Anatomy and physiology of cardiovascular system
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
49 Terms
Key components of CV system
blood (liquid)
Blood vessels (pipe)
Heart (pump)
How much body mass does blood make and how much in M and F?
8% body mass
M = 5-6L
F = 4-5L
What are the functions of blood?
transportation
Homeostasis
Protection
Describe transportation - function of blood
transport O2 from lungs to body cells and CO2 back to lungs
Transport nutrients from GI tract to body cells
Transport hormones from endocrine glands to body cells
Transport heat and wasted products to lungs, kidneys and skin for elimination from body
Describe homeostasis - function of blood
control pH through buffer
Adjust temp
Osmotic pressure to control water content of cell
Describe protection - function of blood
white cells and Ab can be carried to pathogens to protect against infection
Blood can clot to protect against excessive loss and then form barrier for protection from infection
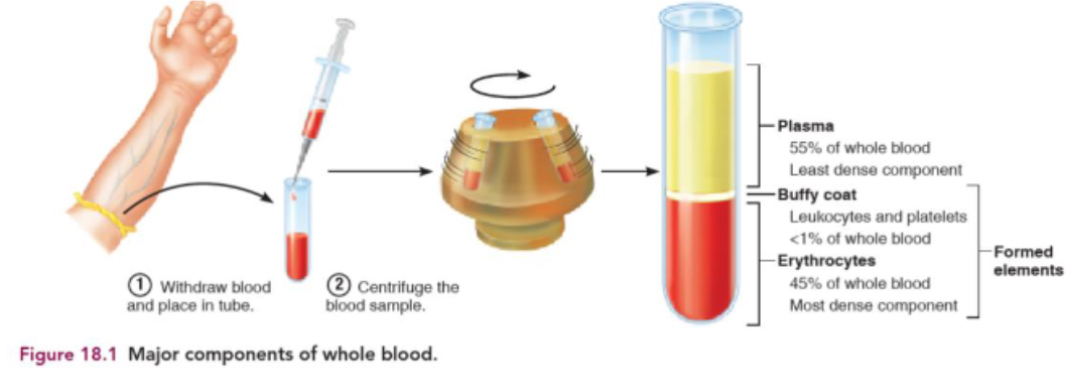
Components of blood and quantity
blood plasma - 55%
Erythrocytes RBC - 45%
Leukocytes WBC - <1%
Platelets - <1%
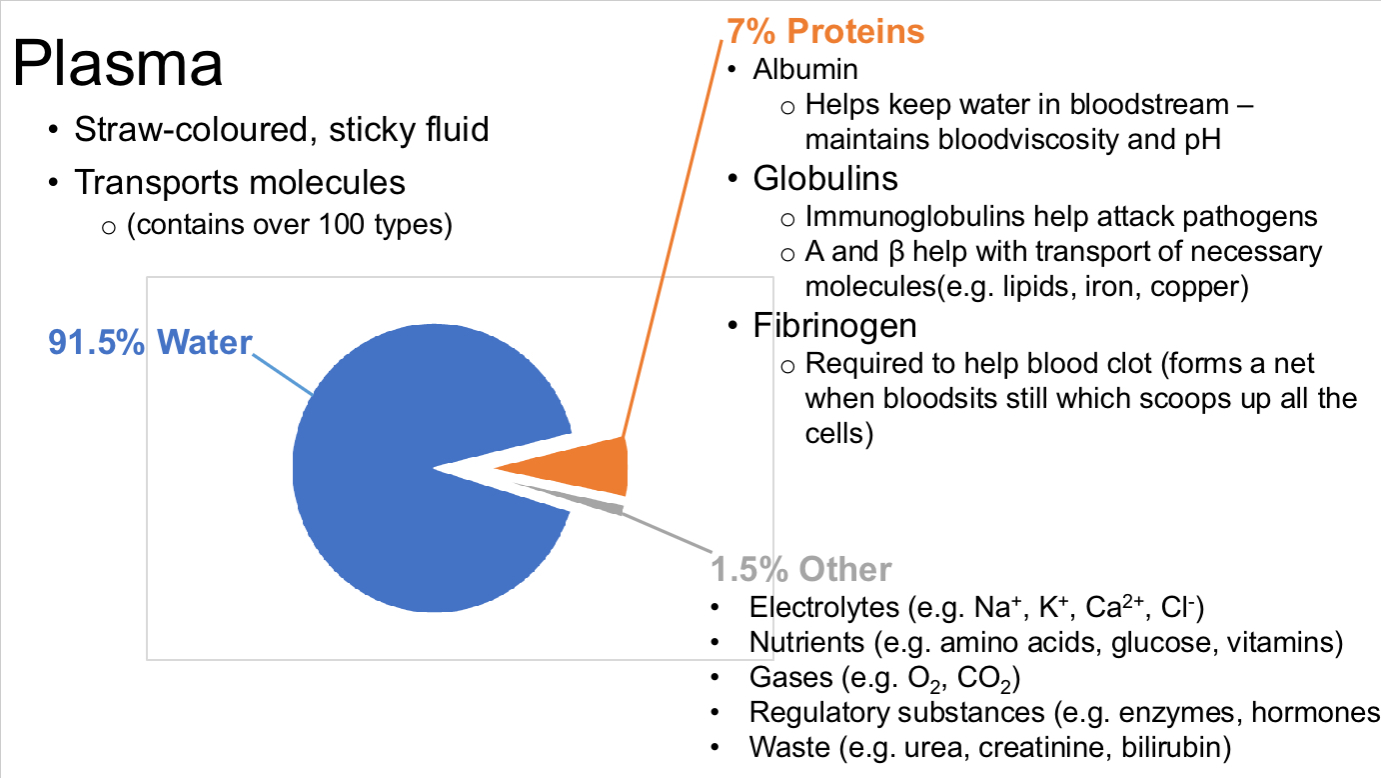
Describe plasma and what it is made out of?
Straw coloured sticky fluid
Transport molecules - over 100 types
Made from : 91.5% water, 7% protein, 1.5% others
Draw pie chart of components of plasma and describe what each is made of I.e what proteins and their functions, for others what’s in it?
What are erythrocytes? And structure?
