Athletic injuries 3336 Midterm
1/138
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
139 Terms
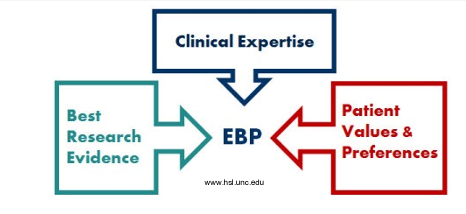
what is evidence based practice
The conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients.
Incorporation of a clinician’s expertise and the best current research evidence with the patients values
EBP = individual clinical expertise + best external evidence + patient values and expectations
why is evidence based practice important
level of evidence varies greatly for the efficacy of much of what we do, much of it is based on perceived clinical success
how do we accomplish this?
1. read all the scientific journals
2. more focused techniques (CAPs and CATs and infographics) critically appraised paper/topic
what are the steps in EBP (evidence based process) 1-6
ASSESS the patient: Start with the patient --a clinical problem or question arises from the care of the patient
ASK the question: Construct a well built clinical question derived from the case
ACQUIRE the evidence: Select the appropriate resource(s) and conduct a search
APPRAISE the evidence: Appraise that evidence for its validity (closeness to the truth) and applicability (usefulness in clinical practice)
APPLY: talk with the patient: Return to the patient --integrate that evidence with clinical expertise, patient preferences and apply it to practice
Self-evaluation: Evaluate your performance with this patient
grade practice recommendations
A - strong recommendation
B - recommendation
C - option
D - option
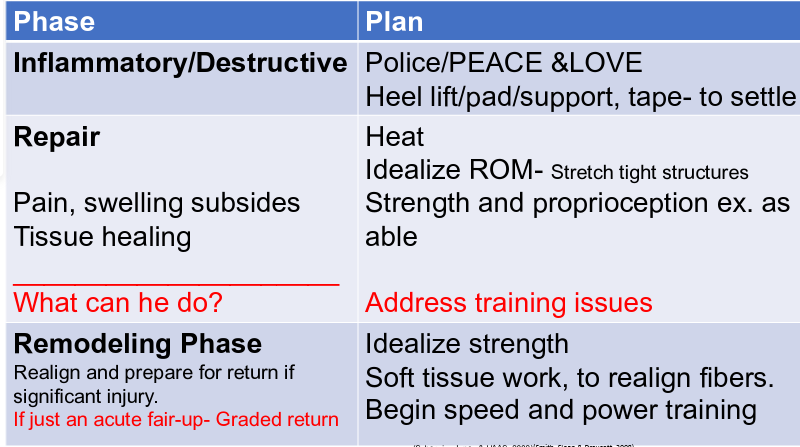
phases of healing
Body goes through a predictable sequence of healing
Our treatment choice will be dependent on the phase of healing
We have minimal ability to speed up this process, but interfering with this sequence will slow both recovery and return to sport !
what are the 3 phases of healing
inflammatory/destruction phase
repair phase
remodelling phase
inflammatory/destruction phase
generally 1st 1-4 days
cellular injury = altered metabolism + release of chemical mediators/proteins
these cause the inflammation response?
invasion by extrinsic cells
phagocytosis (engulf bacteria, cellular debris)
primary damage
damage at time of injury
immediately irreversible
secondary damage
Damage by released proteins
Damage as a result of body processes swelling pinches off blood flow, without O2, cells die off
Edema
Damage due to decreased blood flow
Decreased oxygen
we want to drop metabolic rate of tissues: decreasing what they require can save them from dying
signs and symptoms of inflammation
red
swollen
painful
hot
loss of function
repair (fibroblastic) phase
72 hours to 6 weeks
proliferative and regenerative healing leading to formation of connective tissue scar (type 3 collagen)
fibroplasia begins within first few days and inflammatory signs should be decreased
growth of endothelial capillary buds into the wound is stimulated by lack of O2 (new growths allow increased O2 and BF)
body lays down type 3 collagen (weak, delicate scar)
remodeling/maturation phase
usually firm strong non-vascular scar by end of 3 weeks
long term process - 3 weeks to years
with increased stress and strain, the collagen changes to type 1 and begins realignment
wolfs law
remodeling phase
wolfs law - bone and soft tissue will respond to the physical demands placed on them, causing them to align along lines of tensile force progressively
Critical that injured structures be exposed to progressively increasing loads
