Chapter 17: Postpartum Physiological Adaptations
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
35 Terms
Chapter 17: Postpartum Physiological Adaptations
It is important to provide comfort measures for the client during the fourth stage of labor.
This recovery period starts with delivery of the placenta and includes at least the first 2 hr after birth.
Also during this stage, parent-newborn bonding should begin to occur.
The main goal during the immediate postpartum period is to prevent postpartum hemorrhage.
Other goals include assisting in a client’s recovery, identifying deviations in the expected recovery process, providing comfort measures and pharmacological pain relief, providing client education about newborn and self-care, and providing baby-friendly activities to promote infant/family bonding.
QEBP
Determine whether the fundus is firm or boggy. If the fundus is boggy (not firm), lightly massage the fundus in a circular motion.
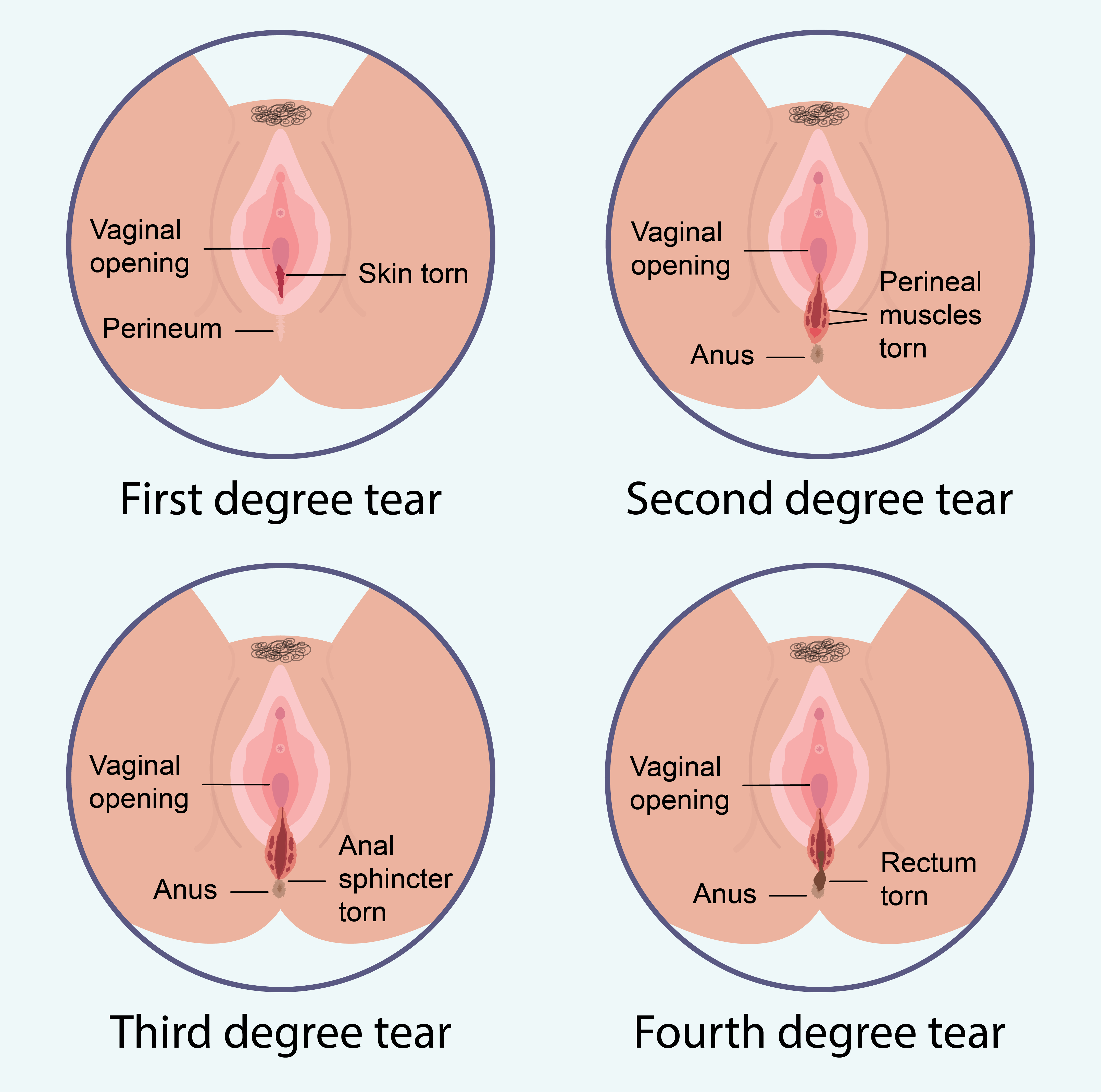
Enemas and suppositories are contraindicated for clients who have third- or fourth-degree perineal lacerations. Q
Postpartum Key Physiological Changes & Risks
Uterine & Cervical Involution
The uterus contracts and shrinks back to its pre-pregnancy size.