Oxygen carrying cells:
cytoplasm packed w/Hb
Hb has single Fe2+ ion which reversible binds to O2
Biconcave shape:
provide 30% more SA than sphere
Allow more rapid o2 diffusion
No nucleus/organelles:
exclude H2O, 97% RBC is Hb
Generate energy anaerobically so don’t use up O2
Live for 100-120 days
replacement can be slow for this reason
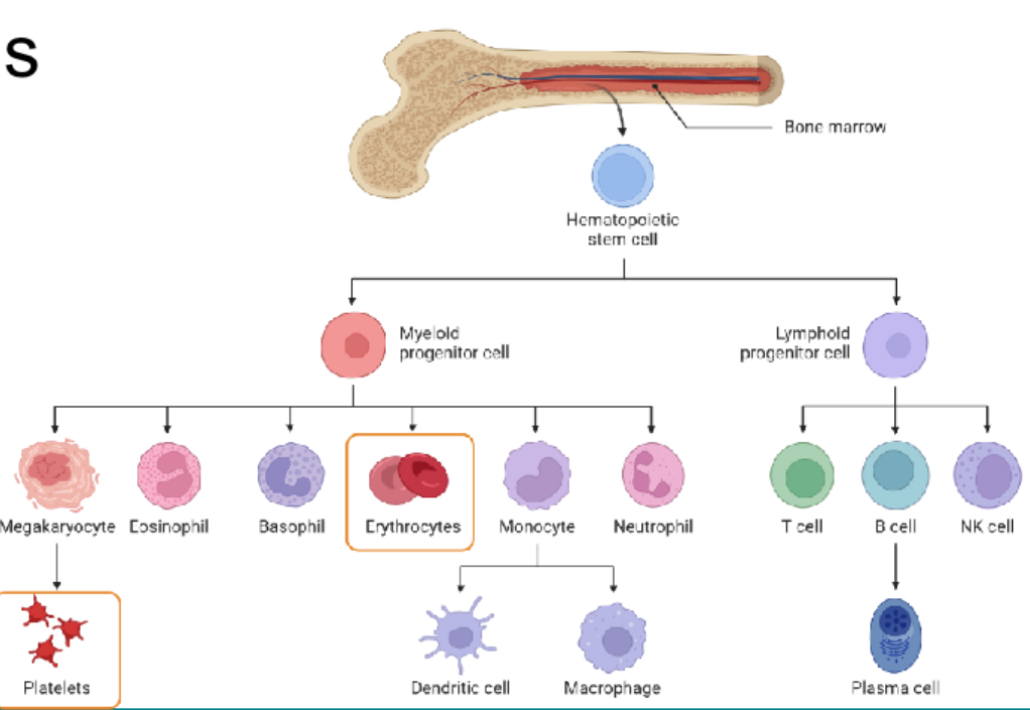
What are leukocytes and what are 5 types and their functions
WBC
Mobile part of immune system
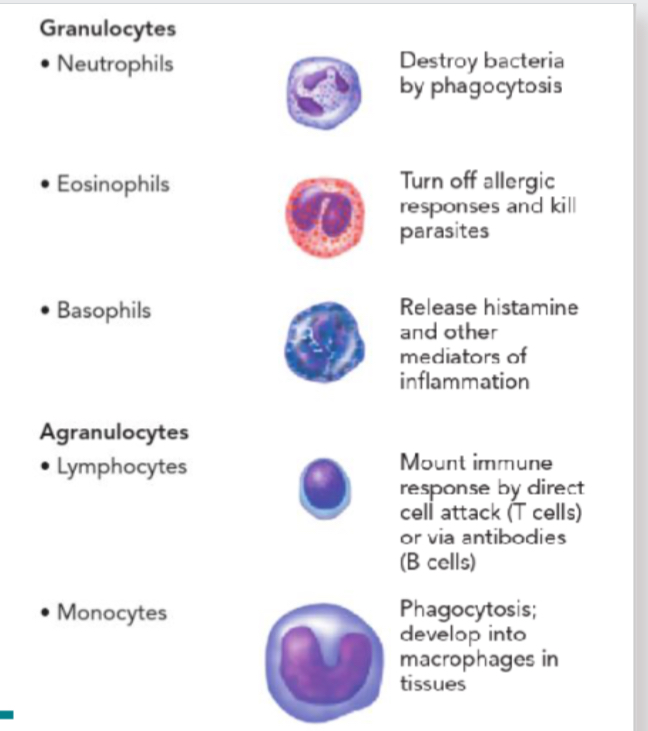
5 types of WBC
Granulocytes:
neutrophils
Eosinophils
Basophils
Agranulocytes:
lymphocytes
Monocytes
What are platelets (thrombocytes)? And functions
Fragment of cells (megakaryocytes)
cells grown huge then splinter into 2000-3000 fragments
Each fragment wrapped in membrane and is a platelet
Chemicals inside can promote blood clotting
React to tissue damage and activate - become sticky
help form clotting
Whats haematopoisesis? What do they receive? What to progenitor cells produce?
red marrow
Haematopoietic stem cells receive cytokine, erythropoietin and thrombopoietin signals
Progenitor cells produce precursors cells that become “committed” to type of blood cell
Mature cells enter blood stream (diapedesis)
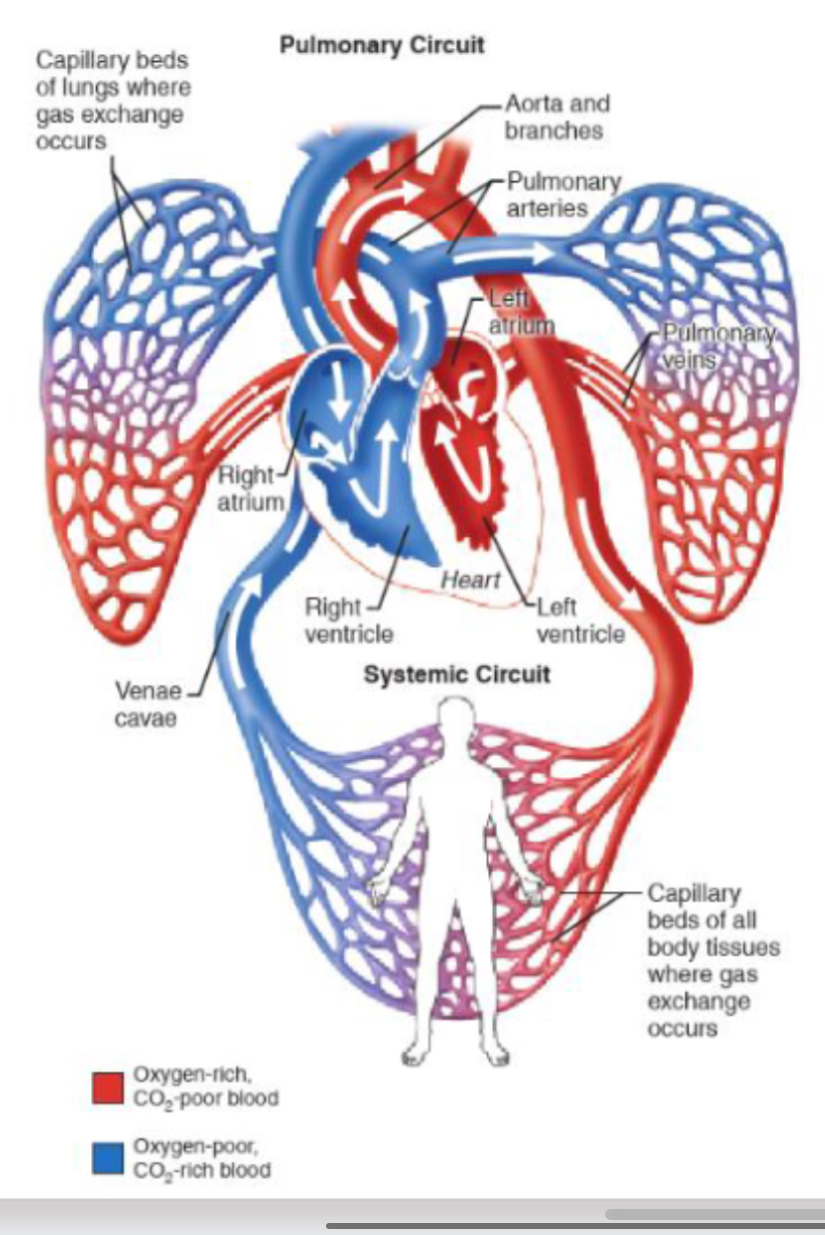
What are the 2 distinct circuits that blood never leaves?
