Lecture 11 - Cardiovascular System - Cardiac Physiology
0.0(0)
Card Sorting
1/132
Earn XP
Description and Tags
Last updated 11:00 PM on 1/27/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
133 Terms
1
New cards
What is cardiac muscle?
Heart muscle.
2
New cards
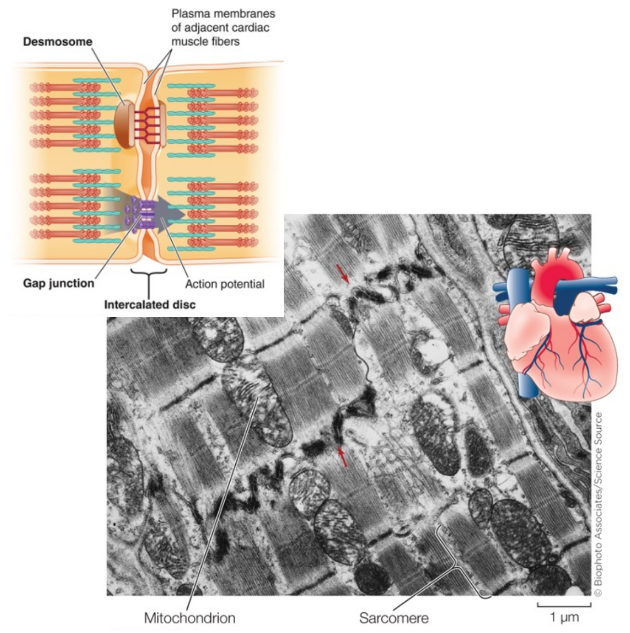
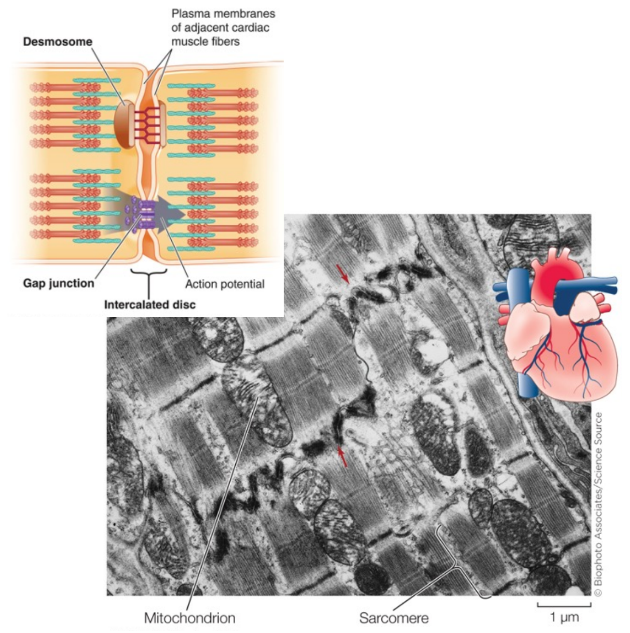
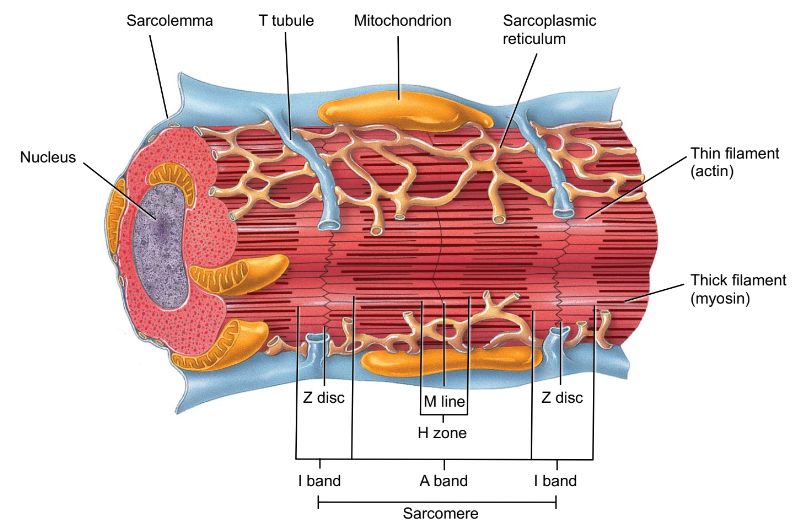
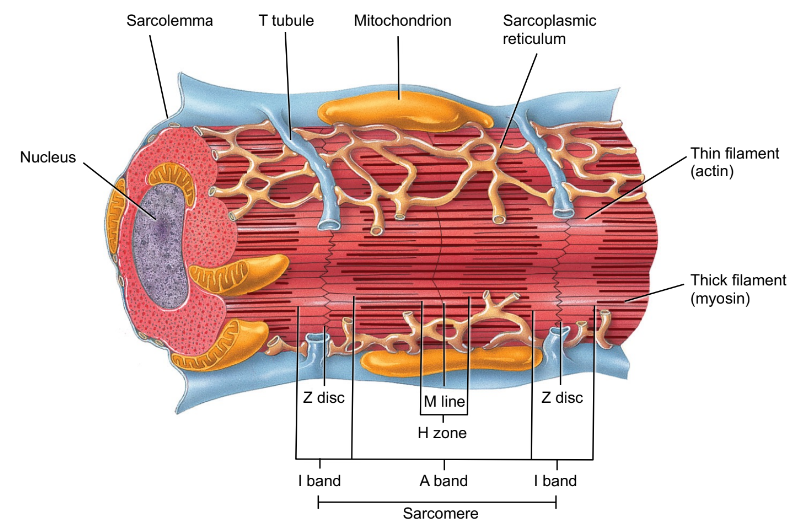
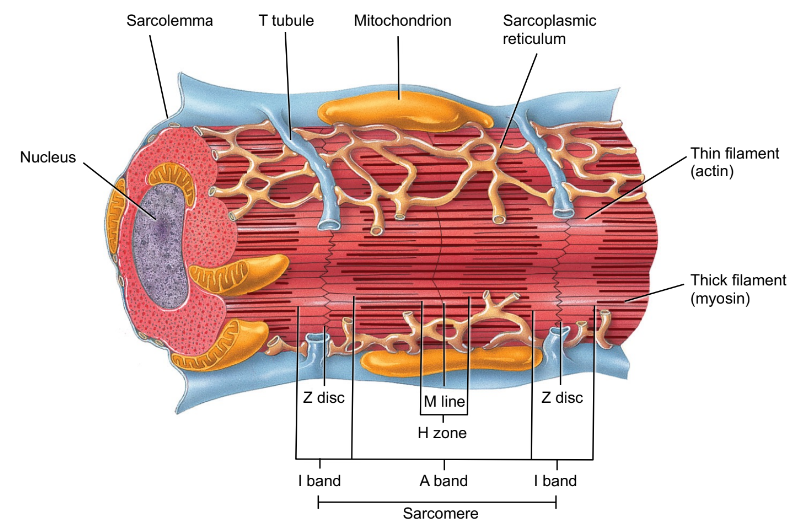
Describe the features of cardiac muscle. (4)
- Striated.