The cervix gradually returns to a closed position.
Lochia Flow (Vaginal Discharge)
A mix of blood, mucus, and uterine tissue expelled after birth.
Vaginal & Ovarian Function Changes
Decrease in vaginal distention.
Return of ovulation and menstruation depends on lactation status.
Cardiovascular, Urinary, Breast & GI Changes
Adaptations in fluid balance, blood volume, and hormone levels.
Hemorrhage (due to uterine atony or retained placenta).
Shock (caused by excessive bleeding).
Infection (such as endometritis, UTIs, or mastitis).
Postpartum period (Puerperium)
Involves both physiological and psychological adjustments.
Time: Between birth and the return of the reproductive system to its nonpregnant state
Traditionally lasts 6 weeks
Postpartum Hormonal Adjustments
After placental delivery, estrogen, progesterone, and placental enzyme insulinase drop, leading to:
Lower blood glucose levels (reversal of pregnancy-induced diabetes effects).
Breast engorgement and increased sweating (diaphoresis) & urination (diuresis) to eliminate excess fluid.
Reduced vaginal lubrication → may cause intercourse discomfort.
Higher muscle tone due to decreased progesterone.
hCG disappears quickly but can be detected for up to 4 weeks postpartum.
Oxytocin's Role Postpartum
Released from the pituitary gland to strengthen uterine contractions.
Breastfeeding stimulates oxytocin, which aids in uterine contraction.
Synthetic oxytocin may be given to enhance uterine tone.
Causes afterpains (painful uterine cramps), especially during breastfeeding.
Human chorionic gonadotropin (hcG)
Hormone produced by the placenta that forms around the embryo during pregnancy
Ovulation & Menstruation Resumption
Lactating Clients:
Elevated prolactin levels suppress ovulation.
Ovulation return depends on breastfeeding frequency, feeding length, & supplementation use.
First postpartum ovulation: ~6 months.
Nonlactating Clients:
Prolactin levels drop to pre-pregnant levels by ~3 weeks postpartum.
First postpartum ovulation: 7-9 weeks postpartum.
Menstruation Resumption: 12 weeks postpartum.
Postpartum Frequency of Assessments
First 2 hours
Blood pressure & pulse → Every 15 minutes (Q15×8)
Temperature → Every 4 hours
After 8 hours:
Temperature → Every 8 hours
Postpartum Assessment: BUBBLE-E
B: Breasts
Check for engorgement, redness, lumps, pain, or cracked nipples.
Assess latch and breastfeeding effectiveness (if applicable).
U: Uterus
Measure fundal height (should decrease daily).
Check uterine firmness → Should be firm, midline, and at or below umbilicus.
A boggy uterus may indicate postpartum hemorrhage.
B: Bowel & GI Function
Assess for constipation, hemorrhoids, and bowel sounds.
Encourage hydration and fiber intake to prevent straining.
B: Bladder
Monitor for urinary retention or burning sensation (UTI risk).
Encourage frequent voiding to prevent uterine displacement.
L: Lochia (Postpartum Bleeding)
Assess COCA:
Color: Rubra (red, 1-3 days), Serosa (pink, 4-10 days), Alba (white, 10-6 weeks).
Odor: Should be mild, foul odor = infection.
Consistency: Clots should be small; large clots may indicate hemorrhage.
Amount: Moderate to light flow; excessive soaking may signal PPH.
E: Episiotomy / Perineum
Check for redness, swelling, bruising (ecchymosis), and proper healing.
Encourage sitz baths and pain management if needed.
Vital Signs & Pain
Monitor temperature, heart rate, respiratory rate, and blood pressure.