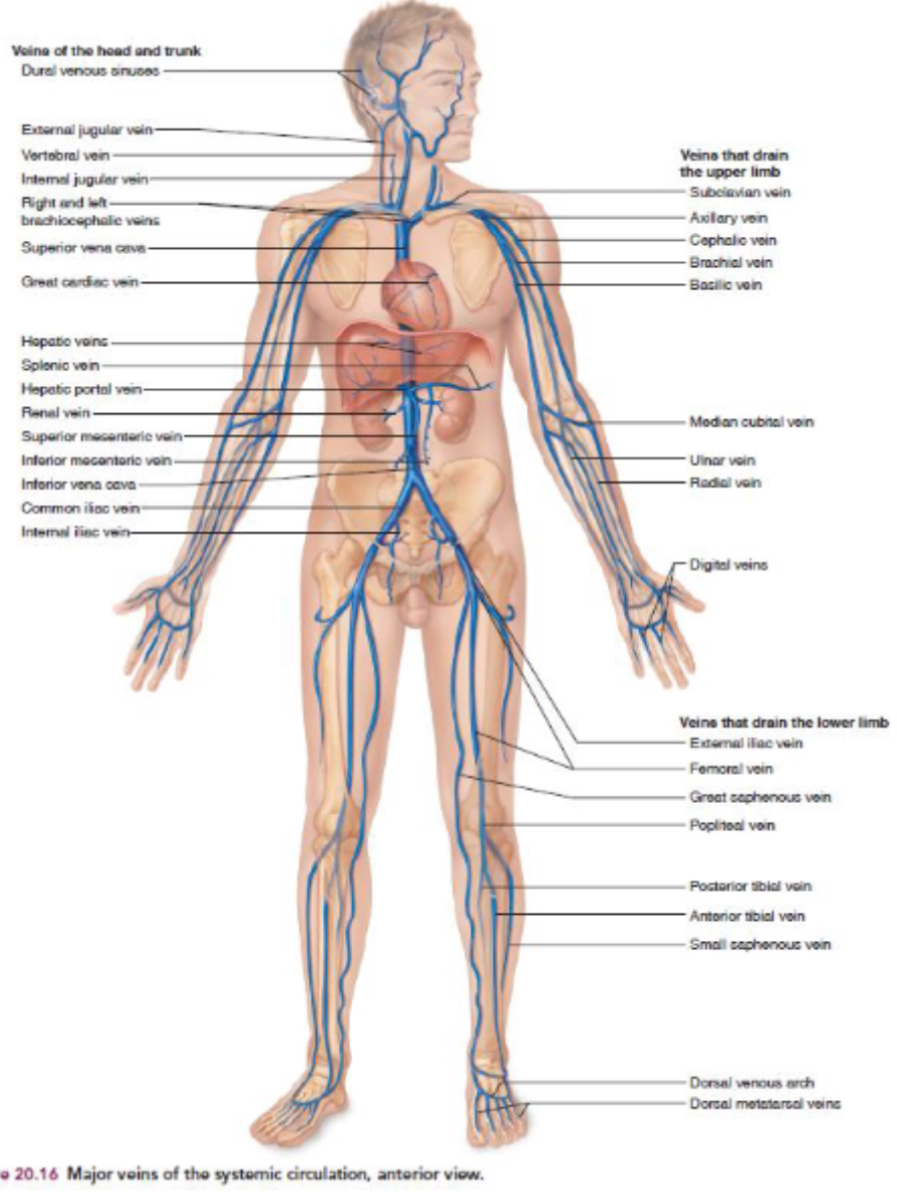
Systemic circulation:
oxygenated blood pumped out of heart through aorta
Blood returns to heart via vena cava
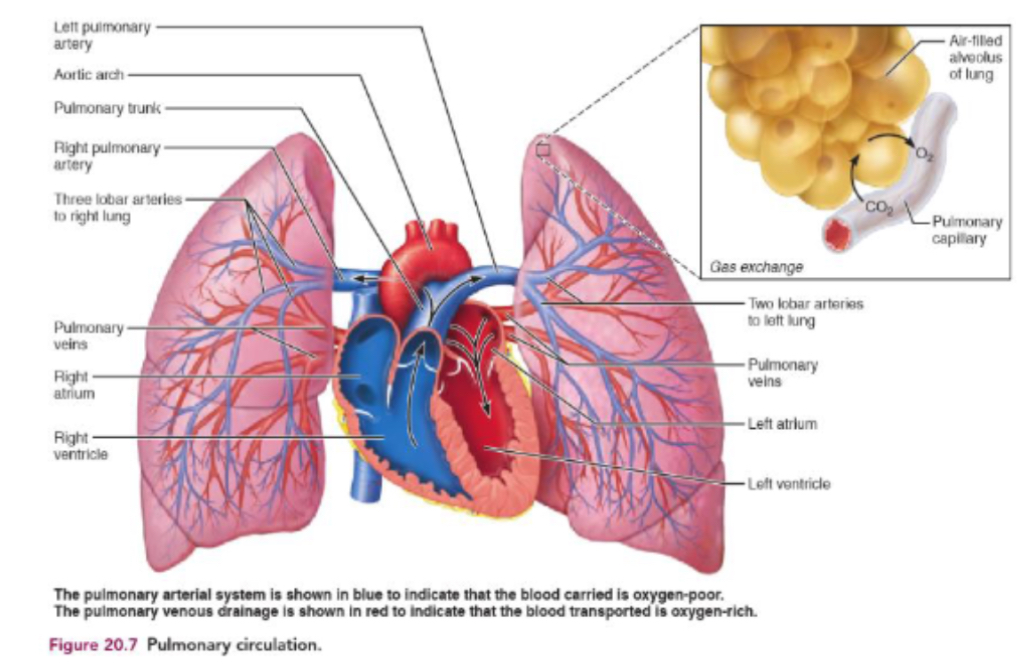
Pulmonary circulation:
deoxygenated blood pumped through pulmonary artery to lungs
Blood returns to heart via pulmonary vein
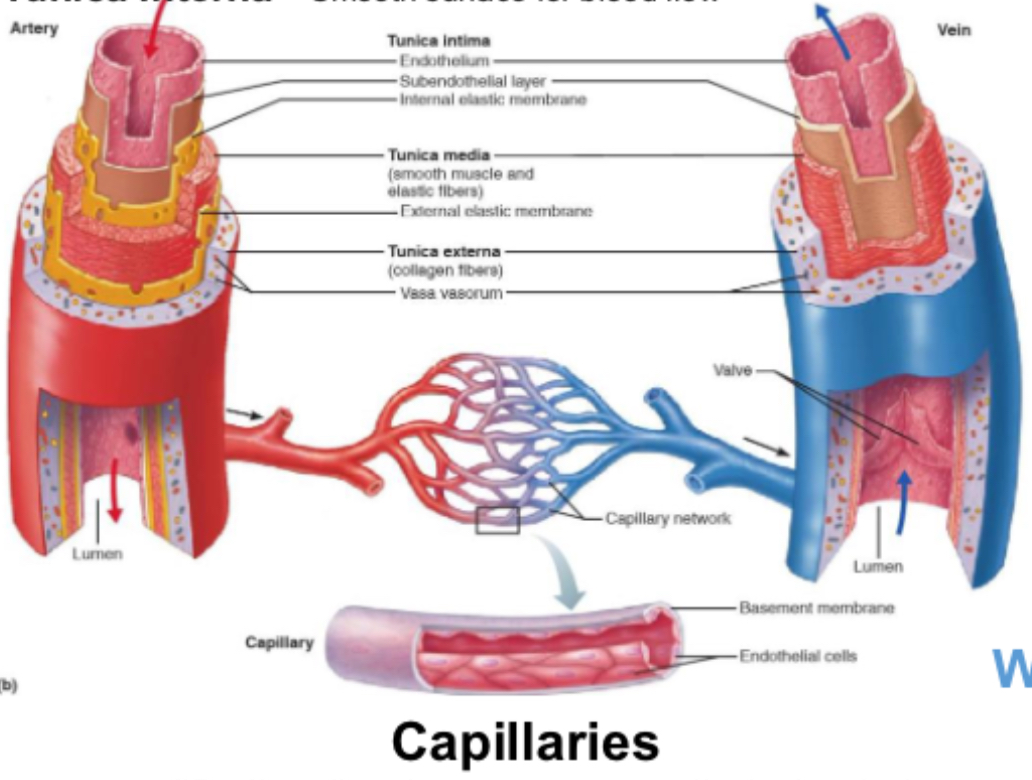
Describe arteries and structures
away from heart
Thicker muscle
Higher BP
Muscle contracts forcing blood through
Thicker walls allow them to withstand high pressures
Describe veins and structure
toward heart - in
Thinner muscle
Lower BP
Presence of valves to prevent backflow
Thinner walls so catch withstand high pressure but good at adapting to different blood volumes
Veins primarily rely on heart pumping to move blood but veins in lower limbs also use contraction of muscles.