Can work up to aggressive strengthening to facilitate remodeling and alignment
Watch out for pain and swelling after exercise (dont want to do too much_
SOAP notes
subjective
objective
analysis/assessment
plan/program
subjective
most important
includes statements provided by patient regarding their symptoms
from this history you develop assessment plan
subjective assessment: why
most clinicians rate medical history as having greater diagnostic value than physical exam or results of lab
interviewing one of hardest skills to master
subjective assessment: how
used to develop a strat for further examination
ask open ended questions
active listening (eye contact, non verbal cues)
history- basic info needed
primary complain
history of injury
MOI
symptoms/pain profile
symptom
organic manifestation which only patient is aware of, cant see symptoms
immediate or delayed issues
MSK injuries
medical conditions
red flags
what to ask for history
What happened? When did it happen, Specific MOI
Were you able to continue
How did/does it feel
Swelling –Yes, no, fast or slow? Fast (<4hrs) hemarthrosis, Slow (4-8 hrs) capsular swelling
Describe your pain/other, Dull, Sharp, Shooting, bright, Numbness, tingling
objective
signs - observable physical phenomenon indicative of a conditions presence
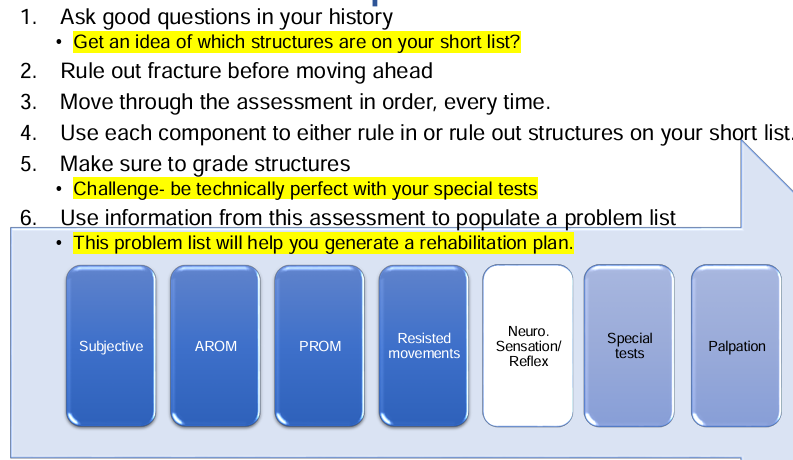
order of assessment
subjective
observation/visual inspection
AROM
PROM
resisted
neuro
special tests
palpation
observation/visual inspection
We need to assess their general demeanor: Expression (pain, tired, angry) Tone of voice
Posture: protective postures, guarding, stiff, etc. deformity asymmetry
Obvious deformity/asymmetry
Signs of inflammation: Swelling, redness, bruising
quality of movement: How are they moving: Speed, Quality (smooth, jerky), Amount of movement
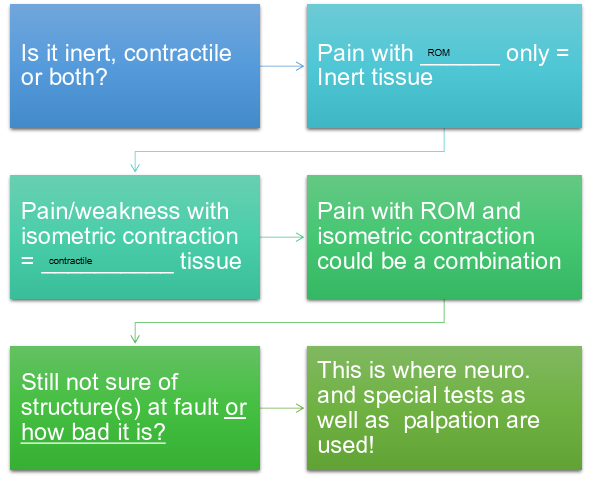
theory of selective tissue tension
dr. James Cyriax developed
method for locating and identifying a lesion by applying tensions selectively to each of the structures that might produce pain
inert and contractile
when tension is applied to an injures tissue, it will give rise to pain
inert
ligaments
bursa
capsules
fascia
nerve roots
dura mater
contractile tissues
muscles
tendons
tenoperiosteal insertion
selective tissue tension: contractile tissue
Increases in tension when the contracted tissue is both contracted or stretched
Active motion in one direction and passive motion in the opposite
selective tissue tension: inert
Increase in tension when they are stretched
Will elicit pain on active and passive movement in one direction, only
AROM
Movement assessment should begin with Active Range of motion (AROM)
Active movements which cause pain do not specifically indicate either an inert or contractile lesion
Muscle tension and joint movement causes contractile and inert tension to both occur!
agonist contract
antagonist stretch
Inert tension in only one direction
what info does AROM give
where they are sore
willingness to move
amount of movement
available ROM
give us clues on how we handle them
PROM: how
patient must relax completely allowing therapist to move extremity
look for limitation of ROM and presence of pain
specific attention should be paid to how they feel at the end of ROM
pain prior to end usually signifies inflammation or red flag
what info does PROM tell us
Passive movements are used to detect lesions in inert tissues
This stretching of the inert tissue will cause pain
What is happening in surrounding contractile tissue during PROM?