- Branched.
- Single nucleus.
- Joined end to end.
- Branched.
- Single nucleus.
- Joined end to end.
3
New cards
Cardiac muscle is joined end to end. What features allow this to happen?
- Intercalated discs that connect muscles with the help of desmosomes.
- Gap junctions that allow electrical current transmission.
- Gap junctions that allow electrical current transmission.
4
New cards
What are desmosomes?
A type of junction in which cells are fastened together in strong sheets (like rivets).
5
New cards
What are gap junctions?
Small tunnels that connect cells, facilitating the movement of small molecules and ions between the cells.
6
New cards
The way cardiac muscles interact (joined end to end) allow what?
- Functional syncytium where individual chambers act as a single coordinated unit.
- All or none contraction pattern (no graded responses).
- All or none contraction pattern (no graded responses).
7
New cards
Why is the all or none contraction of the heart important?
To ensure that equal amounts of blood are being sent out and brought in.
8
New cards
Cardiac muscle relys on what type of metabolism?
Aerobic (oxygen-requiring).
9
New cards
25% of the volume of cardiac muscle is what?
Mitochondria.
10
New cards
In order for aerobic metabolism to take place in heart muscle, there must be an abundance of oxygen. How does the muscle keep oxygen?
Using myoglobin.
11
New cards
What is myoglobin?
This is a protein found in muscles and it is very similar to hemoglobin. It is an oxygen-binding compound.
12
New cards
Cardiac muscle has a less extensive sacroplasmic reticulum compared to skeletal muscle, meaning what?
It has a smaller intracellular Ca2+ reserve.
13
New cards
How is calcium used in the sacroplasmic reticulum of cardiac muscle?
It is not used in the same way as skeletal muscle. The sacroplasmic reticulum holds calcium and will only release it when there is calcium coming into the tissue from outside the cell. This will then trigger the sacroplasmic reticulum to release the rest of the Ca2+, if needed.
14
New cards
Does the heart contract with or without the nervous system?
Without. However, rhythm can be altered by the autonomic nervous system (ANS).
15
New cards
What are the two types of electrical events of the heart?
The intrinsic conduction system and the extrinsic innervation of the heart.
16
New cards
What is the intrinsic conduction system?
Heart muscle cells contract, without nerve impulses, in a regular, continuous way. It sets the basic rhythm of the heart. This comes from inside the heart.
17
New cards
What is the extrinsic innervation of the heart?
Heartbeat modified by ANS via cardiac centers in medulla oblongata (ANS). This comes from outside the heart.
18
New cards
The intrinsic conduction system consists of what?
Cardiac pacemaker cells.
19
New cards
What are cardiac pacemaker cells?
Non-contractile cardiac muscle cells.
20
New cards
What is the job of the pacemaker cells?
It produces the electrical impulses that cause your heart to beat.
21
New cards
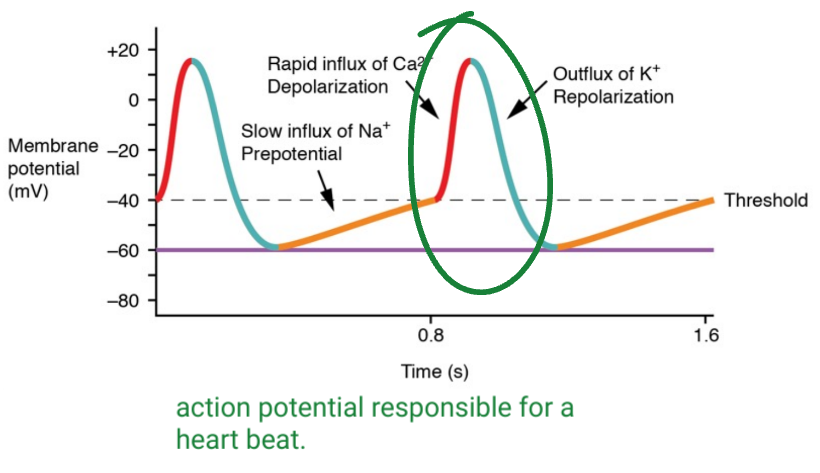
What are pacemaker potentials?
Unstable resting potential that leads to an action potential. This is due to "funny" Na+ leak channels (channels that stay open at rest).
22
New cards
The action potential of a pacemaker cell is caused by what type of channels?
Voltage-gated Ca 2+ channels.
23
New cards
True or False: During the unstable resting potential of a pacemaker cell, there is some Na+ that is entering the cell, thus making it positive. Once it hit threshold, an abundance of Ca2+ enters the cell, thus causing depolarization and an action potential. An outflux of K+ will then bring down the "positivity" within the cell and return it back to the unstable resting potential
True.
24
New cards
Does calcium cause depolarization in only non-contractile muscle cells?
Yes.
25
New cards
What is the sinoatrial (SA) node?
It is a structure in the right atrium that tells the heart to "beat" or squeeze by sending out an electrical signal.
26
New cards
Action potentials are conducted throughout the heart via?
Gap junctions and conducting system.
27
New cards
The action potentials of the pacemakers are responsible for what?
Heart beats.
28
New cards
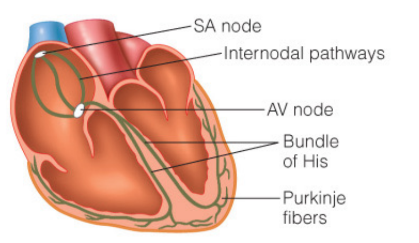
The intrinsic conduction sequence consists of four landmarks where the impulse passes through the pacemaker cell. What is the order?
