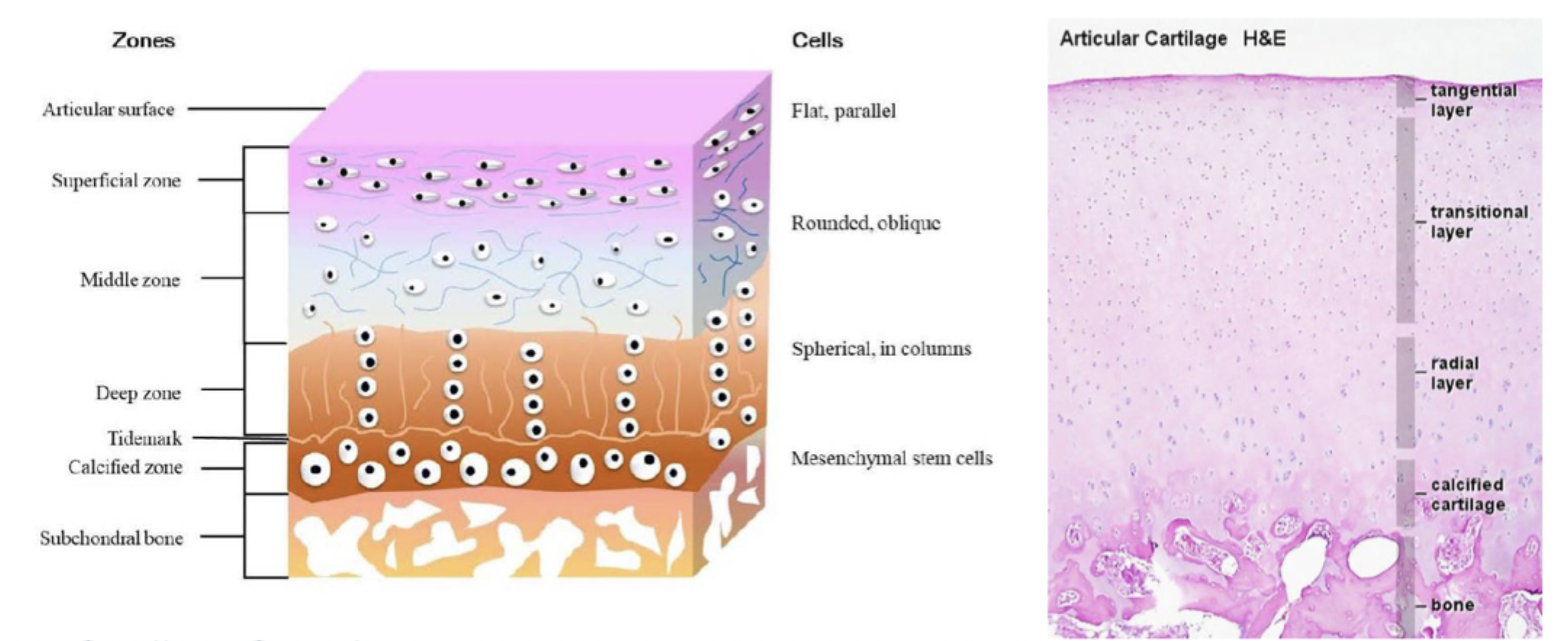
describe the calcified zone of articular cartilage
Anchors cartilage to subchondral bone
Contains mineralized matrix and hypertrophic chondrocytes
Separated from deep zone by the tidemark (a histological boundary)
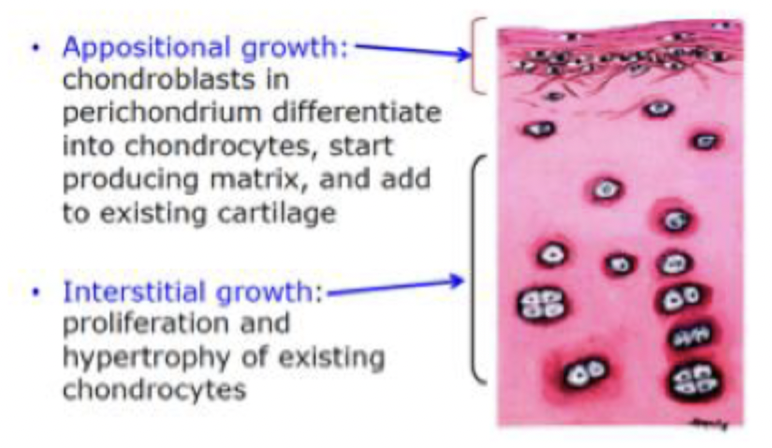
what are the two types of cartilage growth?
