VT 100 Lec. 4 Chemical Restraint (wk. 2)
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
35 Terms
Purposes
Advantages:
Reduces anxiety, fear related aggression, stress and struggling
Immobilization
Analgesia (pain relief)
Anesthesia (medically induced sleep)
Disadvantage:
Most are CNS depressants
Many are CV and/or respiratory depressants
Hypothermia
Injury during induction or recovery
Routes of Administration
Oral
Spray
Pill/liquid
Parenteral
S.Q. = Subcutaneous
I.M. = Intramuscular
I.V. = Intravenous
Darts
Considerations
Species
Physical factors
1. Age
2. Sex
3. Physical condition
4. Emotional status
5. Environment
Sedatives: Tranquilizers
Tranquilizers – decreased anxiety and struggling but have normal consciousness
Ace Promazine (phenothiazine) “Ace”
Depresses CNS
Anti-emetic
Potent – long lasting
Sedatives: “Pre-visit pharmaceutical” (PVP)
Trazodone
Antidepressant (SARI class)
Reduces anxiety = “anxiolytic”
Use in caution with patients that have kidney or liver disease
Gabapentin
Used to treat seizures and nerve pain
Mechanism of action is not fully understood
Inhibits excitatory neurotransmitters in CNS
Often used as sole PVP in cats
Commonly used in combination with trazodone in dogs
Sedative: Agonist
Substance that binds to a receptor and activates it
Sedative: Antagonist
Substance that binds to a receptor and inhibits activation
Sedative: Opioid Receptors
Proteins found on the surface of cells in the brain, spinal cord, and other organs
Mu (µ) receptor = abundant, analgesia/euphoria
Kappa (ĸ) receptor = regulate sedation, GI function
Delta (δ) receptor = analgesia, reward/addiction
Sedatives: Butorphanol
Opioid analgesic/sedative
Much stronger sedative
Partial mu (µ) receptor antagonist
Minimizes respiratory depression
Kappa (ĸ) receptor agonist
Causes more sedation more than analgesia
Anxiolytics (anti-anxiety): Benzodiazepines
Anti-convulsants
Muscle relaxants
Increases GABA in CNS
Examples:
Diazepam
Midazolam
Alprazolam
Anxiolytics: Diazepam
Administered PO or IV
Recommend not IM
“Lipophilic”
Dissolves readily in lipids
Slower onset of action
Longer duration
Anxiolytics: Midazolam
Administered PO, IV, IN or IM
More “hydrophilic” than diazepam
Rapid onset of action
Shorter duration
Pharmacokinetics: absorption, distribution, metabolism, excretion
Lipophilic Drugs:
Dissolves in lipid/fat
Fair absorption
Uneven distribution in fat/cells
Typically longer half-life
Hydrophilic Drugs:
Dissolves in water
Excellent absorption
Good distribution in bloodstream
Typically shorter half-life
Alpha-2 Adrenergic Agonist: Dexmedetomidine (Dexdomitor)
Causes sedation and analgesia
IM on aggressive dogs
IV-sedation in 3-5 min; IM -5 to 10 min
Often mixed with opioid
Reversible
Antisedan (also reverses analgesia)
Alpha-2 Adrenergic Agonist: Xylazine (Rompun)
Sedative/analgesic
CNS depressant
Increased CV effect
Can be given IV or IM
Commonly used in equine/large animal for standing sedation (ie: dental, sheath cleaning)
Alpha-2 Adrenergic Agonist: Detomidine (Dormosedan)
Sedative and analgesic
Longer duration than other alpha-2 agonists
Administered IV, IM or transmucosally (PO)
Can cause bradycardia and hypovolemia
Dissociative Anesthetics: Ketamine
Sedation -> General anesthetic
NMDA antagonist
Short duration of action
Provides analgesia too
Often used as induction drug in combination with a benzodiazepine/alpha-2 agonist
Dissociative Anesthetics: Telazol
Equal parts zolazepam (benzodiazepine) and tiletamine (dissociative)
Long duration of action
Used often with pigs and companion animals
Administered IV, IM, IN, PO
TIVA = Total Intravenous Anesthesia
Using multi-modal approach to maintenance of general anesthesia with minimal cardiovascular depression
Using agents that are not cumulative (have a relatively short half-life)
Using agents that are reversible
PIVA = Partial Intravenous Anesthesia
Using multi-modal approach to maintenance of general anesthesia by minimizing the required MAC (mean alveolar concentration) to improve cardiovascular CRI (constant rate infusion) often used to maintain lowest MAC
Lidocaine, ketamine, fentanyl, morphine
Often “MLK” or “FLK” – all three used together as CRI
General Anesthesia Definition
“a state of medically-induced, reversible unconsciousness that provides pain relief and muscle relaxation for surgical procedures, keeping patients unaware of the procedure and allowing for control of breathing and other vital functions”
General Anesthetics: Anesthetic Gases
Isoflurane, Sevoflurane
Intubation necessary
Metabolized through lungs
Rapid adjustment of doseand effect
Causes vasodilation and hypotension
Try to minimize inhalant dose with multi-modal anesthesia
General Anesthetics: Barbiturates
Pentobarbital
Used as primary euthanasia drug
Not safe as an anesthetic
Narrow margin of safety
No longer used
Phenobarbital
Used primarily as treatment for epilepsy
General Anesthetics: Propofol (Rapinivet)
Used for sedation, induction and/or anesthetic maintenance by repeated bolus injection or CRI
IV administration only.