Assess pain level and provide appropriate interventions.
Education & Teaching Needs
Educate on breastfeeding, self-care, and signs of complications.
Encourage hydration, ambulation, and emotional support.
H - Homan’s Sign (DVT assessment) (OUTDATED)
Assess for pain, redness, or swelling in the calves
Dorsiflex the foot → If calf pain occurs, it may indicate DVT (Deep Vein Thrombosis)
E - Emotional Status
Monitor for postpartum blues, anxiety, or signs of depression
Encourage open communication about mood, bonding with baby, and support system
Postpartum Laboratory Tests
Complete Blood Count (CBC)
Monitors:
Hemoglobin (Hgb) & Hematocrit (Hct) → Detects anemia due to blood loss.
White Blood Cell (WBC) Count → Elevated levels may indicate infection.
Platelet Count → Monitors clotting ability (important after birth).
Urinalysis
Checks for protein, glucose, and infection indicators (WBCs, nitrites, bacteria).
Detects postpartum complications like UTIs or kidney issues.
(Future Pregnancy Health)
Rubella Immunity Test (If status is unknown)
Why? If the mother is not immune, she may need a rubella vaccine postpartum to protect future pregnancies.
Rh Factor (Blood Type Compatibility)
If the mother is Rh-negative, testing ensures the newborn’s blood type is compatible.
If the newborn is Rh-positive, RhoGAM is given within 72 hours to prevent complications in future pregnancies.
Detects postpartum hemorrhage effects (low Hgb & Hct).
Prevents infections & complications (WBC count & urinalysis).
Ensures future pregnancy health (Rubella & Rh testing).
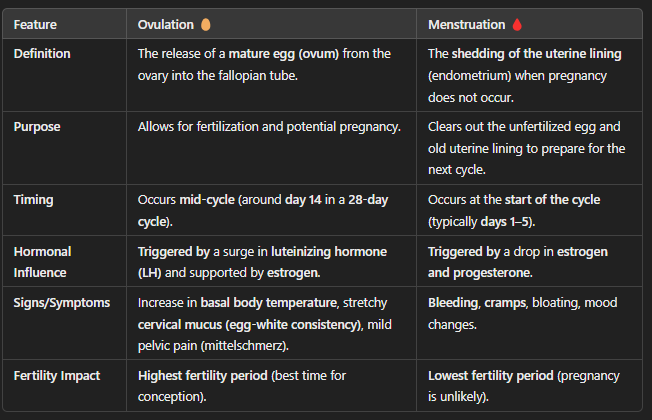
Ovulation vs Menstruation (Table)
The release of a mature egg (ovum) from the ovary into the fallopian tube.
Allows for fertilization and potential pregnancy.
Occurs mid-cycle (around day 14 in a 28-day cycle).
Increase in basal body temperature, stretchy cervical mucus (egg-white consistency), mild pelvic pain (mittelschmerz).
Highest fertility period (best time for conception).
The shedding of the uterine lining (endometrium) when pregnancy does not occur.
Clears out the unfertilized egg and old uterine lining to prepare for the next cycle.
Occurs at the start of the cycle (typically days 1–5).
Bleeding, cramps, bloating, mood changes.
Lowest fertility period (pregnancy is unlikely).
BUBBLE-E vs BUBBLE-HEE Acronym
(Adds two extra assessments!)
Everything in BUBBLE-E, plus:
H - Homan’s Sign (DVT assessment) (OUTDATED)
Assess for pain, redness, or swelling in the calves
Dorsiflex the foot → If calf pain occurs, it may indicate DVT (Deep Vein Thrombosis)
E - Emotional Status
Monitor for postpartum blues, anxiety, or signs of depression
Encourage open communication about mood, bonding with baby, and support system
Uterus (of BUBBLE-HEE): Fundal Assessment & Nursing Care
Assessment Guidelines
Frequency: Every 8 hours after the initial recovery period.
Steps:
Explain the procedure to the patient.
Position the patient supine with knees slightly flexed.
Use gloves and a lower perineal pad to observe lochia during assessment.
Palpation Technique
Use both hands: One above the symphysis pubis for support, the other to palpate the fundus.
NEVER palpate without support to prevent uterine inversion.