What is tunica intima, media, externa
Tunica intima - smooth muscle for blood flow
Tunica media - smooth muscle and elastic tissue control vasodilation and vasoconstriction
Tunica externa - thick layer of connective tissue to protect vessels
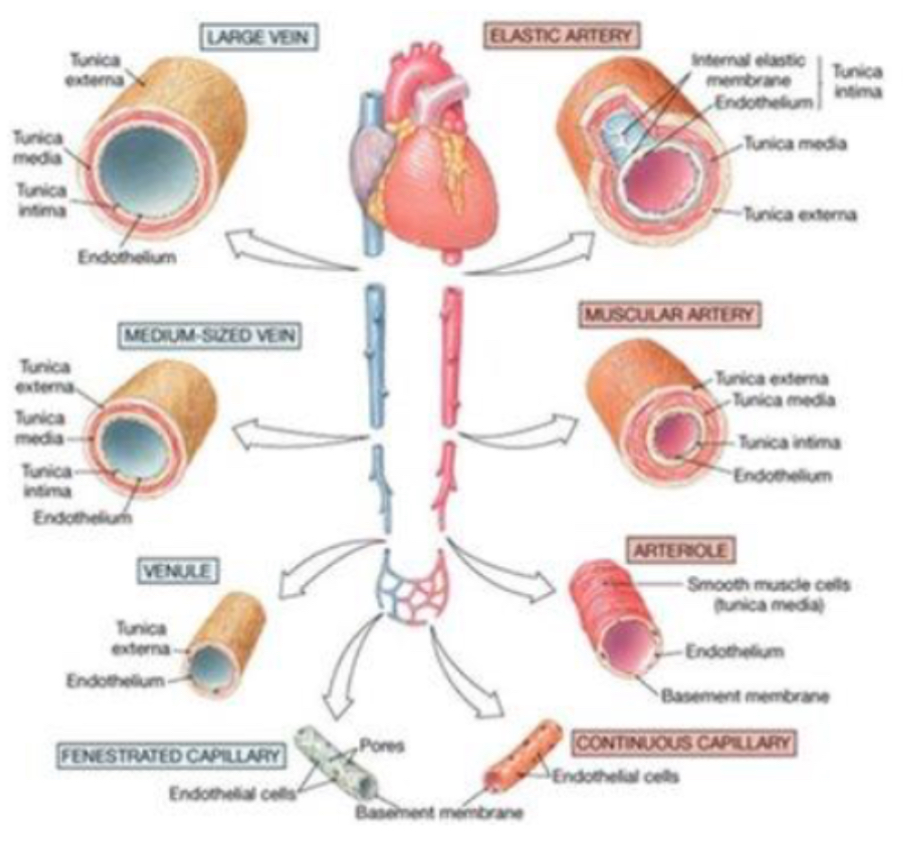
Whats a distributing artery?
Medium sized artery that carries oxygen rich blood from large arteries to specific organs or body parts.
Has thick muscular walls to control blood flow by tightening or relaxing.
E.g brachial artery, radial artery
Whats a conducting artery?
Large arteries that carries blood directly from heart and stretches to handle high pressure,
Has elastic walls that expand and recoil to help smooth out blood flow.
E.g aorta, carotid artery
What are small arteries?
Arteries smaller than distributing arteries that array blood to even smaller vessels called arterioles.
Have thick muscular walls to help regulate blood flow and blood pressure before blood reaches capillaries.
Control blood flow into capillaries
What are little veins?
Venules small blood vessels that collect deoxygenated blood from capillaries and carry towards large veins.
Have thin walls and help start return of blood back to heart.
Drain capillaries blood
Features of large veins to elastic artery photo
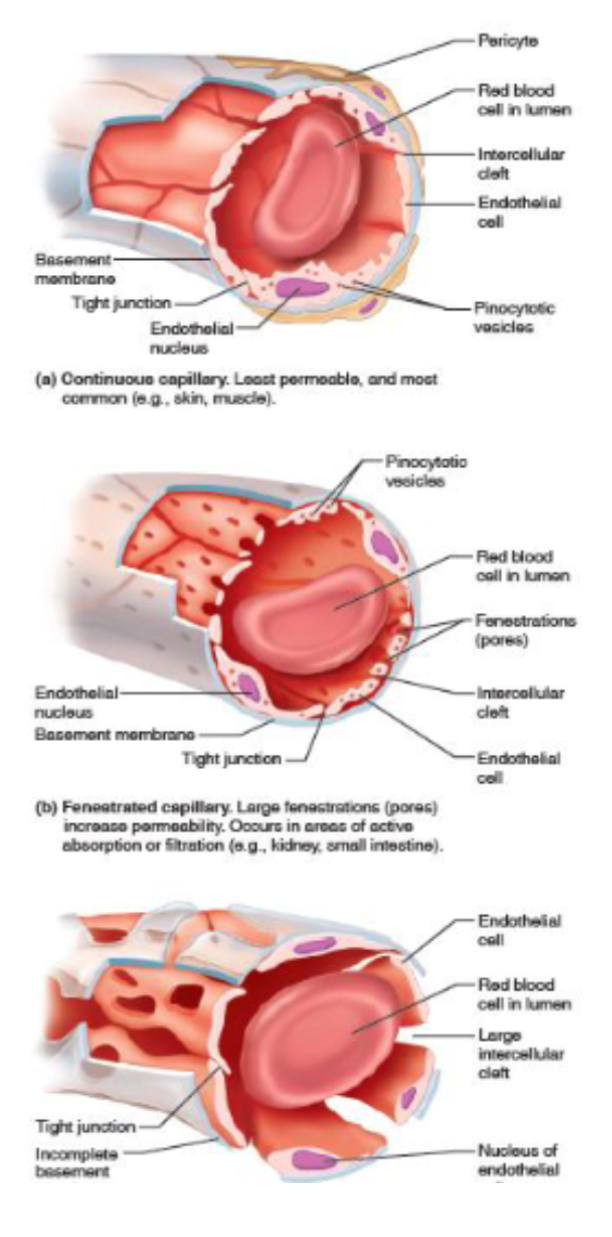
Whats a capillary and 3 kinds?
deliver substances to cells in body in extensive interconnected networks
3 kinds:
Continuous - least permeable - substances leave/enter through intercellular clefs. —> CNS,lungs,skin,skeletal and smooth muscle, connective tissue
Fenestrated: more permeable - pores (fenestrations). Allows more substances to diffuse —> kidneys, small intensive, brain, eyes, endocrine glands
Sinusoid - most permeable - wider and large fenestrations without full membrane surrounding them —> big enough for blood cells to pass through e.g RBC from bone marrow
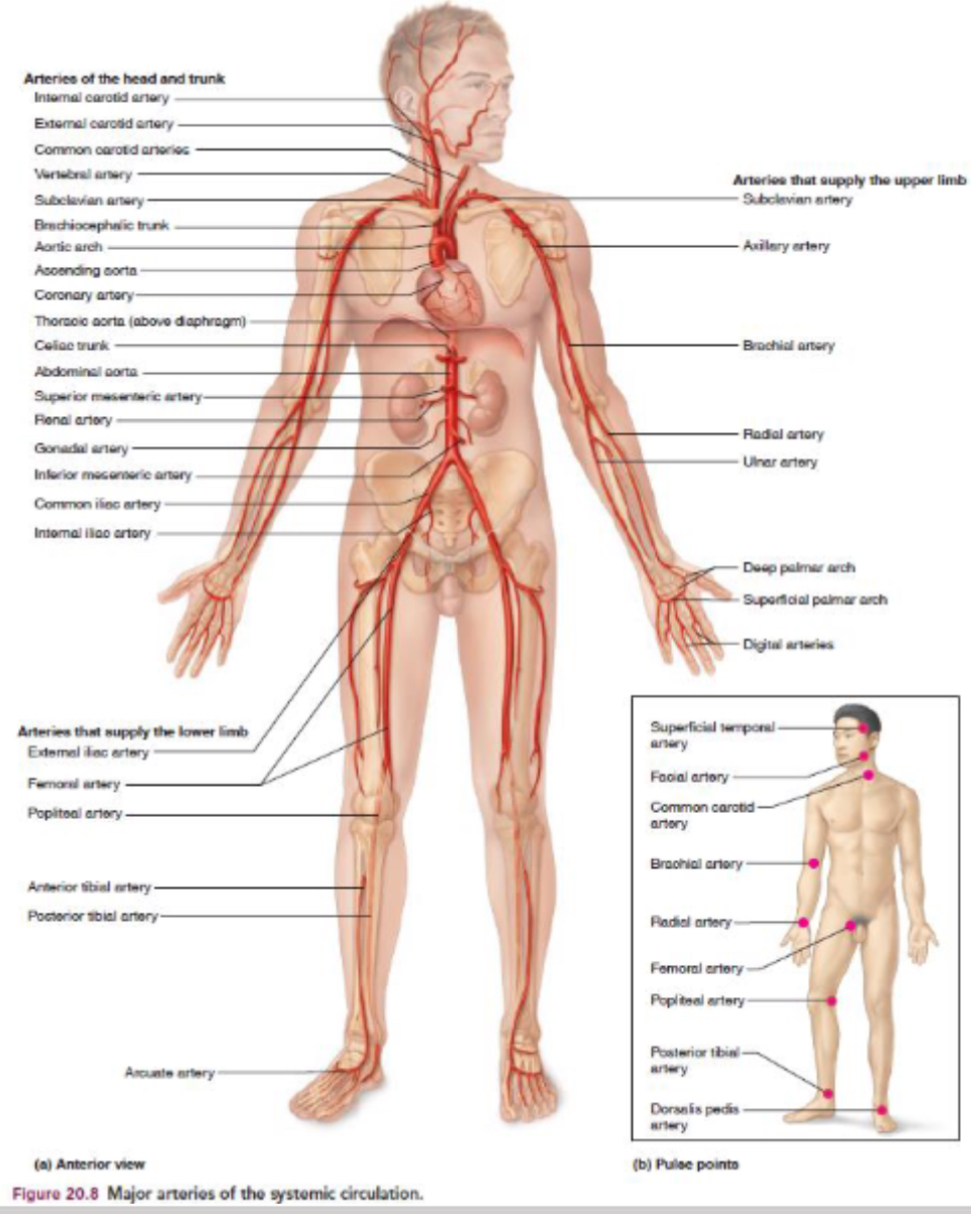
What do arteries and veins carry in systematic circulation?