1. Sinoatrail (SA) node.
2. Atrioventricular (AV) node.
3. Atrioventricular (AV) bundle (bundle of His)
4. Purkinje fibres (subendocardial conducting network).
2. Atrioventricular (AV) node.
3. Atrioventricular (AV) bundle (bundle of His)
4. Purkinje fibres (subendocardial conducting network).
29
New cards
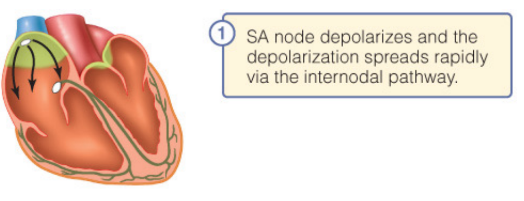
Describe the first landmark, the sinoatrial (SA) node for the impulses of the pacemaker cell.
It is located in the right atrium and is the primary pacemaker for the heart. It causes an impulse that spreads over both atria.
30
New cards
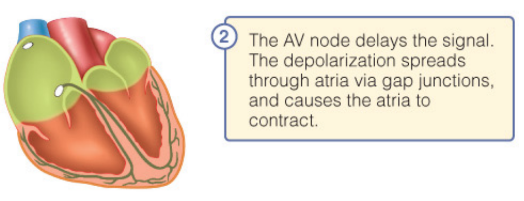
Describe the second landmark, the atrioventricular (AV) node for the impulses of the pacemaker cell.
It is located in the interatrial septum and is the electrical connection to the ventricle. It delays firing slightly to allow atria to finish contracting before ventricles contracts.
31
New cards
Why is it important that atria contract before ventricles?
To ensure that there is blood available in the ventricles for contraction.
32
New cards
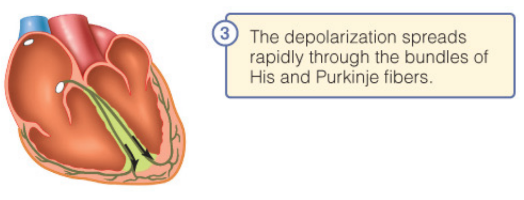
Describe the third landmark, the atrioventricular (AV) bundle (bundle of His) for the impulses of the pacemaker cell.
This conducts impulses into ventricles from the AV node. It has a right and left bundle branches that conduct impulses down the interventricular septum.
33
New cards
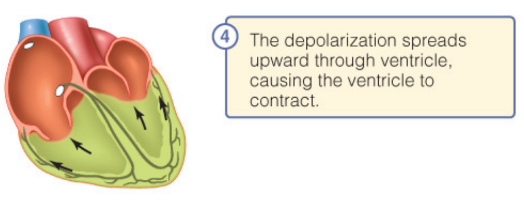
Describe the forth landmark, the purkinje fibres (subendocardial conducting network) for the impulses of the pacemaker cell.
This penetrates throughout ventricular walls, distributing impulses through the ventricles. This allows ventricles to contract, beginning at the apex, and moving towards atria.
34
New cards
Why is it important that contraction begins at the apex (bottom) of the ventricle?
To ensure that the blood is being pushed up and out. If the contraction had occurred at the top of the ventricle, blood would collect at the bottom and bulge since there is no "exit".
35
New cards
Are there gap junctions between atria and ventricles?
No.
36
New cards
What are pacemakers?
Electrical devices used to correct irregularities in the heart rate.
37
New cards
Defects in the intrinsic conduction system can cause what?
Uncoordinated atrial and ventricular contractions.
38
New cards
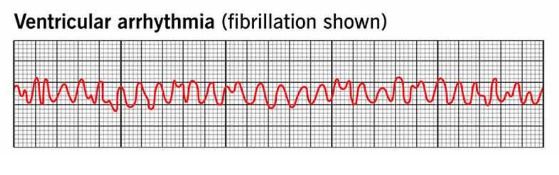
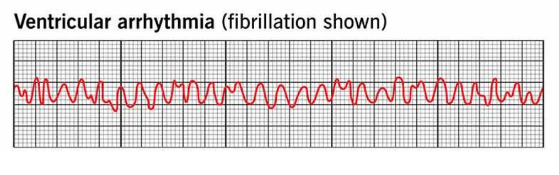
What is arrhythmia?
Irregular heart beat/rhythm.
39
New cards
What is fibrillation?
Rapid, irregular contractions. This causes the heart to become useless for pumping blood, thus causing circulation to cease and can lead to brain death.
40
New cards
What is the treatment for fibrillation?
Defibrillation.
41
New cards
What is defibrillation?
The delivery of an electrical shock that may help re-establish an effective rhythm. It disrupts the chaotic twitching and resets the heart to regular, normal depolarizations.