Fundal Documentation:
Above umbilicus: +1, U+1, 1/U
Below umbilicus: -1, U-1, 1/U
Uterus (of BUBBLE-HEE): Fundal Height Progression
Brief Ascent
Immediately after birth:
Firm, midline, and about 2 cm below the umbilicus.
1 hour post-birth: Rises to umbilical level.
12 hours post-birth: Can be palpated 1 cm above umbilicus.
Gradual Descent
Each 24 hours
Descends 1-2 cm per day.
By day 6: Fundus is halfway between symphysis pubis & umbilicus.
By 2 weeks: No longer palpable in the abdomen.
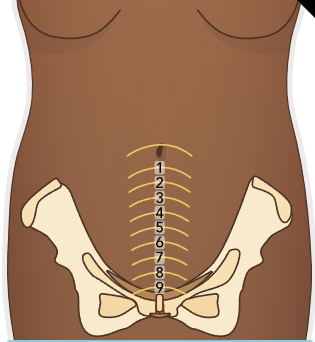
Uterine Involution (Image)
(Uterine Shrinking)
After birth, the uterus contracts to return to its pre-pregnancy size (involution).
Reduces from 1,000g (immediately postpartum) to 60-80g at 6 weeks postpartum.
Fundal height decreases by 1 cm per day until it is no longer palpable (~2 weeks postpartum).
Uterus (of BUBBLE-HEE): Postpartum Uterine Care
Medications to Promote Uterine Contractions
Oxytocin (Pitocin) - First-line drug
Methylergonovine (Methergine) - Avoid in hypertension
Carboprost (Hemabate) - Avoid in asthma
Misoprostol (Cytotec) - Prostaglandin used to prevent hemorrhage
Additional Nursing Interventions
Encourage early breastfeeding (stimulates natural oxytocin).
Encourage bladder emptying
Prevents uterine displacement.
Monitor for side effects:
Oxytocin & Misoprostol → Hypotension
Methergine & Carboprost → Hypertension
Lochia (BUBBLE-HEE): Assessing Lochia Amount
Amount of blood saturating a perineal pad:
Scant: Less than 2.5 cm / 1 inch (small spot of blood)
Light: 2.5 to 10 cm / 1-4 inch (small stain)
Moderate: More than 10 cm (covers a portion of the pad)
Heavy: One pad saturated within 2 hours
Excessive Blood Loss (Warning Sign!):
One pad saturated in ≤15 min
Pooling of blood under the buttocks
Lochia (BUBBLE-HEE): Assessing Lochia for Normal Appearance
Monitor lochia frequently to check for bleeding changes:
First hour: Every 15 minutes (x8)
Next 4 hours: Every 1 hour
Next 24 hours: Every 4 hours
After 24 hours: Every 4-8 hours, per facility protocol
Lochia flow pattern:
Typically trickles but may flow more steadily during uterine contractions.
Pooling under the client (especially when lying down) may indicate heavy bleeding.
Massaging the uterus or walking may cause a gush of lochia (normal)
Should return to a trickle.
Weighing pads helps estimate blood loss accurately.
Clients who had a C-section will have less lochia
The uterus is cleaned out during surgery.
Monitor for hemorrhage signs (excessive saturation or pooling).
Educate clients on expected vs. abnormal lochia patterns.
Encourage early movement to prevent clot formation
Lochia (BUBBLE-HEE): Abnormal Findings & Nursing Care
Report these findings immediately!