What does PROM alone tell us? Allows us to assess end feel
normal end feel
soft tissue approximation - elbow knee flexion: soft spongy gradual painless stop when 2 muscle bellies meet
bony: elbow extension - distinct abrupt endpoint/unyielding, painless
capsular: hip rotation - abrupt firm endpoint with a little give, leathery feeling
abnormal end feel
springy block - internal issue of joint - rebound at end or some point throughout ROM, bouncy
spasm/stretch - hamstrings - involuntary contraction that prevents motion secondary to pain (guarding), more rubbery feel prior to expected end of range
abnormal capsular - occurs prior to expected end of range
empty - did not reach end feel - considerable pain is produced by movement, no mechanical resistance detected, significant soft tissue injury, bursitis, or neoplasm
what do we need for resisted testing
Contraction of only target tissue stretch
No stretch on antagonist (isometric movement, nothing on stretch)
No movement through joint or stretch on surrounding inert tissues
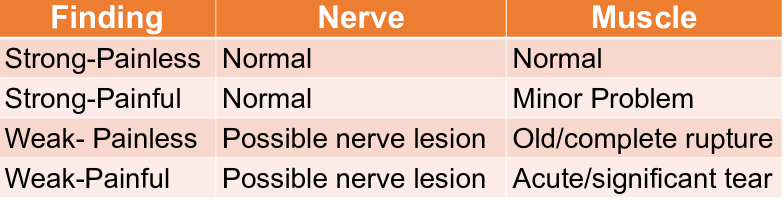
info gained from resisted testing
Will tell us about pain in a contractile tissue
Will also give us an indication of how the nerve is working/how well it contracts
interpreting resisted movements
decision time (flow chart)
neurological testing
reflexes
sensation
key muscles
reflexes
biceps/brachioradialis: C5-C6
triceps: C7-C8
knee jerk: L3
achilles: S1
sensation/dermatomes
Cutaneous area receiving the greater part of its innervation from a single spinal nerve
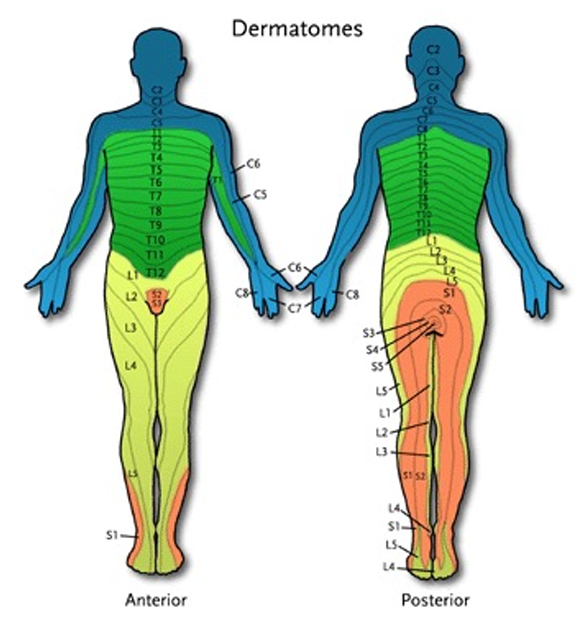
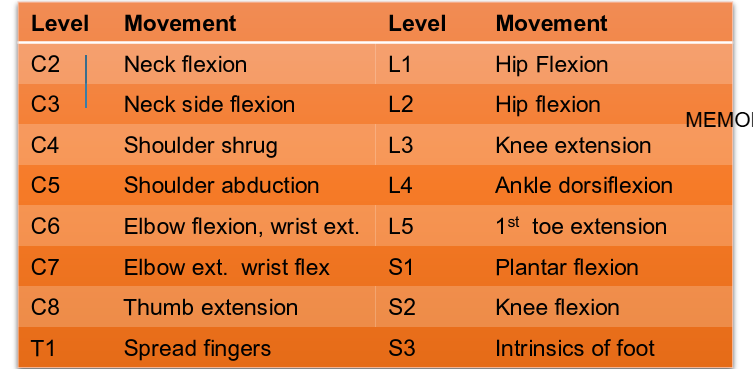
myotomes
A muscle receiving the greater part of its innervation from a single spinal nerve
Isometric contraction held for at least 5 seconds
fatigable weakness vs. no strength for peripheral nerve
special tests
special tests hlp in the differential diagnosis of patients injury
includes manual muscle testing, specific muscle (strength through ROM) and ligament test (laxity, end point, pain)
these are an indication of how bad it is
they allow us to grade the injury
diff than isometric resistance because they move through ROM
manual muscle testing (oxford scale)
0 - Nothing happens
1 - Twitch or flicker only. No movement
2 - Able to move but not against gravity
3 - Able to move the joint fully against gravity
4 - Movement with some resistance
5 - Full movement with resistance equal to opposite side
analysis/assessment
Hopefully at this point we have an idea if it is contractile, inert or both.