42
New cards
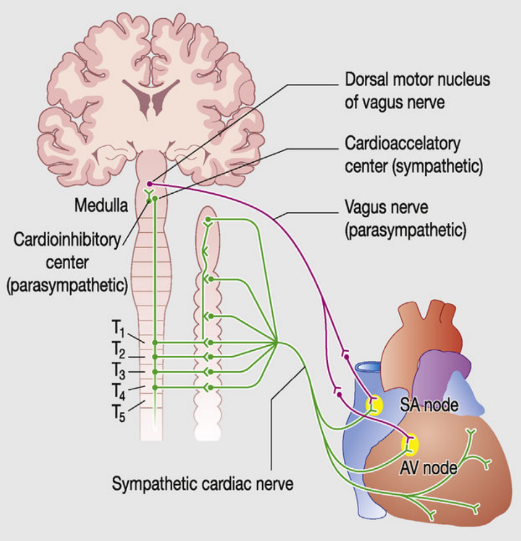
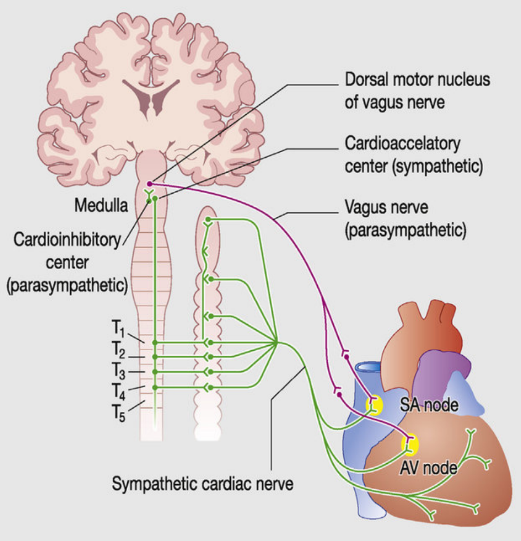
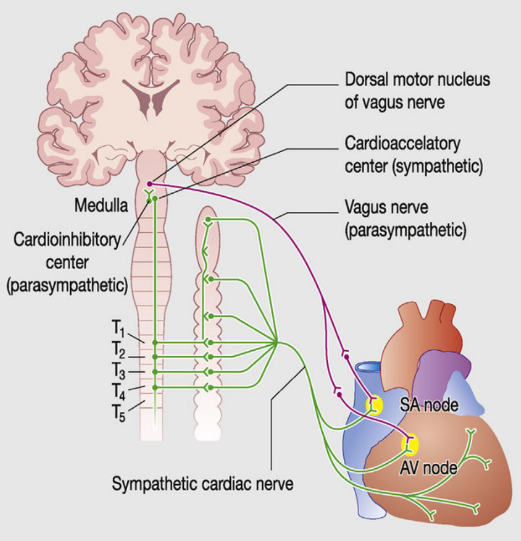
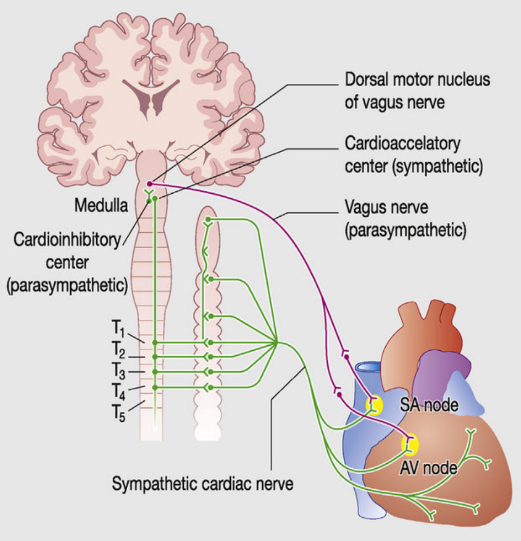
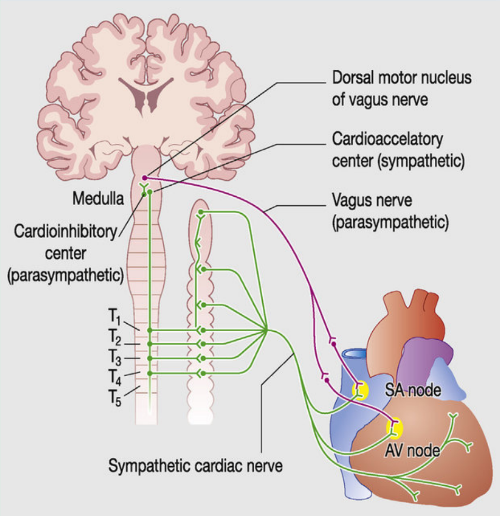
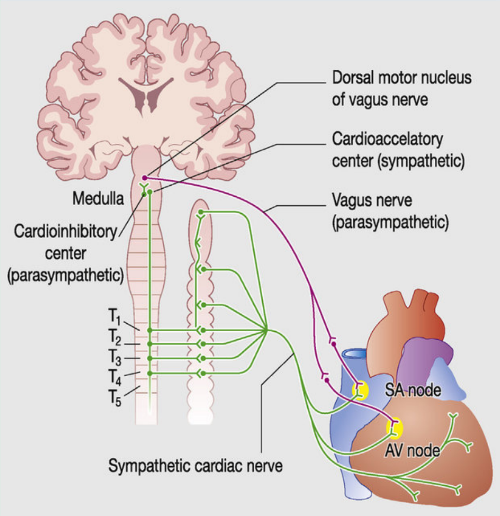
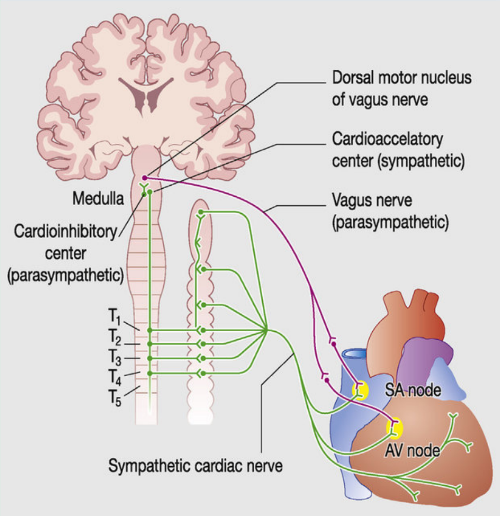
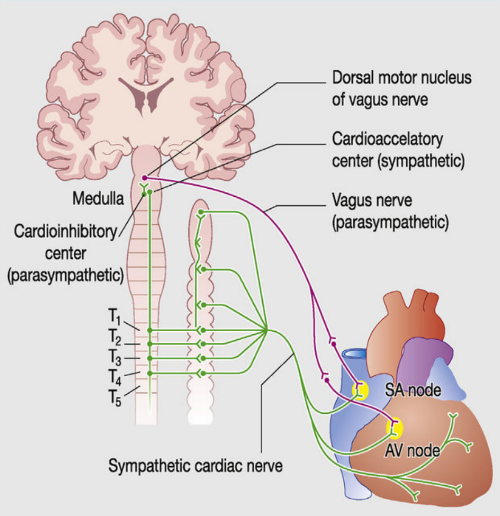
Describe the autonomic regulation of the heart.
The autonomic nervous system (ANS) also plays a role in heart rate as it modifies it and forces contraction through cardiac centres in the medulla oblongata.
43
New cards
In what situation is the ANS vital in controlling heart rate?
Whilst exercising. Your body requires more oxygen to supply muscles, and so the brain signals the medulla oblongata to increase/change the "resting" heart rate.
44
New cards
There are two ways heart rate can be controlled by the ANS, through increasing and decreasing the rate. What are the centres involved in each called?
To increase heart rate, the cardiacceleratory centre is involved. To decrease heart rate, the cardioinhibitory centre is involved.
45
New cards
Describe how the carioacceleratory centre works.
It projects to sympathetic neurons throughout the heart. This increases both the heart rate and contractile force.