Arteries = carry oxygenated blood
Veins = deoxygenated
What do arteries and veins carry in pulmonary circulation?
Only in pulmonary circulation are arteries deoxygenated (blue) and veins oxygenated (red)
Location of heart to sternum, diaphragm, lungs
Posterior to sternum
Superior to diaphragm
Medial to lungs
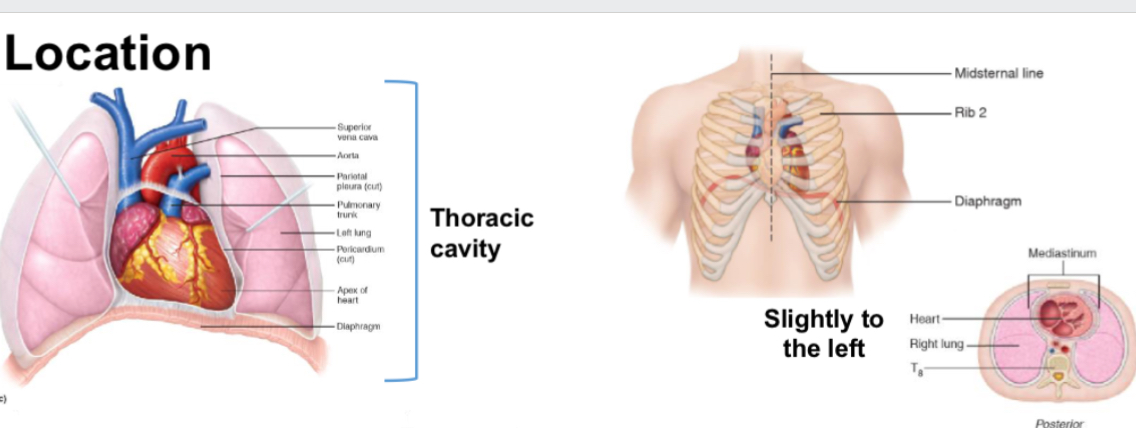
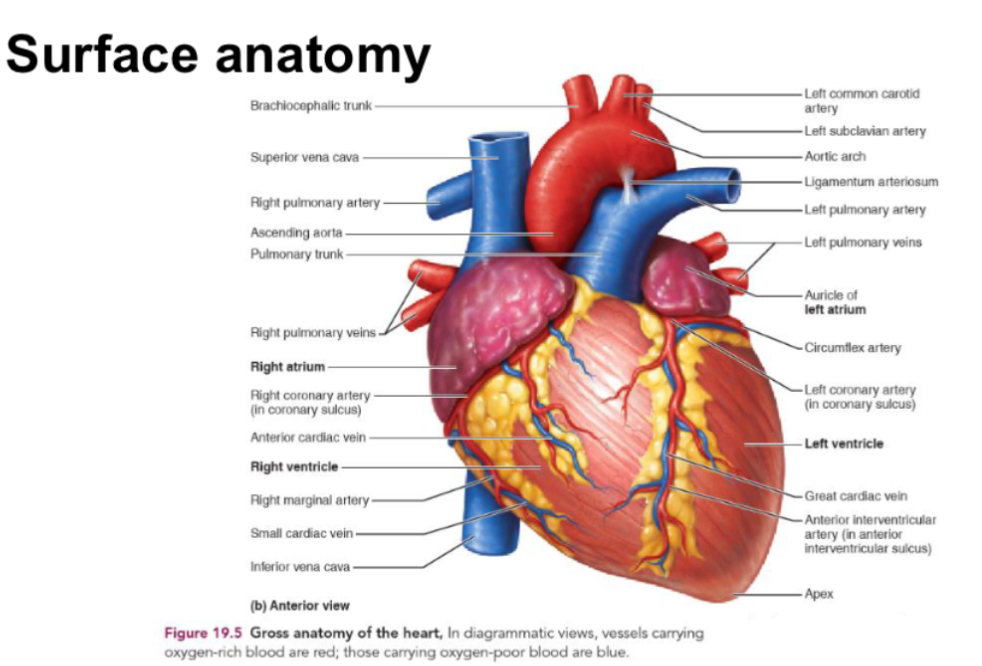
Draw rough what heart looks like and surface anatomy
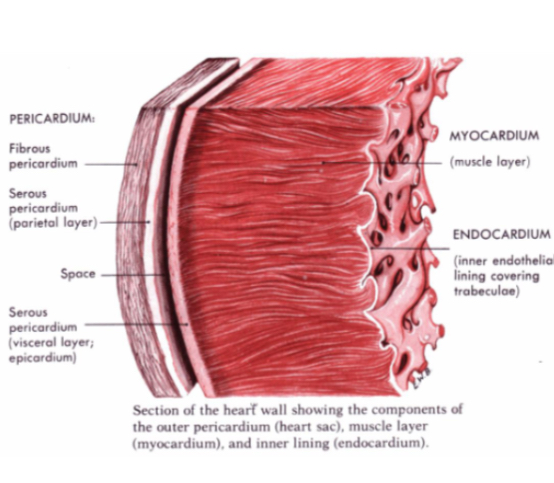
What 4 things is heart wall made out of?
Pericardium
Epicardium
Myocardium
Endocardium
Describe structure of 4 tissues in heart
Pericardium
protective membrane w/ multiple layers of connective tissue, fluid filled to reduce friction. Keeps heart in position whilst allowing movement for breathing
Epicardium:
connective and adipose fat tissues for protection - fat accumulates here during to weight and age
Mycocardium:
thickest part of wall (95%), cardiac muscle that contracts for heart beats
Endocardium:
interior lining covering valves also. Thin smooth layer which minimised surface friction w/ blood.
What are the 4 chambers of the heart?
Left atrium - receives oxygenated blood from lungs
Right atrium - receive deoxygenated blood from body
Right ventricle - blood to lungs
Left ventricle - blood to body
Which heart chamber has least muscle? Which has more and why? Whats brachial systemic and pulmonary systolic BP?
atria has least muscle as only needs to move blood to next chamber
Ventricles needs more muscle to push blood out of heart
Muscle of left ventricle substantially thicker to allow for even stronger force of contraction.