After neuro, special tests and palpation, we should have a good idea of the degree of injury and contribution by each structure.
Based on these findings we form a clinical opinion or diagnosis- this is your analysis/assessment
make a problem list, (pain, decreased ROM), then make goals (decrease pain increase ROM)
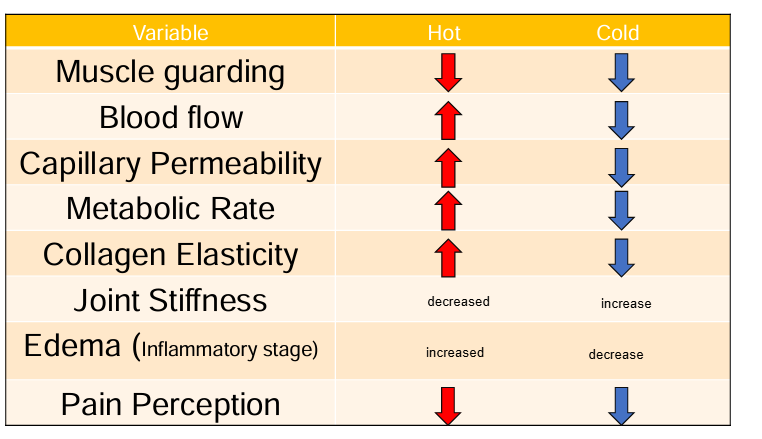
the bodys response to hot and cold depends on":
media being applied
conductivity of area
length of exposure time
hot and cold depends on media being applied
ice, cold water immersion, sprays
moist heat (better for deep tissues, dry heat (better tolerated), ultra sound (mechanical)
hot and cold depends on conductivity of the area
High water content in tissue means > change
Joints>muscle
Decreased conductivity through fat
hot and cold depends on length of exposure time
With ice, longer not always better prevents reflex vasodilation
Bleakley et al (2006) Cold 10 on -10 off-10 on is superior to 20 min on. Less pain in first week no change after that
With heat, the body will reach a peak heat in in 5-7 minutes and
physiological responses to hot and cold (chart)
the case for using ice
good for pain:
C not myelinated!
For every 10 drop in temp. you cool a nerve, you decrease conduction velocity.
With a 4 degree cooling you knock out C fibers
when combined with exercise
Demonstrated better ability to decrease swelling vs. heat
Significant improvement in function vs. functional training
ice shown to maintain cell viability after injury
⇩chemical reactions +⇩ ATP demand= ⇩cellular collapse (anti-oxidant)
the case against using ice
The inflammatory or destruction phase of healing is a necessary stage
We need the athlete to go through the stage, but not get stuck there.
There is evidence that one early ice treatment may slow down healing over the first 3-7 days
More necrosis in ice group at day 3 but equal at day 7
Less neutrophils day 1 and more day 3 in ice group
Less macrophages at day 1 and 3 with more at day 7 in ice group
what are the goals for inflammation/destruction phase
what is happening at the tissue level
red, hot, swollen, painful
tissue inflammation/destruction: primary and secondary
based on that, what are our immediate goals
optimize healing environment
palliate pain
decrease swelling
PEACE and LOVE and POLICE
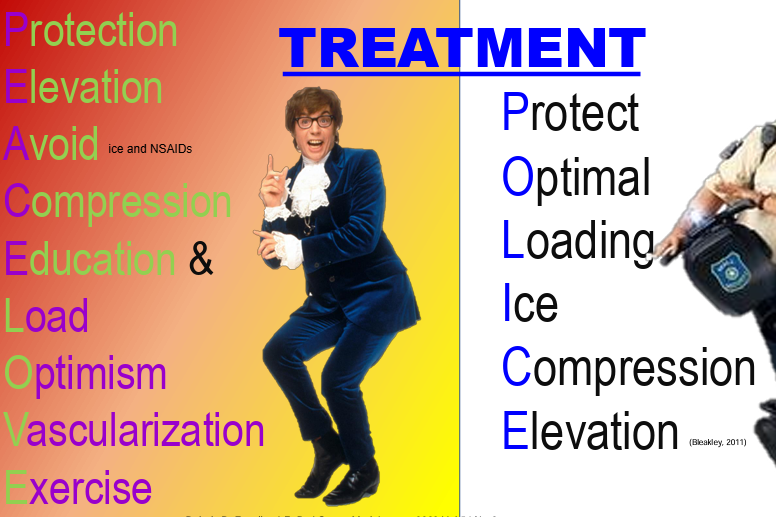
protection (PEACE and LOVE and POLICE)
Protection and rest after injury are supported by interventions that shield, unload and/or prevent joint movement for various periods.
Recent animal models show that short periods of unloading are required after acute soft tissue injury and that aggressive ambulation or exercise should be avoided.