46
New cards
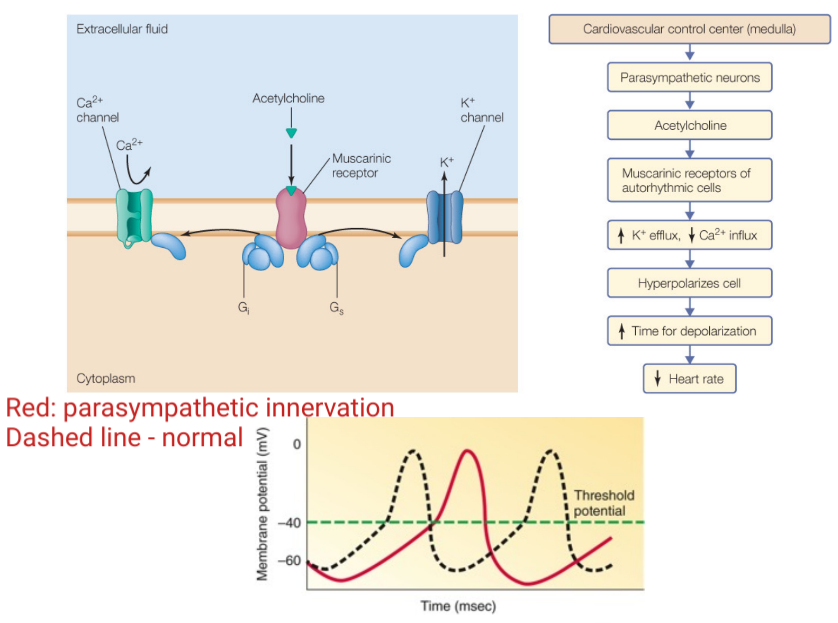
Describe how the cardioinhibitory centre works.
It sends impulses to parasympathetic dorsal vagus nucleus in the medulla oblongata where it will then stimulate the vagus nerve to the heart. This slows heart rate but has LITTLE to NO effect on the contraction force.
47
New cards
Where are both the cardioacceleratory and cardioinhibitory centres found?
In the medulla oblongata.
48
New cards
How is the heart rate adjusted using the sympathetic branch?
1. Adrenergic neurons release norepinephrine/noradrenaline.
2. Adrenal medulla releases epinephrine.
3. B1 adrenergic receptors in the heart (G-protein coupled receptors) are activated by the sympathetic system using both epinephrine and norepinephrine.
4. cAMP-mediated signalling pathway affects ion channels, thus causing Na+ and Ca2+ influx, resulting in depolarization.
5. Enhanced "slow" Ca2+ channels allow for an increase in Ca2+, thus increasing the contractile strength.
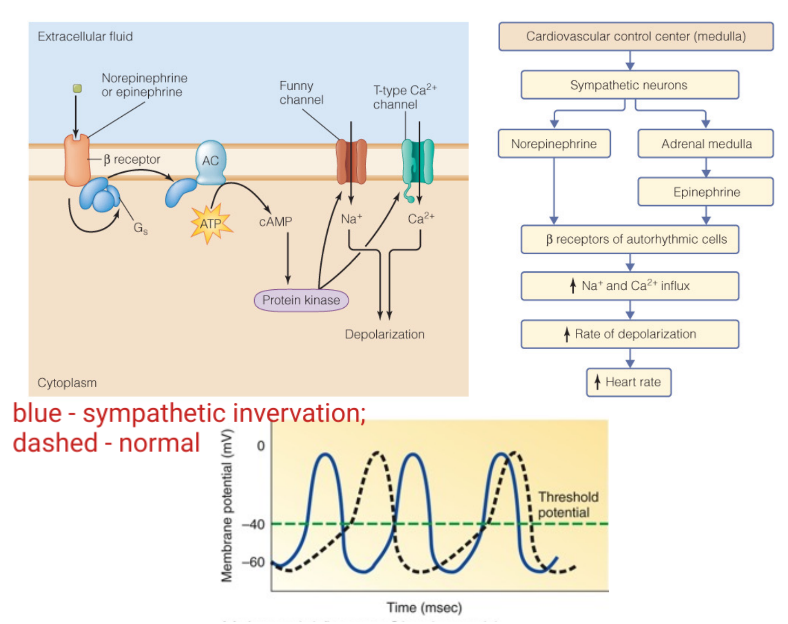
49
New cards
B1 adrenergic receptors are what kind of receptors?
Excitatory receptors.
50
New cards
How is heart rate adjusted using the parasympathetic branch?
1. Cholinergic neurons release ACh.
2. ACh binds to M2 muscarinic cholinergic receptors in the heart.
3. Triggers K+ channels to open, Na+ channels to close. This hyperpolarizes the cell due to it becoming negative (K+ leaving \= increased efflux) and the Ca2+ slowly getting in causing a slower depolarization of the pacemaker potential (Ca2+ not being able to enter \= decreased influx).
2. ACh binds to M2 muscarinic cholinergic receptors in the heart.
3. Triggers K+ channels to open, Na+ channels to close. This hyperpolarizes the cell due to it becoming negative (K+ leaving \= increased efflux) and the Ca2+ slowly getting in causing a slower depolarization of the pacemaker potential (Ca2+ not being able to enter \= decreased influx).
51
New cards
What does cholinergic mean?
This refers to the fact that a receptor uses acetylcholine almost exclusively as their primary neurotransmitter.
52
New cards
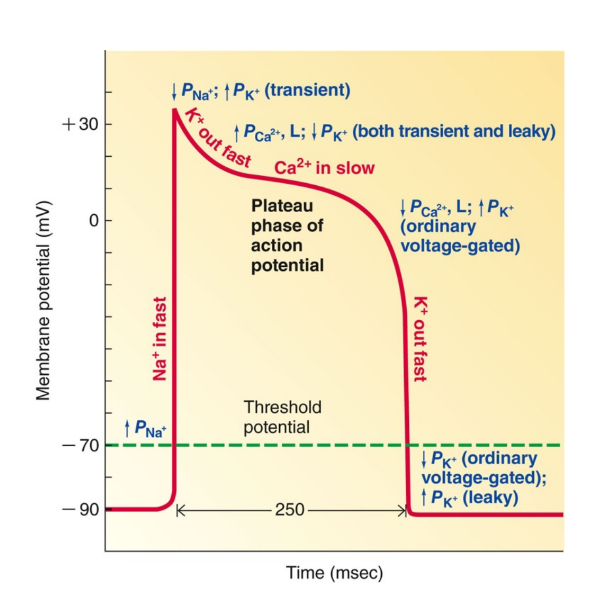
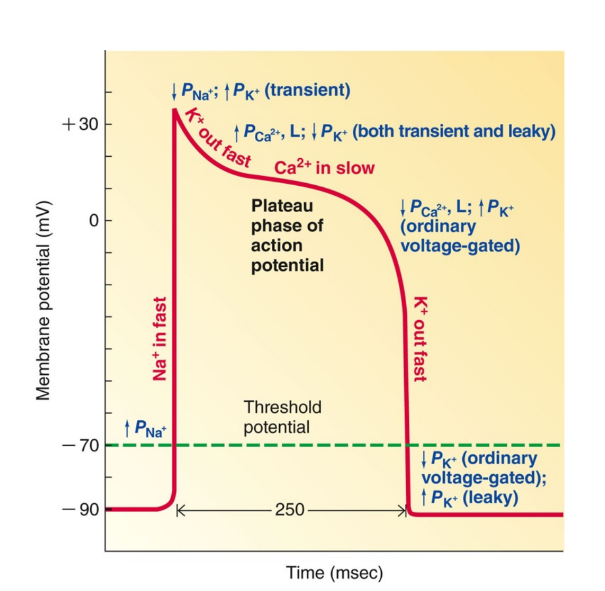
What are the five phases of contractile cardiac muscle cells? (action potential)