Bright red blood spurting from the vagina
Possible cervical or vaginal tear
Large clots & excessive bleeding (saturating a pad in ≤15 min)
Possible postpartum hemorrhage
Foul-smelling lochia
Infection (endometritis)
Persistent heavy lochia rubra beyond Day 3
Possible retained placental fragments
Lochia serosa or alba lasting too long (beyond expected duration)
Endometritis (inflamed inner lining especially if with fever, pain, or tenderness)
Nursing Interventions
Notify the provider immediately
Assess vital signs (watch for tachycardia & hypotension
Monitor fundal height & firmness
To rule out uterine atony
Encourage frequent bladder emptying
Prevent proper uterine contractions)
Administer prescribed medications (e.g., oxytocin, methylergonovine)
Prepare for possible surgical intervention (D&C for retained placenta)
Client Education
Change pads frequently
Perform hand hygiene after perineal care
Avoid tampons (higher risk of infection)
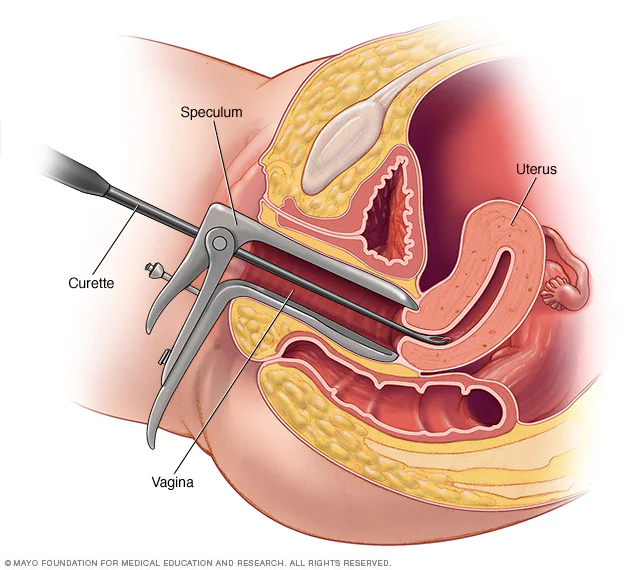
Dilation and curettage (D&C)
Surgical procedure that involves dilating (opening) the cervix and removing tissue from the inside of the uterus (endometrium)
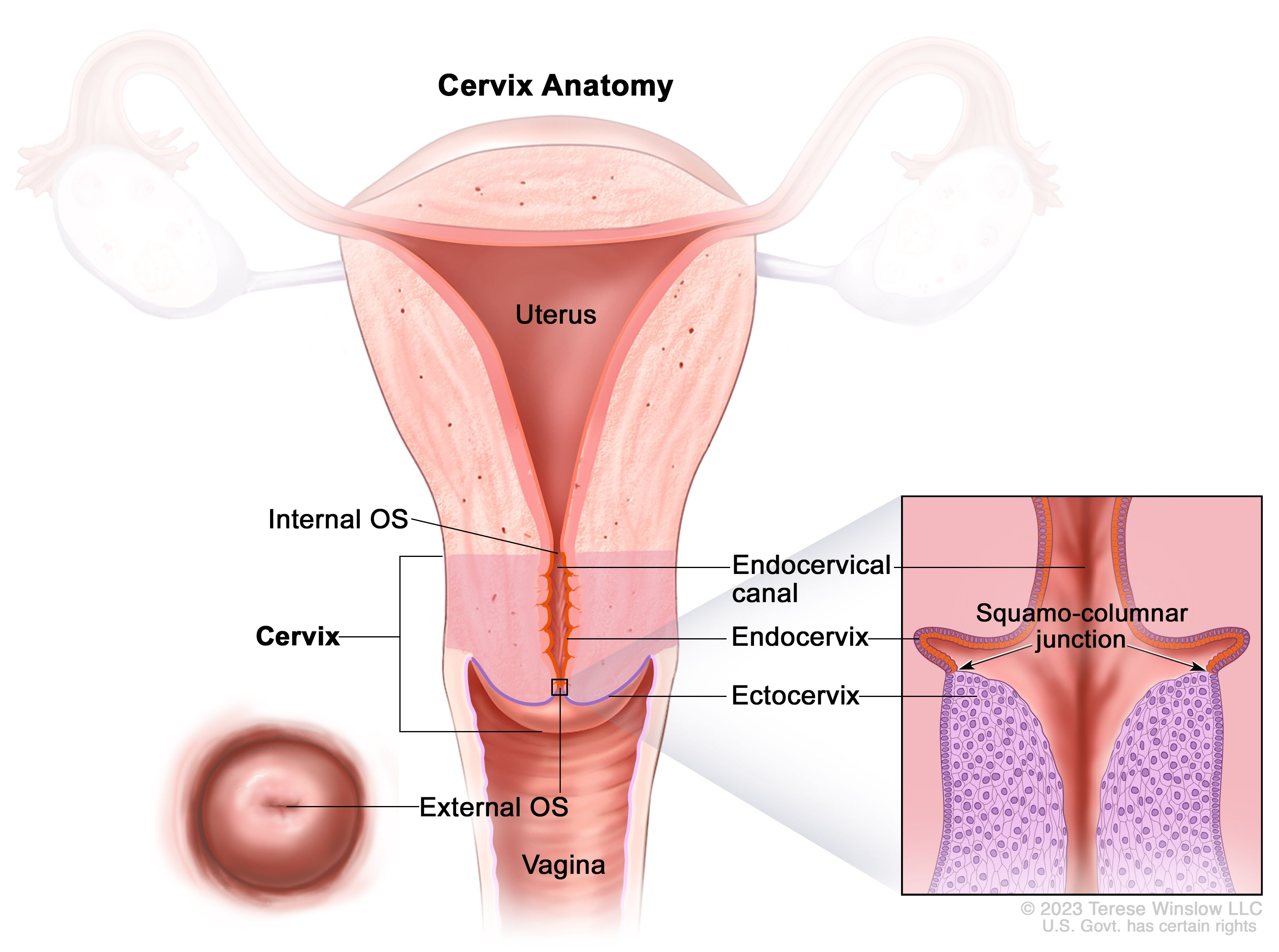
Postpartum Changes: Cervix, Vagina, and Perineum
Cervical
Immediately after birth: Soft, edematous (swollen), bruised, and may have small lacerations
By 2-3 days postpartum:
Shortens, regains its firm shape, and gradually closes
Lacerations can reduce cervical mucus production
The external os shape changes from round to a slit-like opening
Vaginal
Stretched during birth, then gradually returns to prepregnancy size
Reappearance of rugae
folds in the vaginal wall) and thicker vaginal mucosa
Permanent muscle tone loss
Does not fully return to pre-pregnancy state
Breastfeeding mothers may experience increased vaginal dryness & atrophy
Low estrogen levels
Perineal
Redness (erythema) & swelling (edema) common
Especially near episiotomy or laceration sites
Pelvic floor muscles may be weak and overstretched
Hemorrhoids & hematomas may develop
Pressure and pushing during labor
Cervix Anatomy (Image)
Postpartum Assessment & Care: Cervix, Vagina, and Perineum
Assessment
Monitor perineal healing for:
Redness (erythema), swelling (edema), and hematoma formation
Episiotomy/laceration site for approximation, drainage, bleeding, and healing
Bright red trickle of blood from episiotomy is normal in the early postpartum period
Healing Timeline:
Initial healing: 2 to 3 weeks
Complete healing: 4 to 6 months
Perineal Tenderness, Laceration, & Episiotomy Care
Ice/cold packs for first 24 hours
Reduce swelling and pain (do not apply directly to skin)
Heat therapy (hot packs, sitz baths, moist heat) for circulation & healing
Sitz baths (warm or cool) for 20 minutes, twice a day
Pain relief:
Nonopioid (Acetaminophen) & NSAIDs (Ibuprofen)
Opioids (Codeine, Hydrocodone) for severe pain