Remember our goal: control inflammation and prevent further injury
loading (PEACE and LOVE POLICE)
Optimal loading means replacing rest with a balanced incremental rehabilitation program where early activity encourages early recovery
This includes safe cardio, which will increase blood flow. - Vascularization
Injuries vary, so there is no single one sized fits all strategy or dosage.
Functional rehabilitation of ankle sprain, which involves early weight-bearing usually with an external support, is superior to cast immobilization for most types of sprain severity.
compression (PEACE and LOVE, POLICE)
Compression has been shown to decrease local edema
Applying a pad or ice bag underneath will increase pressure over the injured area
Helps disperse edema and makes it more available for absorption, by limiting the physical space is able to occupy it.
An elastic bandage pulled tight can limit blood flow by up to 95% within a few seconds
elevation (POLICE and PEACE and LOVE)
No reduction of blood flow until the injured area is at least 30 cm above the heart
At 50 cm flow is 80% of normal
At 70 cm flow is 65% of normal
Think about what people usually do with their sprained ankle
optimism and education (PEACE and LOVE)
Let them know:
Why they are doing things
How you will measure their progress goals
Set goals with your patient and share their results
By setting and achieving small goals you will condition their brain to be positive and confident
This ”buy-in” will continue to pay dividends as they will work harder and stay motivated
Teach them that rehabilitation is an active process
icing - clinical hack
Best cooling effect comes from ice mixed with water in plastic bag directly on skin
Fill bag with ice chips or ice and cold water.
Take air out of the bag, so the ice molds to the skin
Mold ice bag to skin
Compression over top is best
Use of towel, wet or dry compression bandage decreases conductivity
Explain to the athlete what they will feel
CBAN
Timing- 10 on, 10 off, 10 on
repair/fibroblastic phase goals
What is happening at the tissue level? Based on that, what are our immediate goals?
Protect the tissue and idealize healing environment
increase blood flow**
Before the end of this stage:
Idealize ROM** (they feel better at this stage)
Begin gentle strengthening **= helped by application of heat
heating - clinical hack
Most clinics will use moist heat from hot packs kept in hydrocollators full of hot water 160° to 165°F (71°–74°C)
1. Remove hot pack with tongs and place in terrycloth slip-cover.
2. Add one folded towel and apply to patient (Terrycloth slip-cover is equal to 4-6 layers of towel. If not available add 6-8 layers of towel under the hot pack)
3. Place on patient and let them know that it will take a few minutes to feel the heat.
4. Direct them: • Not to remove towels at this time • That they need to let you know if it feels too hot
5. Check back in 5 minutes and add or remove layers as needed
Total time 10-20 minutes depending on depth
ankle injuries
fractures
sprains
strains
ankle sprains
most common injury in sports
85% lateral
5% syndesmosis
10% medial
ankle stability comes from (1-3)
shape of bones
passive stabilizers (capsules and ligaments)
dynamic stabilizers (muscles that cross the joint)
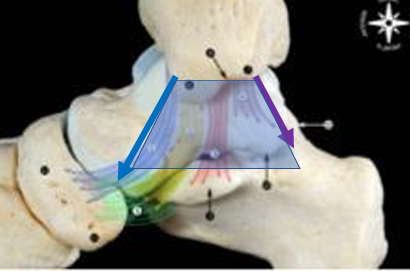
the bones of the ankle (talocrural joint)