1. Rapid depolarization.
2. Brief repolarization.
3. Plateau phase.
4. Rapid repolarization.
5. At rest.
2. Brief repolarization.
3. Plateau phase.
4. Rapid repolarization.
5. At rest.
53
New cards
Describe a contractile cardiac muscle cell during rapid depolarization.
Fast voltage-gated Na+ channels open.
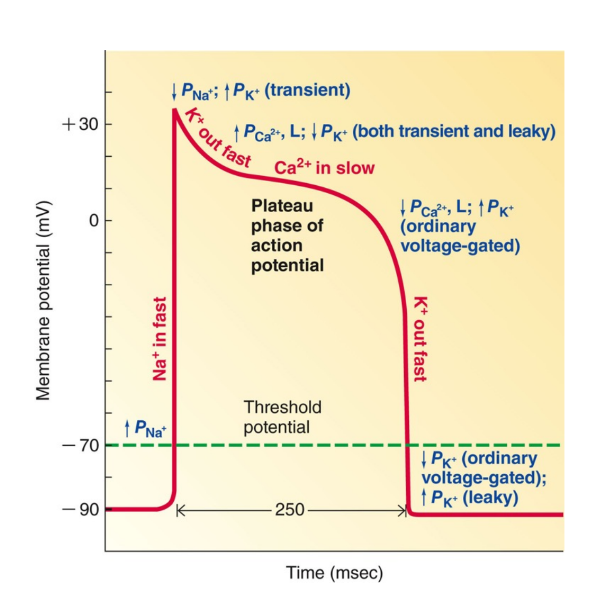
54
New cards
Describe the brief repolarization of contractile cardiac muscle cells.
Transient K+ channels open.
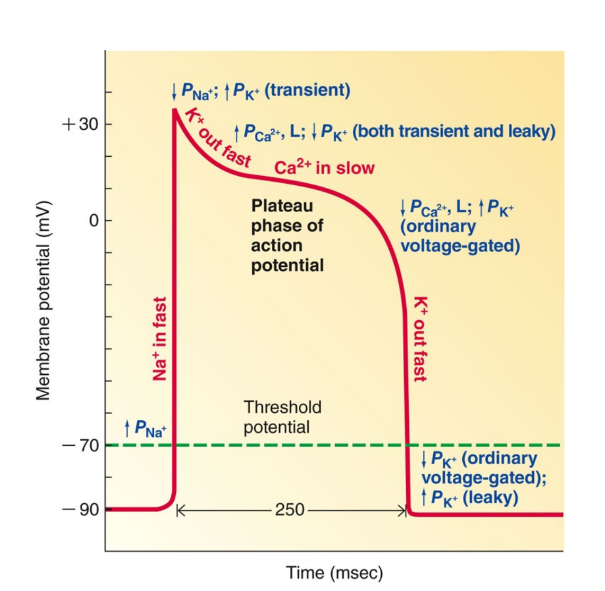
55
New cards
Describe the plateau phase of contractile cardiac muscle cells.
- Only found in contractile cells.
- Has slow Ca2+ channels that open and decrease K+ permeability.
- Has slow Ca2+ channels that open and decrease K+ permeability.
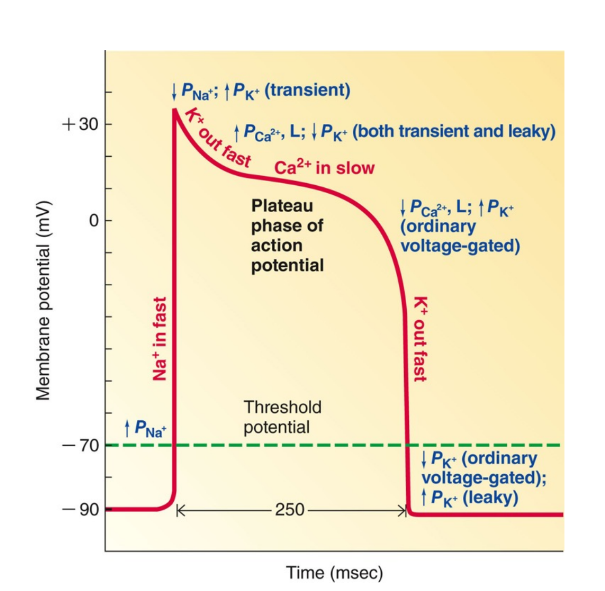
56
New cards
Describe the rapid repolarization phase of contractile cardiac muscle cells.
Innactivation of the Ca2+ channels and delayed activation of "normal" voltage-gated K+ channels.
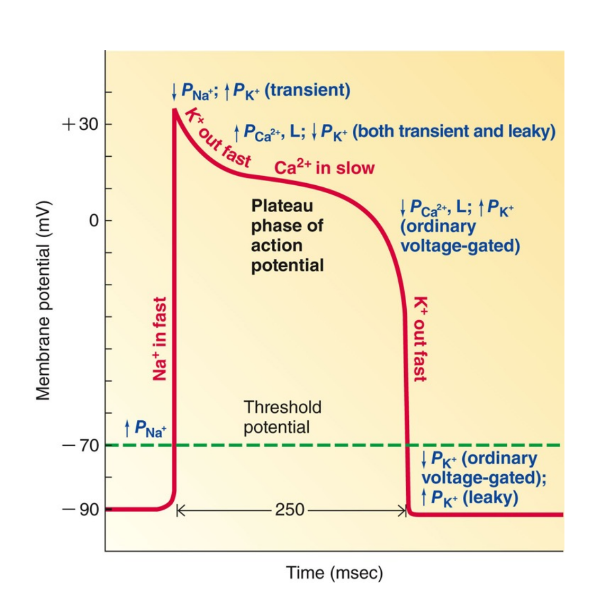
57
New cards
What is the difference between noncontractile cardiac muscle cells and contractile cardiac muscle cells in terms of their channels?