appositional growth
interstitial growth
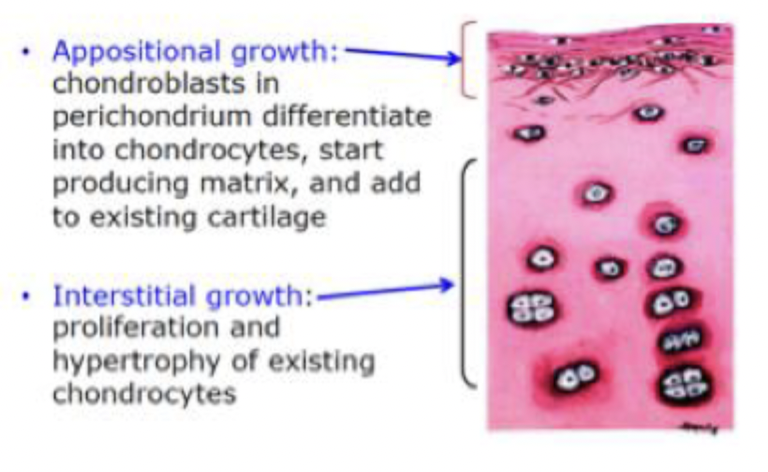
what is appositional growth
Growth at the surface of existing cartilage
Involves chondroblasts derived from progenitor cells in the inner perichondrium
Chondroblasts secrete extracellular matrix and mature into chondrocytes
Results in increased cartilage width (thickness)
Requires a perichondrium → does not occur in articular cartilage or fibrocartilage
Important in cartilage repair and postnatal growth.
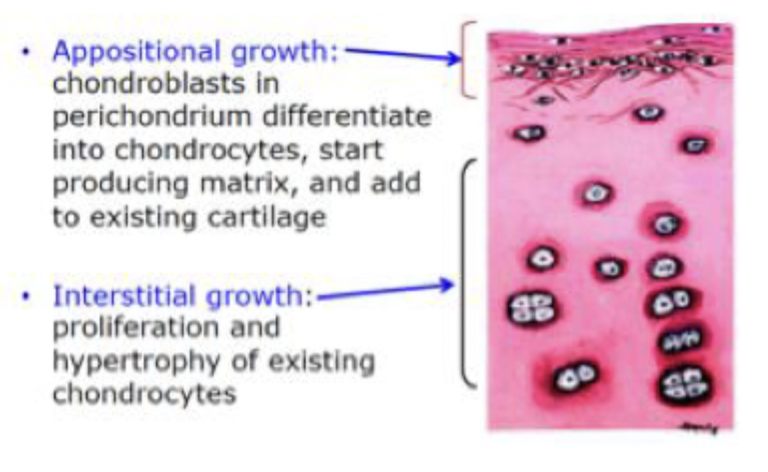
what is interstitial growth?
Growth from within the cartilage (independent of the perichondrium)
Involves chondrocytes dividing in their lacunae
Daughter cells form isogenous groups
Expands cartilage internally and increases length and volume of cartilage
Important in early cartilage development and in cartilage lacking perichondrium (e.g., articular cartilage, fibrocartilage)
explain the repair of hyaline cartilage
Very limited repair capacity, even after minor injuries
Impaired healing due to:
Avascularity
Immobile chondrocytes
Low proliferative ability of mature chondrocytes
Repair only occurs if the perichondrium is involved:
Progenitor cells from the inner perichondrium may respond
Results mostly in dense connective tissue, not new cartilage
Articular cartilage, which lacks perichondrium, shows no true regeneration
Molecular repair is minimal and uncoordinated:
Dominated by scar tissue (type I collagen)
Limited restoration of normal type II collagen matrix
Chronic damage leads to cartilage loss, joint space narrowing, and formation of bone spurs (osteophytes)

explain the calcification of hyaline cartilage
Hyaline cartilage can undergo calcification, particularly as part of aging or during endochondral ossification.
This process involves mineralization of the extracellular matrix.
Chondrocytes hypertrophy, secrete enzymes (e.g., matrix metalloproteinases), and initiate deposition of calcium salts.
Calcification leads to matrix hardening and eventual cell death (chondrocyte apoptosis).
In the skeleton, this is a normal step in the transformation of cartilage into bone during development.
In adults, pathologic calcification may occur, often contributing to cartilage degeneration (e.g., in osteoarthritis).