Topical anesthetics (Benzocaine spray) & witch hazel pads for pain & hemorrhoid relief
Infection Prevention:
Educate on proper perineal hygiene
Client Education
Wash hands before & after voiding
Use warm water or antiseptic squeeze bottle after each voiding
Blot dry from front to back (urethra to anus)
Avoid rubbing—instead, pat dry gently
Change perineal pad frequently, removing from front to back
Breasts (of BUBBLE-HEE)
Physical Change
Colostrum: Clear yellow fluid produced 2–3 days after birth
Milk Production: Begins 72 to 96 hours postpartum
Engorgement: Breasts become tight, tender, warm, and full due to increased blood flow and lymphatic circulation
Non-breastfeeding clients: Use breast binders, support bras, ice packs, or cabbage leaves to relieve discomfort
Breastfeeding clients: Frequent feedings and proper breast care help manage engorgement
Assessment
Redness (erythema), tenderness, cracked nipples, or mastitis (breast infection with flu-like symptoms)
Proper newborn latch to prevent nipple soreness
Ineffective feeding patterns (related to dehydration, discomfort, or poor positioning)
Patient-Centered Care
Encourage breastfeeding within 1–2 hours after birth
Early & frequent feeding stimulates oxytocin release, which helps with uterine contractions and prevents hemorrhage
Assist with comfortable breastfeeding positions:
Football hold (under the arm)
Cradle hold
Modified cradle hold
Side-lying position
Teach proper latching techniques (baby should take in part of the areola, not just the nipple) to prevent soreness
Clients who do not plan to breastfeed should avoid stimulation and expression of milk
Postpartum Cardiovascular and Vital Sign Changes
Blood loss during childbirth
Vaginal birth: 300–500 mL (~10% of blood volume)
Cesarean birth: 500–1,000 mL (~15–30% of blood volume)
Diaphoresis (sweating) and diuresis (urination): Eliminates excess fluid accumulated during pregnancy
Weight loss of ~19 lb (8.6 kg) occurs within the first 5 days postpartum
Hypovolemic shock is uncommon postpartum because:
The placenta is eliminated, reducing demand for blood flow
The uterus shrinks, redirecting blood back into maternal circulation
Blood Composition
Hematocrit (Hct) decreases for 3–4 days postpartum, then increases to normal by 8 weeks
Elevated white blood cell (WBC) count:
Common range: 20,000–25,000/mm³ (may reach 30,000/mm³)
This is called postpartum leukocytosis, a normal response to prevent infection and aid healing
Coagulation factors and fibrinogen levels remain elevated postpartum
Increases risk for blood clots (DVT, thrombophlebitis)
VS
Blood pressure (BP) remains stable, but a significant increase may indicate preeclampsia
Postural hypotension: Can occur when standing due to fluid shifts—advise sitting at the bedside before standing