Non-contractile uses calcium, whereas contractile uses sodium.
58
New cards
Describe contracticle cardiac muscle cells at rest.
Voltage-gated K+ channels close, and leaky K+ channels open to allow the cycle to continue again.
59
New cards
Contracticle cardiac muscle cells have no pacemaker potential, meaning what?
That they require a trigger from the conducting cells (pacemaker cell) located somewhere else in the body.
60
New cards
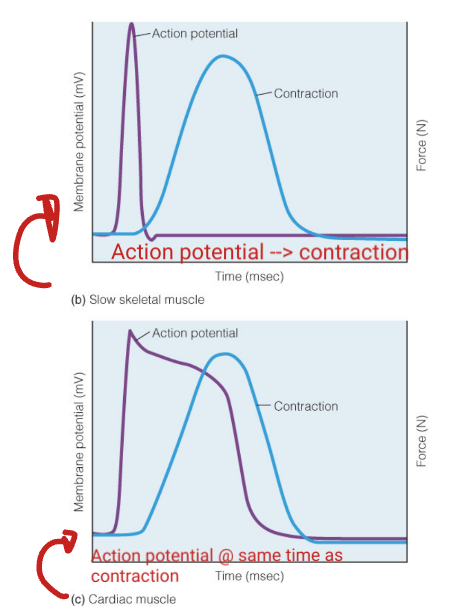
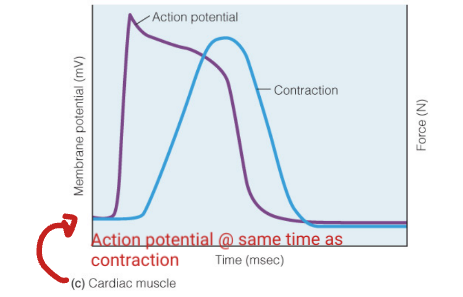
In contractile cardiac muscle cells, the action potential is (shortens/prolonged) relative to skeletal muscle.
Prolonged.
61
New cards
Why are action potentials in cardiac muscle cells more prolonged?
This is due to the more significant role of Ca2+ entry from the extracellular fluid.
62
New cards
Slow contraction of the heart is sustained to ensure what?
All of the blood is squeezed out of the heart.
63
New cards
The heart has a long refractory period. Why?
- The heart can be refilled with blood before contracting again.
- Prevents tetanus of the heart because their is no way you can stimulate another action potential UNTIL the contraction is over.
- Prevents tetanus of the heart because their is no way you can stimulate another action potential UNTIL the contraction is over.
64
New cards
Why would tetanus be bad in the heart?
It cause cause fatigue of the heart muscle and this lead it to halt.
65
New cards
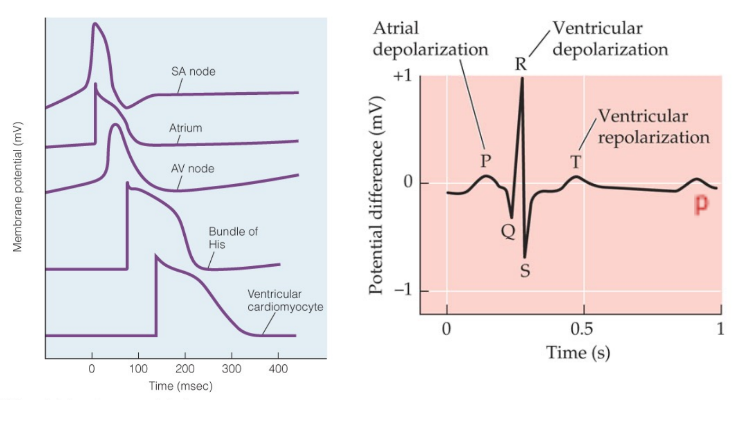
What does ECG stand for?
Electrocardiogram.
66
New cards
Is ECG and EKG the same thing?
Yes.
67
New cards
What is an ECG?
A summation of membrane potential changes (depolarization and repolarization) across all heart cells.
68
New cards
Is an ECG a direct recording of the actual electrical activity of the heart?
No.
69
New cards
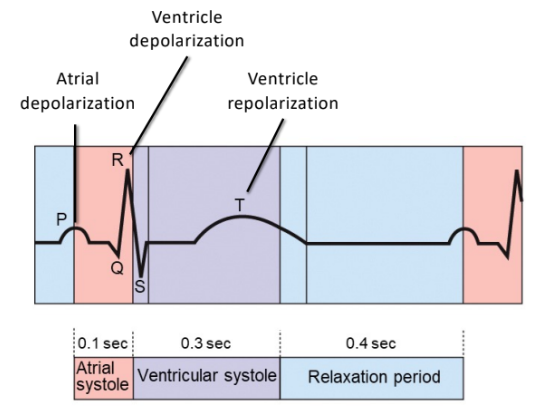
A typical ECG has three deflections, what are they?
- P wave
- QRS complex
- T wave
- QRS complex
- T wave
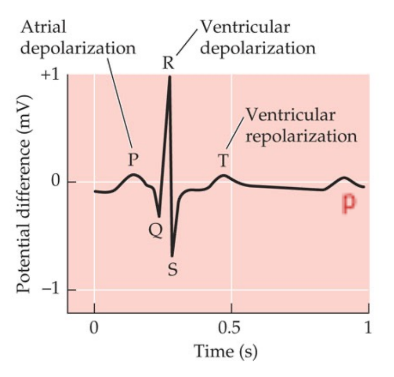
70
New cards
What is a p wave?
It indicated depolarization of the atria.
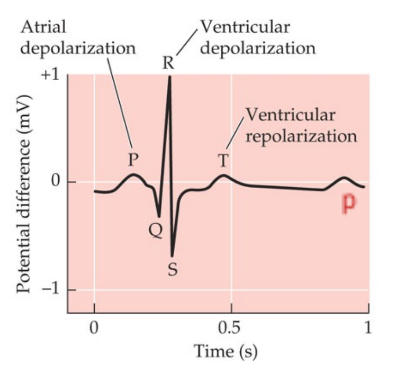
71
New cards
What is the QRS complex?