The ankle mortice is a U-shaped structure making up the top of the talocrural joint
Made up of:
Lower end of tibia
Medial malleolus (Tibia)
Lateral malleolus (Fibula)
Lateral malleolus longer and more posterior than medial
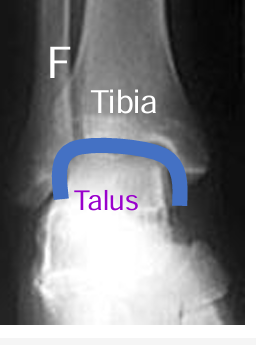
the bones of the ankle ( the talus)
Has no muscles that attach to it
Very extensive articular surface
Convex on top and concave on the sides
Allows it to better articulate with the Tibia and Fibula anteriorly
Trochlear surface (top) is wider anteriorly than posteriorly
With dorsiflexion the wider portion lies between the malleoli (Tibia and Fibula) might have more fratcures or high ankle sprains in dorsiflexion
What could that mean for stability? more stable in dorsiflexion
bones of the ankle (fibula)
with dorsiflexion
Fibula externally rotates and it moves superiorly
External rotation of fibula increases the tension in the structures that hold the tibia and fibula together
Opposite happens in plantar flexion
passive stabilizers - capsule and ligaments
Ankle is surrounded by fibrous capsule
thin and weak anteriorly and posteriorly to allow movement (dorsiflexion and plantarflexion)
Talocrural joint is further strengthened medially and laterally by ligaments
Some communicate (ATFL, PTFL , deep Deltoid) with the capsule, while others do not. more swelling with capsula
passive stabilizers - lateral ankle
ATFL
Communicates with/is within capsule (Increase swelling)
Considered the weakest of the lateral ligaments plantarflexion
Increased strain in plantarflexion and inversion
CFL
Extracapsular capsular ligament
Provides stability to the lateral talocrural joint as it moves into neutral/dorsiflexion
Up to 3.5 x stronger than the ATFL
PTFL
Primarily supports talocrural joint in
May provide secondary support to the talocrural joint throughout range
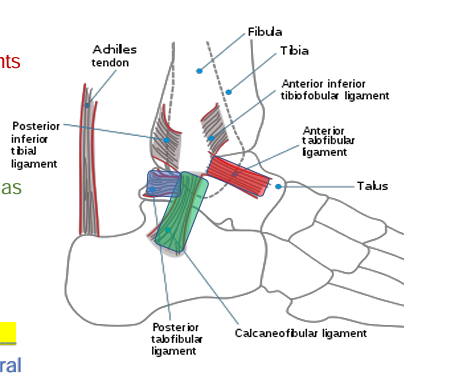
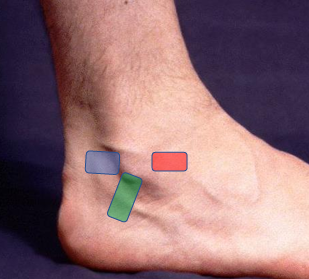
surface anatomy hacks: how to find ATFL, CFL, PTFL
ATFL
slide anteriorly and medially off of the distal tip of the lateral malleolus
CFL
slide inferiorly and slightly posteriorly off of the lateral malleolus
PTFL
slide posteriorly off of the posterior aspect of the distal tip
passive stabilizers of ankle: deltoid ligament
Deltoid ligament- limits talar/subtalar abduction or eversion
Very broad from front to back
Deep portion communicates with capsule
Described as up to 6 bands with considerable variability anatomically
Anterior part is tight in plantar flexion
Middle portion in neutral
Posterior portion tight in Dorsiflexion
Surface Anatomy Hack- Slide off of the medial malleolus with your thumb and finger. Notice how the separate. This is the broad Deltoid ligament
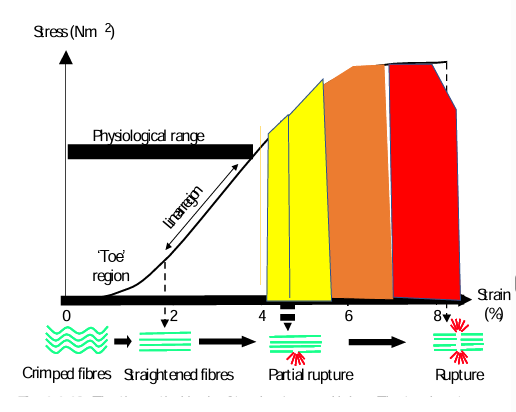
ligament sprains (percentages of range)
0-4 % strain is physiological range
Pathological irreversible ligament elongation occurs after 4% strain
As this continues intra and inter- molecular cross-links are disrupted until macroscopic failure is clinically evident
Early part = mild/ grade 1 < 50 %
2nd part= grade 2 50-80% fiber disruption
Obvious clinical laxity 3rd part=Grade 3. Rupture zone 80-100%
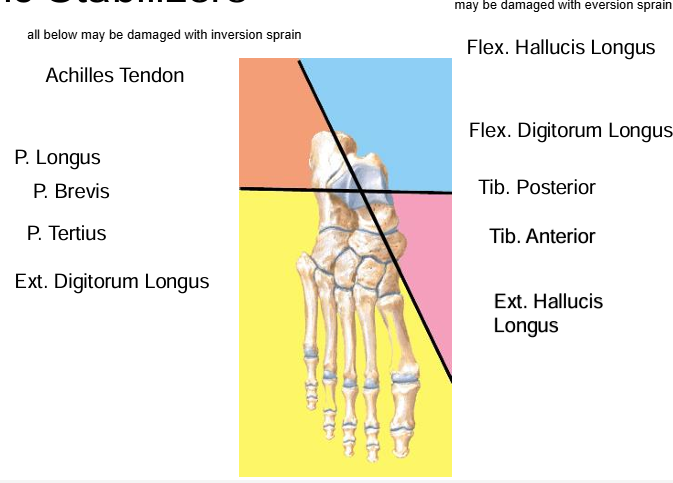
dynamic stabilizers of ankle
assessment tips
what does an ankle sprain look and sound like
MOI: inversion or eversion, plantarflexed or dorsiflexed
were you able to continue (make sure it isnt fractured)