Heart rate (HR) can drop to 40 bpm (postpartum bradycardia) within the first 2 days, returning to normal by 6–8 weeks
Elevated temperature up to 38°C (100.4°F) within 24 hours after labor is normal due to dehydration
Persistent fever after 24 hours may indicate infection
Assessment
Monitor cardiovascular and blood changes
Compare postpartum vitals to pregnancy baseline
Check pulses, skin turgor, and assess legs/feet for edema
Inspect lower legs for redness, warmth, swelling (signs of venous thrombosis)
Care
Encourage hydration to prevent dehydration and hypotension
Promote early ambulation to prevent blood stasis and clots
Apply compression stockings/SCDs to high-risk clients for DVT prevention
Administer medications (anticoagulants, pain relief) as needed
Laceration Tears (Image)
Enemas and suppositories are contraindicated for clients who have third- or fourth-degree perineal lacerations.
Bowels (of BUBBLE-HEE)
Physical Changes
Increased appetite immediately after birth
Constipation
Decreased peristalsis and muscle tone
Hemorrhoids (common)
From pushing during labor
Assessment
Hunger levels (clients will likely have a strong appetite)
Bowel sounds and function
Delayed bowel movement (2–3 days postpartum) is normal
Muscle tone changes, dehydration, or pain medications
Defecation discomfort
Perineal tenderness, episiotomy, lacerations, or hemorrhoids
Rectal area assessment for hemorrhoids or varicosities
Care
Encourage early ambulation, fluid intake, and high-fiber foods to improve bowel function
Administer stool softeners (docusate sodium)
Prevents constipation
Avoid enemas/suppositories in clients with third- or fourth-degree perineal lacerations
Manage gas pain (common after cesarean birth)
Encourage movement (rocking, walking) to relieve flatus
Avoid gas-producing foods
Anti-flatulent medications may be needed
Urinary (of BUBBLE-HEE)
Changes
Urinary retention may occur
Loss of bladder elasticity, decreased bladder sensation from trauma or anesthesia, and the effects of labor.
A distended bladder can lead to uterine displacement, increasing the risk of hemorrhage and infection.
Postpartum diuresis (increased urine output) typically begins within 12 hours after birth
Helps eliminate excess fluids retained during pregnancy.
Assessment
Check for pain or difficulty urinating due to perineal or urethral swelling.
Assess the elimination pattern
Eecessive urination over 3,000 mL/day is normal for the first 2-3 days
Look for signs of bladder distension, which may include:
Fundal height above the umbilicus or baseline level
Uterus displaced laterally
Visible or palpable bladder bulge
Excessive lochia (postpartum vaginal discharge)
Tenderness over the bladder area
Frequent voiding of less than 150 mL per urination
Can indicate urinary retention with overflow.
Care
Encourage urination within 6-8 hours after birth
If unable to void, catheterization may be necessary.