Ventricular depolarization.
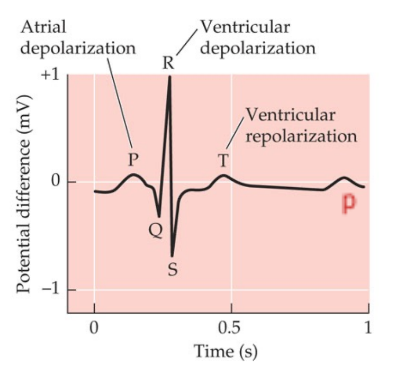
72
New cards
What is a T wave?
Ventricular repolarization.
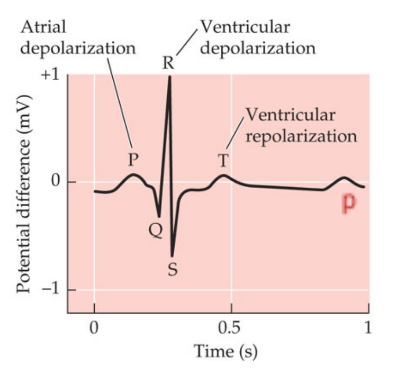
73
New cards
How many different phases are there in a ECG?
6.
74
New cards
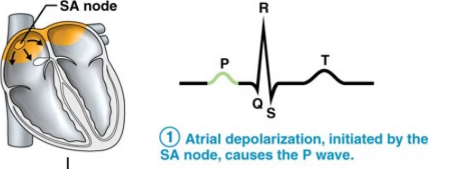
Describe phase 1 of an ECG.
Atrial depolarization occurs. This is initiated by the SA node and causes the P wave.
75
New cards
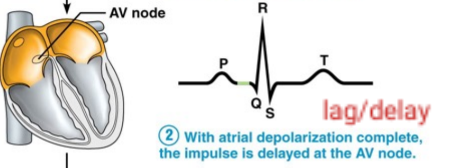
Describe phase 2 of an ECG.
With atrial depolarization complete, the impulse is delayed at the AV node.
76
New cards
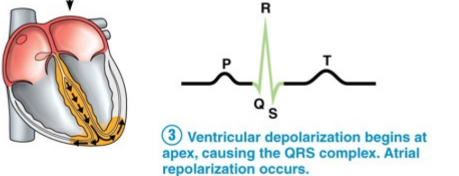
Describe the phase 3 of an ECG.
Ventricular depolarization begins at the apex. This causes the QRS complex. Additionally, atrial repolarization occurs.
77
New cards
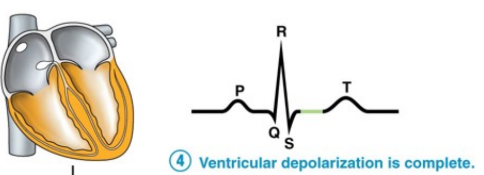
Describe phase 4 of an ECG.
Ventricular depolarization is complete.
78
New cards
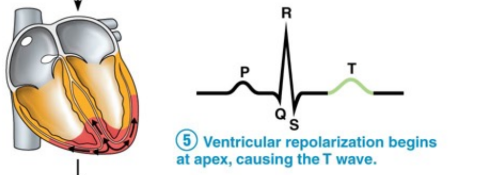
Describe phase 5 of an ECG.
Ventricular repolarization begins at the apex, causing the T wave.
79
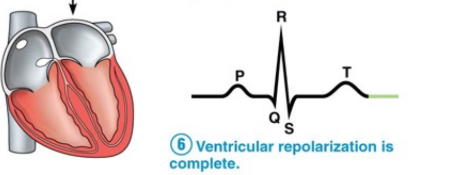
New cards
Describe phase 6 of an ECG.
Ventricular repolarization is compete.
80
New cards
What are the mechanical events of the heart?
- Cardiac cycle
- Systole
- Diastole
- Systole
- Diastole
81
New cards
What is the cardiac cycle?
A series of mechanical events, pressure and volume changes, in the heart during ONE heartbeat.
82
New cards
What is systole?
The contractile phase of the cardiac cycle.
83
New cards
What is diastole?
The relaxation phase of the cardiac cycle.
84
New cards
Atrial systole and diastole are followed by?
Ventricular systole and diastole.
85
New cards
When do ventricles fill?
During mid-to-late ventricle diastole.
86
New cards
Describe the filling of blood that occurs during mid-late ventricular diastole.
- AV valves open and semilunar valves close.
- Blood flows (~80%) passively into ventricles.
- Blood flows (~80%) passively into ventricles.
87
New cards
When do the atria contract?
During the end of the ventricular diastole.
88
New cards
Describe the contraction of atria that occurs during the end of the ventricular diastole.
- Propels final blood volume (remaining 20%) into ventricles.
89
New cards
What is the end diastolic volume?
The volume of blood in each ventricle at the end of ventricular diastole. (after the atrium contracts, but before the ventricle contracts).
90
New cards
What is ventricular systole?
Where the atria relax and the ventricles contract.
91
New cards
What is isovolumetric contraction?
The first phase of ventricular systole. All the valves are closed at this point because the volume of the ventricle is not changing.
92
New cards
What is ventricular ejection?
Where the ventricular pressure exceeds that of the atrial pressure. This forces semilunar valves open to eject blood into the arteries.
93
New cards
What is the end systolic volume?
The volume of blood remaining in each ventricle after systole. This prevents the atria from having more pressure than the ventricles.
94
New cards
When does isovolumetric relaxation occur?
During early diastole.
95
New cards
What is isovolumetric relaxation?
A brief period in early diastole when all valves are closed.
96
New cards
How does isovolumetric relaxation occur?
Results in a drop in ventricular pressure which causes the closing of semilunar valves before the opening of AV valves. This prevents backflow.
97
New cards
Is there a change in volume during isovolumetric relaxation?
No.
98
New cards
What is the dicrotic notch?
A brief rise in blood pressure as blood rebounds off semilunar valves due to the backflow of blood in the aorta and pulmonary trunk.
99
New cards
When atrial pressure exceeds ventricular pressure, what happens?
AV valves open and the cycle begins again.
100
New cards
What are the normal sounds of the heart?
Lub (S1) and Dub (S2)