did you hear or feel a pop or crack (fracture/significant ligament injury)
observation: ankle sprain (what are we looking for)
swelling
obvious deformity (lower leg, ankle, foot)
weight bearing (static - equal pressure on front and back or side to side, dynamic - guarded/painful movement)
Ottawa ankle rules
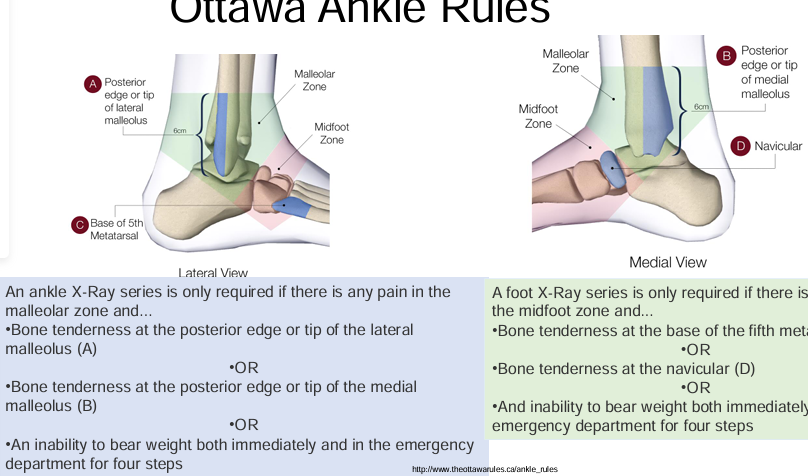
what test is sued to rule out an ankle fracture
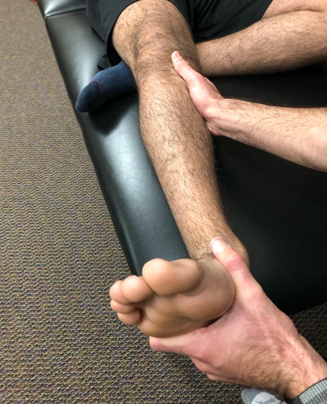
external rotation test for fibular fracture
pry open mortis putting pressure on lateral side of ankle
send for leg xray if pain
this is an INDIRECT test for fracture
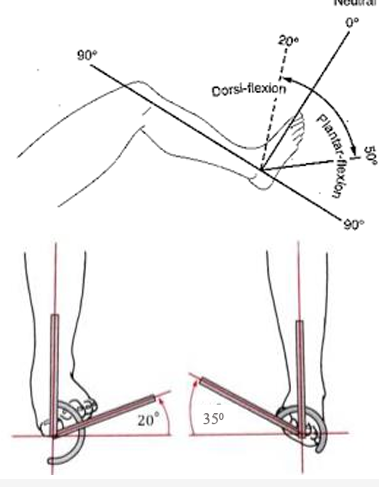
what is considered normal ankle range for movements
Plantar flexion- 50 degrees
Dorsiflexion- 20 degrees
Inversion- 30-35 degrees
Eversion- 15-20 degrees
what are the special tests for ankle ligaments
anterior drawer
talar tilt
external rotation (already done and was positive
ottawa ankle rules (already done and was positive)
anterior drawer test for ankle
Used to determine damage to Anterior Talofibular Ligament, primarily
Tested in slight plantarflexion
A positive test occurs when foot slides forward and/or makes a clunking sound as it reaches the end point
Grade ligaments by assessing pain, laxity and endpoint
talar tilt test
Performed to determine extent of injury to the calcaneofibular ligament (inversion) or Deltoid ligament (eversion )
With foot at 90 degrees, the calcaneus is inverted . Pain and excessive motion indicates injury to Calcaneofibular ligament and possibly the anterior and posterior talofibular ligaments
If the calcaneus is everted deltoid , the deltoid ligament is tested

special tests for contractile tissue does what
allows us to grade injury
manual muscle testing (oxford scale)
resisted tells us if a contracted tissue is injured
manual muscle testing tells us how bad it is
symptoms and signs of ATFL sprain
most common sprain
symptoms
inversion in plantar flexion MOI
Pain on the lateral side of the ankle, anterior to malleolus
May report instability with high grade sprain
signs
Significant swelling
Pain with active and passive inversion in plantar flexion
Pain, laxity, endpoint? Findings with Anterior Draw Test
Possible pain with resisted eversion (dynamic stabilizers)
Pain on palpation over the Anterior Talofibular ligament
symptoms and signs of CFL sprain
3.5x stronger than ATFL
symptoms
Inversion mechanism of injury in neutral to slight dorsiflexion
Pain on the lateral side of the ankle inferior to the malleolus
May report instability with high grade sprain
signs
May not have significant swelling if injured in isolation
Pain with active and passive inversion in neutral to slight dorsiflexion
Pain, laxity, endpoint? Findings with talar tilt (inversion)
Possible pain with resisted eversion (dynamic stabilizers)
Pain on palpation over the CFL ligament
symptoms and signs of deltoid ligament sprain
least common sprain
Stability of the medial ankle depends upon the Deltoid Ligament and supported by lateral malleolus.
symptoms
eversion MOI
Pain on the medial side of the ankle
May report instability with high grade sprain
signs
Pain with active and passive eversion
Pain, laxity, endpoint? Findings with Talar tilt (eversion)
Possible pain with resisted inversion (dynamic stabilizers)
May have increased pronation - Navicular dropped?