Brachial systemic artery systolic BP = 120mmHg
Pulmonary artery systolic BP = 12mmHg
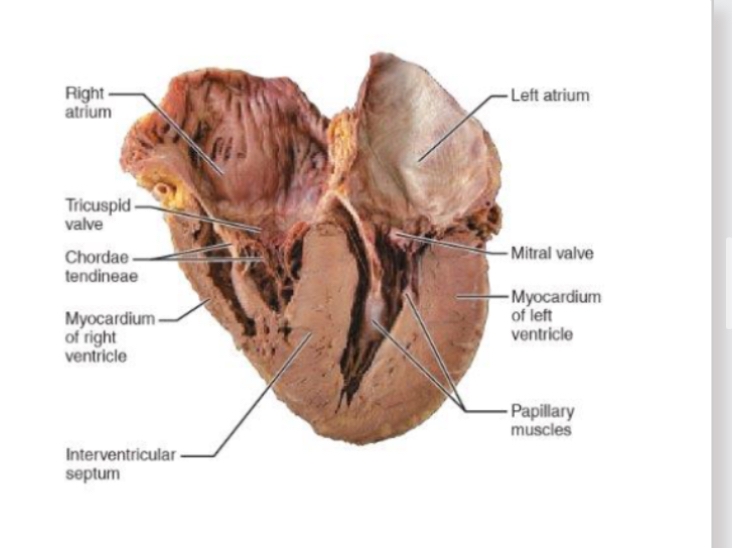
What are valves? What do they do?
prevent blood from flowing backwards by only opening one way
Open and close dependent upon pressure e.g mitral opens when pressure higher In atria than ventricles and close when reverse is true
“Slam” closed which can be heard with stethoscope “lub dub”
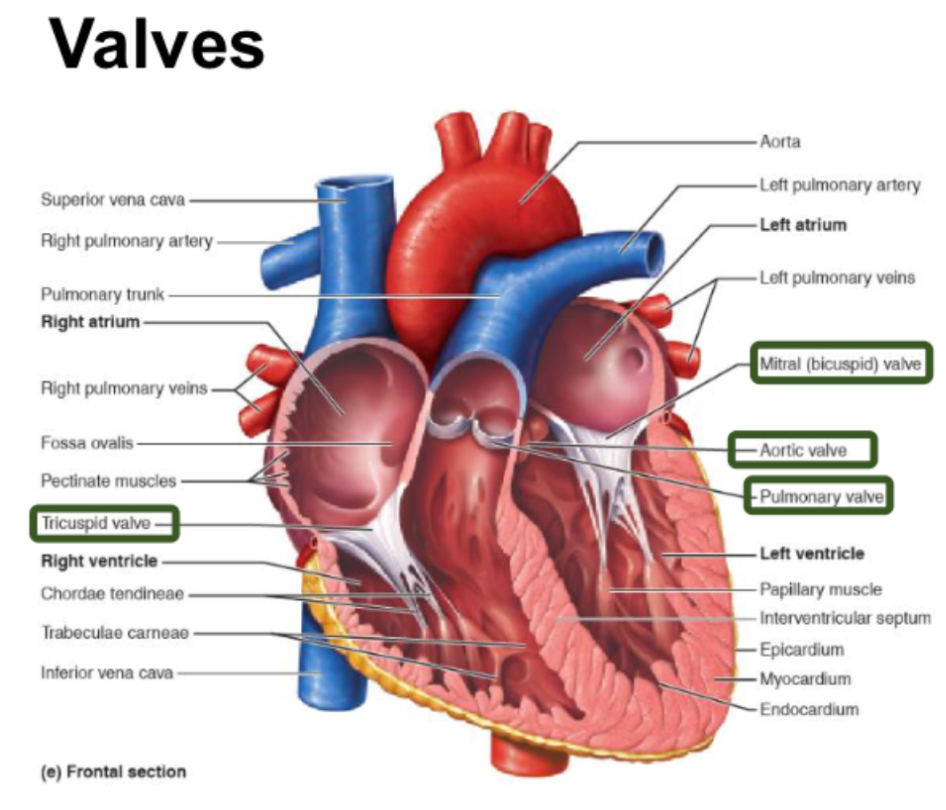
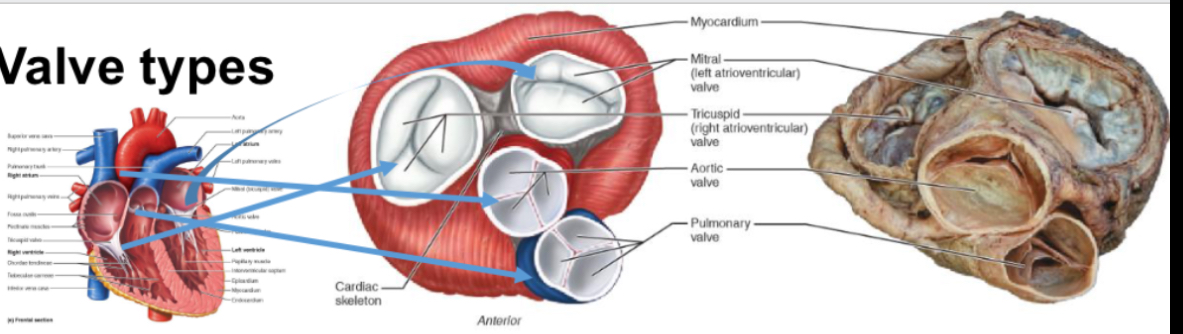
What are the 2 types of valves and functions
Atrioventricular valve:
tricuspid - 3 leaflets
Bicuspid (mitral) - 2 leaflets
Between atria and ventricles
Allow blood flow to ventricle but not back to atria
Feature chordate tendinea and papillary muscles which reinforce against pressure of ventricle contraction
Semilunar valves:
aortic
Pulmonary
Named after 3 leaflets being crescent moon shaped
Attached to arterial walls
Allow blood flow to arteries but not back to ventricles
Are there any valves from vein to atria?
No valves between atria and veins
When atria contracts some blood does flow backwards but it’s minimised by direction of contraction of atria
Describe blood Flow inside the heart
deoxygenated blood enters RA from vena cava (back from rest of body) - end of systemic circulation
RA contracts and forces tricuspid valve open as pressure in atrium is higher than pressure in ventricle
Deoxygenated blood pushed by RA into RV
RV contract, pressure causes tricuspid valve to close
Pulmonary valve opens
Deoxygenated blood pushed into right ventricle into pulmonary arteries
Blood travels to lungs - beginning of pulmonary circulation
Oxygenated blood enters LA from pulmonary vein - end of pulmonary circulation
LA contracts and cause mitral (bicuspid) valve to open
Oxygenated blood pushed by LA into LV
LV contracts and forces mitral valve to close
Aortic valve opens
Oxygenated blood pushed by LV into aorta
Blood travels around body - beginning of systemic circulation
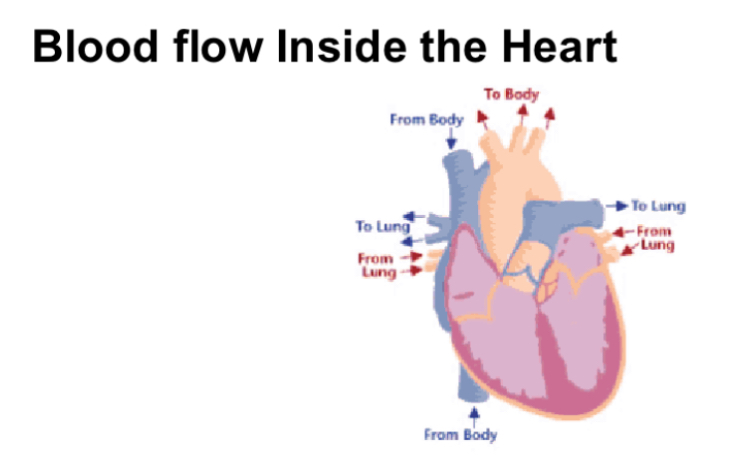
Summarise blood flow in heart
Heart relaxes
Blood flows into atria
Atria contract
Blood flows into ventricles
Ventricles contract
Blood flows into arteries
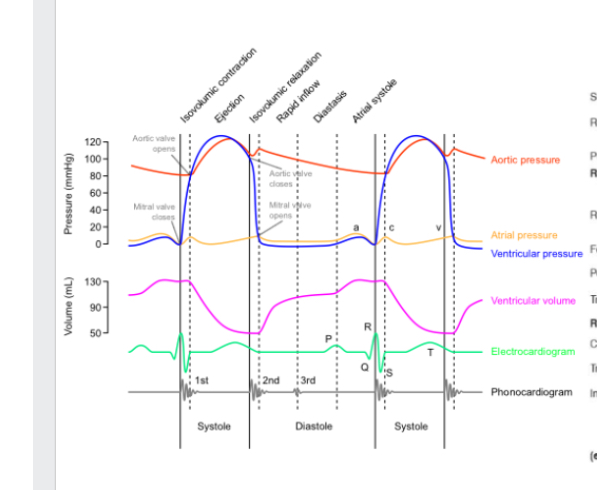
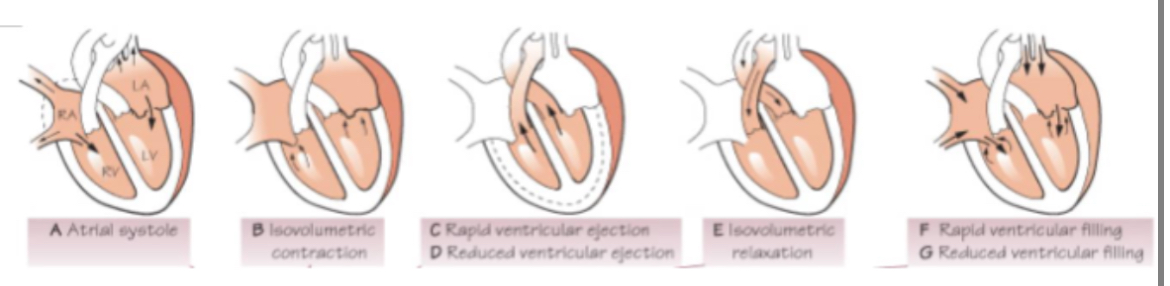
What are the 3 phases of cardiac cycle?