Minimal CV effect.
Transient apnea
General Anesthetics: Alfaxalone (Alfaxan)
Neuroactive steroid
Affects GABA receptor
Rapid onset
Short duration of action
Minimal CV effects
Opioids
Provide sedative, hypnotic and analgesic properties
Decrease respiration
Causes bradycardia
Impair thermoregulation
Hypersensitivity to noise
Can be given SQ, IV, IM, PO or transdermal
Varying duration of action
Types of Opioids
Hydromorphone
Fentanyl
Butorphanol
Buprenorphine
Morphine
Methadone
Codeine
Opioids: mu (µ) agonist
Pure mu (µ) agonist
Hydromorphone
Fentanyl
Morphine
Methadone
Partial mu (µ) agonist
Buprenorphine
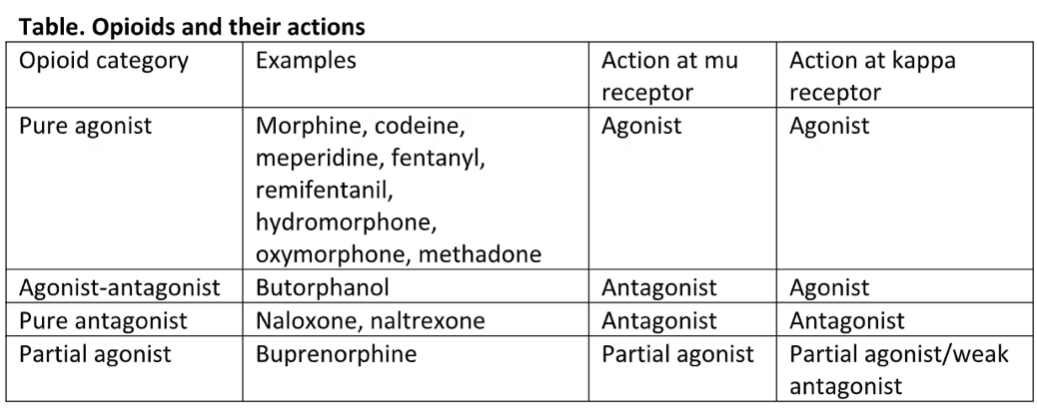
Pure mu (µ) agonist
Provides excellent analgesia
Can cause significant CV and respiratory depression
Can cause significant nausea and vomiting
Can cause excitation in cats
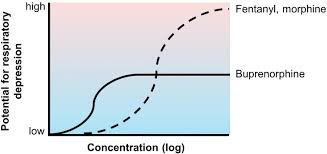
Partial mu (µ) agonist
Still good analgesia
“Ceiling effect”
Less CV/respiratory depression
Less nausea/vomiting
Buprenorphine
Long half-life, provides analgesia for up to 24 hrs or longer
New transdermal product Zorbium ideal for post-surgery analgesia for up to 4 days!
Immobilizing Agents
Important in veterinary medicine to facilitate examination, treatment and relocating of wildlife and feral animals
Requires careful drug selection, dosage calculation, and administration to account for species-specific anatomical and physiological differences
Common drug classes
Dissociative anesthetics
Ketamine, tiletamine
Opioids
Cafentanil, etorphine
Reversible (naloxone)
Alpha-2 agonists
Xylazine, medetomidine
Reversible (atipamezole)
Immobilizing Techniques
Dart Guns
These devices fire darts containing the anesthetic drugs over a distance (up to 60 yards)
Pole Syringes
Used for closer distances or physically restrained animals, these devices allow for hand injection or delivery via pressurized syringes
Wildlife immobilization poses unique challenges and risks, including:
Species variability: Unpredictable, influenced by its species, age, sex, and health status.
Capture myopathy: Muscle damage that can lead to death in captive wild animals.
Hyperthermia: Agitated animals and certain drug combinations.
Human safety: Potent drugs, dangerous animals
Capture Myopathy
Muscle damage (rhabdomyolysis) is central to the pathogenesis of capture myopathy
Myoglobin and creatine kinase (CK), are released from the injured muscle fibres into the blood stream
Blood lactate concentration is elevated leading to a decrease in pH and acidosis
Acute kidney injury (AKI) often occurs and is associated with myoglobinemia
Capture Myopathy continued
Eventually, multiple organ failure and death follow around 1-2 days after the initiating event
There is no treatment for capture myopathy. The most successful approach is adopting preventative practices
The use of tranquilizers during and after capture has aided in reducing the occurrence of capture myopathy but remains anecdotal at best
Most commonly reported in ungulates(hoofed mammals), such as deer, mountain goats, and pronghorn, and long-legged wading birds like cranes and geese