Pain on palpation over the deltoid ligament
ankle sprain prognostic indicators
Higher age, poor weightbearing status and higher grade of injury at baseline are associated with poorer outcomes.
Not achieving full ROM within 2 weeks may be a sign of accompanying injury.
Medial pain on palpation (bone bruise) and pain with dorsiflexion at week 4 were prognostic of poorer function at 4 months
ankle sprain treatment in acute phase
NSAIDs to reduce pain and enhance self-reported function in conjunction with ice, compression, and elevation early in the rehabilitation process.
Early return to motion over immobilization
protect injured tissue
maintain ROM to uninjured tissue
Ice, compression, elevation
protected gait (crutches)
ankle sprain treatment in subacute repair phase
Strong evidence for using exercise to prevent future sprains • Including balance and coordination training as soon as weight bearing can be tolerated.
Proprioceptive and neuromuscular interventions after ankle injuries can be effective for the prevention of recurrent injuries.
Limited evidence for use of manual therapy
Strong evidence for use of external support for return to activity
heat
Begin ROM ex. and idealize by 2 weeks
Maintain strength of uninjured tissue.
Begin gentle strengthening of injured tissue, once ROM is achieved
increase weight bearing
Begin proprioception exercise
ankle sprain treatment in late repair/remodeling
idealize strength of dynamic stabilizers through full range
Continue with balance and coordination training
Repetition in practice helps develop effective movement solutions
Aids in avoidance of reinjury as the cognitive load decreases and we “tune” perception and action
This will allow for improved agility and power
Jumping, cutting, push-off, etc
Decide on return to play taping or bracing x 1 year
retrocalcaneal bursitis
Bursa in the recess between the anterior inferior side of the Achilles tendon and the posterosuperior aspect of the calcaneus (retrocalcaneal recess)
Sometimes seen with insertional tendinopathy
Structural irritants (tight/pokey)
Pain just above the insertion of the Achilles Tendon
Pain with squeeze from side
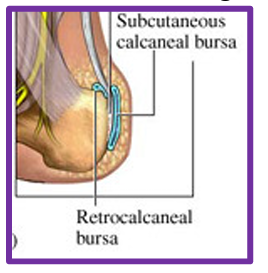
Achilles bursitis (superficial calcaneal bursitis)
Bursa located between calcaneal prominence or the Achilles tendon and the skin posterior
Pain posterior aspect of heel with solid swelling
Often due to excessive friction or by wearing shoes that are too tight or too large
management of bursitis
POLICE/PEACE & LOVE
Address training and equipment issues
Heel lift? takes tension off achilles
Pad? donut shape that takes tension off achilles
Achilles Stretch
New Shoes/popped out
lower leg tendinitis
Tendons are mechanically responsible for transmitting muscle forces to bone and in doing so permit locomotion and enhance joint stability
Tendons are structured to withstand stretch
Tendon has no synovial sheath but some are surrounded by paratenon
Only vascular tendons are surrounded by paratenon
Tendinitis- is inflammation of the tendon itself and is relatively rare
paratenonitis
inflammation, pain, and crepitation of the paratenon as it slides over the structure
normally happens at the same time as tendinitis, one causes the other
causes of tendinitis/paratenonitis (external and internal factors)
acute irritation: too much too soon
External factors such as:
Rub from shoe/equipment
Running down hill- Tibialis anterior
Rub from laces- Tibialis anterior
Hyper dorsiflexion- Achilles
Internal factors such as:
Foot malalignment
Rub over bone
Cavus or flat/pronating feet
symptoms and signs of paratenonitis/tendinitis
symptoms and signs:
Pain and/or crepitation (of Paratenon- creaking feeling of tendon rubbing through paratenon) of acute onset
Red and hot over involved structure
Usually precipitated by movement around the ankle joint - Remember too much too soon
diagnosis:
Made on the basis of local swelling
STTT- what will that look like?
Palpation over structures
ITIS rehab (same for almost EVERYTHING)
scenario for achilles tendinosis
Bob is an active 45 year-old office worker with pain on the back of his foot and up his leg.
Has been training for a marathon and has ramped up his already excessive running schedule
He reports steadily worsening pain over the past 6 months and is now finding it difficult to run at all.
What could it be?