Atrial systole - atrial walls contract
Ventricular systole - ventricular walls contract
Diastole - relaxation of heart muscle
Systole - contraction of heart muscle (myocardium)
Describe process of electrical signalling
excitation begins at sinoatrial SA node (pacemaker) in RA and flows through RA across to LA. Signal can’t enter ventricles through walls between chambers
Signal hits Atrioventricular AV valve where it’s held for 0.1s.
AV bundle connects atria to ventricles
Signal travels down insulated routes down blunder of his and slits into left and right bundle branches. Bundle branches conduct impulses through interventricular septum
Signal travels to purkinje fibres which spread around heart muscle and aren’t insulated allowing signal to reach ventricle muscle.
Subendocardial conducting network stimulated contractile cells of both ventricles
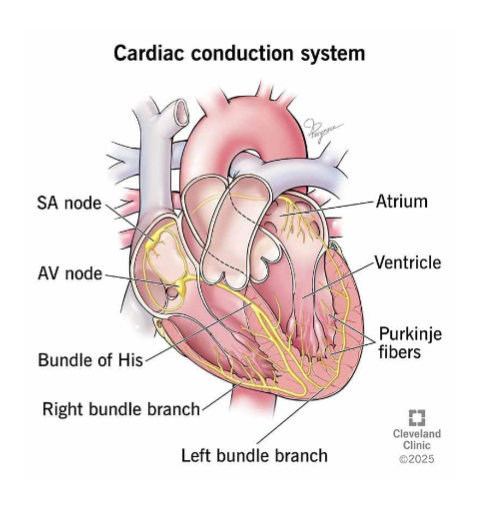
Summarise electrical signalling
SA node
Atria contract
AV node - delay
Bundle of his
Bundle branches
Purkinje fibres
Ventricles contract
What causes higher BP? Systolic or diastolic?
Systolic - 120

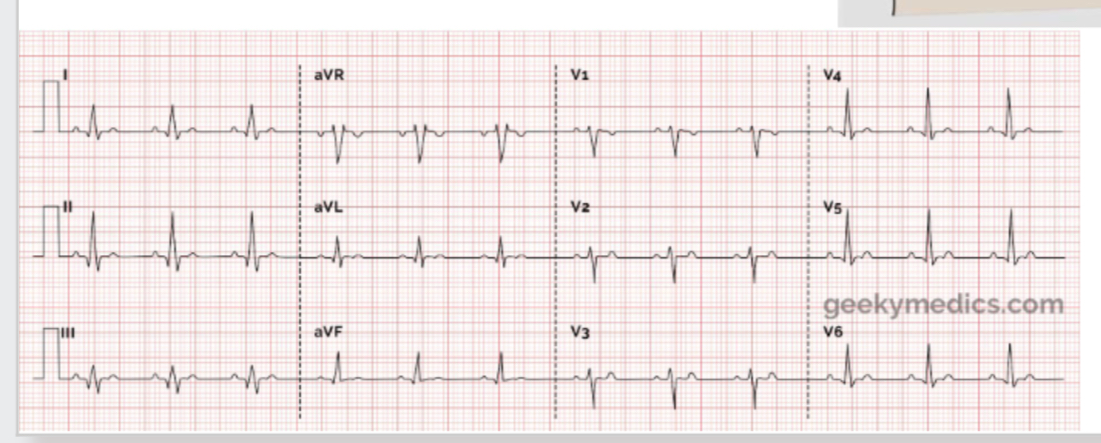
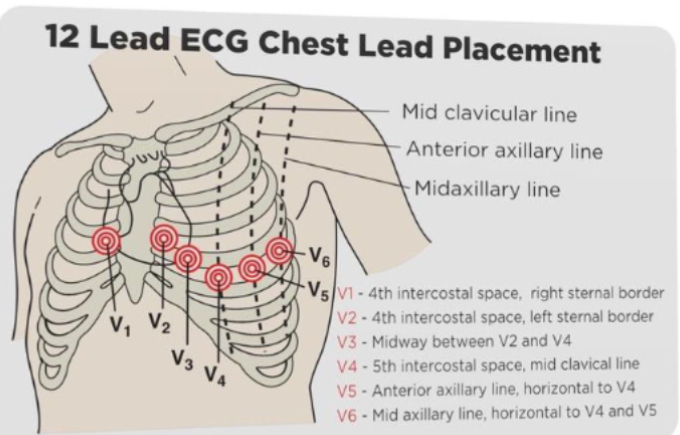
How do we measure movement of electrical current in heart?
ECG
V4 is apex
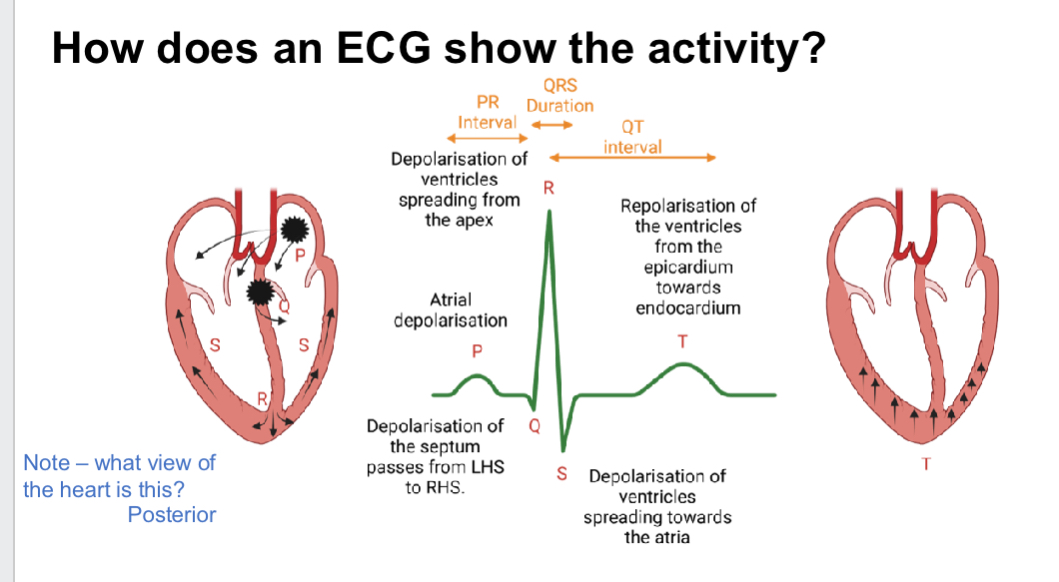
How does ECG show activity?