Promote frequent bladder emptying
Prevents uterine displacement and atony (lack of uterine tone).
Measure the first few voidings to ensure proper bladder emptying.
Encourage oral fluid intake to replace lost fluids and prevent dehydration.
Postpartum Musculoskeletal System
Changes
Joints stabilize and return to their normal state.
Feet may remain permanently increased in size.
Muscle tone begins to restore as progesterone levels drop after placenta delivery.
Abdominal muscles (rectus abdominis) and pelvic muscles (pubococcygeus) regain strength over time.
Assessment
Monitor musculoskeletal changes as the body recovers.
Assess for diastasis recti (separation of the abdominal muscles)
Usually resolves in 6 weeks.
Care
Fall prevention protocol
Client Education
Start with gentle postpartum exercises, gradually increasing intensity.
Delay abdominal exercises for 4 to 6 weeks after a cesarean birth (or follow provider recommendations).
Use proper body mechanics to avoid strain.
Ambulate early to improve circulation and muscle strength.
Perform Kegel exercises to strengthen pelvic muscles.
Postpartum Immune System Considerations
Rubella (MMR Vaccine)
Given postpartum to clients nonimmune to rubella or with a low titer.
Protects future pregnancies from congenital rubella syndrome.
Contraindication: Avoid pregnancy for 4 weeks (28 days) after vaccination.
Rh Factor (Rho(D) Immune Globulin)
For Rh-negative mothers who give birth to an Rh-positive newborn.
Administer IM within 72 hours postpartum to prevent maternal sensitization.
Nursing Considerations:
Check if the client has already been sensitized before administration.
Monitor for allergic reactions for at least 20 minutes post-administration.
Test immunity after 3 months to confirm effectiveness.
Varicella (Chickenpox Vaccine)
Given if the client has no immunity to varicella.
Avoid pregnancy for 1 month after vaccination.
A second dose is administered 4 to 8 weeks later.
Tetanus, Diphtheria, and Acellular Pertussis (Tdap) Vaccine
Recommended for clients who have never received it.
Also recommended for family members and caregivers who will be around the newborn.
Administer before discharge or as soon as possible postpartum.
Safe during breastfeeding.
Rubella (MMR Vaccine)
Given postpartum to clients nonimmune or with a low titer.
Protects future pregnancies from congenital syndrome.
Contraindication
Avoid pregnancy for 4 weeks (28 days) after vaccination.
Rh Factor (Rho(D) Immune Globulin)
For Rh-negative mothers who give birth to an Rh-positive newborn.
Administer IM within 72 hours postpartum to prevent maternal sensitization.
Nursing Considerations:
Check if the client has already been sensitized before administration.
Monitor for allergic reactions for at least 20 minutes post-administration.
Test immunity after 3 months to confirm effectiveness.
Varicella (Chickenpox Vaccine)
Given if the client has no immunity
A second dose is administered 4 to 8 weeks later.
Contraindication
Avoid pregnancy for 1 month after vaccination.
Tetanus, Diphtheria, and Acellular Pertussis (Tdap) Vaccine
Recommended for clients who have never received it.
Also recommended for family members and caregivers who will be around the newborn.
Administer before discharge or as soon as possible postpartum.
Safe during breastfeeding.
Postpartum Comfort & Psychosocial Well-being
Assessment & Interventions
Assess pain related to:
Episiotomy, lacerations, incisions
Afterpains (uterine contractions postpartum)
Sore nipples from breastfeeding
Assess pain location, type, and intensity to tailor interventions.
Administer prescribed pain medications.
Teach nonpharmacological pain relief:
Distraction techniques (e.g., music, imagery)
Heating pads, cold packs
Position changes
Psychosocial Adjustments
Clients may experience a wide range of emotions due to hormonal changes, adjusting to newborn care, and fatigue.
Assessment & Interventions
Encourage verbalization of feelings.
Assess emotional status.
Observe parent-newborn bonding.
Monitor for postpartum blues or depression, which may include:
Decreased appetite
Difficulty sleeping
Decreased social interactions
Lack of communication
Patient-Centered Care
Encourage skin-to-skin contact with the baby.
Document bonding interactions.
Encourage rooming-in (keeping the baby in the client’s room at all times).
Provide emotional support and refer for counseling if needed.