P QRS T
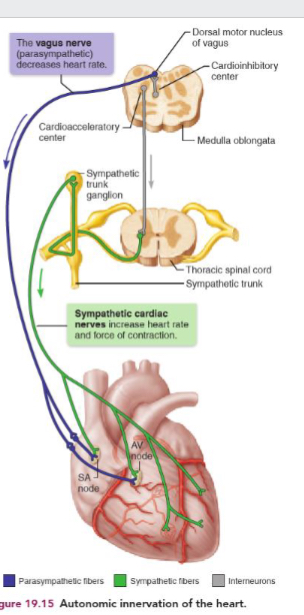
Whats autonomic and innervation? How can SA node operate and how does it link to medulla oblongata?
Autonomic = involuntary or unconscious
Innervation = stimulate an activity
Heart rate of contraction set by SA node
SA node can operate independent of signals
But rate can be altered by neural controls from medulla oblongata
Medulla oblongata receives instructions from higher brain regions e.g hypothalamus
Whats the cardioinhbitory centre and cardioacceleratory centre? Functions?
Cardioinhibitory:
parasympathetic innervation - rest and digest
Decreases HR
Restricted to SA and AV nodes and coronary arteries
Cardioacceleratory:
sympathetic innervation - fight or flight
Increase HR and strength contraction
Targets same structure as parasympathetic fibres but also project to cardiac musculature throughout heart
Whats the normal HR? How to count?
60-100 bpm
Count by pressing radius pulse on wrist under thumb for 15s then x4
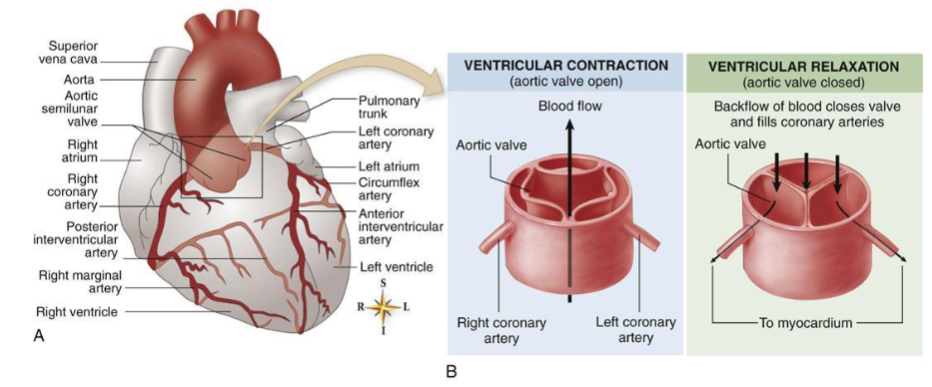
How does heart get its blood supply?
walls of heart too study for blood inside it to diffuse into tissue and there are no capillaries on inside
Provides O2 and nutrient the wall has own blood supply called coronary arteries
Heart is muscle so when works hands it needs more o2
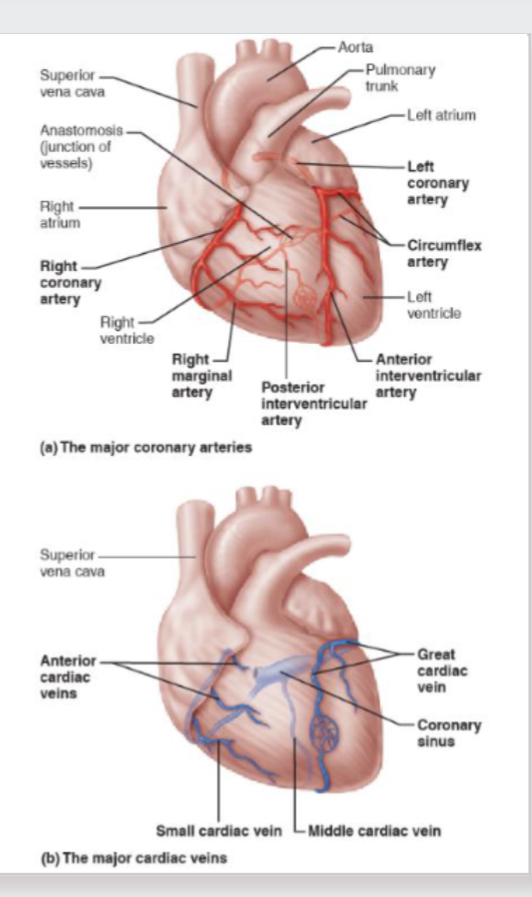
What phase does heart receive blood?
Heart only part of body that receives its blood supply in diastolic phase
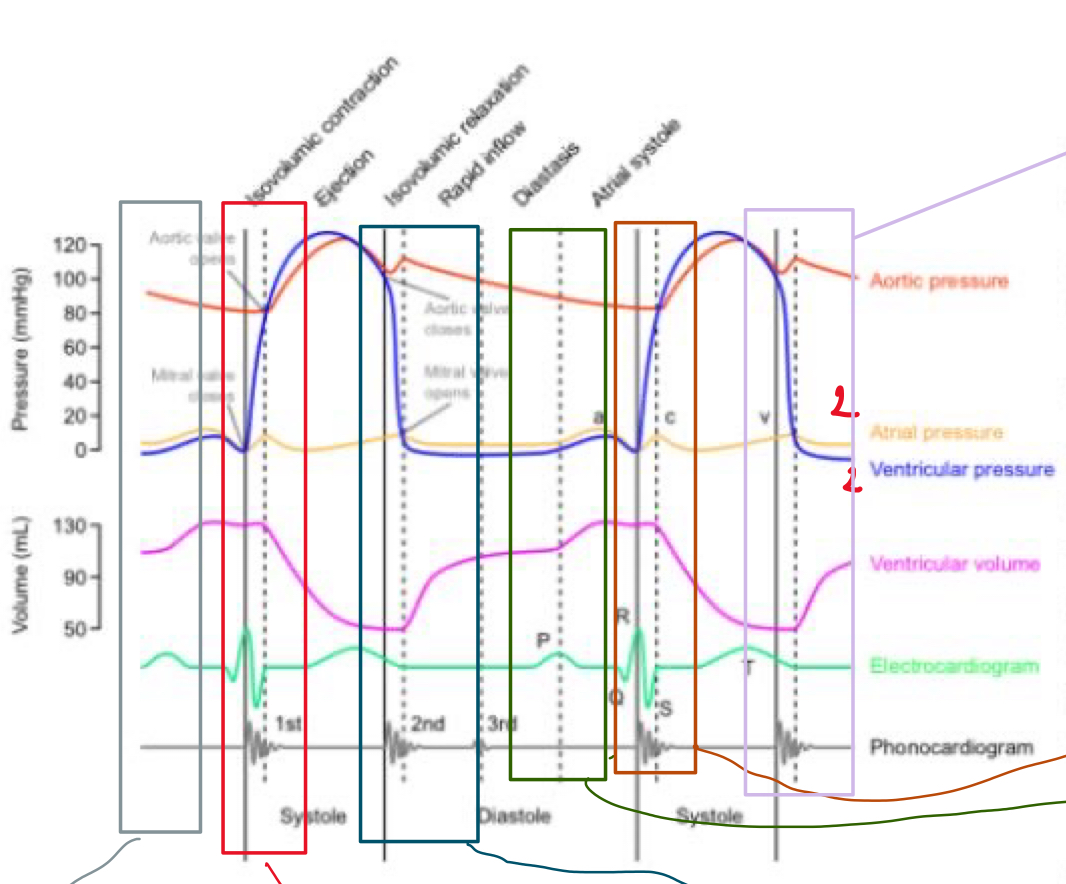
Describe what’s happening in the 6 boxes - grey, red, blue,green,orange, purple
Grey - Atrial Systole - P wave - electrical signal in L+R atria. Pushes blood into ventricles —> ventricular volume increases as blood pushed in
Red - Ventricular systole - ventricle start contracting. Pressure increases. As soon as pressure in it exceeds pressure in atria, it forced mitral + aortic valve closed —> “lub”. Then reaches point where pressure in ventricle height that in atria and that opens aortic + pulmonary valve —> blood flows into circulation. QRS complex
Blue - Diastole - relax - BP in aorta higher than in ventricles so slam shuts valves —> “dub” - blood can trickle into atria here
Green - Atrial systole - electrical signal flow through atria and pushes blood into ventricles
Orange - ventricles contract into circulation - 1st heart sound.
Purple - relaxes. Valves close. 2nd heart sound